Abstract
Background
Treatment options for patients with metastatic hormone-sensitive prostate cancer (mHSPC) have broadened, and treatment decisions can have a long-lasting impact on patients' quality of life. Data on patient preferences can improve therapeutic decision-making by helping physicians suggest treatments that align with patients' values and needs.
Objective
This study aims to quantify patient preferences for attributes of chemohormonal therapies among patients with mHSPC in the USA, Canada, and the UK.
Methods
A discrete-choice experiment survey instrument was developed and administered to patients with high- and very-high-risk localized prostate cancer and mHSPC. Patients chose between baseline androgen-deprivation therapy (ADT) alone and experimentally designed, hypothetical treatment alternatives representing chemohormonal therapies. Choices were analyzed using logit models to derive the relative importance of attributes for each country and to evaluate differences and similarities among patients across countries.
Results
A total of 550 respondents completed the survey (USA, 200; Canada, 200; UK, 150); the mean age of respondents was 64.3 years. Treatment choices revealed that patients were most concerned with treatment efficacy. However, treatment-related convenience factors, such as route of drug administration and frequency of monitoring visits, were as important as some treatment-related side effects, such as skin rash, nausea, and fatigue. Patient preferences across countries were similar, although patients in Canada appeared to be more affected by concomitant steroid use.
Conclusion
Patients with mHSPC believe the use of ADT alone is insufficient when more effective treatments are available. Efficacy is the most significant driver of patient choices. Treatment-related convenience factors can be as important as safety concerns for patients.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Preferences of patients with prostate cancer were derived from choices between experimentally designed treatment alternatives. |
Patients preferred treatment options with the highest efficacy and ones without risks of serious infections. |
Patients valued treatment convenience as much as treatment-related side effects. |
1 Introduction
Prostate cancer (PC) is the second most commonly diagnosed cancer in men in the USA, with an estimated 288,300 new cases, and 34,700 deaths in 2023 [1]. Prostate-specific antigen (PSA) testing and digital rectal examination enable early diagnosis of the disease and, in up to 80% of patients, PC is diagnosed in localized stages that are characterized by slow progression and no symptoms, while, in 6–8% of patients, it is diagnosed directly in the metastatic stage. Approximately 20% of patients with localized disease go on to develop metastatic hormone-sensitive prostate cancer (mHSPC) within 5 years [2, 3]. Thus, a meaningful minority of patients with PC are expected to develop advanced disease. Further, patients with high-risk localized prostate cancer (HRLPC) show an extracapsular extension of the prostate, with grade group 4 or 5, or PSA level > 20 ng/ml. In contrast, in patients with very-high-risk localized PC, the tumor spreads to the seminal vesicles, with Gleason pattern 5 tissue biopsy and > 4 biopsy cores have grade group 4 or 5 [4]. These patients are at an increased risk of having the tumor spread beyond the prostate and of having a more aggressive form of the disease.
International guidelines detail various treatment options for patients with PC [4,5,6]. Patients with HRLPC are treated with external beam radiation therapy and long-term androgen-deprivation therapy (ADT) for 18–36 months [7]. The current standard of care for patients with mHSPC includes ADT in combination with one of the novel hormonal therapies (i.e, abiraterone acetate with prednisone, apalutamide, enzalutamide, or darolutamide) or in combination with docetaxel or prostate radiotherapy [4]. While these therapies offer similar survival benefits, their adverse-effect profiles vary. Due to the similarity of outcomes and a lack of comparative data, guidelines offer similar levels of support for these various regimens [8]. Clinical equipoise among treatment options implies that treatment decisions are sensitive to patients’ relative preferences for expected adverse effects and administration requirements [9, 10]. The required long-term treatment commitments also imply that failing to account for patient preferences can result in an accumulation of quality-of-life (QoL) impacts over time, both functionally and psychologically [11].
Shared decision-making has emerged as a model that involves patients in the clinical decision-making process[12]. Evidence shows that shared decision-making leads to better-informed patients, decreased decisional conflicts between patients and physicians, and minimal posttreatment decisional regret by patients [10, 11, 13]. While shared decision-making is an individual endeavor, the assessment of preferences at a population level can produce evidence that supports the use of shared decision-making in specific treatment decisions[14]. For example, quantitative measures of population-level patient preferences can provide useful benchmarks for treatment discussions between physicians and patients.
Population-level preference measures can be obtained using stated-preference methods, such as discrete-choice experiments (DCEs) [15, 16]. DCE surveys have been increasingly used by regulatory agencies and policymakers for decision-making [17, 18], and they have been used in the past to evaluate the preferences of patients with PC. Previous DCEs in PC mainly focused on efficacy [19, 20], safety concerns [21,22,23,24], and convenience factors [25, 26] in castration-resistant prostate cancer (CRPC) [26, 27]. However, there are limited DCE data on the preferences of patients with mHSPC [25]. While we can expect that patients with mHSPC would care about treatment efficacy and safety, the role of convenience factors (administration factors [route, frequency, and setting], concomitant use of steroids, and monitoring requirements) on treatment preferences among patients with mHSPC is unclear, given the long-term use of some relevant therapies.
Our study sought to understand patient perspectives on the relative importance of adverse effects and process factors associated with treatments for HRLPC and mHSPC across three English-speaking countries: the USA, the UK, and Canada. These countries share a similar cultural background but have profoundly different healthcare systems and socioeconomic support for patients. We aimed to understand how patients in these countries choose to balance treatment benefits, risks, and their need for treatment convenience, to help inform recommendations for PC treatments. While we wanted to assess the preferences of patients in each of these countries, we also wanted to evaluate the degree to which patients in these countries exhibited unique preference patterns and what patient characteristics allowed us to consider them part of a common model of preferences.
