Abstract
Purpose
A randomized, double-masked, multicenter, phase 2 trial to evaluate the long-term safety and efficacy of travoprost intraocular implant, an extended-release drug delivery system designed to provide uninterrupted sustained intraocular pressure (IOP)-lowering therapy, thereby reducing patient treatment burden and improving adherence with IOP-lowering medication.
Methods
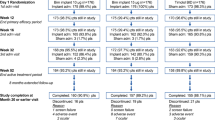
Patients with open-angle glaucoma or ocular hypertension were administered a fast-eluting implant (FE implant, n = 51) and received twice-daily (BID) placebo eye drops, a slow-eluting (SE implant, n = 54) and received BID placebo eye drops, or underwent a sham surgical procedure and received BID timolol 0.5% (n = 49). IOP was measured at baseline, day 1–2, day 10, week 4, week 6, month 3, and every 3 months thereafter through 36 months. Efficacy was evaluated by mean change from 8:00 AM unmedicated baseline IOP through month 36, and the percentage of patients receiving the same or fewer topical IOP-lowering medications as at screening (pre-study). Safety was evaluated by adverse events and ophthalmic parameters.
Results
Clinically and statistically relevant IOP-lowering treatment effects were observed through month 36 after a single administration of the travoprost implant compared with BID timolol with mean IOP reductions ranging from 7.6 to 8.8 mmHg for the FE implant group, from 7.3 to 8.0 mmHg for the SE implant group, and from 7.3 to 7.9 for the timolol group at the 8:00 AM timepoint (P < 0.0001 for all treatment groups at all visits). At months 12, 24, and 36, a greater percentage of FE and SE implant patients versus timolol patients were well controlled on the same or fewer topical IOP-lowering medications compared with screening with 63 and 69% for the FE and SE implants groups, respectively, versus 45% for the timolol group at month 36. The safety profile of the implant was favorable; there were no dislodgements, no explantations, no adverse events of conjunctival hyperemia or periorbital fat atrophy, no discontinuations due to study eye adverse events, nor any serious adverse events in the study eye. Comparable changes from baseline in corneal endothelial cell counts were observed in the three treatment groups over the 36 months.
Conclusion
The travoprost intraocular implant demonstrated robust IOP-lowering and substantially reduced topical IOP-lowering medication burden for up to 36 months following a single administration, while maintaining a favorable safety profile. The travoprost intraocular implant promises to be a meaningful addition to the interventional glaucoma armamentarium by addressing the key shortcomings of topical IOP-lowering medications, including low adherence and topical side effects while controlling IOP for up to 36 months.
Trial Registry
ClinicalTrials.gov identifier NCT02754596 registered 28 April 2016.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The travoprost intraocular implant (fast-eluting and slow-eluting models) effectively reduced intraocular pressure in patients with open-angle glaucoma or ocular hypertension. |
At month 36, 63% (fast eluting) and 69% (slow eluting) of implant patients reduced or maintained their topical medication burden relative to pre-study medications. |
The safety profile of the travoprost intraocular implant was favorable over the 36 month study. |
1 Introduction
Glaucoma therapies have improved and diversified; however, the treatment burden and the loss of vision due to this disease remains high, causing decreased quality of life and more irreversible blindness than any other ocular disease worldwide [1]. Intraocular pressure (IOP) is the only known modifiable risk factor, and numerous landmark glaucoma studies have established the vital role of IOP lowering in decreasing glaucoma development and progression [2,3,4,5,6,7,8]. Currently available glaucoma treatments include topical and oral medications, laser procedures, micro-invasive glaucoma surgery (MIGS), and/or more invasive procedures such as minimally invasive bleb-forming surgery (MIBS), traditional filtration surgery (e.g., trabeculectomy or tube shunt), or laser cilioablation. Pharmacotherapy with topical medications remains the primary means of treating patients with mild-to-moderate open-angle glaucoma (OAG) and ocular hypertension (OHT). Among medications, topical prostaglandin analogs (PGAs) are the most commonly used first-line glaucoma treatment [9], with proven effectiveness, safety, and ability to prevent visual field loss [10].
Despite these positive attributes, topical medications such as PGAs have a number of drawbacks such as poor adherence and ocular side effects, which may negatively impact both their effectiveness and patients’ quality of life. Patient adherence with eye drops is poor, and worsens in proportion to increased medication burden in terms of both number of bottles and frequency of dosing [11,12,13,14]. Approximately half of patients on no-cost travoprost as monotherapy take fewer than three-quarters of the prescribed doses [15,16,17]. Moreover, greater than 90% of patients do not refill their prescriptions for topical glaucoma medications uninterruptedly over a period of 3 years [11]. Medication adherence declines dramatically when more than one medication is prescribed [18,19,20]. Other factors resulting in patients’ nonadherence with treatment may include physical and cognitive difficulties with administering eye drops, especially in an elderly population. Prior studies have demonstrated that glaucoma patients require an average of 1.4–1.8 drops to successfully instill one drop of medication on the eye [21], and approximately one-third of patients are persistently unable to get drops onto the eye [22]. Poor medication adherence is correlated with worsened disease prognosis and higher risk of blindness [23,24,25,26].
Chronic topical medication usage has consistently been shown to have a detrimental effect on patient quality of life due to several potential factors, including symptoms of ocular surface disease (OSD), adherence-related concerns, cosmetic side effects, caregiving needs, and lifestyle burden of frequent drop instillation and associated perception of overall health [27,28,29,30,31,32,33]. Topical glaucoma agents and their benzalkonium chloride (BAK) preservatives can induce chronic conjunctival inflammation; OSD, including film instability and dry eye; and periocular side effects [34,35,36,37,38,39,40,41,42]. Higher numbers of drops and greater dosing frequency are both correlated with increasing side effects [29]. Chronic conjunctival inflammation can negatively impact drug tolerability, further reducing adherence and increasing the risk of subsequent glaucoma surgical failure [37, 39, 43]. Given the impact of medication burden on adherence, ocular surface health, and quality of life, any therapy designed to reduce the number of topical medications is of significant interest.
