Abstract
Background
Evidence is lacking for cognitive enhancer therapy in patients with Alzheimer’s disease (AD) and concomitant cerebrovascular disease (mixed AD) as such patients would have been excluded from clinical trials. Earlier studies of mixed AD have focused on large vessel cerebrovascular disease. The influence of small vessel cerebrovascular disease (svCVD) in the form of white matter hyperintensity (WMH) on treatment outcomes in mixed AD has not been addressed.
Objective
In this long-term naturalistic study, we evaluated the effectiveness of cognitive enhancers in patients with mixed AD with svCVD.
Methods
We conducted a retrospective analysis of a prospective clinical database from a memory clinic of a tertiary hospital. Magnetic resonance imaging WMH was used as a marker of svCVD. Demographic, cognitive, and treatment data were analysed. Linear mixed models with patient-specific random effects were used to evaluate cognitive outcomes over time while adjusting for confounders.
Results
Patients with mixed AD (n = 137) or AD without svCVD (pure AD) (n = 28) were studied over a median duration of 28.7 months. Patients with mixed AD had a higher prevalence of hypertension (62.8 vs. 35.7 %, p = 0.011). The majority (75.2 %) of the study sample were managed with monotherapy. Mini Mental State Examination (MMSE) scores decreased over time (−0.04, p = 0.007), and the decrease was similar for both diagnosis groups (−0.03, p = 0.246). Annual estimated mean MMSE decline was 0.84 for pure AD and 0.48 for mixed AD. Similar trends were observed with Montreal Cognitive Assessment (MoCA) scores, with annual estimated mean reduction of 0.72 and 0.48 for pure AD and mixed AD, respectively.
Conclusion
Cognitive enhancers are effective in slowing the rate of cognitive decline in patients with AD with svCVD. These findings would need to be confirmed in randomized clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cognitive enhancers demonstrate long-term benefit in the treatment of mixed Alzheimer’s disease (AD) and cerebrovascular disease |
Among cerebrovascular diseases, the small vessel subtype may demonstrate greater benefit with cognitive enhancers |
Randomized clinical trials of AD patients with small vessel cerebrovascular disease are urgently needed in view of the high prevalence of small vessel cerebrovascular disease in AD |
1 Introduction
Alzheimer’s disease (AD) is a major cause of dementia, with a global prevalence of 3.9 % in people older than 60 years [1]. The failure of anti-amyloid clinical trials necessitates exploration of other biological factors that can potentially delay the onset and progression of AD [2]. Cerebrovascular disease can modify the clinical expression and treatment response in AD [3].
Small vessel cerebrovascular disease (svCVD) is prevalent among patients with AD, resulting in mixed AD [4, 5]. On neuroimaging, AD patients with svCVD will demonstrate white matter hyperintensity (WMH) and lacunes [6]. WMH has been strongly associated with other markers of vascular disease [7, 8], greater cognitive impairment in AD, and higher risk of progression from mild cognitive impairment to AD [9–11]. The Honolulu-Asia Aging Study has demonstrated the role of co-prevalent brain lesions such as amyloid pathology, brain atrophy, and microvascular infarcts in AD, hence the importance of recognizing and treating patients with AD and svCVD [12].
Cholinergic dysfunction is well recognized in AD, and acetylcholinesterase inhibitors have shown benefit on cognitive and functional outcomes in AD [13–16]. Similarly, WMH has been shown to impair cholinergic function in the brain [17]. The combined effect of AD pathology and WMH on cerebral cholinergic function is likely to be greater than the individual effects of each of the two pathologies [18]. We thus postulate that AD patients with svCVD (mixed AD) will demonstrate greater cognitive benefit with cognitive enhancers. In this study, we compared the effectiveness of cognitive enhancers between AD patients with and without svCVD in a real-world tertiary clinic setting.