2 Methods
2.1 Survey Development
We developed a DCE survey following good-practice guidance [28]. In this DCE survey, respondents were asked to select their most preferred option from a series of three experimentally controlled treatment alternatives. Each alternative was defined by a hypothetical treatment profile constructed from a fixed set of treatment characteristics known as attributes. Each attribute consisted of several clinically plausible treatment outcomes known as attribute levels. The survey used three broad categories of attributes: efficacy, tolerability, and convenience. The efficacy category included 5-year overall survival (OS). The tolerability category included attributes such as fatigue, skin rash, neurotoxicity, and common chemotherapy-related toxicities. The convenience category included attributes such as administration factors (route, frequency, and setting), concomitant use of steroids, and monitoring requirements. Study attributes and their levels were selected based on information from a targeted literature review, early interviews with patients about their concerns with treatment, and consultations from clinical experts. Feedback from five patients in the USA was collected via virtual interviews to determine their priorities regarding treatment and to help finalize the selection of attributes and their levels. Final study attributes and levels are presented in Table 1. Patient-appropriate language was used to assist respondents in understanding attribute descriptions and questions asked in the survey.
Following attribute selection, a draft survey instrument was developed and tested in one-on-one pretest interviews with 21 patients from the USA. During these interviews, the study team corroborated that the attribute definitions were clear, that the included attributes covered the relevant aspects in treatment decisions, and that the levels were salient enough to induce trade-offs. The DCE survey was updated and finalized based on the feedback from the pretest interviews. The final survey for the USA was adapted for patients in Canada and the UK. Adaptations included treatment regimens as per the local regulatory agencies, and clarification was provided for treatment descriptions that were not consistent with a country-specific standard of care. Five pretest interviews were conducted in Canada and in the UK each to reaffirm that survey adaptations were relevant to each specific country. The survey instruments then were updated and finalized based on the feedback from the pretest interviews. In addition, the survey was developed under the active guidance of a steering committee comprised of international experts and practicing physicians (AKM, SJH, BFT, CDS, and DJG were part of the steering committee).
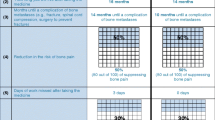
To accommodate such a large number of attributes, two DCE modules were constructed. Module 1 examined the trade-offs between efficacy and tolerability, and module 2 examined the trade-offs between efficacy and convenience. With the two modules, we were able to reduce the number of attributes that patients were asked to consider simultaneously but still collect enough information to estimate preferences for all attributes together. This approach can be seen as an extension of the use of overlaps in choice questions, where we systematically “overlapped” (or eliminated from the choice question) process attributes in some questions and later did the same with outcomes. Evidence for the impact of attribute overlap on cognitive burden and measurement improvements offered a strong basis for the approach [29]. In addition, pretest interviews confirmed that including more questions with fewer attributes was a viable option for respondents. Example DCE questions from each module are shown in Fig. 1a and b. Of the three treatment choices, “ADT alone” represents a baseline choice for patients, and the other choices show the treatment profiles of additional medications.
a An example of questions from module 1 showing a triplet of treatment profiles comprising attributes with a specific outcome level pertaining to treatment efficacy and risks. b An example of questions from module 2 showing a triplet of treatment profiles comprising attributes with a specific outcome level pertaining to treatment efficacy and convenience factors. ADT, androgen-deprivation therapy; IV, intravenous
2.2 Experimental Design
DCEs require constructing multiple versions of choice questions. To populate the survey, the experimental design determines the combinations of attribute levels for each hypothetical treatment profile. The smallest feasible experimental design requires as many questions as preference parameters to be estimated. To ensure statistical efficiency in the experimental design, a fractional–factorial design was prepared to identify patient preferences for each study attribute level independently [30]. Two statistically efficient experimental designs were developed with a minimum number of questions necessary to generate preference weights for each attribute level in the study. For module 1, an experimental design with 36 questions was generated and grouped into six blocks of six questions each. For module 2, another experimental design with 36 questions was developed and grouped into nine blocks of four questions each. The designs for both modules were prepared using the SAS 9.4 system (SAS Institute Inc, Cary, NC, USA) to maximize statistical efficiency (D-optimality), in accordance with the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) guidance on good practice for constructing experimental designs of DCEs [16]. The option for ADT alone was fixed in all questions to include a 30% chance of 5-year OS and no additional safety issues in module 1. In module 2, ADT alone always included injections every 3 weeks, no concomitant steroid use, and four monitoring visits per year.
Each respondent was randomly assigned to one unique block from module 1 and two nonrepetitive blocks from module 2. Respondents first answered 12 questions: six questions from module 1, four questions from the first assigned module 2 block, and two questions from the second assigned module 2 block. Respondents were then asked if they were willing to answer two more questions (i.e., the remaining two questions from the second assigned module 2 block). Thus, each respondent answered up to 14 questions from both modules. The number of questions survey respondents would be able to answer comfortably was determined using feedback from patient pretest interviews. In addition to the DCE modules, the survey also included reading materials and background questions. The survey was expected to take 20–30 minutes to complete.
Data quality checks included performance on comprehension questions that were built into the survey. These comprehension questions helped identify respondents who did not completely understand the study attributes or question format. Additionally, respondents who completed the survey in less than 5 minutes were excluded from the final study sample as this was considered a strong indication of inattentiveness to the survey. Further, straight-line responders (those who always chose ADT and Medicine A or ADT and Medicine B) were eliminated from the final sample as the questions were designed to avoid this pattern. However, respondents who always chose ADT alone were left in the sample, as that option was fixed and not experimentally designed, raising the possibility that patients indeed preferred that option consistently.