To overcome the drawbacks of topical IOP-lowering medications while still providing the eye with adequate levels of the active therapeutic agent, several extraocular and intraocular drug-delivery products have been proposed. Some examples of extraocular modalities have included a ring-type drug-eluting insert located in the fornix, a drug-eluting contact lens, drug-eluting punctal plugs, and nanoparticulate drug-delivery systems [44]. Although promising, these products generally have been plagued by poor retention, tolerability, cosmesis, and inferior IOP reduction, with most not reaching later stages of human testing [45, 46]. Regarding intraocular implants, the bimatoprost sustained release (SR) biodegradable intracameral implant (Durysta™, bimatoprost intracameral implant, 10 µg; Allergan Corp, Irvine, CA) was approved by the US Food and Drug Administration (FDA) in 2020 to reduce IOP in patients with OAG and OHT [47]. Durysta is an unanchored implant that was designed to be injected into the anterior chamber every 3–4 months [48]. The phase 3 data for the product showed IOP reductions of 5–8 mmHg from baseline over 15 weeks in patients with mean baseline IOP of 24.5 mmHg [49, 50].
Despite these promising findings, which show the potential of implantable drug-delivery products, the bimatoprost implant has several limitations. Due to the slow rate of bimatoprost implant biodegradation and the 3–4 month dosing interval in the clinical trials, multiple bimatoprost implants were observed to reside in the iridocorneal angle at the same time [49, 50]. The accumulation of polymer matrix from the bimatoprost implant in the iridocorneal angle has been hypothesized as one possible cause for the increased rate of corneal adverse events (e.g., endothelial cell loss, corneal edema) with each subsequent administration [49, 50]. As a result, the prescribing information for Durysta includes a warning that due to possible corneal endothelial cell loss, administration of Durysta should be limited to a single implant per eye without retreatment [47].
One of the recent entrants into the sustained release pharmacotherapy armamentarium, designed to address the shortcomings of topical IOP-lowering medications, is the travoprost intraocular implant (Glaukos Corp., Aliso Viejo, CA, USA). The implant aims to overcome the limitations of prior drug-delivery modalities in several ways: micro-scale size, which allows for a tissue-sparing, low-footprint presence in the angle and a fixed and stable intraocular position to eliminate implant mobility reducing the risk of contact with the corneal endothelium and other complications related to mobile implants. The travoprost intraocular implant is designed to continually elute travoprost in a gradual fashion over time. This elution profile eliminates the peaks and troughs of travoprost concentrations, thereby dampening peak IOP and minimizing IOP fluctuations that can predispose patients to progressive visual field damage [51,52,53,54]. Travoprost was selected as the active ingredient as it has a long history of safe and effective use and is more potent in binding to prostaglandin F2α receptors than other PGAs including latanoprost and bimatoprost [55]. Two models of the travoprost implant have been evaluated clinically: a fast-eluting travoprost intraocular implant (FE implant) and a slow-eluting travoprost intraocular implant (SE implant), with the results of this study helping to inform the decision to commercialize only the SE implant. The travoprost intraocular implant has also been evaluated for readministration, in which a new implant is administered and the previous implant with depleted travoprost is removed during the same entry into the anterior chamber.
The travoprost intraocular implant is a microscopic titanium container, measuring 1.84 mm in length (including the anchor) and 0.494 mm in outer diameter (Fig. 1a), which elutes travoprost through one of two versions of a thin membrane held in place with a titanium cap. Each implant was preloaded into a single-use biocompatible inserter which the surgeon advances ab internally across the anterior chamber to place the implant anchor through the trabecular meshwork into the scleral wall (Fig. 1b). The implant is thereby anchored into the sclera in the anterior chamber angle of the eye.
Travoprost intraocular implant inserter system. A safety clip holds the release button in the forward position during shipping, storage, and handling, thus preventing the premature release of the implant. The magnified view shows the inserter tip with grasper and a released implant (a). Anchored location of the travoprost intraocular implant in the anterior chamber angle of the eye (b)
The objective of the current study was to report on the 3 year safety of the implant, and percentage of patients who reduced or maintained their topical IOP-lowering medication burden relative to pre-study medications.
2 Methods
2.1 Study Design
This was a prospective, randomized, double-masked, sham-controlled, parallel-group, multicenter, phase 2 clinical trial (ClinicalTrials.gov identifier NCT02754596). The study evaluated the safety and IOP-lowering efficacy of two travoprost intraocular implants with different elution rates versus timolol eye drops (Timolol Maleate Ophthalmic Solution, USP, 0.5%) in patients with OAG or OHT.
Patients were enrolled from 15 March 2016 to 21 July 2020 at 23 sites in the USA and one site in the Philippines.
The study was performed in compliance with good clinical practice and the principles of the Declaration of Helsinki. Institutional review board (Western Institutional Review Board for sites in the USA and the St. Cabrini Medical Center—Asian Eye Institute Ethics Review Committee for the site in the Philippines) approval was obtained at each site before the study began, and all patients provided written informed consent before undergoing any study-related procedure.
2.2 Study Participants and Inclusion/Exclusion Criteria
A total of 154 patients, 18 years of age and older, diagnosed with OAG (primary, pseudoexfoliative, or pigmentary) or OHT, on 0–3 topical IOP-lowering medications were included. Patients were required to meet all inclusion criteria and none of the exclusion criteria to be eligible for participation. Key inclusion criteria included the ability to provide an adequate interpretable visual field with a mean deviation no worse than − 12 dB, a cup/disc ratio of ≤ 0.8, best-corrected visual acuity score of + 0.6 logMAR (Snellen equivalent of 20/80) or better in each eye, an open iridocorneal angle (Shaffer grade ≥ 3) with normal anatomy, and phakic or pseudophakic with a posterior chamber intraocular lens that had been implanted a minimum of 90 days prior to the screening visit. Phakic eyes were required to have a minimum corneal endothelial cell count between 1600 and 2000 cells/mm2 dependent on age, and pseudophakic eyes were required to have a minimum endothelial cell count between 1120 and 1540 cells/mm2 dependent on age. Additionally, female patients of childbearing potential were required to have a negative urine pregnancy test result at the screening visit and agree to use reliable birth control throughout the study.