2 Methods
2.1 Study Design and Study Sample
The study was a retrospective review of a prospective electronic clinical database of dementia patients with data on diagnosis, treatment, follow-up (monitoring), and cognitive and functional outcomes. The study was approved by the Institutional Review Board.
The study sample included outpatients from a tertiary dementia clinic, who were enrolled between January 2006 and July 2013. Sociodemographic, clinical (including use of cognitive enhancers), and outcome information on these patients were recorded on our medical electronic database. We focused primarily on cognitive outcomes, and considered the cognitive enhancers acetylcholinesterase inhibitors and N-methyl-d aspartate (NMDA) antagonists.
We queried the database for all dementia outpatients who satisfied the following inclusion criteria: diagnosis of mild to moderate AD based on Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision (DSM-IV TR) criteria [19], clinical dementia rating (CDR) of 1–2 [20], availability of neuroimaging data and Mini-Mental State Examination (MMSE) score [21], and treatment with cognitive enhancers for at least 6 months. Patients who had a break in the use of cognitive enhancers for more than 3 months were excluded from the study.
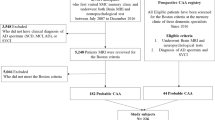
Of 951 dementia patients seen from January 2006 to July 2013, a total of 165 eligible patients were identified. Of these, 137 (83 %) patients had mixed AD (AD + svCVD) and 28 (17 %) patients had AD without svCVD (pure AD) (Fig. 1).
2.2 Measurements
AD was diagnosed based on the DSM-IV TR criteria. The presence of WMH on brain magnetic resonance imaging (MRI) was used as a surrogate marker for svCVD. WMH were semi-quantitatively rated using the modified-Fazekas scale on T2-weighted MRI images by an experienced clinician [22]. Periventricular WMH (pv-WMH) was graded as 0 = absence, 1 = ‘caps’ or thin lining, 2 = ‘halo’, and 3 = irregular pv-WMH extending into the white matter. Deep subcortical WMH (dsc-WMH) was rated as 0 = absence, 1 = punctuate foci, 2 = confluent foci and 3 = large confluent areas. Total score was obtained by the summation of pv-WMH and dsc-WMH in the right and left hemispheres for a total score of 12. AD patients with a total WMH score of ≥6 points were classified as mixed AD, and pure AD otherwise.
Patients were receiving either donepezil (5–10 mg/day), rivastigmine (oral 3–12 mg/day or patch 4.6–9.8 mg/day), galantamine (8–24 mg/day), or memantine (10–20 mg/day), or a combination of these cognitive enhancers. Cognitive outcomes were routinely assessed during each clinic visit using the MMSE, Montreal Cognitive Assessment (MoCA), and Geriatric Depression Scale (GDS) [23, 24]. MMSE and MoCA were used as the primary outcomes of this study. These endpoints were used to estimate the severity of cognitive impairment at ‘baseline’ and to follow the course of cognitive changes over time. We defined ‘baseline’ as the first time a patient was diagnosed or assessed at our institution.
2.3 Statistical Methods
Summary tables were used to describe the frequency and proportion of patients, as well as mean or median of sociodemographic and clinical characteristics and outcomes, by diagnostic groups (mixed AD and pure AD). Line plots were used to depict the evolution of outcomes over time, at the patient level and the diagnostic group level. The two-sample t-test and Kruskal–Wallis test were used to compare means and medians, respectively, of continuous variables between diagnosis groups. Fisher’s exact test was used to test associations between categorical variables and diagnosis groups.
Linear mixed models (LMM) with patient-specific random effects were used to evaluate the evolution of the outcomes over time while accommodating the dependence in the data, due to repeated assessments of each patient over time; identifying and adjusting for potential confounders; and accounting for missingness in the data [25–27]. Results from LMM were valid under the missing at random missingness assumption, which implied that, conditional on the observed data, the missingness was independent of the unobserved assessments [28, 29]. Patient-specific random effects and an unstructured (general) variance-covariance matrix were used to account for the differences in number of assessments as well as duration between assessments, between patients.
