Abstract
Background
Better understanding of the factors that influence patients to make a financial claim for compensation is required to inform policy decisions. This study aimed to assess the relative importance of factors that influence those who have experienced a patient safety incident (PSI) to make a claim for compensation.
Method
Participants completed an online discrete choice experiment (DCE) involving 10 single profile tasks where they chose whether or not to file a claim. DCE data were modelled using logistic, mixed logit and latent class regressions; scenario analyses, external validity, and willingness to accept were also conducted.
Results
A total of 1029 participants in the United Kingdom responded to the survey. An appropriate apology and a satisfactory investigation reduced the likelihood of claiming. Respondents were more likely to claim if they could hold those responsible accountable, if the process was simple and straightforward, if the compensation amount was higher, if the likelihood of compensation was high or uncertain, if the time to receive a decision was quicker, and if they used the government compensation scheme. Men are more likely to claim for low impact PSIs.
Discussion and Conclusions
The actions taken by the health service after a PSI, and people’s perceptions about the probability of success and the size of potential reward, can influence whether a claim is made. Results show the importance of giving an appropriate apology and conducting a satisfactory investigation. This stresses the importance around how patients are treated after a PSI in influencing the clinical negligence claims that are made.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
It is important to understand the relative importance of factors that influence people to make a claim for financial compensation after a patient safety incident (PSI) so that health services can appropriately respond to such events. |
If participants are satisfied with the investigation and if they received an apology, the probability to claim decreases. |
The probability of claiming increases if the process to apply is made easier and if the time to receive a decision is shorter. |
The probability of claiming decreases when the health service responds appropriately after the PSI and also makes the claims process more accessible to patients. |
1 Background
It is inevitable that in some cases unintentional harm occurs in the delivery of medical treatment; therefore, it is vital that where patients experience harm while receiving clinical care (hereafter referred to as a patient safety incident [PSI]), health systems have appropriate mechanisms in place to provide redress. In the United Kingdom (UK), patients who experience a PSI may choose to make a financial claim for compensation resulting from clinical negligence against the National Health Service (NHS). While in 2020/2021 the liabilities arising from claims decreased by £1.3 billion, from £84.1 billion to £82.8 billion, and the cost of settling claims reduced by £120 million to £2.26 billion, the expenditure on administration of all activities of NHS Resolution rose by 15% to £35.4 million [1]. The costs of these claims are covered from the NHS budget, representing significant opportunity costs. It may be that other schemes can be devised that provide appropriate redress but avoid costly administration and adversarial legal processes.
Prior qualitative research has identified factors that influence whether people who have experienced a PSI choose to make a claim of clinical negligence [2]. However, the relative importance of factors, or how the combination of these influenced the choice to make a claim, is not considered. Better understanding of both the factors that influence the choice to make a claim and the relative importance of these factors are now required to inform policy development. This paper was designed to provide this more detailed understanding through evidence gathered from a discrete choice experiment (DCE). The DCE explored a range of candidate factors that influence the choice of a patient who had experienced harm to pursue compensation claims, and their relative importance, alone and in combination.
This study expands upon the work of Rowen et al. [3], which investigated the preferences of the UK general population regarding factors influencing clinical negligence claims. It could be argued that the informed stated preferences of people who have experienced a PSI would be more directly relevant for policy decisions than the preferences of members of the general population imagining whether they would claim for financial compensation following a hypothetical PSI. The rationale for replicating the research with a sample of people who experienced harm is that their preferences will be informed by their prior experiences. The aim of this paper was to determine the relative importance of the factors that people who have experienced a PSI consider in their decision whether to make a financial claim to compensate them for the unintended or unexpected harm caused while receiving treatment from the NHS. The objectives of this paper were to (1) understand the harm experienced by the participants; (2) understand the experience of participants in the aftermath of a PSI; and (3) elicit and model the stated preferences of people who have experienced unintended harm (to themselves or to relatives) arising from treatment in the NHS.
2 Methods
In this online DCE, participants had to imagine the PSI that they had themselves experienced, or the PSI experienced by a member of their immediate family. Participants were asked to simultaneously think about the features of the PSI they experienced (context setting) and consider hypothetical actions taken after the PSI and the features of a scheme (DCE choices). The design of the DCE was a single profile task where participants were provided with a binary choice as to whether they would make a financial claim for compensation or not.
