Abstract
Fenfluramine (Fintepla®) is an oral anti-seizure medication (ASM) with a novel mechanism of action consisting of activity in the serotonergic system coupled with positive allosteric modulation effects at sigma-1 receptors. Originally approved for use at high doses as an appetite suppressant, it was subsequently withdrawn after being linked to valvular heart disease (VHD) and pulmonary arterial hypertension (PAH), before being investigated for use at low doses as an adjunctive ASM in patients with developmental epileptic encephalopathies, including Dravet syndrome (DS) and Lennox-Gastaut syndrome (LGS) who have pharmacoresistant seizures. In clinical trials, treatment with adjunctive fenfluramine markedly reduced convulsive seizure frequency in patients with DS that were sustained for up to 3 years, and reduced drop seizure frequency in patients with LGS that were sustained for up to 1 year. Notably, fenfluramine was also associated with clinically meaningful improvements in aspects of everyday executive functioning (EF) not entirely explainable by seizure reduction alone. Furthermore, it was generally well tolerated with, importantly, no reports of VHD or PAH. Thus, adjunctive fenfluramine is a novel and effective treatment for pharmacoresistant seizures associated with DS and LGS that may also improve aspects of everyday EF in some patients.
Plain Language Summary
Emerging in infancy and childhood, respectively, Dravet syndrome (DS) and Lennox-Gastaut syndrome (LGS) are severe developmental and epileptic encephalopathies. They are characterized by seizures that are frequently ‘pharmacoresistant’ [i.e. cannot be controlled by ≥ 2 anti-seizure medications (ASMs)] and that, along with cognitive and behavioural comorbidities, can have a major impact on the quality of life of patients (and their caregivers/family members) as they grow. Fenfluramine (Fintepla®) is an oral ASM with a distinctive dual mechanism of action, that is used at low doses. In clinical trials in patients with DS or LGS, adding fenfluramine to the existing ASM regimen produced significant and sustained reductions in pharmacoresistant seizures and was associated with clinically meaningful improvements in aspects of everyday executive functioning (EF; i.e. the ability to regulate cognition, emotions and/or behaviour). Importantly, there was no evidence of the heart complications previously observed with the use of high doses of fenfluramine as an appetite suppressant. Adjunctive fenfluramine is an effective and generally well-tolerated treatment for pharmacoresistant seizures associated with DS and LGS that may also improve aspects of everyday EF in some patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Digital Features for this Adis Drug Evaluation can be found at https://doi.org/10.6084/m9.figshare.22358086. |
Novel (dual) mechanism of action at both serotonergic and sigma-1 receptors |
Markedly reduces monthly convulsive seizure frequency in patients with DS, and reduces monthly drop seizure frequency in patients with LGS |
In addition to reducing seizures, appears to have potential to improve aspects of everyday EF |
Most common adverse event in clinical development programme is decreased appetite, with no reports of VHD or PAH with low-dose use |
1 Introduction
Dravet syndrome (DS) and Lennox-Gastaut syndrome (LGS) are rare, but nonetheless severe, developmental epileptic encephalopathies (DEEs), with infantile- and childhood-onset, respectively [1,2,3]. Among other features, both conditions are characterized by multiple types of seizures, varying degrees of cognitive dysfunction and behavioural problems, and a high mortality rate [1,2,3]. Both are highly treatment-resistant, with seizures often remaining poorly controlled, despite polypharmacy with anti-seizure medications (ASMs), such as valproate, clobazam and stiripentol in DS, and valproate, clobazam, lamotrigine and topiramate in LGS [1,2,3]. Despite the availability of > 30 first, second and third generation ASMs with mechanisms of action that fall into four broad categories [4], there continues to be a need for innovative ASMs with distinct mechanism(s) of action that can reduce refractory seizures (and potentially also improve other comorbidities) in DS and LGS [5, 6]. Administered orally, fenfluramine (Fintepla®) is a novel adjunctive ASM with dual activities as a pro-serotonergic agent and as a positive allosteric modulator of sigma-1 receptors (σ1-Rs) [1, 2, 6, 7]. It is suggested that the activity of the drug at serotonin (5-HT) receptors primarily increases inhibitory γ-aminobutyric acidic signalling, while that at σ1-Rs primarily decreases excitatory glutamatergic signalling [7].
Oral fenfluramine is approved in the EU for the treatment of seizures associated with DS and LGS as an add-on therapy to other ASMs for patients aged ≥ 2 years [8]. Additionally, it is approved in the USA for the treatment of seizures associated with DS and LGS in patients aged ≥ 2 years [9], as well as in Japan for the treatment of seizures associated with DS in patients aged ≥ 2 years whose seizures are not controlled by other ASMs [10]. Of note, fenfluramine has been repositioned from an appetite suppressant to an ASM [11, 12]. In this respect, it is used at comparatively low doses in patients with DS and LGS (maximum 17–26 mg/day; Sect. 6), having previously been used at relatively high doses (typically 60–120 mg/day; often in combination with phentermine) as an appetite suppressant in adults with obesity until 1997, when it was withdrawn due to an association with the serious cardiovascular (CV) adverse events (AEs) of valvular heart disease (VHD) and pulmonary arterial hypertension (PAH) [6, 11]. This review focuses on the efficacy and tolerability of low-dose fenfluramine in patients with DS or LGS. Relevant pharmacological properties of the drug are also discussed.