First, a ‘base-model’ was developed based on diagnosis group, follow-up time, and patient-specific random effects only. Second, each sociodemographic and clinical characteristic was added separately to the base model in order to identify potential confounders. We henceforth refer to such models as univariable models. Third, a final model was developed by adding all potential confounders simultaneously to the base model, henceforth referred to as multivariable models. Medication was considered as a time varying covariate in the univariable and multivariable models. Appropriate mixture of Chi-squared tests were used to test the variances of the patient-specific random effects [26, 27].
The significance level was set at 5 % and all tests were two-sided. SAS version 9.2 software (SAS Institute, Cary, NC, USA) was used for the analyses.
3 Results
3.1 Baseline Characteristics
A total of 165 patients (137 [83 %] mixed AD patients and 28 [17 %] pure AD patients), met the study eligibility criteria, of whom 140 (84.8 %) were Chinese and 70 (42.4 %) were male. At baseline, the median age was 73 years; the median years of education was 6 years; the prevalence of diabetes, hypertension, and hyperlipidemia was 26.1, 58.2 and 57.9 %, respectively; the mean GDS score was 3.1 (standard deviation [SD] 3.2); the mean MMSE score was 20.6 (SD 5.4); and the mean MoCA score was 20.9 (SD 5.0). The mean WMH in the pure AD group was 1.8 (SD 3) and that for AD + svCVD was 8.1 (SD 3.4).
Table 1 summarizes the baseline characteristics by diagnosis group. Compared with patients with mixed AD, patients with pure AD were younger (8 years, p = 0.001), had more years of education (3 years, p = 0.019), and had a lower prevalence of hypertension (27.1, p = 0.011). Patients with mixed AD performed significantly worse (20.1 vs. 23.0, p = 0.007) on the MMSE. The mixed AD group had lower baseline scores on the MoCA, but this was not statistically different (20.5 vs. 22.5, p = 0.142).
3.2 Follow-up Characteristics
Patient management (treatment, monitoring, and assessment) was reviewed, and adjusted if necessary, routinely within 4–6 months of the previous clinic visit. The relationship between duration of follow-up and number of assessments was influenced by our practice as well as patient compliance with their clinic appointments. Consequently, the number of assessments and the duration between repeated assessments within patients were not fixed.
The median duration of follow-up of the eligible sample was 28.7 months (range 5–85). The duration of follow-up in the mixed AD group (median 28.2 months; range 5–85) was not significantly different to that of the pure AD group (median 36.0 months; range 8–82), although it was slightly longer for the pure AD group on average. The median number of assessments per patient was six (range 2–10) and was slightly higher, on average, for the pure AD group, possibly owing to the slightly longer follow-up (Table 1).
3.3 Use of Cognitive Enhancers
Overall, i.e. based on the number of patients who received any of the cognitive enhancers considered at least once, the most commonly used cognitive enhancer was rivastigmine in patch or oral form (57.6 %), followed by donepezil (37.0 %), memantine (20.0 %), and galantamine (13.3 %). Rivastigmine was the most prescribed first-line treatment, whereas galantamine and memantine were the most prescribed second-line treatments. The same pattern of prescription was observed for both mixed AD and pure AD groups.
The majority (75.2 %) of the study sample were managed based on monotherapy with a cognitive enhancer, while the cognitive enhancer for some patients was switched once (21.8 %) or twice (3.0 %). The median time to the first switch of cognitive enhancers, mostly due to intolerance or side effects, was 4.8 months (range 0.5–30). Patients with mixed AD had a slightly longer median time to first switch (5.2 months [range 1–30]) than patients with pure AD (3.0 months [range 0.5–7]) (Table 2).