2.1 Determining the Discrete Choice Experiment (DCE) Attributes, Scenarios and Wording
The same attributes used in the previous general population DCE survey were maintained to describe the actions of the NHS following the PSI and details of the claims process for this research to ensure comparability of results across both pieces of research [3]. As detailed in the latter paper, the attributes for the DCE were identified by conducting a literature review with inputs from policy makers [2, 4,5,6,7,8,9,10]. Minor changes to some attribute levels were required to ensure these were appropriate for use in a population who were answering about the harm they (or an immediate family member) had experienced.
Survey participants were asked to answer the questions about whether or not they would make a claim for the PSI that they themselves experienced either personally or experienced by an immediate member of the family. It was important that participants were able to complete the survey on behalf of an immediate family member to ensure that preferences around the more severe PSIs, including those resulting in death, severe disability and paediatric PSIs were captured. In circumstances where participants had experienced more than one PSI, they were asked to imagine the most recent one experienced by themselves or by an immediate family member. We did not provide a definition for an immediate family member, but if participants were reporting on behalf of someone else they were asked to state their relationship to them. Participants were also asked to self-report on the impact of the PSI on physical/mental health. This question was used to allocate participants to two routes of the DCE. Those who classified the impact as insignificant, short-term minor and short-term major, and death of an immediate family member were allocated to the low impact route with lower compensation amounts. Those who considered the impact to be long-term minor and long-term major were allocated to the severe impact route and shown higher compensation amounts. While death is a serious event, the compensation amounts paid in such situations tend to be low and are capped. Consequently, participants reporting a death were shown levels commensurate with what they might have been offered in the real-world compensation process.
While the wording of attributes had already been tested in the previous survey with the general population [3], qualitative interviews were conducted to ascertain whether potential participants were able to use their own experience of harm as the context and framing for the DCE questions, while simultaneously considering attributes that were likely to be different from what they experienced. The qualitative interviews were undertaken with a sample of 10 participants (6 females, 4 males) who experienced harm while receiving treatment in the NHS, recruited via a list of volunteers at the University of Sheffield (n = 2) and from a third sector organisation (charity) specialising in patient safety (n = 8).
The DCE included the following eight attributes (number of levels): apology (2); investigation and prevention (3); holding to account (2); difficulty of making a claim (2); length of claim process (3); chance of compensation (3); amount of compensation (4); and the compensation avenue in the form of a legal claim or a government compensation scheme (2). More details on the attributes and levels are reported in electronic supplementary material (ESM) Table S1. The attribute ‘investigation and prevention’ contains two separate factors that were merged as a single attribute in the analyses since they are interrelated. Although the two factors were presented separately in the survey, they are combined into a single attribute in the modelling.
2.2 Design
A fractional factorial, single profile design was selected using a D-optimality algorithm using the dcreate command in Stata 17 [11]. The same design was used for each of the two routes, with each route consisting of 64 choice sets. From the 64-choice set, eight DCE questions were randomly drawn without replacement and presented to the respondents to complete. The choice sets allow for the estimation of all main effects and six interaction effects (ESM Table S2).
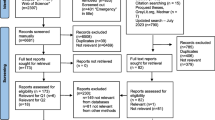
2.3 The Sample and DCE Survey
Participants in England, Wales, Scotland and Northern Ireland were recruited through a market research panel. Eligibility to take part in the study was assessed using screening questions. Respondents self-reported whether they experienced harm themselves or have had an immediate family member who had experienced harm while receiving treatment from the NHS. Participants were excluded from the survey if they completed the survey in under 5 min. This cut-off was introduced to exclude people who were ‘speeding’ without paying attention to the tasks.
Participants viewed an information sheet about the survey and provided informed consent before being allowed to proceed to the survey. There were five parts to the survey: (1) questions around the PSI; (2) a short video explaining the DCE tasks and the factors covered in the DCE; (3) two practice DCE questions followed by a free-text box to provide a brief justification for their decision to claim or not; (4) respondents allocated to either low or severe impact routes and given eight DCE questions to complete (Fig. 1); and (5) sociodemographic characteristics, health, attitudes towards the NHS (questions taken from the British Social Attitudes Survey) and perceived difficulty of the DCE tasks [12]. Participants who always chose to make a claim for compensation or always chose not to (i.e. did not trade), were asked to provide a reason for their choice in part 4 of the survey.