2 Pharmacodynamic Properties of Fenfluramine
Although the exact mechanism(s) underlying their therapeutic effects in DS and LGS are still being elucidated, fenfluramine and its major active metabolite, norfenfluramine, are thought to reduce seizures and potentially improve cognitive impairment associated with these conditions via actions on certain 5-HT receptors, as well as on σ1-Rs [5,6,7, 13, 14].
Fenfluramine exhibits both indirect and direct serotonergic activities [6, 13]. It is a 5-HT-releasing agent that increases extracellular 5-HT levels by disrupting vesicular storage of the transmitter and inhibiting its pre-synaptic re-uptake [15]. In addition, fenfluramine and norfenfluramine exhibited antiepileptiform activity attributed to agonism at 5-HT1D, 5-HT2A, 5-HT2C and 5-HT4 receptors, as well as antagonism at 5-HT1A receptors in preclinical (rodent and Zebrafish) models of seizures or epilepsy [14, 16,17,18,19]. Thus, although agonism at 5-HT1D, 5-HT2A and 5-HT2C receptors is thought to be primarily responsible for the anti-seizure activity of the drug [6, 13], 5-HT4 agonism and 5-HT1A antagonism may also have a role [13, 19]. Agonism of 5-HT2C receptors is also thought to contribute directly to the anorectic effect of fenfluramine [13], while additional agonism at 5-HT2B receptors is associated with the drug-induced valvulopathy that led to the previous withdrawal of the high-dose formulation (Sect. 1) [5]. Of note, both fenfluramine and norfenfluramine consist of a racemic mixture of two (d- and l-) isomers [6, 13, 20]; both l-isomers of the parent compound, as well as the d-isomer of the active metabolite, contributed to the efficacy of fenfluramine in the Zebrafish model of DS [20].
The interaction(s) between fenfluramine and norfenfluramine and σ1-Rs appear complex and multifaceted. For example, fenfluramine and norfenfluramine displayed antiepileptiform activity attributed to antagonism at σ1-Rs in the aforementioned animal models of seizures [16] and DS [18]. In a chemically-induced rodent model of amnesia, however, fenfluramine behaved as positive allosteric modulators of σ1-Rs and attenuated learning deficits, whereas norfenfluramine acted as antagonists of σ1-Rs and exhibited no such cognitive benefit [7, 21].
3 Pharmacokinetic Properties of Fenfluramine
Following a single oral dose of fenfluramine 0.7 mg/kg in fed healthy volunteers, the time to the maximum plasma concentration (Cmax) of fenfluramine and norfenfluramine (the major active metabolite of fenfluramine) was 3 h and 12 h [22]. The Cmax and area under the plasma concentration-time curve from time zero to infinity (AUC0–∞) appeared dose-proportional for fenfluramine, but less than dose-proportional for norfenfluramine, over the dose range of 0.35–0.7 mg/kg [8]. Steady-state for fenfluramine and norfenfluramine was reached in ≈ 4 and ≈ 5 days, respectively, with a Cmax accumulation ratio of 3.7- and 6.4-fold, respectively [8]. The absolute bioavailability of fenfluramine is 75–83%, and food has no effect on the absorption and bioavailability of, or systemic exposure to, fenfluramine [8, 9, 22]. Fenfluramine is 50% bound to human plasma proteins in vitro (binding is independent of fenfluramine concentration) and the geometric mean (GM) volume of distribution of orally administered fenfluramine in healthy volunteers is 11.9 L/kg [8].
Fenfluramine is largely (> 75%) metabolised to norfenfluramine prior to elimination, mainly by CYP1A2, CYP2B6 and CYP2D6, and, to a minor extent, CYP2C9, CYP2C19 and CYP3A4/5 [8, 9]. Norfenfluramine is then deaminated and oxidized to form inactive metabolites, a process that may also involve glucuronidation [8, 9]. Most (> 90%) of an orally administered dose of fenfluramine is excreted in the urine, predominantly as parent drug and metabolites; < 5% is found in the faeces [8, 9]. The GM clearance of orally administered fenfluramine in healthy volunteers is 6.9 L/h; the elimination half-lives of fenfluramine and norfenfluramine are 20 h and ≈ 30 h, respectively [8].
Age, gender, race, body mass index and CYP genetic polymorphisms have no notable effects on the pharmacokinetics of fenfluramine or norfenfluramine [8, 9]. No clinical data are available concerning the effects of mild or moderate kidney impairment on the pharmacokinetics of fenfluramine and norfenfluramine [8]; however, in patients with severe kidney impairment (i.e. estimated glomerular filtration rate ≥ 15 to < 30 mL/min/1.73m2), the Cmax and AUC0–∞ of fenfluramine and norfenfluramine following a single oral dose of fenfluramine 0.35 mg/kg were up to 20% and 88%, respectively, higher than in matched healthy volunteers [8, 9]. Additionally, after a single oral dose of fenfluramine 0.35 mg/kg, the combined molar Cmax and AUC from time zero to the last measurable concentration (AUC0–t) of fenfluramine were increased by up to 8% and 82%, respectively, in patients with mild, moderate or severe liver impairment compared with those with normal liver function [9]. Dosage modifications may be required in patients with kidney or liver impairment (Sect. 6) [8, 9].