3.4 Outcomes
Loess line plots of MMSE and MoCA scores over time by diagnosis groups indicated the plausibility of an average linear profile over time (Fig. 2b, d). Similarly, patient level loess line plots of MMSE and MoCA scores over time indicated an approximate linear profile over time (Fig. 2a, c). Thus a base model was specified with the following fixed effects: of diagnosis group (pure AD) with mixed AD as the reference group, follow-up duration (FDur), interaction between diagnosis group and duration of follow-up (pure AD × FDur). The random effects consisted of patient-specific intercepts and slopes as well as a residual variance. The variance of the random intercept, D(1,1), represented the degree of variability of patients’ cognitive impairment at baseline, while the variance of the random slope, D(2,2), indicated whether response to management over time was similar (small) or variable (large) between patients. The covariance (correlation) between the patient-specific intercept and slope indicated whether the evolution of patients’ cognitive impairment over time was related to their condition at baseline. Higher order (quadratic and cubic) models were considered at both the fixed- and random-effects level and Akaike’s information criteria (AIC) indicated that the linear model was acceptable (Table 3) [30].
LOESS line plots of cognitive outcomes over time by randomly selected patients and diagnosis groups: a patient-level evolution of MMSE, b average evolution of MMSE by diagnosis group, c patient-level evolution of MoCA, and d average evolution of MoCA by diagnosis group. AD Alzheimer’s disease, MMSE Mini-Mental State Examination, MoCA Montreal Cognitive Assessment, svCVD small vessel cerebrovascular disease
‘Years of education’ was the only confounder with significance on the MMSE, as well as the MoCA scores. Based on MMSE, pure AD patients seemed to be less cognitively impaired at baseline (2.36, p = 0.023), but this difference was not significant in the multivariable analysis after adjusting for years of education (1.48, p = 0.156). There was a slight decrease in MMSE scores over time (−0.04, p = 0.007), and the decrease over time was similar for both diagnosis groups (−0.03, p = 0.246). The annual estimated mean reduction of MMSE score was less than 1 for both the pure AD (0.84) and the mixed AD (0.48) groups. Similar trends were observed based on the MoCA scores, with annual estimated mean reduction of 0.72 and 0.48 for pure AD and mixed AD groups, respectively (Table 3).
For both MMSE and MoCA scores, the variance of the patient-specific intercept was ‘large’ (>20), indicating that the severity of cognitive impairment at baseline varied substantially from patient to patient. This was expected in data obtained from clinical practice, unlike randomized controlled trial data. The small variances of the patient-specific slopes indicated that the reduction in cognition over time was similar from patient to patient, and the reduction in cognition did not depend on the severity of cognitive impairment at baseline, as indicated by the small covariances between the patient-specific intercepts and slopes. These trends were similar for the base, univariable, and multivariable models.
4 Discussion
In our study of a clinical cohort of patients with AD, we found that cognitive enhancers are effective in slowing the rate of cognitive decline in both patients with pure AD and those with mixed AD. Importantly, there was a trend to greater cognitive benefit, characterized by a slower rate of cognitive decline in patients with mixed AD than in those with pure AD. The results remain significant even after adjusting for years of education and inherent variability in the severity of cognitive decline between patients.
Both the MMSE and MoCA demonstrated a trend towards cognitive benefit for patients with mixed AD when treated with cognitive enhancers. MMSE and MoCA were both validated for screening and monitoring of AD, with the MoCA found to be a better cognitive tool than MMSE [31]. The MoCA had also been shown to reveal higher sensitivity to cognitive decline in longitudinal monitoring. The MMSE and MoCA score changes showed similar trends during the follow-up period (Fig. 2), suggesting a robust benefit when patients with mixed AD were treated with cognitive enhancers. As clinical trials with cognitive enhancers in AD only include patients with probable AD, effectively excluding AD patients with concomitant svCVD, this real-life study from a clinic cohort for the first time provided direct evidence for benefit when patients with mixed AD with svCVD were treated with cognitive enhancers.