2.4 Pilot DCE Survey
The DCE survey was soft launched with a sample of 100 people to check whether participants were engaging with the task; the random selection of choice sets functioned as intended; the data were being recorded without any errors; and the routing of participants to the low or severe impact routes of the survey was working as intended. The data were analysed to inform whether changes were required before proceeding to recruit the remaining participants.
2.5 Modelling Preferences of the Sample
Due to the differences in the severity levels for the compensation and length of process attributes, separate models were estimated for each route. The DCE survey data were modelled using both logistic and mixed logit regressions. To explore preference heterogeneity, mixed logit models were estimated with all attributes and the constant normally distributed. The models were fitted using 1000 Halton draws with the Stata command mixlogit [14]. Linearity of the compensation attribute was assessed and when appropriate, willingness to accept (WTA) values were calculated. This was calculated by dividing the regression coefficients of each attribute by the coefficient for compensation amount. The resulting marginal WTA indicates the amount of money that an individual would require to forgo compensation for each attribute level change. The 95% confidence intervals were calculated using the delta method.
The choice probability of making a claim in a base-case scenario with all categorical attributes set to their reference level are reported, along with the difference in the choice probability of making a claim in an alternative scenario when a combination of attributes are changed from the level used in the base case. The choice probabilities (probabilities hereafter) are derived from a hypothetical stated preference survey and are not intended to predict actual behaviour. Instead, the probabilities are calculated to understand the scenarios that would most or least likely lead to a claim given the set of factors described in the DCE.
Latent class models were used to further examine preference heterogeneity using the Stata command lclogitml2 [13]. The optimal number of classes were selected using the Bayesian Information Criterion (BIC) and Consistent Akaike Information Criterion (CAIC). After selecting the optimal number of latent classes, we included sociodemographic characteristics and attitudes in the class membership part of the model. The covariates considered were sex, age, ethnicity, income, employment, impact of PSI, NHS satisfaction, and made a claim for their own PSI. These covariates were included in the model one at a time and the final model only contains the covariates that led to convergence. In addition, to evaluate the robustness of the original latent class results, a further latent class model was estimated with an additional class that constrained all attributes to zero. This model was used to examine task non-attendance with the assumption that there is a group of respondents who are inattentive to all the attributes presented in the task [16, 17].
As the survey also gathered data on revealed preferences, concordance between predicted choice and actual choice was calculated. The revealed preference data included whether the respondent made a claim, whether they received an apology and whether they were satisfied with the prevention steps put in place by the NHS. For the remaining attributes, actual data were unavailable, hence assumptions were made (Table 6) for these attributes for all respondents. Using the results of the latent class model, we calculated the predicted choice probability (unconditional on class) using the respondents’ actual data. A threshold value of 0.5 was used to dichotomise this predicted probability, with a value < 0.5 representing that the respondent did not make a claim, and a value > 0.5 representing that the respondent did make a claim. This predicted choice was then compared with the respondents’ actual choice of making a claim to determine the concordance between predicted and actual choices as a percentage of predictive accuracy.
3 Results
3.1 Pilot DCE Survey
Data analysis based on 100 participants revealed no issues of concern. The justifications provided after the practice questions were indicative of participants having understood the tasks. No changes were made to the DCE tasks but one minor change was made to a question in the first section of the survey, where a free-text answer was replaced by a multiple-choice answer.
3.2 Main DCE Survey Sample
Table 1 shows the sociodemographic characteristics of the sample consisting of 1029 participants. Most of the sample were female (57%), under 40 years of age (61%), married (74%), employed (76%), of White ethnicity (85%), educated to A-level or above (79%) and healthy (82%). Data collection took place between July and August 2021.
3.3 Understanding the Harm Experienced by Participants
Only one-quarter of the population answered the survey based on the experience of harm that happened to them; the remaining participants responded about a PSI that occurred to an immediate family member (Table 2). For 7% of respondents, the harm occurred to their child. Approximately 80% of the time the PSI took place in the last 5 years, at a hospital setting (Table 2). A variety of PSIs were reported by participants, but among the most common PSIs were harm related to wrong or missed diagnosis (19%) and delay in treatment (18%). The impact of the PSI on health was short-term or insignificant in 60% of the sample, long-term in 34% of the sample and resulted in death 6% of the time. After the PSI, 39% of people had to take time off work and 19% each had to retire or move to a less demanding job (Table 2). Further details about the PSI are presented in ESM Table S8.
