Abstract
Background and Objective
Methylmalonic aciduria (MMA) and propionic aciduria (PA) are organic acidurias characterised by the accumulation of toxic metabolites and hyperammonaemia related to secondary N-acetylglutamate deficiency. Carglumic acid, a synthetic analogue of N-acetylglutamate, decreases ammonia levels by restoring the functioning of the urea cycle. However, there are limited data available on the long-term safety and effectiveness of carglumic acid. Here, we present an interim analysis of the ongoing, long-term, prospective, observational PROTECT study (NCT04176523), which is investigating the long-term use of carglumic acid in children and adults with MMA and PA.
Methods
Individuals with MMA or PA from France, Germany, Italy, Norway, Spain, Sweden and the UK who have received at least 1 year of carglumic acid treatment as part of their usual care are eligible for inclusion. The primary objective is the number and duration of acute metabolic decompensation events with hyperammonaemia (ammonia level >159 µmol/L during a patient’s first month of life or >60 µmol/L thereafter, with an increased lactate level [> 1.8 mmol/L] and/or acidosis [pH < 7.35]) before and after treatment with carglumic acid. Peak plasma ammonia levels during the last decompensation event before and the first decompensation event after carglumic acid initiation, and the annualised rate of decompensation events before and after treatment initiation are also being assessed. Secondary objectives include the duration of hospital stay associated with decompensation events. Data are being collected at approximately 12 months’ and 18 months’ follow-up.
Results
Of the patients currently enrolled in the PROTECT study, data from ten available patients with MMA (n = 4) and PA (n = 6) were analysed. The patients had received carglumic acid for 14–77 (mean 36) months. Carglumic acid reduced the median peak ammonia level of the total patient population from 250 µmol/L (range 97–2569) before treatment to 103 µmol/L (range 97–171) after treatment. The annualised rate of acute metabolic decompensations with hyperammonaemia was reduced by a median of – 41% (range − 100% to + 60%) after treatment with carglumic acid. Of the five patients who experienced a decompensation event before treatment and for whom a post-treatment rate could be calculated, the annualised decompensation event rate was lower after carglumic acid treatment in four patients. The mean duration of hospital inpatient stay during decompensation events was shorter after than before carglumic acid treatment initiation in four of five patients for whom length of stay could be calculated.
Conclusions
In this group of patients with MMA and PA, treatment with carglumic acid for at least 1 year reduced peak plasma ammonia levels in the total patient population and reduced the frequency of metabolic decompensation events, as well as the duration of inpatient stay due to metabolic decompensations in a subset of patients.
Clinical Trial Registration
ClinicalTrials.gov, NCT04176523. Registered 25 November, 2019, retrospectively registered, https://clinicaltrials.gov/ct2/show/NCT04176523.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Propionic aciduria and methylmalonic aciduria are inherited metabolic disorders that result in the accumulation of toxic metabolites and excessively high levels of ammonia. |
Carglumic acid decreases ammonia levels and is a recognised treatment for acute hyperammonaemia in propionic aciduria and methylmalonic aciduria; however, there is limited experience with its long-term use. The PROTECT study is an ongoing observational study of the effects of long-term carglumic acid treatment in adults and children with propionic aciduria or methylmalonic aciduria. |
The interim analysis reported in this article presents data from ten individuals in the PROTECT study. The data indicate that treatment with carglumic acid for at least 1 year reduces peak plasma ammonia levels and the frequency of metabolic decompensation events, as well as the duration of inpatient hospital stay due to metabolic decompensations in some patients. |
1 Introduction
Organic acidurias (OAs) are a class of autosomal recessive inherited diseases that arise from defects in fatty acid, carbohydrate or amino acid metabolic pathways [1]. The pathophysiology of OAs is complex and multifactorial and can be due to mutations in several genes [2,3,4,5,6]. Organic acidurias resulting from defects in the propionate metabolic pathway include propionic aciduria (PA) and methylmalonic aciduria (MMA), which are caused by deficiencies of propionyl-coenzyme A (CoA) carboxylase and methylmalonyl-CoA mutase, respectively [7, 8]. Because of these enzyme deficiencies, there is an accumulation of their associated acyl CoA esters [7, 8], inducing CoA depletion and secondary cataplerosis, which is associated with low blood glutamate and glutamine levels in these diseases [9]. This, in turn, leads to a secondary deficiency of N-acetylglutamate (NAG) synthesis. As NAG is an activator of carbamoyl phosphate synthetase 1, which is involved in the first step of the urea cycle, these diseases induce secondary hyperammonaemia [10, 11]. In addition, disrupted metabolism associated with MMA and PA can cause secondary carnitine depletion [12], inhibition of pyruvate dehydrogenase and pyruvate carboxylase [13, 14], inhibition of respiratory chain complexes [15], impaired replenishment of the Krebs cycle, increased glutamate release [16], and altered neuronal and glial gene expression [16, 17].