Key exclusion criteria included glaucoma of traumatic, uveitic, or neovascular etiology or associated with a vascular disorder; prior glaucoma surgery including filtration surgery, incisional surgery, argon laser trabeculoplasty (ALT), iridectomy/iridotomy, or trabecular bypass or suprachoroidal procedures; a history of selective laser trabeculoplasty (SLT) within the prior 90 days; a visual field status that would place the patient at risk by being washed out of IOP-lowering medication(s); active corneal inflammation or edema; clinically significant corneal dystrophy or guttata; corneal thickness of < 440 microns or > 620 microns; presence of significant corneal scarring or irregularities that could interfere with reliable IOP measurement; corneal opacities or disorders that inhibited visualization of the nasal angle; congenital or traumatic cataract, or visually significant cataract that was likely to require surgical intervention during the study period; choroiditis, choroidal detachment, effusion, neovascularization, or any active choroidopathy; degenerative or evolutive retinal or optic nerve disorders (e.g., proliferative diabetic retinopathy, central retinal artery occlusion, central retinal vein occlusion, wet age-related macular degeneration, advanced dry age-related macular degeneration, significant retinal pigment epithelial changes, or optic atrophy). Additionally, patients were to be excluded if they had uncontrolled systemic disease (e.g., diabetes, hypertension) or an immunodeficiency disorder; used systemic medications (either current, within 30 calendar days of the screening visit, or anticipated) that may cause an increase in IOP [e.g., systemic steroids including oral or intravenous (IV) formulations, topical steroids applied on the periorbital surface within 1/4 inch of the external lid margins] or oral inhaled steroids; were unable to discontinue use of nonsteroidal anti-inflammatory medications (NSAIDs) (topical dermal NSAIDs were acceptable) or aspirin (any dosage) within 7 calendar days prior to surgery and for 1–2 days following surgery; or were unable to discontinue blood thinners for a period of 1–7 days dependent on the type of medication. Additionally, patients were to be excluded from participation if they used an oral carbonic anhydrase inhibitor (CAI); if they had a known allergy or hypersensitivity to the study medication or their components; used any ocular medications, other than IOP-lowering medications, within 1 week prior to the screening visit; and were not on a stable dosing regimen of chronic systemic therapy that could affect IOP within 30 days prior to the screening visit or anticipated a change in such therapy during the study duration.
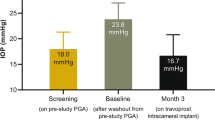
Patients on no IOP-lowering medications within the 4 weeks prior to the screening visit were required to have an IOP of 21–36 mmHg in the study eye, and then complete a 3 day waiting period and return for a baseline visit. Patients on IOP-lowering medications at the screening visit were required to stop their medication and undergo a washout period dependent on the class of medication: 5 days for miotics, 7 days for CAIs, 3 weeks for alpha adrenergic agonists, and 4 weeks for beta adrenergic antagonists and PGAs. A topical CAI could be substituted to replace a medication requiring a longer washout (e.g., PGA) provided that the CAI was stopped at least 7 days prior to the baseline visit.
At the baseline visit, all patients were required to have unmedicated mean diurnal IOP (average of the 8:00 AM, 10:00 AM, and 4:00 PM values) of 21–36 mmHg in the study eye and meet all other entry criteria.
2.3 Study Treatments and Postoperative IOP Management
Eligible patients were randomized 1:1:1 to one of the following three treatments: FE implant, SE implant, and timolol control group. The FE and SE implants were identical in size and appearance, which aided in masking.
To maintain postoperative masking, patients in both implant groups received a placebo topical ophthalmic solution (Advanced Eye Relief Dry Eye Rejuvenation; Bausch & Lomb, Bridgewater, NJ) to be administered twice daily (BID). Patients randomized to the control group underwent a sham surgical procedure before receiving masked timolol maleate ophthalmic solution, 0.5% to be administered BID. Following implantation of the travoprost intraocular implant or sham surgery, all patients were given fluoroquinolone antibiotic eye drops to be administered four times daily for 1 week and topical NSAID eye drops to be used in accordance with the prescribing information. The fellow eye was maintained on pre-study IOP-lowering medication(s).
From week 4 onward, additional topical IOP-lowering therapy was to be initiated in any study eye in which IOP exceeded 18 mmHg.
2.4 Assessments
Following the surgical or sham procedure, patients were evaluated at day 1–2, day 10, week 4, and week 6, as well as at month 3, 6, 9, 12, 15, 18, 21, 24, 27, 30, 33, and 36 visits. IOP was measured at 8:00 AM ± 30 minutes at all study visits, with the exception of the day 10, week 6, and month 3 study visits at which diurnal assessments were collected at 8:00 AM ± 30 min, 10:00 AM ± 30 min, and 4:00 PM ± 30 min. IOP was measured by Goldmann applanation tonometry using a two-person technique in which one person unmasked to treatment viewed through the slit lamp and turned the dial, while the second person masked to treatment recorded the measurements.
Additional assessments included measurement of visual acuity (VA), slit lamp examination (of the cornea, anterior chamber, iris, pupil, and lens), gonioscopy, dilated fundus examination (including vertical cup/disc ratio), computerized perimetry, specular microscopy, and pachymetry.
Conjunctival hyperemia was assessed at the slit lamp and graded on a five-point scale (normal, trace, mild, moderate, severe) by comparison to a photographic images, iris color was evaluated for any changes in pigmentation, the periorbital region was assessed to detect PGA-associated periorbitopathy, and the eyelashes were assessed for density and length.
Adverse events were both solicited and based on observations, with any clinically significant worsening from baseline in a parameter reported as an adverse event.
2.5 Study Measures and Data Analysis
Safety outcomes included surgical complications and adverse events, best-corrected VA (BCVA), gonioscopy, ophthalmoscopy (including cup/disc ratio), central corneal thickness, conjunctival hyperemia, visual field, slit lamp biomicroscopy, endothelial cell density, and periorbital or eyelash changes.
The sample size of this phase 2 study was not determined to have prespecified power for formal hypothesis testing. Instead, the sample size was chosen to obtain appropriate precision around endpoints for subsequent phase 3 trials.
The mean change from baseline in IOP at each timepoint was analyzed with one-sample t tests comparing the reduction from baseline to 0. The percentage of study eyes at months 12, 24, and 36 that maintained or reduced their topical IOP-lowering medication burden was analyzed using a Pearson chi-square test.
3 Results
3.1 Patient Baseline Characteristics and Disposition
A total of 270 patients were screened, of whom 116 (43.0%) were not enrolled due to not meeting inclusion criteria or meeting exclusion criteria at screening or baseline. The most common reasons for screen failure included inability or lack of willingness to attend follow-up examinations for 3 years postoperatively (30/116, 25.9%), failure to meet IOP entry criteria following washout (24/116, 20.7%), failure to meet IOP criteria at screening for patients not requiring a washout (11/116, 9.5%), withdrawal by patient at baseline (9/116, 7.8%), and patient on greater than three IOP-lowering medications at screening (7/116, 6.0%).
A total of 154 patients were randomized 1:1:1 to the FE implant (n = 51), SE implant (n = 54), or timolol (n = 49), of whom 135 (87.7%) completed month 36 (FE implant, n = 44; SE implant, n = 46; timolol, n = 45) (Table 1).
Demographics were similar among the three groups. Overall, mean age (± standard deviation, SD) was 62.7 ± 12.2 years, 53.2% of patients where < 65 years of age, 52.6% were female, 77.3% were White, and 94.8% were not of Hispanic or Latino ethnicity (Table 2).