3.4 Understanding the Experience of Participants in the Aftermath of the Patient Safety Incident
Approximately half of the respondents did not receive an apology or explanation, or were told that an investigation was not carried out after the PSI (ESM Table S8). Of those who did receive an apology or explanation, most (86%) were totally or partially satisfied with it. Similarly, most people (84%) were totally or partially satisfied with the outcome of the investigation that was carried out. After the PSI, half of the sample (52.4%) made a complaint. One-third of the sample were not satisfied with the outcome of the complaint. Half the sample decided against making a legal claim, but 22% made a legal claim and 16% are yet to make a legal claim. The main reasons why respondents decided against making a legal claim were the unwillingness to pursue a legal claim against the NHS or that they did not want NHS funds to be used in this way. The main reasons for making a claim for compensation were because the PSI had ‘too much of an impact’ (16%) and to hold the NHS to account (14%). When respondents were asked what the NHS could have done to prevent them from making a claim for compensation, 17% stated an apology and explanation from those responsible for the PSI, 17% stated that the NHS could have taken appropriate measures to prevent this type of PSI from happening again, 16% mentioned that the NHS could have been more upfront and honest about what happened, 16% stated that the NHS could have held those responsible for the PSI to account, 15% mentioned that the NHS could have carried out a satisfactory investigation, and another 15% stated that the NHS could have provided support to cope with the effects of the harm. It is worth noting that only 3% stated that nothing could have been done. More details on the harm experienced and the aftermath can be found in ESM Table S8.
3.5 Participants’ Understanding of the DCE Tasks
The majority of participants found the survey easy to understand (90%) and answer (86%). All participants completed two practice questions and provided a rationale behind their decision to claim or not. Unsurprisingly, the two main reasons why people chose to claim were to receive an apology or compensation and to hold the NHS to account. Some reasons why people chose not to claim were length of the claims period, the hassle of making a claim, and not wanting to use NHS funds in this way. The median time taken to complete the survey was 9.78 [6.35] min and is broadly similar in the low and severe impact routes.
Thirty-three percent of the sample displayed ‘non-trading’ behaviour, thereby always choosing to make a claim (19%) or always choosing not to make a claim (14%) in all of the eight DCE tasks presented to them (Table 3). The reasons provided by the participants about why they always chose to make a claim in the DCE tasks were because they believed that the NHS had ‘let them down’ leaving them with life-changing complications (in some cases death of immediate family members) and thus they felt it was justified to receive compensation to deal with the consequences of the harm experienced. The reasons provided by the participants about why they never chose to make a claim in the DCE tasks was because they did not want NHS funds to be used in this way and because the respondents had ‘forgiven the NHS’.
3.6 Modelled Preferences
Low impact route (Fig. 2 and ESM Table S4): Modelled mixed logit results show that participants are less likely to claim if an appropriate apology and explanation is given, or if an investigation was carried out and they were satisfied/not satisfied that the NHS had taken appropriate measures to prevent this PSI from happening again. Respondents are more likely to claim if they can hold those responsible to account, if the compensation amount is larger; if there is a high chance of receiving compensation; if the process is easy and straightforward; if they do not know how likely they are to get compensation; if the time to receive a decision is 1 year; and if they used the government compensation scheme, all compared with the base level. The constant is negative and significant, suggesting that overall respondents are choosing not to claim.
Severe impact route (Fig. 3 and ESM Table S5): Attributes that decrease the likelihood of making a claim are receiving an apology or explanation, carrying out an investigation, and the NHS taking appropriate measures to prevent a similar PSI from happening again. The factors that increase the likelihood of making a claim are if they can hold those responsible to account; if the process is easy and straightforward; if there is a high chance of receiving compensation; if the compensation amount is higher; if the time to receive a decision is 6 or 3 years; and if they used the government compensation scheme, all compared with the base level. The constant is negative and significant, suggesting that overall respondents are choosing not to claim.