In a drug-drug interaction study, coadministration of a single oral dose of fenfluramine 0.7 mg/kg with single oral doses of stiripentol 3.5 g, clobazam 20 mg and valproate 25 mg/kg (maximum 1.5 g) increased exposure to fenfluramine by ≈ 70% while decreasing exposure to norfenfluramine by ≈ 40% compared with a single oral dose of fenfluramine 0.7 mg/kg alone [23]. Thus, the maximum daily dose of fenfluramine should be reduced when coadministered with stiripentol-containing ASM regimens (Sect. 6) [8, 9, 23].
Fenfluramine and norfenfluramine are not inhibitors or inducers of CYP enzymes [8, 9]. However, as they are primarily metabolized by CYP1A2, CYP2B6 and CYP2D6, coadministration of fenfluramine with strong CYP1A2 or CYP2D6 inhibitors or strong CYP1A2, CYP2B6 or CYP3A inducers increases or decreases plasma concentrations of fenfluramine. If coadministration with these agents is unavoidable, dosage modification of fenfluramine may be required (Sect. 6) [8, 9].
4 Therapeutic Efficacy of Fenfluramine
4.1 Dravet Syndrome
4.1.1 Clinical Trials
Based on encouraging early results from an ongoing open-label, investigator-initiated, phase II study [13], the efficacy of adjunctive fenfluramine against treatment-resistant seizures associated with DS was evaluated in three randomized, double-blind, placebo-controlled, multinational, phase III trials (hereafter referred to as Studies 1 [24], 2 [25] and 3 [26]). The longer-term efficacy of the drug was assessed in an open-label extension (OLE) study that enrolled patients who completed any of Studies 1–3 [27,28,29].
Eligible patients in Studies 1–3 were males and females aged 2–18 years with a clinical diagnosis of DS who experienced ≥ 6 convulsive seizures during a 6-week baseline observation period, despite receiving stable ASM therapy [24, 26]. In addition, in order to participate in Study 2, the existing ASM regimen of patients had to include stiripentol (plus clobazam and/or valproate, at a minimum) [25]. Conversely, patients who had received stiripentol within 3 weeks before screening were ineligible to participate in Studies 1 and 3 [24, 26].
Of note, Studies 1 and 3 were prospective-merged analyses of patients from two identical, randomized, double-blind, placebo-controlled trials, one of which was conducted in North America and the other in Europe, Australia and Japan [30]. Databases of Studies 1 and 3 were combined due to slow enrolment, with the first 119 participants forming the Study 1 patient population, and the final 143 participants forming the Study 3 patient population [30]. Study 2 (87 participants) was conducted in North America and Europe [25].
Following the 6-week baseline period, Study 2 participants were randomized and stratified according to age (< 6 vs ≥ 6 years) to receive placebo or fenfluramine 0.4 mg/kg/day (uptitrated from 0.2 mg/kg/day over a 3-week period; maximum daily dose 17 mg) on top of their stiripentol-including ASM regimen for a total of 15 weeks (Table 1) [25]. Study 1 and 3 participants were randomized and, where known [24], stratified according to age (< 6 vs ≥ 6 years), to receive placebo, fenfluramine 0.2 mg/kg/day or fenfluramine 0.7 mg/kg/day (uptitrated from 0.2 mg/kg/day over a 2-week period; maximum daily dose 26 mg) on top of their stiripentol-excluding ASM regimen for a total of 14 weeks (Table 1) [24, 26]. The primary efficacy endpoint was the change in the mean monthly convulsive seizure frequency (MCSF) during the total treatment period compared with baseline in the fenfluramine 0.4 mg/kg/day group versus placebo (Study 2 [25]) or the fenfluramine 0.7 mg/kg/day group versus placebo (Studies 1 and 3 [24, 26]) [Table 1]. Patient demographics and baseline characteristics were comparable across the treatment arms in all three studies [24,25,26].
Patients receiving fenfluramine 0.7 mg/kg/day in Studies 1 and 3 demonstrated a > 60% greater reduction from baseline in mean MCSF than those receiving placebo, while those receiving fenfluramine 0.4 mg/kg/day with stiripentol in Study 2 showed a > 50% greater reduction from baseline in mean MCSF than those receiving placebo (Table 1) [24,25,26]. Fenfluramine at dosages of 0.2 and 0.7 mg/kg/day in Studies 1 and 3, and at 0.4 mg/kg/day with stiripentol in Study 2, was also significantly more effective than placebo for all prespecified key secondary endpoints in the respective studies, including the 50% responder rate [RR50; the proportion of patients achieving a ≥ 50% (‘clinically meaningful’) reduction in in seizure frequency], the 75% responder rate [RR75; the proportion of patients achieving a ≥ 75% (‘profound’) reduction in in seizure frequency] [26], and the duration of the longest seizure-free interval (Table 1) [24,25,26]. There was an apparent dose-response relationship for fenfluramine on the primary and all key secondary endpoints, both in Study 1 [24] and Study 3 [26] (Table 1). Additionally, according to a number-needed-to treat analysis of pooled data from Studies 1 and 2, one of every two to three patients with DS achieved RR50 or RR75 with fenfluramine compared with placebo [31].