The study was conducted in accordance with the protocol, applicable International Council for Harmonization of technical requirements for pharmaceuticals for human use (ICH) guidelines for Good Clinical Practice, and ISPOR guidance on the design of DCEs [28, 30, 31]. It followed applicable regulations and guidelines governing clinical study conduct and ethics principles as per the Declaration of Helsinki [32]. It was reviewed and approved by the Duke University Health System Institutional Review Board (Pro 00106523). Individual patient medical information and sensitive personal information obtained as a result of this study were kept confidential, and data related to patient identification numbers and/or initials, when used, were anonymized. Informed consent was obtained and documented from all respondents in the DCE survey.
2.3 Study Population
In the USA and Canada, patients willing to participate in the DCE survey were identified by a treating physician and contacted by the study team to evaluate their eligibility. In the UK, patient associations, advocacy groups, and social media networks dedicated to prostate cancer were leveraged to bring awareness about the ongoing survey, and patients were invited to participate. There were no advertisements in the National Health Service or on any public notice boards for patient recruitment. Patients willing to participate in the survey contacted the study team via phone or email. They underwent a screening process by phone to ascertain their eligibility to participate in the survey. Adult males with a diagnosis of mHSPC or HRLPC, with or without previous experience with ADT, and who were able to read and understand English and provide informed consent were invited to participate in the survey via email. To determine the necessary sample sizes for country-level preference models, we considered several factors, including the number of DCE questions, largest number of levels for any attributes, number of attributes, number of treatment alternatives, inclusion of the status quo (ADT alone), and number of probabilistic attributes [33, 34].
2.4 Study Outcomes
The key outcomes of the survey included: (1) patient preference weights and international variations, (2) the relative importance weights of aspects related to combination therapies and international variations, and (3) the preference weights for patients who share similar characteristics/concerns across the study countries.
2.5 Statistical Analysis
The statistical analysis of patient choices provided a measure for the effects of changes in the attribute levels on the likelihood that treatments would be selected by respondents. The resulting log-odds parameters are interpreted as attribute-level relative preference weights [35]. Respondent choices were examined for data quality through comprehension questions, time spent on the survey, and internal consistency checks. Data were analyzed using a scale-adjusted (by question module) random-parameters logit (RPL) model [36] for each country. In addition, a latent-class/random-parameters logit (LCRPL) model was used to evaluate the influence of task nonattendance on preference weights. This model assumed that samples in each country included a group of respondents who were not attentive and for whom preference weights for all attributes were zero [37]. The latent-class portion of the LCRPL model used patients’ response patterns to assign them probabilistically to this nonattendant class. At the same time, the LCRPL model used this probability to down-weight respondents who were more likely to be exhibiting this pattern of choices [38]. The relative importance of attributes was calculated from the country-specific results to evaluate the overall impact of each attribute (independent variable) on respondent choices (dependent variable). The relative-importance measures were normalized to facilitate comparisons across countries using profile-based normalization [15].
Differences in preferences between respondents with mHSPC and HRLPC in each country were directly evaluated using a scaled-controlled RPL model by country. A broader evaluation of preference heterogeneity was conducted by pooling responses from all countries in a LCRPL model. The model included five classes. One of these classes (class 1) estimated a single density for the distribution of preferences across all respondents. In other words, this class was set up to estimate both mean preferences and their standard deviations—as an RPL would—for the full sample. A second class (class 2) controlled for task nonattendance across all respondents as described above. These two classes together provide a mixture of densities with best possible characterization of preferences across countries given the assumptions in the model. The remaining classes (3–5) included estimates that were only attributable to one of the three countries in the study and were meant to capture country-specific effects that were not appropriately captured by the overall distribution of preferences in class 1 and class 2 [38]. Testing the significance of membership probabilities to classes 3–5 identified the countries that had a significant group of respondents who could not be pooled in an overall preference model. Class-assignment probabilities in the LCRPL model were correlated with respondent-specific covariates.
To facilitate comparisons across attribute levels, preference weights for levels associated with the “ADT alone” treatment option were set to zero. A positive preference weight implies a greater preference for the attribute level over the corresponding “ADT alone” attribute level, and a negative preference weight implies a greater preference for “ADT alone” over the attribute level. Importance weights represent the greatest difference in preference weights observed between the levels of an attribute and describe the importance that patients assign to a particular attribute. Relative importance weights were normalized to add up to 1 to facilitate comparisons across attributes and countries. Data analysis was conducted using Stata 16 (Stata Corp LLC, College Station, TX, USA) and Latent GOLD 5.1 (Statistical Innovations, Arlington, MA, USA).
3 Results
Surveys were administered in the USA between 7 September and 4 December 2021; in Canada between 15 November and 5 April 2022; and in the UK between 18 January and 6 May 2022. Not all of the enrolled patients completed the survey; rejection rates among patient respondents were 7% in the USA, 9% in Canada, and 4% in the UK. A total of 550 patients with PC across the USA (n = 200), Canada (n = 200), and the UK (n = 150) completed the survey. One patient from the UK sample was removed from the DCE analyses due to response nonvariation. Patient demographics and clinical characteristics of survey respondents are presented in Tables 2 and 3, respectively. Respondents took a median time of 23.1 minutes (IQR, 16.8–29.7 minutes) to complete the survey. Overall, the population responding to the survey was racially and ethnically diverse, with a mean age of 64.3 years (standard deviation, 10.4 years). Sixty-nine percent were married, and a majority of respondents across all three countries were retired (47.5%). The average time since diagnosis of PC ranged from 5.8 to 7.4 years across the three countries. While the majority of respondents across the USA and UK (70% and 64%, respectively) had prior exposure to steroid treatment for PC, most respondents from Canada (67.5%) did not. A decrease in in-person visits to treat cancer was reported by 38.5% of respondents, and 52.4% of respondents reported an increase in their use of telehealth due to the COVID-19 pandemic (Table 3). No significant inconsistencies between the respondent characteristics and the known epidemiology of the disease were noted.