Because of this complex pathophysiology, including the accumulation of toxic compounds, energy deprivation and hyperammonaemia, patients with severe OAs, such as MMA and PA, have typically poor outcomes [18], often experiencing neurological complications (such as cognitive impairment, movement disorders, stroke, loss of vision), cardiomyopathy, pancreatitis, renal failure and growth failure [1, 7, 8, 17, 19]. If not treated immediately, metabolic decompensations of OAs with hyperammonaemia progress to seizures, coma, multi-organ failure and even death [7, 8, 20]. The treatment of OAs aims to restore the biochemical and physiological homeostasis, thereby promoting normal growth and development [7]. In addition to dextrose-containing emergency regimes provided in case of intercurrent illness, mainstay treatment generally involves the prevention of endogenous protein catabolism by regular meals and avoidance of fasting, dietary protein restriction, use of antibiotics to decrease propionyl-CoA production by gut flora and scavenging of the accumulated toxins [7, 8]. Cofactors (such as vitamin B12 for B12-responsive MMA and biotin as a cofactor for propionyl-CoA carboxylase in PA) and supplements (such as carnitine) are used to help remove the intermediate products of the metabolic decompensation, which is suggested to improve patient prognosis [21, 22]. The management of secondary hyperammonaemia is also important, as this is a medical emergency for which delays in treatment are associated with poor prognosis [23]. Carglumic acid (Carbaglu®; Recordati Rare Diseases, Lebanon, NJ, USA), a synthetic analogue of NAG that activates carbamoyl phosphate synthetase 1, can be used in the acute setting to restore functioning of the urea cycle and, hence, to reduce the levels of ammonia.
Carglumic acid was approved by the European Medicines Agency for the treatment of hyperammonaemia due to primary NAG deficiency in 2003, and for the treatment of hyperammonaemia due to MMA, PA or isovaleric aciduria in 2011 [24, 25]. Several large retrospective analyses have shown that short-term treatment with carglumic acid is efficacious and well tolerated for the management of hyperammonaemia during metabolic decompensation events [26, 27], and a more recent 2-year randomised trial reported that carglumic acid in addition to standard treatment significantly reduced the number of emergency room visits in patients with PA and MMA compared with standard treatment alone [28]. Case reports [29, 30] and case series [31, 32] have reported a reduction in metabolic decompensation events with long-term carglumic acid treatment.
Here, we present an interim analysis of the PRospective Observational study of long-TErm Carbaglu® for the Treatment of PA & MMA (PROTECT), a prospective observational study that aims to investigate the long-term management of MMA and PA with carglumic acid. The data presented herein provide an initial assessment of the effectiveness of long-term treatment with carglumic acid, which will be helpful to guide the treatment of patients with these rare diseases until more follow-up data become available from studies such as PROTECT. When completed, PROTECT will be the largest long-term study to date of carglumic acid in patients with MMA and PA.
2 Methods
2.1 Study Design and Participants
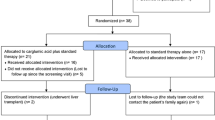
PROTECT (ClinicalTrials.gov record: NCT04176523) is a prospective, multicentre, observational study enrolling patients from France, Germany, Italy, Norway, Spain, Sweden and the UK. The enrolment phase of the study was initiated in January 2019 and is ongoing.
Children or adults with MMA or PA who have received at least 1 year of treatment with carglumic acid as part of their usual care are eligible for this study. Inclusion in this study is not dependent on metabolic decompensation. There are no exclusion criteria, with the exception of the patient or caregiver not agreeing to participate in the study.
The study is being conducted in accordance with the ethical standards of the institutional and/or national research committees at each centre and with the 1964 Declaration of Helsinki, as revised in 2013. The study protocol has been approved by the local institutional review board at each study site, and written informed consent is being collected from all participants or their caregivers before initiating the study.
2.2 Outcomes
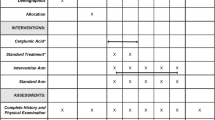
The primary objective of the PROTECT study is to describe and compare the number and duration of acute metabolic decompensation with hyperammonaemia events before and after treatment with carglumic acid. Acute metabolic decompensation is defined as an increased ammonia level (> 159 µmol/L during a patient’s first month of life or > 60 µmol/L thereafter) with an increased lactate level (> 1.8 mmol/L) and/or acidosis (pH < 7.35), based on the investigators’ clinical experience in treating patients with MMA and PA. The peak plasma ammonia levels are being recorded during the last decompensation event before the start of carglumic acid and the first decompensation event after the initiation of long-term carglumic acid. The annualised rate of decompensation events before and after treatment with carglumic acid is also being assessed. For patients who were < 3 months of age when treatment with carglumic acid was initiated, it is not possible to estimate the rates of decompensation before treatment because insufficient time will have elapsed since the diagnosis and initiation of treatment to allow such rates to be calculated. The secondary objectives are to assess the healthcare resources utilised in association with a decompensation event and to describe the patient and caregiver burden associated with MMA and PA, and patient and/or caregiver satisfaction with treatment. The outcomes reported in this interim analysis are summarised in Table 1.