A previous longitudinal study of AD showed that the annual rate of cognitive decline based on MMSE scores was 2.3 without treatment with cognitive enhancers [32]. A review of cholinesterase inhibitors for AD showed that MMSE mean change from baseline to 6 months ranged from −0.5 to 1.35 [33]. In this current study, we demonstrated in a long-term real-life clinic study that, with cognitive enhancers, the average annual decline in MMSE scores was 0.84 for patients with pure AD and 0.48 for patients with AD + svCVD. The change of −0.84 for pure AD is in keeping with previous literature. More importantly, we demonstrated that patients with mixed AD of the svCVD category showed less annual cognitive decline when treated with cognitive enhancers.
Patients with long-standing hypertension have been shown to have increased rates of white matter lesions, both periventricular and subcortical, while hyperlipidemia had been associated with less severe WMH [34, 35]. In our cohort, cardiovascular risk factors were more prevalent, significantly so for hypertension, in mixed AD patients than in pure AD patients, which is consistent with current literature.
WMH has been associated with greater cognitive impairment in AD [10]. The baseline MMSE scores of our patients with mixed AD were significantly lower than those of the pure AD patients (20.1 vs. 23), although this significance disappeared after adjusting for years of education in the multivariable analysis. Interestingly, there were no sharp changes in MMSE scores over the period of follow-up, and the baseline MMSE scores did not influence the progression of MMSE scores.
Cholinergic dysfunction has been well described in AD [13]. In vivo imaging studies provided supportive evidence that periventricular white matter lesions were associated with cortical cholinergic deafferentation in elderly patients with leukoaraiosis [17]. CVD may directly affect cholinergic white matter projections and may exacerbate pre-existing cholinergic deficits in AD [36]. The presence of periventricular WMH is also significantly associated with lower cortical cholinergic activity, supporting a regionally specific disruption of cholinergic projection fibers by WMH [37]. The cognitive benefit seen in our analysis confirmed the presence of cholinergic dysfunction in both patients with pure AD and those with mixed AD. The greater cognitive benefit seen in patients with AD + svCVD supported our hypothesis that the combined effect of AD pathology and WMH resulted in greater cholinergic dysfunction.
The key strengths of our study was the length of follow-up of our patients; the median duration of follow-up for mixed AD and pure AD was 28.2 and 36 months, respectively. Furthermore, our study was a naturalistic study on outcomes of cognitive enhancers in AD that aimed to describe results from treatment in patients who were treated by usual care. Naturalistic studies mirrored naturalistic outpatient settings and so served a complementary role to more structured efficacy trials and pragmatic studies of AD. The study also has several limitations: this was a retrospective study without randomization of cognitive enhancer assignment and no control for prestudy exposure to other medications. The results were findings from a single center with the types of cognitive enhancers used representing the practice in our center. However, this practice was based on evidence of cognitive enhancers that were shown to delay cognitive impairment in patients with mild to moderately severe AD, with no robust support for any one drug [14]. Patients with AD + svCVD were over-represented in our sample, which may reduce the generalizability of our findings. Hence, these findings should be confirmed in independent samples with adequate representation of patients with ‘pure AD’ and ‘AD + svCVD’.
5 Conclusion
Cholinergic dysfunction is present in both AD and mixed AD of the svCVD category. Cognitive enhancers are effective in slowing the rate of cognitive decline in patients with AD, and seemingly more so for patients with mixed AD of the svCVD category. The finding of potential benefit of cognitive enhancer therapy for patients with AD + svCVD will need to be confirmed in randomized clinical trials.
References
Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366(9503):2112–7.
Salomone S, Caraci F, Leggio GM, Fedotova J, Drago F. New pharmacological strategies for treatment of Alzheimer’s disease: focus on disease modifying drugs. Br J Clin Pharmacol. 2012;73(4):504–17.
Honjo K, Black SE, Verhoeff NP. Alzheimer’s disease, cerebrovascular disease, and the beta-amyloid cascade. Can J Neurol Sci. 2012;39(6):712–28.