3.1 Preference Weights and International Variations for Specific Combination Therapies
In all countries, respondents showed strong significant preferences for treatments with higher efficacy. After considering treatment outcomes in module 1, patients in the USA, Canada, and the UK opted for a combination therapy 77%, 75%, and 80% of the time, respectively. In module 2, patients in the USA, Canada, and the UK opted for a combination therapy 87%, 87%, and 89% of the time, respectively. Treatments with additional side effects, risks, and inconvenience factors were associated with negative preference weights, indicating that, all else being equal, patients were less likely to choose treatments with worse side effects and more inconvenience than ADT alone. Patients in the USA showed a larger preference weight for efficacy compared with tolerability or convenience (Fig. 2a). Preference weights for convenience attributes were comparable with preference weights for tolerability attributes, suggesting that a patient’s choices about treatment convenience are akin to their choices about treatment tolerability. Preference patterns for patients in Canada (Fig. 2b) and the UK (Fig. 2c) were similar to those in the USA. Five-year OS also had the greatest influence on patients’ choices in these two countries. Similarly, patients in all three countries showed a strong preference to avoid the treatment-related risk of serious infections. Unlike patients in the USA, patients in Canada had no significantly negative preferences for nausea; weakness, tingling, and pain; or administration factors (route, frequency, and setting). Data also suggested that there may be no difference between convenience and tolerability (nausea, weakness, tingling, and pain) attributes for patients in Canada. In the UK, respondents had no specific preference for oral administration, but they least preferred an intravenous (IV) route of administration. In all three countries, the impact of efficacy (OS), even at the lowest level presented (40% survival chance), exceeded that of most other attributes or levels.
3.2 Relative Importance of Attributes of Combination Therapies that can Influence Patients’ Treatment Choices
Efficacy was the most important attribute for patients in the USA (36%), Canada (27%), and the UK (39%), followed by chemotherapy-related problems, steroid use, and treatment convenience attributes (Fig. 3). For patients in the USA and UK, efficacy was greater than 100% more important relative to chemotherapy-related problems, whereas for patients in Canada, efficacy was only approximately 50% more important than chemotherapy-related problems. The need for steroid use was more important for patients in Canada (19%) than for patients in the USA (13%) and the UK (10%). Route of administration was less important for patients in Canada (2%) compared with patients in the USA (10%) and the UK (9%). Factors associated with treatment convenience, such as route, duration, and location of administration, as well as frequency of monitoring visits, were generally as important to survey respondents as tolerability issues such as skin rash, tiredness, and problems with the nervous system.
3.3 Understanding Variations in Patient Preferences Among Survey Respondents from All Three Countries
Results from the five-class LCRPL showed that preferences for most (59.9%) respondents across the USA, Canada, and the UK were adequately characterized by the preference estimates derived for class 1 (Table 4). Sixteen percent of all respondents were considered to be nonattendant (class 2). Finally, 17% of respondents in the US (6.3% of the overall sample) and the UK (4.6% of the overall sample) were considered to have preferences that differed from the general preferences captured in class 1. That percentage was much higher for Canadian respondents (35.6%, or 13.0% of the overall sample), suggesting that Canadian respondents were less like their US and UK counterparts.
The preference patterns of patients in the pooled class (Fig. 4) were similar to the RPL model for individual countries observed in Fig. 2a–c. The pooled class shares similar preference patterns, with higher preference for efficacy relative to side effects. Similar patient preferences were noted for treatment-related side effects and treatment-related convenience factors.
The impact of covariates on class membership was examined to characterize which patients were more likely to be in the task nonattendant class relative to the pooled class (Table 5). These results are presented as odds ratios, where >1 indicates a greater probability of being in the task nonattendance class and <1 indicated a greater probability of being in the class with poolable preferences. Respondent characteristics, such as age 70 years or above, having undergone hormone or ADT therapy, PC diagnosis within the past 2 years, cessation of treatment in the past, having HRLPC, and self-reported limiting fatigue currently, were significantly associated with membership to the pooled-preference class. By contrast, being employed, failing survey comprehension questions, and prior exposure to steroid treatment for PC were associated with the task nonattendance class.
4 Discussion
This is the first DCE study to elicit patient preferences for treatments of mHSPC and HRLPC across three English-speaking countries, implemented during the COVID-19 pandemic. The USA, Canada, and the UK share a cultural history but differ in terms of healthcare systems and the socioeconomic support that patients receive. Therefore, it is interesting to observe how patients’ perspectives and preferences vary among these three countries. Furthermore, unlike cross-country comparisons available in the literature [22, 23, 25] that aim to demonstrate differences, our study focused on identifying both similarities and differences in patient treatment choices in these countries. In the USA, Canada, and the UK, patients showed the highest preference for treatment efficacy, followed by a strong preference to avoid treatment-related risk of serious infections. Our results imply that patients consider the use of ADT alone inadequate, given the availability of combination therapies that can improve efficacy. The study also observed that treatment-related convenience factors, such as route of drug administration and frequency of monitoring visits, were as important as some treatment-related side effects, such as skin rash, nausea, and fatigue. This study also highlights the relative importance patients in Canada place on concomitant steroid use. The study data provide information related to treatment-emergent adverse events and patient perspectives, supporting patients and physicians in having a conversation about treatment attributes that matter most to them. Importantly, no specific treatment responses or side effects are discussed; instead, a wide array of adverse events that patients may experience are presented in comparison with ADT, thus providing an opportunity for patients and physicians to understand and prioritize treatment choices.