In addition, baseline ocular characteristics were well balanced among the three treatment groups, with the exception of the distribution of patients on 0–1 IOP-lowering medication classes at screening (P < 0.0311). A greater proportion of patients in the FE implant group (82.4%, 42/51) were on 0 or 1 IOP-lowering medication compared with the SE implant (68.5%, 37/54) and timolol (61.2%, 30/49) groups (Table 2).
3.2 Efficacy Outcomes
The 8:00 AM mean overall study eye IOP reductions through month 36 (unweighted average from day 10 to the indicated visit) are shown in Fig. 2. These mean IOP reductions varied between 7.6 and 8.8 mmHg for the FE implant group, 7.3 and 8.0 mmHg for the SE implant group, and 7.3 and 7.9 for the timolol group. Reductions from baseline at all visits for all treatment groups were statistically significant (P < 0.0001).
Mean 8:00 AM IOP change from baseline in the travoprost intraocular implant (FE implant and SE implant) and topical timolol 0.5% BID groups through month 36. IOP change from baseline was calculated using the unweighted average of the treatment group mean change from baseline from day 10 to the indicated visit. IOP change from baseline was statistically significant (P < 0.0001; one-sample t tests) at all visits for all treatment groups. BID twice daily, FE Implant fast-eluting travoprost intraocular implant, IOP intraocular pressure, SE Implant slow-eluting travoprost intraocular implant
Figure 3 shows the percentage of patients with well-controlled IOP on the same or fewer topical IOP-lowering medications compared with screening. As noted previously, from the week 4 visit onward, the study protocol mandated that additional topical IOP-lowering therapy was to be initiated in any study eye with IOP > 18 mmHg. At month 12, a significantly greater percentage of patients in the FE and SE implant groups (86 and 92%, respectively) versus the timolol group (58%) were well controlled on the same or fewer topical IOP-lowering medications compared with screening (FE implant versus timolol, P = 0.0026; SE implant versus timolol, P < 0.0001). At month 24, these percentages were 72% for both the FE and SE implant groups versus 50% for the timolol group (FE implant versus timolol, P = 0.0691; SE implant versus timolol, P = 0.0561), and at month 36, these percentages were 63% for the FE implant group and 69% for the SE implant group versus 45% for the timolol group (FE implant versus timolol, P = 0.1545; SE implant versus timolol, P = 0.0548).
Percentage of study eyes in the travoprost intraocular implant (FE implant and SE implant) and timolol groups at month 12, month 24, and month 36 with well-controlled IOP (i.e., those not requiring additional IOP-lowering medication per the protocol mandated criterion) while on the same or lesser number of topical IOP-lowering medications as at screening. *P ≤ 0.0026 versus timolol, ‡P < 0.10 versus timolol based on Pearson chi-squared test. BID twice daily, FE Implant fast-eluting travoprost intraocular implant, IOP intraocular pressure, SE Implant slow-eluting travoprost intraocular implant
Corresponding 8:00 AM mean (SD) IOP reductions at months 12, 24, and 36 in the subgroup of FE implant patients who were well controlled on the same or fewer topical IOP-lowering medications at that visit compared with screening were 6.1 (5.8), 7.9 (5.1), and 9.7 (6.8) mmHg, respectively. Reductions at these visits in the subgroup of SE implant patients were 7.0 (5.0), 6.8 (5.8), and 8.2 (5.1) mmHg, respectively, and for the timolol patients were 8.0 (4.1), 8.5 (3.3), and 8.9 (3.3) mmHg, respectively (Fig. 4). Reductions from baseline for each subgroup at each of the three visits were statistically significant (P < 0.0001).
Mean IOP reductions in the subgroups of study eyes in the travoprost intraocular implant (FE and SE) and timolol groups at month 12, month 24, and month 36 with well-controlled IOP while on the same or lesser number of topical IOP-lowering medications as at screening. *P < 0.0001 for change from baseline in IOP based on one-sample t test. BID twice daily, FE Implant fast-eluting travoprost intraocular implant, IOP intraocular pressure, SE Implant slow-eluting travoprost intraocular implant
3.3 Safety
A summary of adverse events is presented in Table 3. Study eye adverse events reported in two or more patients in any treatment group are presented in Table 4.
Throughout the study, one or more ocular adverse events, mostly mild or moderate in severity, were reported in the study eyes of 54.9% (28/51), 40.7% (22/54), and 28.6% (14/49) of patients in the FE implant, SE implant, and timolol groups, respectively. The percentage of SE implant study eyes with adverse events was similar to timolol eyes (P = 0.2198). Most study eye adverse events had an onset more than 14 days after the administration procedure.
Severe study eye adverse events were reported in a similar number of patients in each treatment group; one patient with cataract and one patient with both cataract and Meibomian gland dysfunction in the FE implant group, single cases of cataract and hyphema in the SE implant group, and single cases of retinal detachment and IOP increase requiring intervention and cataract surgery in the timolol group.
The most commonly reported treatment-related ocular adverse events in the study eye were eye inflammation, eye pain, and iritis (all of which were mild or moderate in severity, and resolved), occurring in three patients (3/51, 5.9%) each in the FE implant group. In addition, cataract occurred in two patients (2/51, 3.9%) in the FE implant group and one patient (1/54, 1.9%) in the SE implant group. One patient with cataract (in the FE implant group) underwent cataract extraction with placement of an intraocular lens.
There were no ocular adverse events resulting in study discontinuation, and no patient experienced a dislodgement of their FE or SE implant or required explantation of the implant.
There were no serious adverse events reported in the study eye. Nonocular or nonstudy eye serious adverse events were all considered unrelated to study treatment with the exception of one serious adverse event in the timolol group (exacerbation of myasthenia gravis).
No patient in either implant group had an adverse event of eyelash growth or periorbital fat atrophy, while a single patient in the SE implant group (1/54, 1.9%) had an adverse event of iris discoloration.
Based on investigator grading of conjunctival hyperemia, most patients had normal to trace conjunctival hyperemia at baseline. At most timepoints post baseline, the majority of observed hyperemia was trace or mild in nature. In addition, an increase in hyperemia of 1 grade or greater was observed in only a small percentage of patients (9.8% and 14.8% in the FE and SE implant groups, respectively, and 4.1% in the timolol group).
Corneal endothelial cell counts are shown in Fig. 5. At month 36, no statistically significant differences in change from baseline in endothelial cell counts were detected between the implant groups and the timolol group (P > 0.1730).