According to a post hoc analysis, fenfluramine 0.7 mg/kg/day provided significantly more convulsive-seizure-free days per month than placebo in Study 1 (median 24.4 vs 15.1; p = 0.012), as did fenfluramine 0.4 mg/kg/day with stiripentol in Study 2 (median 24.4 vs 20.3; p = 0.001) [32]. Additionally, the proportion of patients who achieved near-freedom from convulsive seizures was higher than with placebo in the fenfluramine 0.4 mg/kg/day with stiripentol group in Study 2, and in the fenfluramine 0.7 mg/kg/day group in Study 1 (Table 1).
In seizure-type subgroup analyses, fenfluramine 0.2 mg/kg/day, 0.4 mg/kg/day (with stiripentol) and 0.7 mg/kg/day reduced the frequency of generalized tonic-clonic (GTC) seizures by a median of 48%, 64% and 80%, respectively, versus 10% for placebo, and reduced the frequency of focal-to-bilateral tonic-clonic seizures by a median of 69%, 33% and 97%, respectively, versus 39% for placebo (pooled data from Studies 1 and 2) [33].
With regard to quality of life (QOL), fenfluramine was not associated with an improvement on the Quality of Life in Childhood Epilepsy Scale or the Pediatric Quality of Life Inventory (PedsQL) in Study 2 [25]; however, in Study 1, fenfluramine showed significant (p ≤ 0.02 vs placebo) improvements in the PedsQL total score [24]. Similarly, whereas fenfluramine 0.4 mg/kg/day with stiripentol exhibited no effect on executive functioning (EF) in Study 2 [25], as assessed using the age-appropriate Behaviour Rating Inventory of Executive Function (BRIEF) instrument [i.e. BRIEF-Preschool (P) version for patients aged 2–5 years; BRIEF for those aged 5–18 years], both the 0.2 and 0.7 mg/kg/day dosages showed significant (p < 0.02 vs placebo) improvements on the BRIEF Behavioural Regulatory Index (BRI) in Study 1 [24]. The 0.7 mg/kg/day dosage also showed a significant (p = 0.02 vs placebo) improvement on the BRIEF summary score [Global Executive Composite (GEC)] [24].
Moreover, fenfluramine was associated with dose-dependent, clinically meaningful improvements (CMIs) in ≥ 1 aspect of everyday EF in a subgroup of preschool children [n = 61; median age 3 (range 2–4) years] with DS and high baseline everyday EF impairment (post hoc analysis of pooled data from Studies 1 and 2) [34]. Specifically, 3 (20%) of 15 fenfluramine 0.2 mg/kg/day recipients, 3 (30%) of 10 fenfluramine 0.4 mg/kg/day with stiripentol recipients and 9 (64%) of 14 fenfluramine 0.7 mg/kg/day recipients achieved CMIs in ≥ 1 BRIEF-P index [Inhibitory Self-Control (ISCI); Flexibility (FI) and Emergent Metacognition (EMI)] compared with 2 (9%) of 22 placebo recipients [reliable change index (RCI) ≥ 90% certainty]; 9 (53%) of these 17 patients also had RR50. Regarding the individual BRIEF-P indexes/composite, patients in the combined fenfluramine 0.2 and 0.7 mg/kg/day groups were significantly more likely than those in the placebo group to experience CMIs in ICSI (31% vs 5%; p = 0.022), FI (21% vs 0%; p = 0.042) and GEC (21% vs 0%; p = 0.042), but not EMI (15% vs 5%). Patients in the 0.7 mg/kg/day group were significantly more likely than those in the 0.2 mg/kg/day group to experience CMIs in ICSI (50% vs 13%; p = 0.050) and EMI (29% vs 0%; p = 0.042), but not FI (36% vs 13%) or GEC (36% vs 7%) [RCI ≥ 90% certainty]. Treatment with fenfluramine 0.2 or 0.7 mg/kg/day was not associated with significant clinically meaningful worsening (CMW) in any BRIEF-P indexes/composite versus placebo (RCI ≥ 80% certainty) [34].