Treatment effectiveness emerged as the most important attribute in a similar DCE study conducted in patients with mHSPC from Spain, Germany, and the UK [25]. It is reasonable to expect patient preferences along similar lines in non-English speaking countries. Another study of patients with metastatic CRPC reported the highest preference for treatments associated with better control of pain [23]. A more recent study with patients with metastatic CRPC in the USA found that OS was about 3 times as important as worsening of fatigue and ~2 times more important as nausea [26]. Yet, this study also found that administration factors were relatively unimportant compared with treatment side effects. That said, the study only included frequency and route of administration, which were also found to be relatively unimportant in our application.
The robust response to factors other than outcomes in our study suggests that information about treatment attributes pertaining to health-related quality of life (HRQoL) could be of great value for patients and physicians when making treatment decisions. The variation we observed in the relative importance of convenience factors highlights potential difficulties with aligning these treatment attributes with patient preferences. Nevertheless, our results suggest that not addressing such factors could have a significant impact on the patient’s well-being. More research into eliciting patient choices will help provide physicians with evidence on patients’ beliefs and preferences that can help inform treatment decisions.
Our study also shows that some patient concerns are largely consistent across the countries studied. We find that the vast majority of respondents in these three countries had concerns that could be adequately characterized with a single model of preferences. In our study, patients who could not provide meaningful responses were identified as those who could not comprehend the survey questions. This is a relevant finding and highlights the importance of effective communication between patients and physicians when evaluating treatment options for mHSPC or HRLPC.
We found no evidence suggesting that patients with mHSPC or HRLPC have meaningful differences in preferences (data not shown). This is not surprising, as both patient groups face similar consequences of treatment-associated adverse effects, which may have a long-term impact on their well-being and QoL.
Patient preferences may have been influenced by the COVID-19 pandemic. During times of limited access to care (such as during the COVID-19 pandemic), patient preferences are particularly important to consider, with the goal of optimizing patient adherence and treatment outcomes. Physicians had to weigh the benefit of treating patients with mHSPC against the risk of them contracting COVID-19 [39], thereby impacting healthcare delivery and treatment plans [40]. In our study, 12% of survey respondents observed a change in their cancer treatment plans due to the pandemic, and approximately 39% observed a decrease in in-person visits during the pandemic. Moreover, mobility restrictions due to the pandemic will have consequences on choice and accessibility to treatments, and understanding the value patients attribute to treatment convenience factors is important during times when access to care may be limited.
This DCE study has several limitations. The DCE survey elicits patient preferences between hypothetical treatment profiles, which do not carry the same consequences as real-world decisions. That said, an elicitation format was utilized, which closely mimicked real-world decision-making to elicit preference-revealing answers. Also, the importance shown by patients primarily depends on the nature of the attributes and their levels included in the study. In that sense, this study represents a more complete evaluation of patient preferences in PC, as a greater number of attributes were considered compared with previous studies. The sample size included for each of the countries may not be sufficient to elicit statistically significant differences between attributes and their levels across countries. Further, the sample of patients surveyed in the study may not be fully representative of patients with mHSPC or HRLPC in each of the countries surveyed. Finally, comparisons between convenience factors and safety concerns were performed indirectly, as no choice question required trade-offs between these factors, other than efficacy. While statistical adjustments were made to allow poolability of the two question modules, it is possible that direct trade-offs between these attribute factors would lead to different relative importance measures. Future work should evaluate this potential issue.
Recent advances suggest the emerging potential of triplet therapy that combines ADT with novel hormonal therapies and docetaxel for patients with mHSPC. In the PEACE-1 trial, patients with mHSPC who received a combination of abiraterone, ADT, and docetaxel showed an improvement in OS and radiographic progression-free survival compared with those who received ADT and docetaxel therapy [41]. Likewise, the ARASENS trial also showed an improvement in OS with a combination of darolutamide, ADT, and docetaxel compared with placebo plus ADT and docetaxel in patients with mHSPC [42]. The standard of care for patients with mHSPC may evolve along with these new combination therapies in the future, although more studies will need to replicate this benefit. Nevertheless, patient preferences are being increasingly used in regulatory decision-making [17, 18, 43], and in the future, DCE data on treatment preferences (efficacy, safety, and convenience) will be pertinent for physicians planning optimal treatment for patients with mHSPC in accordance with their preferences.
5 Conclusions
Our DCE study quantified the treatment attributes of chemohormonal therapies among patients with mHSPC in the USA, Canada, and the UK. Patients believe that given the alternatives that can improve efficacy, the use of ADT alone is not sufficient. Efficacy is the most significant driver of patient choices. Treatment-related convenience factors can be as important as safety concerns for patients.
References
American Cancer Society: Key Statistics for Prostate Cancer. 2023. https://www.cancer.org/cancer/prostate-cancer/about/key-statistics.html#:~:text=About%20288%2C300%20new,from%20prostate%20cancer. Accessed 1 May 2023.
Rebello RJ, Oing C, Knudsen KE, Loeb S, Johnson DC, Reiter RE, et al. Prostate cancer. Nat Rev Dis Primer. 2021;7(1):9. https://doi.org/10.1038/s41572-020-00243-0.
Menges D, Yebyo HG, Sivec-Muniz S, Haile SR, Barbier MC, Tomonaga Y, et al. Treatments for metastatic hormone-sensitive prostate cancer: systematic review, network meta-analysis, and benefit-harm assessment. Eur Urol Oncol. 2022;5(6):605–16. https://doi.org/10.1016/j.euo.2022.04.007.