Data are being collected at baseline (i.e. the date at which consent was received for patient participation in the study, which was following at least 1 year of prior treatment with carglumic acid), and at approximately 12 months’ and 18 months’ follow-up. At baseline, the medical charts of each patient are reviewed, with any relevant demographic and medical history information recorded, as well as baseline safety data (rates, duration, outcomes, severity, action taken and causality of adverse events), disease-related resource use (visits to the emergency room, general practitioners and specialists, number and duration of hospital/inpatient stays and use of outpatient services), clinical outcomes (number and duration of all decompensation events, use of emergency room or hospitalisation for decompensation events, treatments for decompensation events, dietary data, ammonia levels and other laboratory values) and treatment details (names, dose and frequency of drugs used for the long-term management of MMA or PA). During the study, safety data, disease-related resource use, clinical outcomes and treatment details are being collected using medical charts. All data are being recorded through a web-based electronic data capture system.
If possible, each patient (or their caregiver) will also undergo a one-on-one phone interview 6 months after enrolment. The interview will take approximately 1 h, with the aim of obtaining information about the patients’ symptoms and the impact of the disease, as well as the patients’ and caregivers’ experiences with carglumic acid, their treatment preferences and satisfaction with treatment. The interview uses a pre-planned questionnaire consisting of open-ended questions to elicit information from the participants and to orient the discussion, and is audio recorded (with the permission of the patients/caregivers) to allow for transcription and subsequent coding of concepts and qualitative analysis of responses.
2.3 Statistical Analysis
As this study is descriptive in nature, no formal sample size calculation was conducted. Nevertheless, it was estimated that a sample size of 40 would be sufficient to meet the study needs; however, in January 2021, the study protocol was amended to include up to 80 patients.
Descriptive statistics will be used to analyse the data. Continuous variables will be summarised using means, medians and ranges, whilst categorical variables will be summarised by absolute and relative frequencies. All statistical analyses in this interim report were conducted using SAS® version 9.4 (SAS/STAT®; SAS Institute Inc., Cary, NC, USA).
3 Results
3.1 Participants
Between January 2019 and December 2020, a total of 42 patients were enrolled from 32 centres. Of these, data for ten patients (median age 5 [range 1.2–12.8] years; 70% male) from France (n = 3), Norway (n = 1), Spain (n = 1) and the UK (n = 5) were available for this interim analysis (Table 2). Four patients had MMA (all were mutase deficient) and six had PA. None of the patients was vitamin B12 responsive. All but one patient were diagnosed during the neonatal period (first days of life); the remaining patient was diagnosed aged approximately 5 months. At diagnosis, the most common presentation was encephalopathy (patients 1, 2, 3, 5, 6 and 7). Other presentations included renal damage (a typical presentation for patients with MMA that was seen in one patient [patient 2] with MMA in this study), metabolic acidosis and metabolic stroke (in one patient each with PA [patient 8 and patient 5, respectively]; Table 2).
Patients initiated treatment with carglumic acid at a mean age of 28.1 (range 0–95) months; four patients initiated treatment in the neonatal period (MMA, n = 2 and PA, n = 2). Carglumic acid was administered for a mean of 36 (range 14–77) months, giving a total patient-years of carglumic acid treatment of 33.9 years (8 years for patients with MMA and 25.9 years for patients with PA). Table 3 provides the specific doses of carglumic acid administered to each patient and the number of post-initiation dose changes. Dietary management prior to carglumic acid treatment initiation is summarised in Table 4.
3.2 Ammonia Levels
Before treatment with carglumic acid, excluding the primary presenting event in the neonatal period, the median peak ammonia level was 250 µmol/L (range 97–2569) in the total patient population; median peak ammonia level was 127.5 µmol/L (range 97–158) and 279 µmol/L (range 201–2569) in patients with MMA and PA, respectively. After treatment with carglumic acid, the median peak ammonia level was reduced to 103 µmol/L (range 97–171) in the total patient population, and 161 µmol/L (range 105–171) and 100 µmol/L (range 97–101) in patients with MMA and PA, respectively.
Of the five patients (patients 2, 3, 8, 9 and 10) who experienced a decompensation event both before and after treatment with carglumic acid, three patients (60%; patients 8, 9 and 10, all with PA) had lower mean peak plasma ammonia levels after treatment with carglumic acid (Fig. 1). All patients who had decompensation events after starting treatment with carglumic acid had mean peak ammonia levels of <175 µmol/L.
Mean (95% confidence interval) peak plasma ammonia levels recorded before/after initiation of carglumic acid treatment. #Error bars incalculable because there was only one decompensation event. As peak plasma ammonia levels were recorded only during decompensation events, and patients 4 and 7 did not have decompensation events before/after carglumic acid treatment recorded within the time window of the follow-up, their peak plasma ammonia levels were not measured. MMA methylmalonic aciduria, NDE no decompensation events in time window, PA propionic aciduria
3.3 Decompensation Events
Decompensation events recorded in each patient are shown in Fig. 2, for the period before initiating long-term treatment with carglumic acid, as well as after this treatment. When all events are considered, two patients (patients 4 and 7) had no decompensation events before or after treatment with carglumic acid, and one patient (patient 1) had a decompensation event after initiating carglumic acid treatment but no event was reported before carglumic acid treatment; however, this patient commenced carglumic acid at day 2 of life. Of the remaining seven patients, the median number of events (with or without accompanying hyperammonaemia) prior to initiating long-term treatment with carglumic acid was nine events (range 1–36). After treatment with carglumic acid, four patients had a reduction in the number of decompensation events (patients 2, 5, 6 and 9) and three patients had an increase (patients 3, 8 and 10; Fig. 2). Of the seven patients who had decompensation events that were determined to be accompanied by hyperammonaemia (and excluding the aforementioned patient 1), five patients (patients 2, 5, 6, 9 and 10) had a reduction in such decompensation events after carglumic acid treatment (most strikingly in patient 2, who experienced a reduction from 14 events to 1 event; Fig. 2).