Longer term, adjunctive fenfluramine provided durable, clinically meaningful MCSF reductions for up to 3 years in the ongoing OLE [27,28,29]. At the time of the most recent efficacy analysis (14 October 2019), 330 participants had been treated with fenfluramine for a median of 631 (range 7–1086) days; 282 and 128 patients had > 12 and > 24 months of drug exposure, respectively [29]. Of note, all patients entering the OLE initiated fenfluramine at a dosage of 0.2 mg/kg/day, irrespective of what dosage (or treatment) they previously received in Study 1 or 2; following the first month of treatment, this was titrated up to a maximum of 0.7 mg/kg/day (maximum daily dosage 26 mg/day)] or 0.4 mg/kg/day in those concomitantly treated with stiripentol (maximum daily dosage 17 mg/day). MCSF was significantly (p < 0.001) reduced by a median of 65% relative to baseline in the core studies. The RR50 and RR75 for MCSF were 63% and 38%; three patients were seizure-free during their entire time in the OLE [29]. Similar results were seen in the subgroup of 91 preschool-aged children (< 6 years) [35].
Thus far, exploration of the longer-term effect of fenfluramine on everyday EF is limited to a post hoc analysis of 58 patients [mean age 11 (range 5–18) years] who had enrolled from Study 1 and completed ≥ 1 year of treatment in the OLE [36]. The patients who had a median reduction in MCSF relative to baseline in the core study of 75%, were divided into two groups: those who had a ≥ 50% MCSF reduction (n = 45); and those who had a < 50% MCSF reduction (n = 13). Patients in the ≥ 50% MCSF reduction group were significantly more likely than those in the < 50% MCSF reduction group to experience CMIs in the Emotion Regulation Index (ERI; p = 0.002) and the Cognitive Regulation Index (CRI; p = 0.001) of the BRIEF-2nd edition (BRIEF-2) [RCI ≥ 95% certainty] [36].
4.1.2 Real-World Studies
Experience from the EU expanded access programme (EAP) for fenfluramine has provided real-world evidence of its effectiveness against treatment-resistant seizures associated with DS in a clinical practice setting [37]. Consistent with their counterparts in phase III studies (Sect. 4.1.1), the majority of children and adolescents with DS included in this post hoc pooled analysis of EU EAP participants had clinically meaningful reductions in MCSF that were sustained through 12 months of treatment with fenfluramine (Table 2). Moreover, similar results were seen in adults with DS included in this analysis (Table 2) [37]. A total of 149 patients were evaluated (52 from Italy, 78 from Germany, and 19 from Spain and the UK); results for the Italian [38] and German [39] cohorts have also been published separately.
4.2 Lennox-Gastaut Syndrome
Based on the findings of an open-label, phase II pilot study [40], the short-term efficacy of adjunctive fenfluramine against treatment-resistant seizures associated with LGS was evaluated in a randomized, double-blind, placebo-controlled, multinational, phase III trial [41]. Thereafter, the longer-term efficacy of the drug was assessed in an OLE study that enrolled patients who completed the core study [42].
Eligible patients were males and females aged 2–35 years with an Epilepsy Study Consortium-confirmed diagnosis of LGS, a history of seizure onset aged ≤ 11 years, multiple seizure types and abnormal cognitive development who experienced ≥ 2 drop seizures per week during a 4-week baseline observation period, despite receiving stable anticonvulsant therapy (including ≥ 1 but ≤ 4 concomitant ASMs). The study was conducted in North America, Europe and Australia [41].
Following the 4-week baseline, trial participants were randomized and stratified according to body weight (< 37.5 vs ≥ 37.5 kg) to receive placebo, fenfluramine 0.2 mg/kg/day or fenfluramine 0.7 mg/kg/day (uptitrated from 0.2 mg/kg/day over a 2-week period; maximum daily dose 26 mg) on top of their current ASM regimen for a total of 14 weeks [41]. The primary efficacy endpoint was the percent change from baseline in the mean monthly drop seizure frequency (MDSF) during the total treatment period in the fenfluramine 0.7 mg/kg/day group versus the placebo group. Patient demographics and baseline characteristics were comparable across the three treatment arms [41].
Fenfluramine 0.7 mg/kg/day, but not 0.2 mg/kg/day, significantly reduced the mean MDSF relative to placebo; both dosage strengths significantly increased the RR50 (Table 3) [41]. Fenfluramine 0.7 mg/kg/day also significantly (p = 0.003) reduced the frequency of all countable motor seizures during the total treatment period by a median of 26% from baseline. Moreover, a seizure-type subgroup analysis suggested that GTC seizures were the most responsive to fenfluramine. The median percentage differences from placebo in GTC seizure frequency in the 0.2 and 0.7 mg/kg/day groups (n = 38 and 38) were, respectively, − 60% and − 50 % (both p ≤ 0.001) [41].