Lim A, Tsuang D, Kukull W, Nochlin D, Leverenz J, McCormick W, et al. Clinico-neuropathological correlation of Alzheimer’s disease in a community-based case series. J Am Geriatr Soc. 1999;47(5):564–9.
Massoud F, Devi G, Stern Y, Lawton A, Goldman JE, Liu Y, et al. A clinicopathological comparison of community-based and clinic-based cohorts of patients with dementia. Arch Neurol. 1999;56(11):1368–73.
Pohjasvaara T, Mantyla R, Ylikoski R, Kaste M, Erkinjuntti T. Clinical features of MRI-defined subcortical vascular disease. Alzheimer Dis Assoc Disord. 2003;17(4):236–42.
Debette S, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ (Clin Res Ed). 2010;341:c3666.
DeCarli C, Murphy DG, Tranh M, Grady CL, Haxby JV, Gillette JA, et al. The effect of white matter hyperintensity volume on brain structure, cognitive performance, and cerebral metabolism of glucose in 51 healthy adults. Neurology. 1995;45(11):2077–84.
Brickman AM, Provenzano FA, Muraskin J, Manly JJ, Blum S, Apa Z, et al. Regional white matter hyperintensity volume, not hippocampal atrophy, predicts incident Alzheimer disease in the community. Arch Neurol. 2012;69(12):1621–7.
Carmichael O, Schwarz C, Drucker D, Fletcher E, Harvey D, Beckett L, et al. Longitudinal changes in white matter disease and cognition in the first year of the Alzheimer disease neuroimaging initiative. Arch Neurol. 2010;67(11):1370–8.
Prasad K, Wiryasaputra L, Ng A, Kandiah N. White matter disease independently predicts progression from mild cognitive impairment to Alzheimer’s disease in a clinic cohort. Dement Geriatr Cognit Disord. 2011;31(6):431–4.
White L, Petrovitch H, Ross GW, Masaki KH, Abbott RD, Teng EL, et al. Prevalence of dementia in older Japanese-American men in Hawaii: The Honolulu-Asia Aging Study. JAMA. 1996;276(12):955–60.
Kalaria RN, Ballard C. Overlap between pathology of Alzheimer disease and vascular dementia. Alzheimer disease and associated disorders. 1999;13 Suppl 3:S115–23.
Takeda A, Loveman E, Clegg A, Kirby J, Picot J, Payne E, et al. A systematic review of the clinical effectiveness of donepezil, rivastigmine and galantamine on cognition, quality of life and adverse events in Alzheimer’s disease. Int J Geriatr Psychiatry. 2006;21(1):17–28.
Gauthier S, Juby A, Morelli L, Rehel B, Schecter R. A large, naturalistic, community-based study of rivastigmine in mild-to-moderate AD: the EXTEND Study. Curr Med Res Opin. 2006;22(11):2251–65.
Santoro A, Siviero P, Minicuci N, Bellavista E, Mishto M, Olivieri F, et al. Effects of donepezil, galantamine and rivastigmine in 938 Italian patients with Alzheimer’s disease: a prospective, observational study. CNS Drugs. 2010;24(2):163–76.
Bohnen NI, Bogan CW, Muller ML. Frontal and periventricular brain white matter lesions and cortical deafferentation of cholinergic and other neuromodulatory axonal projections. Eur Neurol J. 2009;1(1):33–50.
Kim HJ, Moon WJ, Han SH. Differential cholinergic pathway involvement in Alzheimer’s disease and subcortical ischemic vascular dementia. J Alzheimers Dis. 2013;35(1):129–36.
American Psychiatric A. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington D.C: American Psychiatric Association; 2003.
Morris JC. Clinical dementia rating: a reliable and valid diagnostic and staging measure for dementia of the Alzheimer type. Int Psychogeriatr. 1997;9 Suppl 1:173–6; discussion 177–8.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987;149(2):351–6.
Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9.