Decompensation events pre-/post-carglumic acid in each patient, including decompensation events accompanied by hyperammonaemia (HA). Time 0 was defined as the initiation of long-term carglumic acid treatment and Time 1 was the start of the study. Age at Time 0 and carglumic acid dose at Time 1 are shown below the graph for each patient. Decompensation events without ammonia level measurements were not counted. *The reason for initiation of carglumic acid treatment was not recorded. MMA methylmalonic aciduria, PA propionic aciduria
Overall, the annualised rate of all decompensation events (with and without hyperammonaemia) decreased by a median – 41% (range – 100% to + 60%) with carglumic acid treatment (from a median of 3.2 [range 1.1–13.1] to 1.95 [range 0.5–6.8] events per year). Of the five patients who experienced a decompensation event before treatment and for whom a post-treatment rate could be calculated, the annualised rate of decompensation events was lower after treatment with carglumic acid in four of them (patients 2, 8, 9 and 10; Fig. 3). The remaining patient (patient 3) had an increase in the annualised rate of decompensation events from 1.65 to 2.64 events per year.
Annualised rate of all decompensation events pre- and post-carglumic acid initiation. The annualised rates of decompensation events were calculated by dividing the number of events by age at carglumic acid initiation (for pre-carglumic acid rates), and by treatment duration (for post-carglumic acid rates). For patients who were <3 months of age when carglumic acid was initiated (patients 1, 4, 5 and 7), a rate of decompensation before treatment was not estimable. MMA methylmalonic aciduria, NE not estimable, PA propionic aciduria
3.4 Hospitalisations
Of the five patients who had decompensation events both before and after starting treatment with carglumic acid (patients 2, 3, 8, 9 and 10), three (patients 2, 3 and 10) had a shorter duration of hospital stay for the first decompensation event after starting carglumic acid than the duration of hospital stay for the last decompensation event prior to starting treatment (see Fig. 1a of the Electronic Supplementary Material [ESM]), with a particularly marked reduction in the duration of stay for patient 2 (from a 16-day stay before starting carglumic acid to a 5-day stay after starting treatment). The mean duration of hospital stay during decompensation events was shorter, for four out of five patients (patients 2, 3, 9 and 10), after initiation of carglumic acid than before initiation of carglumic acid (see Fig. 1b of the ESM); patient 3 showed the greatest reduction in the mean duration of stay (from 13.2 days before starting carglumic acid to 7 days after starting treatment).
4 Discussion
The results of this interim analysis, conducted in December 2020, of ten patients participating in the ongoing, prospective, multicentre, observational PROTECT study show that long-term treatment with carglumic acid reduces the duration of hospital stays during periods of acute metabolic decompensations with hyperammonaemia, and reduces the annualised rate of decompensation events (with and without hyperammonaemia). The acute metabolic decompensations, including hyperammonaemia, associated with MMA and PA impact the physiology and functioning of multiple organs and, in severe cases, can have a fatal outcome [7, 8, 20]. Thus, prevention of these decompensations, reduction of ammonia levels, restoration of biochemical and physiological homeostasis, and promotion of normal growth and development are the main aims of treatment for the disorders.
Our analysis found that carglumic acid treatment indeed resulted in a reduction in ammonia levels: in the five patients who experienced metabolic decompensation events both before and after treatment with carglumic acid, three had lower peak plasma ammonia levels during decompensation events after treatment with carglumic acid compared with before receiving carglumic acid. All three patients had PA; a more marked effect in these patients than in those with MMA is to be expected, as patients with PA have higher circulating levels of propionate and, thus, a greater potential for hyperammonaemia. In the total patient population, the median peak ammonia level during decompensation was also reduced after carglumic acid treatment. Although one patient (patient 3) showed a very small increase in the number of metabolic decompensation events (by 0.9 events/year) after starting carglumic acid, the mean duration of hospital stay for all events after initiation of carglumic acid treatment in this patient was reduced (by 6.2 days; 47%). Further, most patients in whom an annualised rate of decompensation events could be calculated showed a decrease in this parameter. This effect was particularly marked for patient 2, who had MMA. This finding suggests that, despite the potential for a greater effect in patients with PA (as mentioned above), carglumic acid may also be a useful treatment for individuals with MMA.