National Comprehensive Cancer Network: Prostate Cancer (version1.2023). 2023. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1459. Accessed 5 Apr 2023.
National Institute for Health and Care Excellence (NICE): prostate cancer: diagnosis and management. 2019. https://www.nice.org.uk/guidance/ng131/resources/prostate-cancer-diagnosis-and-management-pdf-66141714312133. Accessed 5 Sep 2022.
Mottet N, van den Bergh RCN, Briers E, Coalition/Europa UOMO), Gillessen S, Grummet F, van der Kwast TH, Lam TB, Mason MB, Oprea-Lager DE, Ploussard G, van der Poel HG, Schoots IG,Tilki D, Wiegel T et al. EAU—EANM—ESTRO—ESUR—ISUP—SIOG guidelines on prostate cancer. 2022. https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-EANM-ESTRO-ESUR-ISUP_SIOG-Guidelines-on-Prostate-Cancer-2022_2022-04-25-063938_yfos.pdf. Accessed 5 Sep 2022.
Khauli R, Ferrigno R, Guimarães G, Bulbulan M, Junior PLSU, Salvajoli B, et al. Treatment of localized and locally advanced, high-risk prostate cancer: a report from the first prostate cancer consensus conference for developing countries. JCO Global Oncol. 2021;7:530–7. https://doi.org/10.1200/go.20.00421.
Ng K, Smith S, Shamash J. Metastatic Hormone-Sensitive Prostate Cancer (mHSPC): advances and treatment strategies in the first-line setting. Oncol Ther. 2020;8(2):209–30. https://doi.org/10.1007/s40487-020-00119-z.
Weiner AB, Nettey OS, Morgans AK. Management of metastatic hormone-sensitive prostate cancer (mHSPC): an evolving treatment paradigm. Curr Treat Opt Oncol. 2019;20(9):69. https://doi.org/10.1007/s11864-019-0668-8.
Johnson DC, Mueller DE, Deal AM, Dunn MW, Smith AB, Woods ME, et al. Integrating patient preference into treatment decisions for men with prostate cancer at the point of care. J Urol. 2016;196(6):1640–4. https://doi.org/10.1016/j.juro.2016.06.082.
Aning JJ, Wassersug RJ, Goldenberg SL. Patient preference and the impact of decision-making aids on prostate cancer treatment choices and post-intervention regret. Curr Oncol. 2012;19(Suppl 3):S37-44. https://doi.org/10.3747/co.19.1287.
Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–7. https://doi.org/10.1007/s11606-012-2077-6.
Greenfield S, Kaplan S, Ware JE. Expanding patient involvement in care. Effects on patient outcomes. Ann Intern Med. 1985;102(4):520–8. https://doi.org/10.7326/0003-4819-102-4-520.
Gonzalez Sepulveda JM, Johnson FR, Reed SD, Muiruri C, Hutyra CA, Mather RC. Patient-preference diagnostics: adapting stated-preference methods to inform effective shared decision making. Med Decis Making. 2023;43(2):214–26. https://doi.org/10.1177/0272989x221115058.
Gonzalez JM. A guide to measuring and interpreting attribute importance. Patient. 2019;12(3):287–95. https://doi.org/10.1007/s40271-019-00360-3.
Reed Johnson F, Lancsar E, Marshall D, Kilambi V, Mühlbacher A, Regier DA, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health. 2013;16(1):3–13. https://doi.org/10.1016/j.jval.2012.08.2223.
US Food & Drug Administration (FDA). Patient preference information—voluntary submission, review in premarket approval applications, humanitarian device exemption applications, and de novo requests, and inclusion in decision summaries and device labeling: guidance for industry, food and drug administration staff, and other stakeholders. 2016. https://www.fda.gov/media/92593/download. Accessed 29 Aug 2022.
Mühlbacher AC, Juhnke C, Beyer AR, Garner S. Patient-focused benefit-risk analysis to inform regulatory decisions: the European Union perspective. Value Health. 2016;19(6):734–40. https://doi.org/10.1016/j.jval.2016.04.006.
Lloyd A, Penson D, Dewilde S, Kleinman L. Eliciting patient preferences for hormonal therapy options in the treatment of metastatic prostate cancer. Prostate Cancer Prostatic Dis. 2008;11(2):153–9. https://doi.org/10.1038/sj.pcan.4500992.
Sculpher M, Bryan S, Fry P, de Winter P, Payne H, Emberton M. Patients’ preferences for the management of non-metastatic prostate cancer: discrete choice experiment. BMJ. 2004;328(7436):382. https://doi.org/10.1136/bmj.37972.497234.44.
Hauber AB, Arellano J, Qian Y, González JM, Posner JD, Mohamed AF, et al. Patient preferences for treatments to delay bone metastases. Prostate. 2014;74(15):1488–97. https://doi.org/10.1002/pros.22865.
Hechmati G, Hauber AB, Arellano J, Mohamed AF, Qian Y, Gatta F, et al. Patients’ preferences for bone metastases treatments in France, Germany and the United Kingdom. Support Care Cancer. 2015;23(1):21–8. https://doi.org/10.1007/s00520-014-2309-x.
Eliasson L, de Freitas HM, Dearden L, Calimlim B, Lloyd AJ. Patients’ preferences for the treatment of metastatic castrate-resistant prostate cancer: a discrete choice experiment. Clin Ther. 2017;39(4):723–37. https://doi.org/10.1016/j.clinthera.2017.02.009.