Mean central corneal endothelial cell counts over time in study eyes treated with travoprost intraocular implant (FE implant or SE implant) or twice-daily (BID) topical timolol 0.5%. At month 36, the difference in change from baseline in corneal endothelial cell counts between the FE implant and timolol groups was −37.9 cells/mm2 (two-sample t test, P = 0.1730, 95% CI: − 92.9, 17.0) and between the SE implant and timolol groups was − 18.3 cells/mm2 (two-sample t test, P = 0.4581, 95% CI: − 67.2, 30.6). Error bars indicate the standard deviation. BID twice daily, CI confidence interval, FE Implant fast-eluting travoprost intraocular implant, SE Implant slow-eluting travoprost intraocular implant
Similarly, central corneal thickness showed no adverse trend throughout the observation period. At baseline, mean (SD) central corneal thickness was 557.9 (34.5), 550.6 (37.1), and 555.1 (34.5) µm in the FE implant, SE implant, and timolol groups, respectively, and at month 36 was 545.4 (34.7), 541.0 (37.5), and 550.2 (32.5) µm in the FE implant, SE implant, and timolol groups, respectively.
There was no clinically meaningful change in the mean visual field mean deviation (MD) over time. The baseline mean MD (SD) was − 2.437 (2.571), − 1.887 (4.234), and − 1.710 (2.900) dB in the FE implant, SE implant, and timolol groups, respectively. At month 36, the MD was − 2.399 (3.610), − 3.610 (6.608), and − 2.319 (5.052) dB in the FE implant, SE implant, and timolol groups, respectively.
4 Discussion
In this study, an intraocular implant containing a proprietary formulation of travoprost was studied in OAG and OHT patients over a period of 3 years.
Travoprost was selected as the PGA to be administered intraocularly because travoprost produg rapidly hydrolyzes to travoprost acid (the active form of travoprost) in the aqueous humor. Furthermore, travoprost free acid is more potent on the prostaglandin F ( FP) receptor than bimatoprost or latanoprost free acid [55].
Topically administered PGAs are highly efficacious when used as directed; however, due to a combination of their side effects and the initially asymptomatic, silent nature of the disease, adherence to topical IOP-lowering medications is poor [11,12,13,14].
The study demonstrated that the travoprost intraocular implant (FE and SE models) attained a combination of robust IOP-lowering efficacy independent of patient adherence, a long duration of efficacy, and a favorable safety profile. This combination of attributes has been a longstanding goal that has largely eluded the ophthalmic community to date. By virtue of being a sustained-release intraocular implant, travoprost implant reduced the number of topical IOP-lowering medications (eye drops) that the patients were using relative to the screening visit, indicative of their pre-study topical pharmacotherapy. At month 12, a significantly greater percentage of patients in the implant groups (86 and 92% of FE and SE implant patients, respectively) compared with the timolol group (58% of patients) were well controlled on the same or fewer topical medications compared with screening. This favorable response rate, accompanied by robust IOP lowering, also was observed at the month 24 and month 36 visits, at which times the percentages of well-controlled patients were numerically higher in the implant groups (72% in both implant groups at month 24, and 63 and 69% in the FE and SE implant groups, respectively, at month 36) than in the timolol group (50 and 45% of patients at months 24 and 36, respectively). This is notable since unmedicated baseline mean (SD) diurnal IOP was 25.4 (3.6), 24.8 (3.9), and 24.8 (3.0) mmHg in the FE implant, SE implant, and timolol groups, respectively, and the protocol required the investigator to prescribe additional IOP-lowering medication if IOP in the study eye was > 18 mmHg at week 4 or later.
By eliminating or greatly reducing topical medications, an intraocular implant optimizes medication adherence, the absence of which is a well-known obstacle to efficacious glaucoma care [15, 18] and a risk factor for blindness [23]. Furthermore, the study’s efficacy outcomes were joined by a favorable safety profile. The intraocular delivery of the drug in the implant further optimized the well-established safety of travoprost resulting in a lower incidence of hyperemia, and absence of periorbital fat atrophy and eyelash/skin pigmentation. In addition, the implant was administered via an optimized insertion technique, resulting in the fixed and stable position of the implant in situ (Fig. 1b). This implant has demonstrated the longest duration of any implantable drug-delivery product for glaucoma to date. The reduction of topical medication burden represents substantial benefit for patients in the form of improved ocular surface, quality of life, and adherence to treatment.
The intraoperative and postoperative safety profile for the travoprost intraocular implants was favorable. The majority of adverse events were mild or moderate across all treatment groups. Only one treatment-related serious adverse event occurred in the study, which was in the control group (myasthenia gravis, related to timolol eye drop treatment). In addition, similar changes from baseline in corneal endothelial cell counts were observed in the travoprost implant groups and the timolol group at month 36. This high level of safety likely can be attributed to achieving the desired efficacy with micro-elution rate of travoprost released intracamerally, thus reducing the daily dose of travoprost by an order of magnitude (at least 10× lesser dose) compared with the topical pulsatile delivery of travoprost via eye drops. Furthermore, the implant’s small size, straightforward implantation technique, anchored position in the anterior chamber angle, and the intraocular tolerability of travoprost contribute to the favorable safety and efficacy profiles of the travoprost intraocular implant.
The study was not without limitations. The active comparator in the trial was timolol eye drops, the most commonly used active comparator in phase 3 trials of new IOP-lowering medications. Travoprost could have been considered as an alternate comparator. Additionally, a contralateral eye control may have allowed for a more clinically relevant evaluation of the safety and efficacy of the travoprost intraocular implants. Observers and patients were masked to treatment assignment (sham procedure versus implant); however, it was not possible for surgeons to be masked and observers may have been able to see the travoprost intraocular implant on slit lamp examination, so may not have remained fully masked to sham versus implant assignment throughout the study. To mitigate this risk of bias, a two-person method was used throughout the study for IOP measurements. There was physician discretion in the type of IOP-lowering medication added if eye drop escalation were needed (e.g., beta-blocker, PGA). As stated previously, the protocol-mandated threshold for adding medication was intentionally set low (IOP > 18 mmHg), reflecting a cautious and conservative approach to this new technology. However, in real-world clinical practice, where physicians may exert greater flexibility in their target IOP range for patients with OHT or mild glaucoma, the length of time before adding topical drops (hence the perceived duration of efficacy, as reported in this trial) would be expected to be greater. Finally, patients in the travoprost intraocular implant arms received an artificial tear solution containing glycerin and propylene glycol as the placebo eye drop, which may have reduced symptoms of dryness or irritation in the implant groups relative to patients receiving timolol eye drops. Two phase 3 trials (NCT03868124, NCT03519386) with larger sample size remain underway to demonstrate the safety and efficacy of this product. In addition, a trial has been completed which demonstrated the feasibility and safety of the administration of a new SE implant followed by removal of the previous implant (“exchange” procedure) (NCT04615403). The SE travoprost intraocular implant was selected for further development due to a combination of more favorable risk-to-benefit profile and improved manufacturability compared with the FE implant.