The interim results of the PROTECT study are in line with those from several case reports [29, 30] and case series [31, 32] reporting the use of long-term carglumic acid in patients with PA and MMA. The first was a case report of a male patient diagnosed with PA at the age of 2 years who, at the age of 9 years, initiated carglumic acid (100 mg/kg/day for 6 months, then 50 mg/kg/day), which resulted in a significant reduction of plasma ammonia levels (from 140.3 ± 47.2 μmol/L to 75.7 ± 37 μmol/L; p < 0.005) over the next 6 years, with only two hospitalisations due to metabolic decompensation in the first year of treatment [29]. Another case report, of a 6-day-old female neonate born with severe PA, demonstrated that treatment with carglumic acid led to metabolic stabilisation by the age of 26 months [30]. Although these two publications were limited to a single patient each and, therefore, the favourable reported outcomes should be interpreted cautiously, a case series assessing the long-term use of carglumic acid in eight patients with MMA (n = 4) or PA (n = 4) demonstrated that long-term treatment with carglumic acid (50 mg/kg/day for 7–16 months) was able to significantly reduce ammonia levels in five patients (all p < 0.05) [31]. Ammonia levels were reduced or maintained within the normal range (11–32 µmol/L) in all but one of the remaining patients; the exception was one patient who experienced a slight increase in ammonia levels (to 80 µmol/L) due to a shortage of the drug. Once the drug was reintroduced, this patient’s ammonia levels normalised [31]. In addition, the number and severity of metabolic decompensations experienced by these patients were reduced, with none of them requiring hospitalisation for such decompensations. These results are further supported by another case series study that included 21 patients (11 patients with MMA and ten patients with PA) treated with carglumic acid for a median of almost 2 years. Of these, data from 11 patients were available to compare ammonia levels in plasma before versus during carglumic acid treatment. Ammonia levels significantly decreased in nine patients (five patients with MMA and four with PA) during treatment (from 69.64 ± 17.828 μmol/L to 55.31 ± 13.762 μmol/L; p = 0.021) with no apparent adverse events and no treatment discontinuation [32], suggesting that long-term carglumic acid effectively reduces ammonia levels in patients with MMA and PA, with a good safety profile.
A recently published, prospective clinical trial has provided more robust evidence of the effectiveness of long-term treatment with carglumic acid in patients with PA and MMA [28]. In this multicentre, randomised, parallel-group, open-label, controlled study, carglumic acid (50 mg/day in two divided doses) plus standard treatment (L-carnitine, metronidazole and a protein-restricted diet; n = 16) was compared to standard treatment alone (n = 17). The primary outcome measure was the impact of treatment on the number of emergency room visits over the course of 2 years. Secondary outcomes included effects on plasma ammonia levels, time to the first episode of hyperammonaemia, levels of relevant biochemical biomarkers and the number of hospitalisation days. Similar to the findings from our interim analysis of the PROTECT study, carglumic acid plus standard treatment was found to reduce emergency room admissions (by 51%) compared with standard treatment alone; however, no significant effects were seen on the secondary endpoints (including ammonia levels), with the exception of a reduction in glycine and free carnitine levels in the carglumic acid group.
The results of the interim analysis of the PROTECT study are also broadly consistent with previous case reports [33,34,35,36,37,38], case series [4, 39,40,41,42,43] and retrospective studies [27] of carglumic acid in patients with MMA or PA, which all established that short-term treatment with carglumic acid is efficacious and well tolerated for the treatment of acute decompensation with hyperammonaemia events in patients with OAs. In a pooled analysis of two retrospective observational studies, carglumic acid with or without ammonia scavengers significantly reduced plasma ammonia levels compared with ammonia scavengers alone in the first 72 h of treatment [26]. These reductions were also associated with improvements in clinical symptoms and neurological signs, indicating the superiority of carglumic acid over ammonia scavengers to manage decompensation events. Another study, this time a retrospective phase 3b trial of 41 patients with a confirmed diagnosis of OA who had at least one metabolic decompensation event that was treated with carglumic acid, demonstrated that plasma ammonia levels decreased rapidly from baseline following initiation of carglumic acid. Normalisation of ammonia typically occurred within 2–3 days of treatment, and carglumic acid was also associated with an improvement in clinical symptoms [27].
There are a number of limitations to our interim analysis, some of which are inherent to observational real-world studies such as the PROTECT study, and to studies of rare diseases such as OAs [44]. These include the small number of patients with data currently available (likely leading to a large degree of variability in inter-patient data), the relatively short duration over which the patients have been treated and the lack of comprehensive information on certain parameters (such as adverse events associated with carglumic acid; concomitant treatments taken at specific timepoints; diet, weight and psychomotor development of the participants at this stage of the study; and dose units and reasons for dose changes). In particular, a meaningful analysis of an annualised rate of decompensation in this study is limited owing to the size of the patient population and the short follow-up time, as well as by the inclusion of all recorded decompensation events (i.e. including the primary presenting event) and the fact that reporting of decompensation events may change over time as patients, family members and medical teams become more effective at early recognition of and aggressive treatment to prevent these events. Inclusion of the primary presenting event in the decompensation rate analysis may have resulted in an overestimation of the effect of carglumic acid given that, in our clinical experience, hyperammonaemia of subsequent decompensation events is typically more modest than the primary event. Further, the PROTECT study is of an open-label design, which can be associated with reporting bias, and data on acidosis and levels of lactate, propionic acid and methylmalonic acid are not being obtained, which limits analysis of the impact of carglumic acid on the overall metabolic profile of the study participants. Finally, plasma ammonia is a metabolite that is prone to pre-analytical errors, which may interfere with direct comparisons of plasma ammonia levels among patients and between timepoints in individual patients. However, as carglumic acid is used to treat extremely rare diseases, and physicians who care for patients with MMA or PA are continuously waiting for new data, we believe the ongoing collection and communication of data from the PROTECT study, in this case an interim analysis of data from ten patients, provides valuable insight to help guide the management of patients with these diseases.