King MT, Viney R, Smith DP, Hossain I, Street D, Savage E, et al. Survival gains needed to offset persistent adverse treatment effects in localised prostate cancer. Br J Cancer. 2012;106(4):638–45. https://doi.org/10.1038/bjc.2011.552.
de Freitas HM, Ito T, Hadi M, Al-Jassar G, Henry-Szatkowski M, Nafees B, et al. Patient preferences for metastatic hormone-sensitive prostate cancer treatments: a discrete choice experiment among men in three European countries. Adv Ther. 2019;36(2):318–32. https://doi.org/10.1007/s12325-018-0861-3.
George DJ, Mohamed AF, Tsai JH, Karimi M, Ning N, Jayade S, et al. Understanding what matters to metastatic castration-resistant prostate cancer (mCRPC) patients when considering treatment options: a US patient preference survey. Cancer Med. 2022. https://doi.org/10.1002/cam4.5313.
Uemura H, Matsubara N, Kimura G, Yamaguchi A, Ledesma DA, DiBonaventura M, et al. Patient preferences for treatment of castration-resistant prostate cancer in Japan: a discrete-choice experiment. BMC Urol. 2016;16(1):63. https://doi.org/10.1186/s12894-016-0182-2.
Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint analysis applications in health-a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14(4):403–13. https://doi.org/10.1016/j.jval.2010.11.013.
Jonker MF, Donkers B, de Bekker-Grob E, Stolk EA. Attribute level overlap (and color coding) can reduce task complexity, improve choice consistency, and decrease the dropout rate in discrete choice experiments. Health Econ. 2019;28(3):350–63. https://doi.org/10.1002/hec.3846.
Kuhfeld WF. Marketing research methods in SAS: experimental design, choice, conjoint, and graphical techniques. Cary: SAS Institute Inc; 2010.
Janssen EM, Hauber AB, Bridges JFP. Conducting a discrete-choice experiment study following recommendations for good research practices: an application for eliciting patient preferences for diabetes treatments. Value Health. 2018;21(1):59–68. https://doi.org/10.1016/j.jval.2017.07.001.
World Medical Association: WMA Declaration of Helsinki—ethical principles for medical research involving human subjects. 2022. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/#:~:text=The%20World%20Medical%20Association%20(WMA,identifiable%20human%20material%20and%20data. Accessed 19 Oct 2022.
Orme B. Getting started with conjoint analysis: strategies for product design and pricing research. 2nd ed. Madison: Research Publishers LLC; 2010.
Yang J-C, Johnson FR, Kilambi V, Mohamed AF. Sample size and utility-difference precision in discrete-choice experiments: a meta-simulation approach. J Choice Model. 2015;16(C):50–7.
Hauber AB, González JM, Groothuis-Oudshoorn CG, Prior T, Marshall DA, Cunningham C, et al. Statistical methods for the analysis of discrete choice experiments: a report of the ISPOR Conjoint Analysis Good Research Practices Task Force. Value Health. 2016;19(4):300–15. https://doi.org/10.1016/j.jval.2016.04.004.
Hensher DA, Rose JM, Greene WH. Combining RP and SP data: biases in using the nested logit ‘trick’—contrasts with flexible mixed logit incorporating panel and scale effects. J Transp Geogr. 2008;16(2):126–33. https://doi.org/10.1016/j.jtrangeo.2007.07.001.
Jonker MF. The garbage class mixed logit model: accounting for low-quality response patterns in discrete choice experiments. Value Health. 2022;25(11):1871–7. https://doi.org/10.1016/j.jval.2022.07.013.
Sepulveda JMG, Baid D, Johnson FR, Finkelstein EA. What is a good death? A choice experiment on care indicators for patients at end of life. J Pain Symptom Manage. 2022;63(4):457–67. https://doi.org/10.1016/j.jpainsymman.2021.11.005.
Assi T, Ibrahim N, Rita-Maria KA, Kattan C, Rassy E, Nemr E, et al. The management of patients with metastatic prostate cancer during the COVID-19 pandemic. Future Oncol. 2020;16(20):1455–61. https://doi.org/10.2217/fon-2020-0361.
Hout M, Arbelaez MCS, Nackeeran S, Blachman-Braun R, Shah K, Towe M, et al. Impact of COVID-19 pandemic on diagnosis and surgical management of common urological conditions: results from multi-institutional database analysis from the United States. World J Urol. 2022;2022:1–6. https://doi.org/10.1007/s00345-022-04167-0.
Fizazi K, Foulon S, Carles J, Roubaud G, McDermott R, Fléchon A, et al. Abiraterone plus prednisone added to androgen deprivation therapy and docetaxel in de novo metastatic castration-sensitive prostate cancer (PEACE-1): a multicentre, open-label, randomised, phase 3 study with a 2 × 2 factorial design. Lancet. 2022;399(10336):1695–707. https://doi.org/10.1016/s0140-6736(22)00367-1.
Smith MR, Hussain M, Saad F, Fizazi K, Sternberg CN, Crawford ED, et al. Darolutamide and survival in metastatic, hormone-sensitive prostate cancer. N Engl J Med. 2022;386(12):1132–42. https://doi.org/10.1056/NEJMoa2119115.
European Medicines Agency (EMA): The patient’s voice in the evaluation of medicines. 2013. https://www.ema.europa.eu/en/documents/report/report-workshop-patients-voice-evaluation-medicines_en.pdf. Accessed 29 Aug 2022.