3.7 Probability of Making a Claim Under Different Scenarios
Table 4 presents the results of the scenario analyses conducted using logistic regression model results (ESM Table S3). There is a base case for each of the low impact and severe impact routes representing the most pessimistic or worst levels of the attributes from the point of view of the participants (see Table 4 for actual levels). If we assume that the base-case scenario reflects the current scheme available to a person who was harmed under the low impact route, scenario A shows that by providing an appropriate apology and carrying out a satisfactory investigation, the predicted probability to claim decreases by 22.14 percentage points from a baseline probability of 43.33%; scenario B shows that by making changes to the scheme like making the application process easy, the length of process of 1 year and via a government compensation scheme would increase the predicted probability to claim by 14.49 percentage points; however, if the same changes to the scheme are made and the NHS apologises to the patient and carries out a satisfactory investigation (scenario C) then the predicted probability of claiming decreases by 10.79 percentage points. Further scenarios are presented in Table 4.
3.8 Further Exploration of Preference Heterogeneity
3.8.1 Low Impact Route
Latent class analysis (LCA) identified three groups of respondents who have distinct preferences for their willingness to make a claim in the low impact route (Fig. 4, Table 5, and ESM Table S6). A model with three classes was preferred to a two-class model based on the goodness-of-fit (BIC/CAIC) scores, while a model with four classes failed to converge. Group one (16% of the sample) were less likely to make a claim and these respondents did not have strong preferences for the attributes presented to them. Qualitative data collected as free text in the online DCE survey showed that such respondents were not willing to make a claim because they did not want to take money from the NHS, among other things. Group two (23.5%) were more likely to make a claim, and the attributes that significantly influenced their decision were not receiving an apology, and receiving £100,000 (relative to £5000) in compensation. Respondents in class three (60.5%) took into account all the attributes presented to them when deciding whether to make a claim, and this group of respondents were therefore the most likely to be influenced by any changes to the claims process and the NHS response to the PSI. The parameters for the compensation attribute were linear only in class three, which means that we can estimate WTA values for this class (see Sect. 3.9) but not for the other classes.
The sociodemographic characteristics used in the class membership function showed the types of respondents who were likely to be in class 2 and 3 compared with class 1. Respondents in class 2 were more likely to be male and have already made a claim or are planning to make a claim for their own PSI. Respondents in class 3 were less likely to be older adults.
3.8.2 Severe Impact Route
LCA identified two groups of respondents who have distinct preferences for their willingness to make a claim in the severe impact route (Fig. 5, Table 5, and ESM Table S6). Respondents in class one (30.2%) were less likely to make a claim; However, the attribute levels that would significantly influence them to make a claim were having a high chance of success in receiving compensation (relative to low chance), and having a shorter (3 years relative to 10 years) time to decision. Group two (69.8%) were more likely to make a claim. The attribute levels that significantly increased their decision to make a claim were having an easy and straightforward claims process (relative to complicated and a hassle), having a high chance of success in receiving compensation (relative to low chance), having a shorter (3 or 6 years relative to 10 years) time to decision, applying under a government scheme (compared with a legal scheme), and receiving £1 million (relative to £100,000) in compensation. They were less likely to make a claim if they received an apology and the NHS investigated and put steps in place to prevent such PSIs from happening again. Respondent characteristics (sex, age, ethnicity, employment, PSI impact, and NHS satisfaction) used in the class membership function were not statistically significant.
To examine the robustness of the results mentioned above, a task non-attendance class was added to the latent class model by constraining preference weights for all attributes in that class to zero. This model converged for the severe impact route but not for the low impact route. The probability of belonging to the task non-attendance class was 17.3%. When the results of the two- and three-class models are compared, the general direction of preferences remain the same, albeit with wider confidence intervals for some attributes in the three-class model (Fig. 5 and ESM Table S7).
3.9 Willingness to Accept Compensation
The WTA estimates derived from the latent class model for the low impact route class 3 and mixed logit models are presented in Fig. 6 and ESM Fig. S1. All attributes except for decision time of 3 years were statistically significant. Positive WTA was found for the attribute level changes of receiving an apology, investigating, and preventing or not preventing, while negative WTA values were found for holding those responsible to account, if there is a high chance of receiving compensation; if the process is easy and straightforward; if they do not know how likely they are to get compensation; if the time to receive a decision is 1 year; and if they used the government compensation scheme. WTA values from the LCA and mixed logit models are similar and not significantly different.