5 Conclusions
Interim results of the PROTECT study suggest that carglumic acid may reduce the frequency of metabolic decompensation events, the duration of hospital stay due to metabolic decompensation, and peak plasma ammonia levels in some patients with PA and MMA. Complete results of the study in a larger cohort of patients are expected in the near future, which will allow a fuller assessment of the place of carglumic acid in the long-term treatment of patients with these OAs.
References
Vaidyanathan K, Narayanan MP, Vasudevan DM. Organic acidurias: an updated review. Indian J Clin Biochem. 2011;26(4):319–25. https://doi.org/10.1007/s12291-011-0134-2.
Coude FX, Sweetman L, Nyhan WL. Inhibition by propionyl-coenzyme A of N-acetylglutamate synthetase in rat liver mitochondria: a possible explanation for hyperammonemia in propionic and methylmalonic acidemia. J Clin Invest. 1979;64(6):1544–51. https://doi.org/10.1172/JCI109614.
Coude FX, Ogier H, Grimber G, et al. Correlation between blood ammonia concentration and organic acid accumulation in isovaleric and propionic acidemia. Pediatrics. 1982;69(1):115–7.
Ah Mew N, McCarter R, Daikhin Y, Nissim I, Yudkoff M, Tuchman M. N-carbamylglutamate augments ureagenesis and reduces ammonia and glutamine in propionic acidemia. Pediatrics. 2010;126(1):e208–14. https://doi.org/10.1542/peds.2010-0008.
Daniotti M, la Marca G, Fiorini P, Filippi L. New developments in the treatment of hyperammonemia: emerging use of carglumic acid. Int J Gen Med. 2011;4:21–8. https://doi.org/10.2147/IJGM.S10490.
Kasapkara CS, Ezgu FS, Okur I, Tumer L, Biberoglu G, Hasanoglu A. N-carbamylglutamate treatment for acute neonatal hyperammonemia in isovaleric acidemia. Eur J Pediatr. 2011;170(6):799–801. https://doi.org/10.1007/s00431-010-1362-9.
Baumgartner MR, Hörster F, Dionisi-Vici C, et al. Proposed guidelines for the diagnosis and management of methylmalonic and propionic acidemia. Orphanet J Rare Dis. 2014;9:130. https://doi.org/10.1186/s13023-014-0130-8.
Forny P, Horster F, Ballhausen D, et al. Guidelines for the diagnosis and management of methylmalonic acidaemia and propionic acidaemia: first revision. J Inherit Metab Dis. 2021;44(3):566–92. https://doi.org/10.1002/jimd.12370.
Longo N, Price LB, Gappmaier E, et al. Anaplerotic therapy in propionic acidemia. Mol Genet Metab. 2017;122(1–2):51–9. https://doi.org/10.1016/j.ymgme.2017.07.003.
Kölker S, Burgard P, Sauer SW, Okun JG. Current concepts in organic acidurias: understanding intra- and extracerebral disease manifestation. J Inherit Metab Dis. 2013;36(4):635–44. https://doi.org/10.1007/s10545-013-9600-8.
Testai FD, Gorelick PB. Inherited metabolic disorders and stroke part 2: homocystinuria, organic acidurias, and urea cycle disorders. Arch Neurol. 2010;67(2):148–53. https://doi.org/10.1001/archneurol.2009.333.
Chalmers RA, Stacey TE, Tracey BM, et al. L-Carnitine insufficiency in disorders of organic acid metabolism: response to L-carnitine by patients with methylmalonic aciduria and 3-hydroxy-3-methylglutaric aciduria. J Inherit Metab Dis. 1984;7 Suppl. 2:109–10. https://doi.org/10.1007/978-94-009-5612-4_29.
Schwab MA, Sauer SW, Okun JG, et al. Secondary mitochondrial dysfunction in propionic aciduria: a pathogenic role for endogenous mitochondrial toxins. Biochem J. 2006;398(1):107–12. https://doi.org/10.1042/BJ20060221.
Bartlett K, Ghneim HK, Stirk J, Dale G, Alberti KGMM. Pyruvate carboxylase deficiency. In: Addison GM, Chalmers RA, Divry P, Harkness RA, Pollitt RJ, editors. Organic acidurias. Dordrecht: Springer; 1984.
Okun JG, Hörster F, Farkas LM, et al. Neurodegeneration in methylmalonic aciduria involves inhibition of complex II and the tricarboxylic acid cycle, and synergistically acting excitotoxicity. J Biol Chem. 2002;277(17):14674–80. https://doi.org/10.1074/jbc.M200997200.