Acknowledgements
The authors acknowledge the contribution made by Kiran Grover during survey development. The authors would also like to thank Lakshman Puli (PhD), Olga Klibanov (PharmD), Jay Patel (PharmD), Laura Huber (BA), and Andrew McCulloch (BA Hons) from IQVIA for medical writing and editorial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Astellas Pharma Inc. and Pfizer Inc., the co-developers of enzalutamide. Astellas Pharma Inc. participated in study design, data collection, data analysis, data interpretation, and writing of the report. The funders reviewed the draft of the manuscript. Pfizer Inc. did not have any role in study design, data collection, data analysis, data interpretation, or writing of the report.
Conflict of Interest
MJW does not have competing interests or any financial disclosures to make. JMG is an employee of Duke University. Duke University received funding to conduct the study reported in the manuscript. Some of that funding may have been used to cover his salary. JCY is a consultant to Duke University. Duke University received funding to conduct the study reported in the manuscript. A part of the funding pays for her participation in the study. CDS is an employee of Duke University and has received grants from Pfizer, Exelixis, Merck, BMS, and Astellas. Duke University has a contract with Astellas to support this study. A portion of his Duke salary is covered by this research contract. CDS did not receive direct payments from Astellas related to this work. BFT is an advisor and study investigator for Astellas, Bayer, Janssen, and Novartis. BFT received grants from Ferring. BFT also received consulting fees or honorarium, travel support from Astellas, Amgen, AstraZeneca, Bayer, Janssen, Myovant, MSD, and Novartis. AKM received honoraria for consulting from the following companies: Astellas, AstraZeneca, AAA, Janssen, Exelixis, Myovant, Novartis, Pfizer, Sanofi, Telix. AKM received grant support from the following companies: Astellas, Bayer, Myovant, and Pfizer. SJH received clinical trial and/or research grant funding (institution) from Astellas, Bayer, and Janssen; and is on an advisory board membership and honoraria (self). HS received grants from Astellas, Bayer, Janssen, and Nihon Kayaku. HS received consulting fees and honoraria from Astellas, AstraZeneca, Bayer, Chugai, Daiichi-Sankyo, Eli-Lily, Janssen, MSD, Roche, and Sanofi. HS had no influence on the conduct of the study and/or the preparation of this manuscript caused by the conflict of interest stated here. AG, HB, and MO are current employees of Astellas Pharma Inc. DJG is not employed by industry. DJG is supported by grants by Astellas, AstraZeneca, BMS, Calithera, Exelixis, Janssen, Novartis, Pfizer, and Sanofi. DJG received consulting fees and honorarium from Astellas, AstraZeneca, Bayer, Exelixis, IdeoOncology, Janssen, Merck, Michael J Hennessey Assoc, Myovant Sciences, Pfizer, Propella Therapeutics, RevHealth, Sanofi, Seattle Genetics, UroGPO, WebMD, and Xcures. DJG is supported for speaker bureaus and travel from Bayer, Exelixis, and Sanofi and received fees for participation in review activities such as data monitoring boards, etc. from Astellas-Advisory Board; AstraZeneca-Advisory Board, CAPI-281 SC; Janssen-Independent Data Monitoring Committee; NCI Genitourinary SC; Pfizer SC. DJG received fees from Wilmer Hale Atty for expert testimony and received royalties from Up-to-Date. DJG also received fees from AAA/Novartis; AACR: Sr Editor; Millennium Medical Publishing, Clinical Advances in Hematology & Oncology, Co-Editor-in-Chief.
Availability of Data and Material
Researchers may request access to anonymized participant-level data, trial-level data, and protocols from Astellas-sponsored clinical trials at www.clinicalstudydatarequest.com. For the Astellas criteria on data sharing, see https://clinicalstudydatarequest.com/Study-Sponsors/Study-Sponsors-Astellas.aspx.
Author Contributions
Conceptualization: Juan Marcos Gonzalez, Arijit Ganguli, Hemant Bhadauria, Mok Oh, Daniel J. George; Methodology: Juan Marcos Gonzalez, Arijit Ganguli, Alicia K. Morgans, Bertrand F. Tombal, Sebastien J. Hotte, Hiroyoshi Suzuki, Hemant Bhadauria, Mok Oh, Charles D. Scales , Jr, Matthew J. Wallace, Jui-Chen Yang, Daniel J. George; Validation: Juan Marcos Gonzalez, Arijit Ganguli, Alicia K. Morgans, Bertrand F. Tombal, Sebastien J. Hotte, Hiroyoshi Suzuki, Hemant Bhadauria, Mok Oh, Charles D. Scales, Jr, Matthew J. Wallace, Jui-Chen Yang, Daniel J. George; Formal analysis: Juan Marcos Gonzalez, Sebastien J. Hotte, Charles D. Scales , Jr, Matthew J. Wallace, Jui-Chen Yang; Investigation: Juan Marcos Gonzalez; Writing—original draft preparation: Juan Marcos Gonzalez, Sebastien J. Hotte, Mok Oh, Charles D. Scales, Jr, Matthew J. Wallace, Jui-Chen Yang; Writing—review and editing: Juan Marcos Gonzalez, Arijit Ganguli, Alicia K. Morgans, Bertrand F. Tombal, Sebastien J. Hotte, Hiroyoshi Suzuki, Hemant Bhadauria, Mok Oh, Charles D. Scales, Jr, Matthew J. Wallace, Jui-Chen Yang, Daniel J. George; Visualization: Matthew J. Wallace, Jui-Chen Yang; Supervision: Juan Marcos Gonzalez, Arijit Ganguli; Project administration: Juan Marcos Gonzalez
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gonzalez, J.M., Ganguli, A., Morgans, A.K. et al. Discrete-Choice Experiment to Understand the Preferences of Patients with Hormone-Sensitive Prostate Cancer in the USA, Canada, and the UK. Patient 16, 607–623 (2023). https://doi.org/10.1007/s40271-023-00638-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-023-00638-7