3.10 External Validity
Table 6 presents the results of the external validity analyses. For the low impact route, the model correctly predicted the actual decision to claim of 63.10% of respondents under the pessimistic assumptions (claims process is cumbersome and lengthy) and 36.90% of respondents under the optimistic assumptions (claims process is streamlined and patient-centric). For the severe impact route, the model correctly predicted the actual decision of 58.67% of respondents under the pessimistic assumptions and 41.33% of respondents under the optimistic assumptions. In general, the model predictions were more accurate when pessimistic assumptions (claims process is cumbersome and lengthy) were made about the missing attribute data.
4 Discussion
This paper has presented the results from an online DCE survey that elicited stated preferences from 1029 people in the UK with experience of a PSI to indicate the relative importance of different factors on the choice to make a claim for compensation. For both the low and severe impact routes, the probability of choosing to make a claim is significantly reduced by receiving an appropriate apology and explanation, having an investigation carried out and being satisfied that appropriate measures were taken to prevent this type of PSI from happening again. The probability of making a claim is significantly increased if there is a high chance of receiving compensation, and if the process is easy and straightforward. Respondents are more likely to claim under the government compensation scheme compared with the legal route, while participants are more likely to claim if the time to receive a decision is the lowest, i.e. 1 year for PSI with a low impact and 3 or 6 years for PSI with a severe impact. In the low and severe impact routes, the likelihood of making a claim increases if the compensation amount is larger. The likelihood of claiming increased even if respondents did not know how likely they are to get compensation. We think this is because of optimism bias and because the base level is ‘low chance’ of compensation.
The results of the current research and the previous study eliciting preferences of the general population around the factors to choose whether to make a financial claim against the health service as a result of a PSI [3] are broadly similar. In both studies, receiving an appropriate apology and explanation, and having an investigation carried out and being satisfied appropriate measures were taken to prevent this type of PSI from happening again, significantly reduced the probability of choosing to make a claim, whereas having a claims process that was easy and straightforward, and if there was a high chance of compensation significantly increased the probability of choosing to make a claim. It is reassuring that the findings from both surveys are consistent, which provides more confidence in their use to inform policy.
These DCE results imply that the actions taken by the health service in the aftermath of a PSI, and people’s attitudes about making a claim, have the ability to influence whether a claim is made or not. Specifically, the scenario analysis clearly shows the importance of the health service apology to the patient and carrying out a satisfactory investigation. However, the exact numbers from the scenario analyses should be treated with caution since these are estimates based on stated preferences to a hypothetical survey. The numbers should not be taken at face value but rather should be interpreted as indicative of the extent to which probabilities increase or decrease for different hypothetical cases in comparison with the base case.
Latent class models assessing preference heterogeneity identified groups of participants with distinct preference for their willingness to make a claim for compensation. In the low impact route, men are more likely to make a claim and those who have already made a claim are also more likely to claim. In the severe impact route, respondent characteristics did not significantly predict class membership. Even though we identified two classes, i.e. a pro-compensation class and a compensation-averse class, we are unable to predict the type of respondents who are likely to belong to these classes. This poses a substantial obstacle for policymakers, as they cannot effectively target policy interventions without understanding the characteristics of each group.
The percentage of people who stated that they have already made a claim in this survey is 22% and another 16% are yet to make a claim. These figures are higher compared with the percentage of claimants observed in previous surveys. Gray et al. analysed data from two UK general population surveys in 2001 (n = 8202) and 2013 (n = 19,746) and found that the proportion who pursued a legal claim for compensation was 10.5% and 11%, respectively [6]. The reasons for this difference could be because the study by Gray et al. was conducted almost a decade ago, therefore perhaps trends in making a claim have increased over the years, or because people who have claimed are self-selecting to complete the DCE as they wanted a platform to describe their experience of the PSI. Exploratory analyses also revealed that people who have made a claim or are yet to make a claim in real life were also more likely to claim in the DCE compared with those who have not made a claim. This is not surprising as they have given more thought to the issue of making a claim for financial compensation.