Limitations notwithstanding, the promising findings of this study are clinically impactful to both physicians and patients, showing sustained and safe IOP reduction and decreased topical medication burden with an implantable drug-delivery product.
The travoprost intraocular implant demonstrated the potential for patient-independent medication delivery, with the objective of promoting steady IOP control that would serve to preserve visual function. Furthermore, reducing topical medications is well known to have substantial quality of life advantages, such as reduced exposure to eye drops and preservatives such as BAK, fewer burdensome side effects and drop instillation regimens, and improved disease prognosis due to preventing the IOP high peak and IOP fluctuations, and visual field damage progression associated with nonadherence to eye drop therapy [23,24,25,26]. These results suggest that the travoprost intraocular implant may represent a meaningful addition to the interventional glaucoma armamentarium, demonstrating safe and well-tolerated IOP lowering for up to 36 months after a single administration and addressing the key shortcomings of topical IOP-lowering medications defined by low adherence and adverse impact on ocular surface health.
References
Tham YC, Li X, Wong TY, Quigley HA, et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90. https://doi.org/10.1016/j.ophtha.2014.05.013.
Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:701–13. https://doi.org/10.1001/archopht.120.6.701.
Gordon MO, Beiser JA, Brandt JD, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):714–20. https://doi.org/10.1001/archopht.120.6.714.
Heijl A, Leske MC, Bengtsson B, et al. Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002;120:1268–79. https://doi.org/10.1001/archopht.120.10.1268.
Leske MC, Heijl A, Hussein M, et al. Factors for glaucoma progression and the effect of treatment: the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2003;121(1):48–56. https://doi.org/10.1001/archopht.121.1.48.
Collaborative Normal-Tension Glaucoma Study Group. The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Am J Ophthalmol. 1998;126:498–505. https://doi.org/10.1016/s0002-9394(98)00272-4.
Lichter PR, Musch DC, Gillespie BW, et al. CIGTS Study Group. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology. 2001;108(11):1943–53. https://doi.org/10.1016/s0161-6420(01)00873-9.
Chauhan BC, Mikelberg FS, Balaszi AG, et al. Canadian Glaucoma Study: 2. risk factors for the progression of open-angle glaucoma. Arch Ophthalmol. 2008;126:1030–6. https://doi.org/10.1001/archopht.126.8.1030.
Gedde SJ, Vinod K, Wright MM, et al. Primary open-angle glaucoma preferred practice Pattern®. Ophthalmology. 2021;128(1):71–150. https://doi.org/10.1016/j.ophtha.2020.10.022.
Garway-Heath DF, Crabb DP, Bunce C, et al. Latanoprost for open-angle glaucoma (UKGTS): a randomised, multicentre, placebo-controlled trial. Lancet. 2015;385:1295–304. https://doi.org/10.1016/S0140-6736(14)62111-5.
Nordstrom BL, Friedman DS, Mozaffari E, et al. Persistence and adherence with topical glaucoma therapy. Am J Ophthalmol. 2005;140(4):598–606. https://doi.org/10.1016/j.ajo.2005.04.051.
Newman-Casey PA, Robin AL, Blachley T, et al. The most common barriers to glaucoma medication adherence: a cross-sectional survey. Ophthalmology. 2015;122(7):1308–16. https://doi.org/10.1016/j.ophtha.2015.03.026.
Tsai JC. A comprehensive perspective on patient adherence to topical glaucoma therapy. Ophthalmology. 2009;116:S30–6. https://doi.org/10.1016/j.ophtha.2009.06.024.
Schwartz GF, Quigley HA. Adherence and persistence with glaucoma therapy. Surv Ophthalmol. 2008;53(Suppl 1):S57-68. https://doi.org/10.1016/j.survophthal.2008.08.002.
Okeke CO, Quigley HA, Jampel HD, et al. Adherence with topical glaucoma medication monitored electronically the Travatan Dosing Aid study. Ophthalmology. 2009;116(2):191–9. https://doi.org/10.1016/j.ophtha.2008.09.004.
Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304–14. https://doi.org/10.4065/mcp.2010.0575.
Kholdebarin R, Campbell RJ, Jin Y-P, et al. Multicenter study of compliance and drop administration in glaucoma. Can J Ophthalmol. 2008;43(4):454–61. https://doi.org/10.1139/i08-076.
Robin AL, Covert D. Does adjunctive glaucoma therapy affect adherence to the initial primary therapy? Ophthalmology. 2005;112:863–8. https://doi.org/10.1016/j.ophtha.2004.12.026.
Siani SD, Schoenfeld P, Kaulback K, et al. Effect of dosing frequency on adherence in chronic diseases. Am J Manag Care. 2009;15(6):e22-33.
Patel SC, Spaeth GL. Compliance in patients prescribed eyedrops for glaucoma. Ophthalmic Surg. 1995;26(3):233–6.
Stone JL, Robin AL, Novack GD, et al. An objective evaluation of eye-drop instillation in glaucoma patients. Arch Ophthalmol. 2009;127:732–6. https://doi.org/10.1001/archophthalmol.2009.96.
Hennessey AL, Katz J, Covert D, et al. A video study of drop instillation in both glaucoma and retina patients with visual impairment. Am J Ophthalmol. 2011;152(6):982–8. https://doi.org/10.1016/j.ajo.2011.05.015.
Grant WM, Burke JF Jr. Why do some people go blind from glaucoma? Ophthalmology. 1982;89(9):991–8. https://doi.org/10.1016/s0161-6420(82)34675-8.
Sleath B, Blalock S, Covert D, et al. The relationship between glaucoma medication adherence, eye drop technique, and visual field defect severity. Ophthalmology. 2011;118:2398–402. https://doi.org/10.1016/j.ophtha.2011.05.013.
Paula JS, Furtado JM, Santos AS, et al. Risk factors for blindness in patients with open-angle glaucoma followed-up for at least 15 years. Arq Bras Oftalmol. 2012;75:243–6. https://doi.org/10.1590/s0004-27492012000400004.
Rossi GC, Pasinetti GM, Scudeller L, et al. Do adherence rates and glaucomatous visual field progression correlate? Eur J Ophthalmol. 2011;21:410–4. https://doi.org/10.5301/EJO.2010.6112.