Fenfluramine improved some aspects of everyday EF in subgroups of children and adolescents aged 6–18 years (n = 137) [43, 44] and adults aged 19–35 years (n = 57) [45], many of whom had high baseline everyday EF impairment, as assessed using the BRIEF-2 and BRIEF-Adult version (BRIEF-A) instruments, respectively (post hoc analyses). Among children and adolescents, approximately twice as many patients in the combined fenfluramine 0.2 and 0.7 mg/kg/day groups (n = 92) achieved a CMI in BRI (24% vs 13%), CRI (27% vs 13%) and GEC (25% vs 11%) compared with those in the placebo group (n = 45) [RCI ≥ 95% certainty] [43]; these effects did not appear to be dose-related [44]. Among adults, patients in the combined fenfluramine 0.2 and 0.7 mg/kg/day groups (n = 18 and 16, respectively) were significantly more likely to experience CMIs in BRI (28% and 25% vs 4%; p = 0.040), MI (28% and 31% vs 4%; p = 0.015) and GEC (33% and 31% vs 9%; p = 0.048), than those in the placebo group (n = 23) [RCI ≥ 90% certainty]; as such, ≈ 1 in 3 fenfluramine recipients achieved CMIs in all aspects of everyday EF [45]. Treatment with fenfluramine 0.2 or 0.7 mg/kg/day was not associated with significant CMW in any BRIEF-2 [44] or -A [45] indexes/composites versus placebo (RCI ≥ 80% certainty).
Longer term, fenfluramine produced sustained, clinically meaningful MDSF reductions for over 1 year in the ongoing OLE [42]. At the time of the most recent interim analysis, 247 participants had been treated with fenfluramine for a median of 364 days; 170 and 142 had up to 12 and 15 months of drug exposure, respectively. All patients started on fenfluramine 0.2 mg/kg/day; after 1 month, this was uptitrated to a maximum of 0.7 mg/kg/day/day (maximum daily dosage 26 mg/day). At months 3, 6, 9, 12 and 15 of the OLE, the MDSF was significantly (p < 0.0001) reduced by a median of 39%, 37%, 43%, 52% and 51%, respectively, relative to baseline in the core study. Over the entire OLE (n = 241), the RR50 and RR75 for MDSF reductions were 31% and 12%; 1% of patients achieved either freedom or near-freedom from drop seizures (i.e. ≤ 1 observed drop seizure). In seizure-type subgroup analyses, the median percentage decrease in the monthly frequency of GTC seizures was 49% (p < 0.0001 vs core study baseline) [42].
5 Tolerability of Fenfluramine
In the phase III clinical trials discussed in Sect. 4, oral fenfluramine was generally well tolerated in patients with DS [24,25,26,27,28,29,30, 46] or LGS [41, 42], both in the short term (14–15 weeks [24,25,26, 30, 41]) and in the longer term (up to 3.5 years [27,28,29, 42, 46]). Real-world tolerability and safety data for fenfluramine were also consistent with the phase III clinical trial data [37].
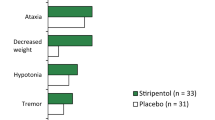
Across the four 14- to 15-week core studies, non-CV treatment-emergent adverse events (TEAEs) were reported by 78–95% of patients receiving fenfluramine 0.2 mg/kg/day and 90–98% of patients receiving either fenfluramine 0.4 mg/kg/day (with stiripentol) or fenfluramine 0.7 mg/kg/day versus 65–96% of those receiving placebo [25, 30, 41]. The drug had a comparable adverse event (AE) profile in patients with DS or LGS [41]. The most common TEAEs (i.e. reported in ≥ 10% of patients in any treatment group in ≥ 3 of the 4 studies) were decreased appetite (20–44% with fenfluramine vs 5–11% with placebo), diarrhoea (11–31% vs 5–8%), fatigue (7–26% vs 2–10%), pyrexia (5–26% vs 8–20%), somnolence (10–17% vs 8–10% [30, 41]), lethargy (2–18% vs 2–5% [25, 30]) and nasopharyngitis (2–18% vs 10–34% [25, 30]) [25, 30, 41]. Most TEAEs were of mild to moderate intensity [24].
Clinically meaningful weight loss (≥ 7% reduction in baseline body weight) occurred in 2% [41] and 13% [24] of patients receiving fenfluramine 0.2 mg/kg/day versus 8–21% of those receiving fenfluramine 0.4 (with stiripentol) or 0.7 mg/kg/day versus 2–5% of those receiving placebo [24, 25, 41]. Thus, similar to decreased appetite (i.e. 20–26% with fenfluramine 0.2 mg/kg/day vs 36–44% with fenfluramine 0.7 mg/kg/day [25, 30, 41]), weight loss with fenfluramine appeared to be dose-related [8, 9].
Serious non-CV TEAEs were reported by 4–14% of patients receiving fenfluramine 0.2, 0.4 (with stiripentol) or 0.7 mg/kg/day versus 4–16% of those receiving placebo across the four core studies; treatment discontinuations due to ≥ 1 TEAEs occurred in 0–13% versus 0–2% [25, 30, 41].
The AE profile of fenfluramine during longer-term treatment in the OLEs was largely consistent with that during short-term treatment in the core studies [27,28,29,30, 41, 42, 46]. Moreover, the TEAEs of decreased appetite and weight loss appeared to resolve over time and/or could be effectively managed while continuing fenfluramine [27]. For example, at the time of the earliest interim analysis of the OLE study for participants with DS (n = 232; median treatment duration 256 days), 37 (16%) patients developed decreased appetite and 31 (13%) patients lost ≥ 7% of their body weight at some time during the OLE. However, ≈ 50% of those with appetite loss subsequently experienced its recovery over a median of 30 days in the study, while ≈ 40% of those with ≥ 7% weight loss subsequently experienced its recovery over 1–9 months in the study [27]. Pyrexia (32%), nasopharyngitis (29%), decreased blood glucose (25%), decreased appetite (24%), diarrhoea (20%), upper respiratory tract infection (17%) and seizure (16%) were the most common non-CV TEAEs that had occurred by the time of the latest interim analysis (n = 343; median treatment duration of 827 days) [46].