The strengths of this study include eliciting preferences from a sample who has experienced a PSI, as well as rigorous pretesting, pilot testing, and conducting internal and external validity checks. Since making a claim for compensation is not an activity that members of the general public are routinely used to doing, this study adds to the literature by assessing the preferences of those with lived experience. Respondents answered the DCE tasks based on their own experience of harm or that of an immediate family member. During pretesting, participants were keen on framing the DCE context around the participant’s own experience of unintended harm. We had to explain to participants that while the PSI they were thinking about was their own, the factors that were presented to them in the DCE questions were not reflective of reality but were hypothetical. To ensure that participants understood the tasks, we produced an instructional video. We used free text in the pilot survey where participants provided a brief justification for their decision to claim or not. Analysis of these justifications and data from an additional free-text box in the main DCE provided strong indications that participants understood the tasks. Nevertheless, robustness analyses (LCA with task non-attendance) showed that a small group of participants were more likely to opt in to seek compensation regardless of the DCE scenarios presented, due to a belief that they were owed compensation for their own real-life experiences. This bias is analogous to the pro-treatment bias observed in the DCE literature [18].
Study limitations include participants self-selecting as having experienced harm (to themselves or to their immediate family). We could not objectively verify whether the respondents fully met the inclusion criteria. While care was taken to provide definitions of harm to screen participants to ensure those participating were indeed those who had experienced harm, there is always a possibility that some may not be providing accurate responses to the screening question. Given this mode of recruitment and the difficulty of recruiting this niche sample, it was not possible to have quotas to ensure an equal representation of the severity of PSIs experienced. However, we managed to recruit 346 participants to the PSI in the severe impact route, which was an adequate size to estimate the regression models. We intended to assess data quality of the online sample by comparing the responses of those recruited from a specialised charity, however due to low recruitment from the charity, despite our best efforts, this was not possible. Moreover, the majority of participants in this sample were employed, educated and under the age of 40 years, which may not be reflective of the whole sample of people who have experienced a PSI. Ideally, we would have liked to have recruited to quotas to obtain a more balanced sample, however due to the difficulty in recruiting these patients, quota restrictions were not imposed. The recruitment of the sample using an existing online panel during the coronavirus disease 2019 (COVID-19) pandemic, which faces the criticism that the sample would not include the computer illiterate or those without internet access, facilitated the inclusion of participants who were shielding due to COVID-19, a group that would have been missed using other modes of administration. Furthermore, the attributes included in this DCE came from a previously conducted general population DCE survey, based on a literature review containing recent qualitative studies assessing the reason why patients decided to make a claim for clinical negligence. Redeveloping the attributes with input from those directly affected by PSIs could potentially yield a slightly modified set of attributes. Moreover, the survey does not include reference to eligibility to make a claim, yet, in practice, the claimant does not determine their own eligibility. Therefore, although the participant may express that they would choose to make a claim for compensation, this does not mean that this would result in a claim being made since they may not be eligible to do so. Finally, results of the external validity should be interpreted with caution as the predictive accuracy is heavily contingent on the assumptions we made. Previous studies have used methods such as correcting the scale or correcting the market shares to adjust for hypothetical bias [19], but since we did not have a full set of revealed preference data, further analyses were not explored. Future research priorities could include collecting more complete data on revealed preferences to confirm the external validity of the developed models.
This study identified the preferences of people who have experienced a PSI to make a financial claim for compensation. The results of the DCE provide a robust understanding on the motivations to seek financial compensation. These findings could be used by decision makers to inform broader policy decisions, including changes to the existing systems in place to improve patient experience after a PSI.
References
NHS Resolution: annual report and accounts 2020/21. 2021. https://resolution.nhs.uk/wp-content/uploads/2021/07/Annual-report-and-accounts-2020-2021-WEB-1.pdf. Accessed 13 Jan 2022.
Behavioural Insights Team: Behavioural insights into patient motivation to make a claim for clinical negligence. Final report by the Behavioural Insights Team on behalf of NHS Resolution. 2018. https://resolution.nhs.uk/wp-content/uploads/2018/10/Behavioural-insights-into-patient-motivation-to-make-a-claim-for-clinical-negligence.pdf. Accessed 13 Jan 2022.
Rowen D, Wickramasekera T, Hole A, Keetharuth A, Wailoo A. A DCE to elicit general population preferences around the factors influencing the choice to make clinical negligence claims. Value Health. 2022;25:1404–15.
Donaldson L. Making amends: a consultation paper setting out proposals for reforming the approach to clinical negligence in the NHS: a report by the Chief Medical Officer. London: Department for Health; 2003.