Skalicky SE, Goldberg I, McCluskey P. Ocular surface disease and quality of life in patients with glaucoma. Am J Ophthalmol. 2012;153(1):1–9. https://doi.org/10.1016/j.ajo.2011.05.033.
Nordmann JP, Auzanneau N, Ricard S, et al. Vision related quality of life and topical glaucoma treatment side effects. Health Qual Life Outcomes. 2003;1:75. https://doi.org/10.1186/1477-7525-1-75.
Leung EW, Medeiros FA, Weinreb RN. Prevalence of ocular surface disease in glaucoma patients. J Glaucoma. 2008;17(5):350–5. https://doi.org/10.1097/IJG.0b013e31815c5f4f.
Fechtner RD, Godfrey DG, Budenz D, Stewart JA, Stewart WC, Jasek MC. Prevalence of ocular surface complaints in patients with glaucoma using topical intraocular pressure-lowering medications. Cornea. 2010;29(6):618–21. https://doi.org/10.1097/ICO.0b013e3181c325b2.
Rossi GCM, Tinelle C, Pasinette GM, et al. Dry eye syndrome related quality of life in glaucoma patients. Eur J Ophthalmol. 2009;19(4):572–9. https://doi.org/10.1177/112067210901900409.
Inoue K. Managing adverse effects of glaucoma medications. Clinical Ophthalmol. 2014;8:903–13. https://doi.org/10.2147/OPTH.S44708.
Janz NK, Wren PA, Lichter PR, et al. Quality of life in newly diagnosed glaucoma patients: the Collaborative Initial Glaucoma Treatment Study. Ophthalmology. 2001;108(5):887–97. https://doi.org/10.1016/s0161-6420(00)00624-2. (discussion 898).
Brandt JD, Wittpenn JR, Katz LJ, et al. Conjunctival impression cytology in patients with glaucoma using longterm topical medications. Am J Ophthalmol. 1991;112:297–301. https://doi.org/10.1016/s0002-9394(14)76730-3.
Baudouin C, Labbe A, Liang H, et al. Preservatives in eyedrops: the good, the bad and the ugly. Prog Retin Eye Res. 2010;29:312–34. https://doi.org/10.1016/j.preteyeres.2010.03.001.
Baudouin C, Pisella CJ, Fillacier K, et al. Ocular surface inflammatory changes induced by topical antiglaucoma drugs: human and animal studies. Ophthalmology. 1999;106(3):556–63. https://doi.org/10.1016/S0161-6420(99)90116-1.
Johnson DH, Yoshikawa K, Brubaker RF, et al. The effect of long-term medical therapy on the outcome of filtration surgery. Am J Ophthalmol. 1994;117:139–48. https://doi.org/10.1016/s0002-9394(14)73068-5.
Arici MK, Arici DS, Topalkara A, et al. Adverse effects of topical antiglaucoma drugs on the ocular surface. Clin Exp Ophthalmol. 2000;28:113–7. https://doi.org/10.1046/j.1442-9071.2000.00237.x.
Noecker RJ, Herrygers LA, Anwaruddin R. Corneal and conjunctival changes caused by commonly used glaucoma medications. Cornea. 2004;23:490–6. https://doi.org/10.1097/01.ico.0000116526.57227.82.
Broadway DC, Grierson I, O’Brien C, et al. Adverse effects of topical antiglaucoma medication. I. The conjunctival cell profile. Arch Ophthalmol. 1994;112:1437–45. https://doi.org/10.1001/archopht.1994.01090230051020.
Broadway DC, Grierson I, O’Brien C, et al. Adverse effects of topical antiglaucoma medication. II. The outcome of filtration surgery. Arch Ophthalmol. 1994;112:1446–54. https://doi.org/10.1001/archopht.1994.01090230060021.
Pisella PJ, Pouliquen P, Baudouin C. Prevalence of ocular symptoms and signs with preserved and preservative-free glaucoma medication. Br J Ophthalmol. 2002;86(4):418–23. https://doi.org/10.1136/bjo.86.4.418.
Broadway D, Hitchings R, Grierson I. Topical antiglaucomatous therapy: adverse effects on the conjunctiva and implications for filtration surgery. J Glaucoma. 1995;4(2):136.
Cvenkel B, Kolko M. Devices and treatments to address low adherence in glaucoma patients: a narrative review. J Clin Med. 2023;12:151–71. https://doi.org/10.3390/jcm12010151.
Gooch N, Molokhia SA, Condie R, et al. Ocular drug delivery for glaucoma management. Pharmaceutics. 2012;4(1):197–211. https://doi.org/10.3390/pharmaceutics4010197.
Shalaby WS, Shankar V, Razeghinejad R, et al. Current and new pharmacotherapeutic approaches for glaucoma. Expert Opin Pharmacother. 2020;21(16):2027–40. https://doi.org/10.1080/14656566.2020.1795130.
Allergan. DURYSTATM (bimatoprost implant), for intracameral administration [Prescribing Information]. Available at: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=3f59da84-0bcc-4c84-b3e2-e215681ef341. Accessed 29 May 2023.
Craven ER, Walters T, Christie WC, et al. 24-Month phase I/II clinical trial of bimatoprost sustained-release implant (bimatoprost SR) in glaucoma patients. Drugs. 2020;80(2):167–79. https://doi.org/10.1007/s40265-019-01248-0.
Medeiros FA, Walters TR, Kolko M, et al. ARTEMIS 1 Study Group. Phase 3, randomized, 20-month study of bimatoprost implant in open-angle glaucoma and ocular hypertension (ARTEMIS 1). Ophthalmology. 2020;127(12):1627–41. https://doi.org/10.1016/j.ophtha.2020.06.018.
Bacharach J, Tatham A, Ferguson G, et al. ARTEMIS 2 Study Group. Phase 3, randomized, 20-month study of the efficacy and safety of bimatoprost implant in patients with open-angle glaucoma and ocular hypertension (ARTEMIS 2). Drugs. 2021;81(17):2017–33. https://doi.org/10.1007/s40265-021-01624-9.
Nouri-Mahdavi K, Hoffman D, Coleman AL, et al. Predictive factors for glaucomatous visual field progression in the Advanced Glaucoma Intervention Study. Ophthalmology. 2004;111:1627–35. https://doi.org/10.1016/j.ophtha.2004.02.017.
Asrani S, Zeimer R, Wilensky J, et al. Large diurnal fluctuations in intraocular pressure are an independent risk factor in patients with glaucoma. J Glaucoma. 2000;9:134–42. https://doi.org/10.1097/00061198-200004000-00002.