Wajner M. Neurological manifestations of organic acidurias. Nat Rev Neurol. 2019;15(5):253–71. https://doi.org/10.1038/s41582-019-0161-9.
Nyhan WL, Bay C, Beyer EW, Mazi M. Neurologic nonmetabolic presentation of propionic acidemia. Arch Neurol. 1999;56(9):1143–7. https://doi.org/10.1001/archneur.56.9.1143.
Nizon M, Ottolenghi C, Valayannopoulos V, et al. Long-term neurological outcome of a cohort of 80 patients with classical organic acidurias. Orphanet J Rare Dis. 2013;8:148. https://doi.org/10.1186/1750-1172-8-148.
Hamilton RL, Haas RH, Nyhan WL, Powell HC, Grafe MR. Neuropathology of propionic acidemia: a report of two patients with basal ganglia lesions. J Child Neurol. 1995;10(1):25–30. https://doi.org/10.1177/088307389501000107.
Dionisi-Vici C, Deodato F, Röschinger W, Rhead W, Wilcken B. “Classical” organic acidurias, propionic aciduria, methylmalonic aciduria and isovaleric aciduria: long-term outcome and effects of expanded newborn screening using tandem mass spectrometry. J Inherit Metab Dis. 2006;29(2–3):383–9. https://doi.org/10.1007/s10545-006-0278-z.
Yudkoff M, Ah Mew N, Payan I, et al. Effects of a single dose of N-carbamylglutamate on the rate of ureagenesis. Mol Genet Metab. 2009;98(4):325–30. https://doi.org/10.1016/j.ymgme.2009.07.010.
Van Leynseele A, Jansen A, Goyens P, et al. Early treatment of a child with NAGS deficiency using N-carbamyl glutamate results in a normal neurological outcome. Eur J Pediatr. 2014;173(12):1635–8. https://doi.org/10.1007/s00431-013-2205-2.
Ali R, Nagalli S. Hyperammonemia. StatPearls. Treasure Island: StatPearls Publishing; 2022.
European Medicines Agency (EMA). Carbaglu 200 mg dispersible tablets: summary of product characteristics. 2003. https://www.ema.europa.eu/en/documents/product-information/carbaglu-epar-product-information_en.pdf. Accessed 23 Feb 2021.
European Medicines Agency (EMA) Committee for Medicinal Products for Human Use (CHMP). Carbaglu: summary of opinion (post authorisation). EMA/CHMP/306613/2011. 2011. https://www.ema.europa.eu/en/documents/smop/chmp-post-authorisation-summary-positive-opinion-carbaglu_en.pdf. Accessed 11 Mar 2021.
Chakrapani A, Valayannopoulos V, García Segarra N, et al. Effect of carglumic acid with or without ammonia scavengers on hyperammonaemia in acute decompensation episodes of organic acidurias. Orphanet J Rare Dis. 2018;13(1):97. https://doi.org/10.1186/s13023-018-0840-4.
Valayannopoulos V, Baruteau J, Delgado MB, et al. Carglumic acid enhances rapid ammonia detoxification in classical organic acidurias with a favourable risk-benefit profile: a retrospective observational study. Orphanet J Rare Dis. 2016;11:32. https://doi.org/10.1186/s13023-016-0406-2.
Alfadhel M, Nashabat M, Saleh M, et al. Long-term effectiveness of carglumic acid in patients with propionic acidemia (PA) and methylmalonic acidemia (MMA): a randomized clinical trial. Orphanet J Rare Dis. 2021;16(1):422. https://doi.org/10.1186/s13023-021-02032-8.
Tummolo A, Melpignano L, Carella A, et al. Long-term continuous N-carbamylglutamate treatment in frequently decompensated propionic acidemia: a case report. J Med Case Rep. 2018;12(1):103. https://doi.org/10.1186/s13256-018-1631-1.
Kido J, Matsumoto S, Nakamura K. Carglumic acid contributes to a favorable clinical course in a case of severe propionic acidemia. Case Rep Pediatr. 2020. https://doi.org/10.1155/2020/4709548.
Burlina A, Cazzorla C, Zanonato E, Viggiano E, Fasan I, Polo G. Clinical experience with N-carbamylglutamate in a single-centre cohort of patients with propionic and methylmalonic aciduria. Mol Genet Metab Rep. 2016;8:34–40. https://doi.org/10.1016/j.ymgmr.2016.06.007.
Kiykim E, Oguz O, Duman C, Zubarioglu T, Cansever MS, Zeybek ACA. Long-term N-carbamylglutamate treatment of hyperammonemia in patients with classic organic acidemias. Mol Genet Metab Rep. 2021;26:100715. https://doi.org/10.1016/j.ymgmr.2021.100715.
Filippi L, Gozzini E, Fiorini P, Malvagia S, la Marca G, Donati MA. N-carbamylglutamate in emergency management of hyperammonemia in neonatal acute onset propionic and methylmalonic aciduria. Neonatology. 2010;97(3):286–90. https://doi.org/10.1159/000255168.
Levrat V, Forest I, Fouilhoux A, Acquaviva C, Vianey-Saban C, Guffon N. Carglumic acid: an additional therapy in the treatment of organic acidurias with hyperammonemia? Orphanet J Rare Dis. 2008;3:2. https://doi.org/10.1186/1750-1172-3-2.