Fenn P, Gray A, Rickman N, Vencappa V. Funding clinical negligence cases; access to justice at reasonable cost. London: Nuffield Foundation; 2016.
Gray AM, Fenn P, Rickman N, Vencappa D. Changing experience of adverse medical events in the National Health Service: comparison of two population surveys in 2001 and 2013. Soc Sci Med. 2017;195:83–9.
Huycke LI, Huycke MM. Characteristics of potential plaintiffs in malpractice litigation. Ann Intern Med. 1994;120:792–8.
National Audit Office: managing the costs of clinical negligence in trusts. 2017. https://www.nao.org.uk/wp-content/uploads/2017/09/Managing-the-costs-of-clinical-negligence-in-trusts.pdf. Accessed 1 Apr 2022.
NHS Improvement: NRLS national patient safety incident reports: Commentary. 2018. https://improvement.nhs.uk/documents/2543/NAPSIR_commentary_FINAL_data_to_December_2017.pdf. Accessed 1 Apr 2022
Vincent C, Phillips A, Young M. Why do people sue doctors? A study of patients and relatives taking legal action. Lancet. 1994;343:1609–13.
Hole AR. DCREATE: Stata module to create efficient designs for discrete choice experiments. London: Statistical Software Components; 2017.
Curtice J, Clery E, Perry J, Phillips M, Rahim N (eds). British Social Attitudes: the 36th report. London: The National Centre for Social Research; 2019. https://www.bsa.natcen.ac.uk/media/39363/bsa_36.pdf. Accessed 17 Nov 2021.
Yoo HI. lclogit2: an enhanced command to fit latent class conditional logit models. Stand Genom Sci. 2020;20:405–25.
Hole AR. Fitting mixed logit models by using maximum simulated likelihood. Stand Genom Sci. 2007;7:388–401.
Hopson E, Wilkinson C. Comparison of furloughed jobs data, UK: March 2020 to January 2022. London: Office for National Statistics; 2021.
Veldwijk J, Marceta SM, Swait JD, Lipman SA, de Bekker-Grob EW. Taking the shortcut: simplifying heuristics in discrete choice experiments. Patient-Patient-Centered Outcomes Res. 2023;16:301–15.
Jonker MF. The garbage class mixed logit model: accounting for low-quality response patterns in discrete choice experiments. Value Health. 2022;25:1871–7.
Johnson FR, DiSantostefano RL, Yang JC, Reed SD, Streffer J, Levitan B. Something is better than nothing: the value of active intervention in stated preferences for treatments to delay onset of Alzheimer’s disease symptoms. Value Health. 2019;22(9):1063–9.
Buckell J, Hess S. Stubbing out hypothetical bias: improving tobacco market predictions by combining stated and revealed preference data. J Health Econ. 2019;65:93–102.
Acknowledgements
Our thanks are extended to all participants in the study. The authors would like to thank Action against Medical Accidents (AvMA) for their collaboration, and Donna Davis for providing administrative support with the project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Financial support for this project was provided by the Department of Health and Social Care (2020/S 123-302675 C0759). The views expressed are those of the authors and not necessarily those of the NHS, the National Institute for Health Research, the Department of Health and Social Care or its arm's length bodies, or other UK government departments. Any errors are the responsibility of the authors.
Conflicts of Interest
Nyantara Wickramasekera, Arne Risa Hole, Donna Rowen, Allan Wailoo, and Anju D. Keetharuth have no conflicts of interest to declare.
Availability of Data and Material
Data are available upon request to the corresponding author.
Ethics
This study has been approved by the University of Sheffield Research Ethics Committee via the Sheffield Centre for Health and Related Research (Ref: 038113).
Informed Consent
Informed consent was obtained from all participants in this study.
Authors’ Contributions
This study was conceived and designed by AK, AW, ARH, DR and NW. AK, NW, and DR were involved in data collection. Data analyses were performed by NW, ARH and AK. The manuscript was drafted by AK and NW, and all authors contributed to subsequent versions, and read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wickramasekera, N., Hole, A.R., Rowen, D. et al. Exploring the Factors that Drive Clinical Negligence Claims: Stated Preferences of Those Who Have Experienced Unintended Harm. Patient 17, 301–317 (2024). https://doi.org/10.1007/s40271-024-00674-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-024-00674-x