Abstract
Background
More Medicaid holders are entering the healthcare system consequential to Medicaid expansion. Their experience has financial consequences for hospitals and crucial implications for the provision of patient-centered care. This study examined how the hospital characteristics, especially the rates of Medicaid coverage and racial/ethnic minorities, impact the quality of inpatient care.
Methods
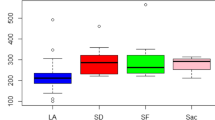
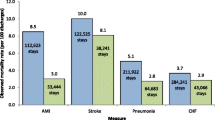
Using data for years 2009–2011 for 870 observations of California hospitals, and data collected from patients via the Hospital Consumer Assessment of Healthcare Providers and Systems survey coupled with data from the Healthcare Cost and Utilization Project and American Hospital Association Annual Survey, we used a generalized estimating equation approach to evaluate patients’ experience with hospital care. Our multivariate model includes a comprehensive set of characteristics capturing market, structural, process, and patient demographics associated with the patient’s hospital stay.
Results
The findings indicate that high concentrations of Medicaid patients in the hospital negatively impact the perceived patient experience. In addition, all things being equal, hospitals with higher concentrations of Hispanic, Black, and Asian patients received lower patient satisfaction results on 28 of the 30 regression coefficients capturing patient satisfaction, with 22 of the 30 negative coefficients statistically significant.
Conclusions
Hospitals serving higher concentrations of Medicaid patients and more racial/ethnic diverse patients experienced a less satisfactory patient experience than patients utilizing other payers or patients who were White. Our research magnifies the challenge for addressing the disparities that exist in healthcare. Further research is called for clarifying the underlying reasons for these disparities and the optimal strategies for addressing these problems.
Similar content being viewed by others
References
Donabedian A. The quality of care: how can it be assessed? JAMA. 1988;260(12):1743–8.
Anhang Price R, Elliott MN, Zaslavsky AM, Hays RD, Lehrman WG, Rybowski L, et al. Examining the role of patient experience surveys in measuring health care quality. Med Care Res Rev. 2014;71(5):522–54.
Spaulding A, Zhao M, Haley DR. Value-based purchasing and hospital acquired conditions: are we seeing improvement? Health Policy. 2014;118(3):413–21.
Medicaid Rosenbaum S. N Engl J Med. 2002;346(8):635–40.
Medicaid and CHIP Payment and Access Commission. Report to Congress on Medicaid and CHIP. Washington, DC; 2011.
The Henry J. Kaiser Family Foundation. State Health Facts. Data source: CMS, Medicaid and CHIP monthly applications, eligibility determinations, and enrollment reports: February 2014–October 2015. Available at: http://kff.org/health-reform/state-indicator/total-monthly-medicaid-and-chip-enrollment/. Accessed 30 Dec 2015.
Chatterjee P, Joynt KE, Orav EJ, Jha AK. Patient experience in safety-net hospitals: implications for improving care and value-based purchasing. Arch Intern Med. 2012;172(16):1204–10.
Neuhausen K, Katz MH. Patient satisfaction and safety-net hospitals: carrots, not sticks, are a better approach. Arch Intern Med. 2012;172(16):1202–3.
Centers for Medicare & Medicaid Services (CMS). HCAHPS fact sheet. Available at: http://www.hcahpsonline.org/Facts.aspx. Accessed 18 Dec 2015.
Ahmed F, Burt J, Roland M. Measuring patient experience: concepts and methods. Patient. 2014;7(3):235–41.
Fung CH, Setodji CM, Kung FY, Keesey J, Asch SM, Adams J, et al. The relationship between multimorbidity and patients’ ratings of communication. J Gen Intern Med. 2008;23(6):788–93.
Mead N, Roland M. Understanding why some ethnic minority patients evaluate medical care more negatively than white patients: a cross sectional analysis of a routine patient survey in English general practices. BMJ. 2009;339:b3450.
Weinick RM, Hasnain-Wynia R. Quality improvement efforts under health reform: how to ensure that they help reduce disparities–not increase them. Health Aff (Millwood). 2011;30(10):1837–43.
Ryan AM. Will value-based purchasing increase disparities in care? N Engl J Med. 2013;369(26):2472–4.
Elliott MN, Haviland AM, Kanouse DE, Hambarsoomian K, Hays RD. Adjusting for subgroup differences in extreme response tendency in ratings of health care: impact on disparity estimates. Health Serv Res. 2009;44(2 Pt 1):542–61.
Weech-Maldonado R, Morales LS, Elliott M, Spritzer K, Marshall G, Hays RD. Race/ethnicity, language, and patients’ assessments of care in Medicaid managed care. Health Serv Res. 2003;38(3):789–808.
Cagney KA, Browning CR, Wen M. Racial disparities in self-rated health at older ages: what difference does the neighborhood make? J Gerontol B Psychol Sci Soc Sci. 2005;60(4):S181–90 (Epub 2005/06/28).
Goldstein E, Elliott MN, Lehrman WG, Hambarsoomian K, Giordano LA. Racial/ethnic differences in patients’ perceptions of inpatient care using the HCAHPS survey. Med Care Res Rev. 2010;67(1):74–92.
Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201–3.
Beach MC, Saha S, Korthuis PT, Sharp V, Cohn J, Wilson I, et al. Differences in patient-provider communication for Hispanic compared to non-Hispanic white patients in HIV care. J Gen Intern Med. 2010;25(7):682–7.
Al-Rashed SA, Wright DJ, Roebuck N, Sunter W, Chrystyn H. The value of inpatient pharmaceutical counselling to elderly patients prior to discharge. Br J Clin Pharmacol. 2002;54:657–64.
Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3(1):e001570. doi:10.1136/bmjopen-2012-001570
Jha AK, Li Z, Orav EJ, Epstein AM. Care in U.S. hospitals: the Hospital Quality Alliance program. N Engl J Med. 2005;353(3):265–74.
Allison JJ, Kiefe CI, Weissman NW, Person SD, Rousculp M, Canto JG, et al. Relationship of hospital teaching status with quality of care and mortality for Medicare patients with acute MI. JAMA. 2000;284(10):1256–62.
Levinton C, Veillard J, Slutsky A, Brown A. The importance of place of residence in patient satisfaction. Int J Qual Health Care. 2011;23(5):495–502.
Lehrman WG, Elliott MN, Goldstein E, Beckett MK, Klein DJ, Giordano LA. Characteristics of hospitals demonstrating superior performance in patient experience and clinical process measures of care. Med Care Res Rev. 2010;67(1):38–55.
Kieft RA, de Brouwer BB, Francke AL, Delnoij DM. How nurses and their work environment affect patient experiences of the quality of care: a qualitative study. BMC Health Serv Res. 2014;14:249.
Jha AK, Orav EJ, Zheng J, Epstein AM. Patients’ perception of hospital care in the United States. N Engl J Med. 2008;359(18):1921–31.
Shahian DM, Liu X, Meyer GS, Torchiana DF, Normand SL. Hospital teaching intensity and mortality for acute myocardial infarction, heart failure, and pneumonia. Med Care. 2014;52(1):38–46.
Centers for Medicare & Medicaid Services. Hospital Consumer Assessment of Healthcare Providers and Systems. Available at: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/hospitalcompare.html. Accessed 10 Feb 2015.
Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP). Available at: http://www.ahrq.gov/research/data/hcup/index.html. Accessed July 2013.
American Hospital Association. AHA Annual Survey Database. 2012. Available at: http://www.ahadataviewer.com/Global/survey%20instruments/2012%20AHA%20Annual%20Survey_FINAL_PRINT_20613.pdf. Accessed 10 Feb 2016.
Westbrook KW, Babakus E, Grant CC. Measuring patient-perceived hospital service quality: validity and managerial usefulness of HCAHPS scales. Health Mark Q. 2014;31(2):97–114.
Giordano LA, Elliott MN, Goldstein E, Lehrman WG, Spencer PA. Development, implementation, and public reporting of the HCAHPS survey. Med Care Res Rev. 2010;67(1):27–37.
American Hospital Association. Fast facts on US hospitals. Available at: http://www.aha.org/research/rc/stat-studies/fast-facts.shtml#community. Accessed 19 Feb 2016.
Smith MW, Friedman B, Karaca Z, Wong HS. Predicting inpatient hospital payments in the United States: a retrospective analysis. BMC Health Serv Res. 2015;15:372.
DeShazo JP, Hoffman MA. A comparison of a multistate inpatient EHR database to the HCUP Nationwide Inpatient Sample. BMC Health Serv Res. 2015;15:384.
The Henry J. Kaiser Family Foundation. State Health Facts. Data source: 1999–2013 AHA annual survey. Available at: http://kff.org/other/state-indicator/total-hospitals/. Accessed 10 Dec 2015.
Werner RM, Goldman LE, Dudley RA. Comparison of change in quality of care between safety-net and non-safety-net hospitals. JAMA. 2008;299(18):2180–7.
Hubbard AE, Ahern J, Fleischer NL, LaanMVd Lippman SA, Jewell N, et al. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology. 2010;21(4):467–74.
Weinick RM, Elliott MN, Volandes AE, Lopez L, Burkhart Q, Schlesinger M. Using standardized encounters to understand reported racial/ethnic disparities in patient experiences with care. Health Serv Res. 2011;46(2):491–509.
Porter ME, Olmsted E. Redefining health care: creating value-based competition on results. Boston: Harvard Business Press; 2006.
Tanenbaum SJ. Pay for performance in Medicare: evidentiary irony and the politics of value. J Health Politics Policy Law. 2009;34(5):717–46.
Werner RM, Dudley RA. Medicare’s new hospital value-based purchasing program is likely to have only a small impact on hospital payments. Health Aff (Millwood). 2012;31(9):1932–40.
Centers for Medicare & Medicaid Services. Summary of HCAHPS survey results. Available at: http://www.hcahpsonline.org/files/HCAHPS%20Survey%20Results%20Table%20(Report_HEI_October_2011_States).pdf . [Public Reporting Period]. Baltimore (MD). Accessed 17 Dec 2015.
Author contributions
Sandra Liu developed the conceptual framework, coordinated the study, reviewed relevant literatures, and drafted and revised the manuscript; Yu-Ping Wen conducted the data analyses, reviewed relevant literatures, and drafted the manuscript; Soumya Mohan reviewed the relevant literatures, and drafted the manuscript; Jaeyong Bae compiled the data and revised the manuscript; and Edmund R. Becker developed the conceptual framework, coordinated the study, reviewed the relevant literatures, and revised the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Sandra S. Liu, Yu-Ping Wen, Soumya Mohan, Jaeyong Bae, and Edmund R. Becker declare that they have no conflicts of interest.
Funding
This research was supported by a Patient-Centered Outcomes Research Institute (PCORI) Pilot Project Program Award (1IP2PI000167-01). All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the PCORI, its board of governors, or its Methodology Committee (http://www.pcori.org/research-results/2012/patient-centered-care-what-factors-drive-outcomes-hospital-setting).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, S.S., Wen, YP., Mohan, S. et al. Addressing Medicaid Expansion from the Perspective of Patient Experience in Hospitals. Patient 9, 445–455 (2016). https://doi.org/10.1007/s40271-016-0167-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-016-0167-y