Fenfluramine had minimal additional impact on the (already impaired) growth of patients aged 2–18 years with DS, based on comparisons of changes in Z-scores for height and weight after 12 and 24 months of treatment in the OLE with historical control data from a reference population with this condition [47].
The assessment of the CV safety of fenfluramine in patients with DS or LGS included the prospective use of serial echocardiography (performed at baseline, after ≈ 6–8 weeks of treatment and at study end in the core studies [24,25,26, 41]; and at study entry, after 4–6 weeks of treatment, and then at 3-month intervals in the OLEs [27, 42, 48, 49]) to monitor cardiac valve function and morphological structure, as well as systolic pulmonary artery pressure (sPAP). VHD was defined as ≥ moderate mitral regurgitation or ≥ mild aortic regurgitation combined with physical signs or symptoms attributable to valve dysfunction; PAH was defined as sPAP > 35 mmHg [49]. No cases of VHD or PAH were observed at any time during treatment with fenfluramine in the core studies [24,25,26, 41], or for up to 1 and 3.5 years in the OLEs for participants with LGS [42] and DS [46], respectively. All echocardiographic examinations revealed valvular function within the normal physiological range in all patients throughout the trials [24,25,26, 29, 30, 41, 49]. Cardiac monitoring via echocardiogram is required before and every 6 months (for the first 2 years and then annually thereafter) during fenfluramine treatment in the EU [8]; and before, every 6 months during, and 3–6 months after finishing, fenfluramine treatment in the USA (black box warning) [9].
It should be noted that fenfluramine may cause mydriasis and precipitate angle closure glaucoma; patients with acute decreases in visual acuity or ocular pain could consider discontinuing treatment [8, 9]. In addition, ASMs, including fenfluramine may increase the risk of suicidal behaviour and ideation; patients treated with fenfluramine should therefore be monitored for signs of suicidal behaviour or ideation [8, 9].
6 Dosage and Administration of Fenfluramine
Oral fenfluramine is approved in the EU and USA for the treatment of seizures associated with DS and LGS (as an add-on therapy to other ASMs in the EU) in patients aged ≥ 2 years [8, 9]. Fenfluramine is administered as an oral solution twice daily (in two equally divided doses), with or without food. In patients with DS or LGS who are not receiving stiripentol, the recommended starting dosage of fenfluramine of 0.2 mg/kg/day is up-titrated at 7-day intervals to 0.4 mg/kg/day, followed by a further increase to 0.7 mg/kg/day [8, 9]. In patients with DS or LGS who are already receiving stiripentol, the recommended starting dosage of fenfluramine of 0.2 mg/kg/day is up-titrated after 4 or 7 days (depending on the required rapidity of titration) to a maintenance dosage of 0.4 mg/kg/day in the EU [8]. Dosage recommendations for patients with DS or LGS who are already receiving stiripentol plus clobazam in the USA are the same as those in the EU, with the exception that the starting dosage of fenfluramine is increased (at 7-day intervals) first to 0.3 mg/kg/day and finally to 0.4 mg/kg/day [9]. The maximum daily doses of fenfluramine with and without concomitant stiripentol (plus clobazam in the USA) are 17 and 26 mg, respectively [8, 9]. The dosage may be increased based on clinical response to the recommended maximum dosage in patients with DS, and the dosage should be increased as tolerated to the recommended maintenance dosage in patients with LGS [8, 9].
In the EU, dosage adjustments are not recommended in patients with kidney impairment (although a slower titration may be considered) and the use of fenfluramine is not recommended in patients with moderate or severe liver impairment [8]. In the USA, the maximum daily dose of fenfluramine without concomitant stiripentol is 20 mg in patients with concomitant use of a strong CYP1A2 or CYP2D6 inhibitor, those with mild or moderate liver impairment and those with severe kidney impairment; the maximum daily dose is 17 mg in patients with severe liver impairment [9]. The maximum daily doses of fenfluramine with concomitant stiripentol plus clobazam are 17, 13 and 17 mg, respectively, in patients with concomitant use of a strong CYP1A2 or CYP2D6 inhibitor, those with mild liver impairment and those with severe kidney impairment, with its use not recommended in patients with moderate or severe liver impairment [9].
Consult local prescribing information for full details concerning the use of fenfluramine, including dosage administration, contraindications, special warnings and precautions, use in special patient populations, including pregnancy and breast feeding, and potential drug-drug interactions.