Caprioli J, Coleman AL. Intraocular pressure fluctuation a risk factor for visual field progression at low intraocular pressures in the advanced glaucoma intervention study. Ophthalmology. 2008;115:1123–9. https://doi.org/10.1016/j.ophtha.2007.10.031.
Leske MC, Heijl A, Hyman L, et al. Early Manifest Glaucoma Trial Group. Predictors of long-term progression in the Early Manifest Glaucoma Trial. Ophthalmology. 2007;114:1965–72. https://doi.org/10.1016/j.ophtha.2007.03.016.
Sharif NA, Kelly CR, Crider JY. Agonist activity of bimatoprost, travoprost, latanoprost, unoprostone isopropyl ester and other prostaglandin analogs at the cloned human ciliary body FP prostaglandin receptor. J Ocul Pharmacol Ther. 2002;18(4):313–24. https://doi.org/10.1089/10807680260218489.
Acknowledgements
Editorial and writing assistance of an earlier version of the manuscript was provided by Dana Hornbeak, MD, MPH. All authors met the ICJME criteria for authorship.
Travoprost Intraocular Implant Study Group: Robert E.T. Ang, MD (Makati City, Philippines); Jason Bacharach, MD (Petaluma, CA, USA); Harmohina Bagga, MD (Beverly Hills, CA, USA); Kent P. Bashford, DO (Fort Collins, CO, USA); John P. Berdahl, MD (Sioux Falls, SD, USA); Yun-Sen Ralph Chu, MD (Bloomington, MN, USA); Robert J. Cionni, MD (Salt Lake City, UT, USA); Charles J. Crane, MD (South Orange, NJ, USA); Francis A. D’Ambrosio, MD (Lancaster, MA, USA); Mohammed K. ElMallah, MD (Ocala, FL, USA); Raj K. Goyal, MD (Chicago, IL, USA); Jason J. Jones, MD (Sioux City, IA, USA); Joshua W. Kim, MD (Sarasota, FL, USA); Robert P. Lehmann, MD (Nacogdoches, TX, USA); Christopher Lin, MD (Redding, CA, USA); David M. Lubeck, MD (Orland Park, IL, USA); Robert E. Marquis, MD (Austin, TX, USA); Cathleen M. McCabe, MD (Bradenton, FL, USA); George R. Reiss, MD (Sun City, AZ, USA); Steven R. Sarkisian, Jr., MD (Oklahoma City, OK, USA); Robert C. Sorenson, MD (Hemet, CA, USA); Farrell C. Tyson, II, MD (Cape Coral, FL, USA); Steven D. Vold, MD (Fayetteville, AR, USA); Charles H. Weber, MD (Salt Lake City, UT, USA); Bin Wu, MD (Lancaster, MA, USA); and David E. Yomtoob, MD (Orange, CA, USA).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
This study was sponsored by Glaukos Corporation (Aliso Viejo, CA). Glaukos participated in the design of the study, data management, analysis and interpretation, and the preparation, review, and approval of the manuscript.
Conflict of interest
John P. Berdahl has received consulting fees, paid advisory board member or received fees for attending a meeting for AbbVie, Aerpio, Alcon, Aldeyra, Aurea Medical, Aurion Biotech/CorneaGen, Balance Ophthalmics, Bausch and Lomb, Dakota Lions Eye Bank, Elios Vision Inc., Equinox, Expert Opinion, Glaukos, Gore, Imprimis, Interfeen, iRenix, Iacta Pharmaceuticals, IVERIC bio, Inc., JNJ, Kala, Kedalion, MELT Pharmaceuticals, MicroOptx, New World Medical, Ocular Surgical Data, Ocular Therapeutix, Omega Ophthalmic, Orasis, Oyster Point, RxSight, Santen, Sight Sciences, Surface Inc., Tarsus, Tear Clear, Vertex Ventures, ViaLase, Vittamed, Vance Thompson Vision, Versea Biologics, Visionary Ventures, Visus and Zeiss; has received lecture fees (honoraria), travel fees or reimbursements when speaking for AbbVie, Alcon and Glaukos; has equity ownership/stock options of Aurion Biotech/CorneaGen, Balance Ophthalmics, Equinox, Expert Opinion, Interfeen, Ocular Surgical Data, Omega Ophthalmic, Surface Inc, Vance Thompson Vision, Verana Health and Zeiss; owns stock of Glaukos; has patents and/or royalties with Imprimis. Steven R. Sarkisian Jr is a consultant/advisor for Alcon, Allergan, Bausch + Lomb, Beaver-Visitec International, Glaukos, Icare USA, Katena Products, MicroSurgical Technology, Ocular Science, Santen, and Sight Sciences; is on the speaker’s bureau for Alcon, Allergan, and Bausch + Lomb; has received grant support from Alcon, Allergan, Allysta Pharmaceuticals, Elios, Glaukos, iSTAR Medical, Ocular Science, Ocular Therapeutix, and Sight Sciences; and holds stock or stock options in Ocular Science and Sight Sciences. Robert E. Ang has been a speaker for, and received research support from Glaukos. Long V. Doan, L. Jay Katz, Angela C. Kothe, Dale W. Usner and Tomas Navratil are employees of Glaukos Corporation and may hold Glaukos stock/stock options.
Ethics approval
Institutional review board or independent ethics committee approval was obtained at each site before the study began, and the study was performed in compliance with good clinical practice, the principles of the Declaration of Helsinki, or the laws and regulations of the country in which the study was conducted (ClinicalTrials.gov registration number NCT02754596).
Consent
All patients in this study provided written informed consent before undergoing any study-related procedure.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to ongoing US Food and Drug Administration review of a New Drug Application for the travoprost intraocular implant but are available from the corresponding author on reasonable request.
Code availability
Not applicable
Author contributions
Study design: LVD, LJK; data collection: JPB, SRS, REA; statistical analysis: DWU; data interpretation: JPB, SRS, REA, LVD, LJK, ACK, DWU, TN; authoring, revisions, and approval of the manuscript: JPB, SRS, REA, LVD, LJK, ACK, DWU, TN.
Additional information
The members of “The Travoprost Intraocular Implant Study Group” are listed in Acknowledgements section.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Berdahl, J.P., Sarkisian, S.R., Ang, R.E. et al. Efficacy and Safety of the Travoprost Intraocular Implant in Reducing Topical IOP-Lowering Medication Burden in Patients with Open-Angle Glaucoma or Ocular Hypertension. Drugs 84, 83–97 (2024). https://doi.org/10.1007/s40265-023-01973-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-023-01973-7