Tuchman M, Caldovic L, Daikhin Y, et al. N-carbamylglutamate markedly enhances ureagenesis in N-acetylglutamate deficiency and propionic acidemia as measured by isotopic incorporation and blood biomarkers. Pediatr Res. 2008;64(2):213–7. https://doi.org/10.1203/PDR.0b013e318179454b.
Gebhardt B, Vlaho S, Fischer D, Sewell A, Bohles H. N-carbamylglutamate enhances ammonia detoxification in a patient with decompensated methylmalonic aciduria. Mol Genet Metab. 2003;79(4):303–4. https://doi.org/10.1016/s1096-7192(03)00095-7.
Yap S, Leong HY, Abdul Aziz F, et al. N-carbamylglutamate is an effective treatment for acute neonatal hyperammonaemia in a patient with methylmalonic aciduria. Neonatology. 2016;109(4):303–7. https://doi.org/10.1159/000443630.
Soyucen E, Demirci E, Aydin A. Outpatient treatment of propionic acidemia-associated hyperammonemia with N-carbamoyl-L-glutamate in an infant. Clin Ther. 2010;32(4):710–3. https://doi.org/10.1016/j.clinthera.2010.04.004.
Abacan M, Boneh A. Use of carglumic acid in the treatment of hyperammonaemia during metabolic decompensation of patients with propionic acidaemia. Mol Genet Metab. 2013;109(4):397–401.
Gebhardt B, Dittrich S, Parbel S, Vlaho S, Matsika O, Bohles H. N-carbamylglutamate protects patients with decompensated propionic aciduria from hyperammonaemia. J Inherit Metab Dis. 2005;28(2):241–4. https://doi.org/10.1007/s10545-005-5260-7.
Jones S, Reed CA, Vijay S, Walter JH, Morris AA. N-carbamylglutamate for neonatal hyperammonaemia in propionic acidaemia. J Inherit Metab Dis. 2008;31(Suppl. 2):S219–22. https://doi.org/10.1007/s10545-008-0777-1.
Lévesque S, Lambert M, Karalis A, Melancon S, Russell L, Braverman N. Short-term outcome of propionic aciduria treated at presentation with N-carbamylglutamate: a retrospective review of four patients. JIMD Rep. 2012;2:97–102. https://doi.org/10.1007/8904_2011_54.
Schwahn BC, Pieterse L, Bisset WM, Galloway PG, Robinson PH. Biochemical efficacy of N-carbamylglutamate in neonatal severe hyperammonaemia due to propionic acidaemia. Eur J Pediatr. 2010;169(1):133–4. https://doi.org/10.1007/s00431-009-1036-7.
Ah Mew N, Cnaan A, McCarter R, et al. Conducting an investigator-initiated randomized double-blinded intervention trial in acute decompensation of inborn errors of metabolism: lessons from the N-Carbamylglutamate Consortium. Transl Sci Rare Dis. 2018;3(3–4):157–70. https://doi.org/10.3233/TRD-180031.
Acknowledgements
We thank Roshini Vara, from Guy’s and St. Thomas’ Hospital NHS Foundation Trust, London, UK, for her contribution to this manuscript. We also thank Simone Tait and Alma Orts-Sebastian of Springer Healthcare Communications who wrote the outline and first draft of this manuscript, respectively, and Kate Palmer, also of Springer Healthcare Communications, who assisted with post-submission revisions. This medical writing assistance was funded by Recordati Rare Diseases.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study, medical writing assistance and the open access fee were funded by Recordati Rare Diseases. The funding source was involved in the writing of the manuscript.
Conflicts of Interest/Competing Interests
Sufin Yap has received funding for conferences and honorarium for lectures, master classes, advisory boards and ‘meet the expert’ sessions from Recordati Rare Diseases; and honorarium for expert advice from OpenVie. Vincenzo Giordano is an employee of Recordati Rare Diseases. Delphine Lamireau, Francois Feillet, Angeles Ruiz Gomez, James Davison, and Trine Tangeraas have no conflicts of interest that are directly relevant to the content of this article.
Ethics Approval
The study is being conducted in accordance with the ethical standards of the institutional and/or national research committees at each centre and with the 1964 Declaration of Helsinki, as revised in 2013. The study protocol has been approved by the local institutional review board at each study site.
Consent to Participate
Written informed consent is being collected from all participants or their caregivers before initiating the study.
Consent for Publication
Not applicable.
Availability of Data and Material
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Code Availability
Not applicable.
Authors’ Contributions
SY, DL, FF, ARG, JD and TT enrolled patients and contributed to the interpretation of the results, and VG contributed to the study design and interpretation of the results. All authors reviewed and revised the manuscript for important intellectual content, approved the version to be published, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yap, S., Lamireau, D., Feillet, F. et al. Real-World Experience of Carglumic Acid for Methylmalonic and Propionic Acidurias: An Interim Analysis of the Multicentre Observational PROTECT Study. Drugs R D 24, 69–80 (2024). https://doi.org/10.1007/s40268-023-00449-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-023-00449-z