Parmelee PA, Katz IR. Geriatric depression scale. J Am Geriatr Soc. 1990;38(12):1379.
Fitzmaurice G, Davidian M, Verbeke G, Molenberghs G. Longitudinal data analysis. London: Taylor & Francis; 2008.
Molenberghs G, Verbeke G. Models for discrete longitudinal data. Springer Science + Business Media, Incorporated; 2006.
Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. Textstream; 2000.
Allison PD. Missing data. Thousand Oaks: SAGE Publications; 2001.
Little RJA, Rubin DB. Statistical analysis with missing data: New York: Wiley; 2002.
Bozdogan H. Model selection and Akaike’s Information Criterion (AIC): the general theory and its analytical extensions. Psychometrika. 1987;52(3):345–70.
Freitas S, Simoes MR, Alves L, Santana I. Montreal cognitive assessment: validation study for mild cognitive impairment and Alzheimer disease. Alzheimer Dis Assoc Disord. 2013;27(1):37–43.
Suh GH, Ju YS, Yeon BK, Shah A. A longitudinal study of Alzheimer’s disease: rates of cognitive and functional decline. Int J Geriatr Psychiatry. 2004;19(9):817–24.
Birks J. Cholinesterase inhibitors for Alzheimer’s disease. Cochrane Database Syst Rev. 2006(1):CD005593.
de Leeuw FE, de Groot JC, Oudkerk M, Witteman JC, Hofman A, van Gijn J, et al. Hypertension and cerebral white matter lesions in a prospective cohort study. Brain J Neurol. 2002;125(Pt 4):765–72.
Warsch JR, Wright CB. Stroke: hyperlipidemia and cerebral small-vessel disease. Nat Rev Neurol. 2010;6(6):307–8.
Swartz RH, Sahlas DJ, Black SE. Strategic involvement of cholinergic pathways and executive dysfunction: Does location of white matter signal hyperintensities matter? J Stroke Cerebrovasc Dis. 2003;12(1):29–36.
Bohnen NI, Muller ML, Kuwabara H, Constantine GM, Studenski SA. Age-associated leukoaraiosis and cortical cholinergic deafferentation. Neurology. 2009;72(16):1411–6.
Acknowledgment
The research was supported by the National Neuroscience Institute, Singapore.
Author Contributions
Ng Kok Pin contributed to the study design, interpretation of data, drafting/revising of the manuscript for intellectual content and gave final approval.
Aloysius Ng contributed to the acquisition of data, statistical analysis, interpretation of the data, drafting/revising of the manuscript for intellectual content and gave final approval.
Pryseley Assam contributed to the statistical analysis, interpretation of results, drafting/revising the manuscript for intellectual content and gave final approval.
Esther Heng contributed to the acquisition of data, statistical analysis, interpretation of data and gave final approval.
Nagaendran Kandiah contributed to the study design, statistical analysis, interpretation of the data, drafting/revising of the manuscript and gave final approval.
Conflict of Interest Disclosures
Ng Kok Pin reports no conflict of interest. Aloysius Ng reports no conflict of interest. Pryseley Assam reports no conflict of interest. Esther Heng reports no conflict of interest. Nagaendran Kandiah has received honorarium and CME sponsorship from Lundbeck, Novartis, Medichem, Pfeizer and Eisai. He has also received research funding from Singhealth Foundation, Media Development Authority of Singapore, National Medical Research Council of Singapore and Biomedical Research Council of Singapore. Ng Kok Pin, Aloysius Ng, Pryseley Assam, Esther Heng, and Nagaendran Kandiah had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Ng, K.P., Ng, A., Assam, P. et al. Role of Cognitive Enhancer Therapy in Alzheimer’s Disease with Concomitant Cerebral White Matter Disease: Findings from a Long-Term Naturalistic Study. Drugs R D 14, 195–203 (2014). https://doi.org/10.1007/s40268-014-0057-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-014-0057-5