7 Place of Fenfluramine in the Management of Dravet and Lennox-Gastaut Syndromes
Fenfluramine, having been successfully repositioned from an appetite suppressant (Sect. 1), is a novel ASM thought to reduce seizures in patients with DS and LGS through a combination of inducing 5-HT release, agonism at 5-HT receptors (primarily 5-HT1D, 5-HT2A and 5-HT2C) and activities at σ1-Rs (Sect. 2). This proposed dual mechanism of action (i.e. involving both serotonergic and non-serotonergic activities) not only differentiates fenfluramine from other types of ASMs [1, 2, 6, 13], but also from other serotonergic drugs (e.g. selective serotonin reuptake inhibitors), which have shown only marginal or inconsistent reductions in seizures in patients with DS [7].
In phase III studies, short-term (14–15 weeks) adjunctive treatment with fenfluramine at the maximum recommended maintenance dosage reduced the MCSF by > 50% and > 60% more than placebo in patients (children and adolescents) with DS whose seizures were inadequately controlled by their existing ASM regimen that contained or did not contain stiripentol, respectively (Sect. 4.1). Fenfluramine also reduced the MDSF by ≈ 20% more than placebo in patients (children, adolescents and adults) with LGS whose seizures were inadequately controlled by their existing ASM regimen (Sect. 4.2). The marked reduction in day-to-day seizure burden in patients with DS was characterized by increases in the number of seizure-free days and in the interval between seizures (Sect. 4.1). Longer term, fenfluramine provided sustained, clinically meaningful reductions in the MCSF in patients with DS for up to 3 years (Sect. 4.1) and in the MDSF in patients with LGS for up to 1 year (Sect. 4.2) in ongoing OLEs.
In seizure subtype analyses in patients with DS and LGS, fenfluramine substantially reduced the frequency of GTCs (Sect. 4), which are the leading risk factor for sudden unexplained death in epilepsy (SUDEP) [50]. Indeed, the SUDEP mortality rate among patients with DS who received fenfluramine in phase III studies, the EU or USA EAPs or two long-term observational studies in Belgium (n = 732; 1185.3 person-years of exposure) was markedly lower than that in literature reports [51]. Further data assessing the use of fenfluramine in reducing the SUDEP mortality risk would be of interest.
As well as treating seizures, managing the main cognitive and behavioural comorbidities of DEEs is important, as these also have a profound impact on the QOL of patients and their caregivers that tends to exceed that of the seizures as the patients grow [52, 53]. In this regard, many preschool-aged children with DEEs develop deficits in EF (i.e. self-regulation of cognition, emotion and behaviour) during this important period of neurodevelopment that can lead to reduced QOL and poor adaptive functioning later in life [34]. Interestingly, evidence from mostly post hoc exploratory (‘hypothesis-generating’) analyses suggests that fenfluramine is associated with CMIs in aspects of everyday EF in preschool-aged children with DS, school-aged children and adolescents with DS or LGS, and adults with LGS after only 14–15 weeks, as well as in school-aged children and adolescents with DS at 1 year (Sect. 4). In particular, in the preschool DS population, fenfluramine was associated with dose-dependent CMIs in ≥ 1 aspect of everyday EF that could not be entirely attributed to improved seizure control, suggesting that the drug may have direct effects on this non-seizure outcome [34]. Moreover, findings for the adult LGS population suggest that fenfluramine treatment may improve everyday EF even when started late in neurodevelopment [45]. Prospective studies with predefined endpoints are warranted to confirm the benefits of fenfluramine on everyday EF in the various age groups of patients with DS or LGS and to evaluate the long-term impact of early treatment (e.g. in preschool-aged children) on QOL and comorbidities [5].
Fenfluramine was generally well tolerated as a low-dose adjunctive treatment for seizures in patients with DS or LGS, both in the short term (14–15 weeks) and in the longer term (up to 1–3.5 years) (Sect. 5). Consistent with the drug being previously marketed as an appetite suppressant, decreased appetite was the most common TEAE in clinical trials and the EU EAP (Sect. 5). However, decreased appetite did not correlate with clinically meaningful weight loss in clinical trials [24, 25, 41]. Moreover, despite careful monitoring of CV safety during the drug (re)development process, no evidence of the VHD or PAH that led to the previous withdrawal of high-dose fenfluramine as an appetite suppressant has thus far been detected with the drug as a low-dose adjunctive ASM (Sect. 5). Echocardiogram monitoring for VHD and PAH is, nonetheless, required prior to, during and after fenfluramine treatment (Sect. 5). Like decreased appetite, weight loss caused by fenfluramine often resolves over time while continuing treatment and, notably, no long-term effects on weight and growth were seen in preschool- and school-aged children and adolescents with DS who received the drug for ≥ 2 years (Sect. 5).
The first fully published evaluations of the real-world effectiveness and tolerability of fenfluramine involve patients with DS enrolled in the EU EAP (Sect. 4.1.2) [37,38,39]. Not only do the data suggest that the anti-seizure benefits of fenfluramine seen in children and adolescents with DS in phase III clinical trials translate to their counterparts in clinical practice, but also that they extend to adults (who were not included in the original phase III studies). Moreover, whereas ASM regimens were required to be stable in clinical trials, approximately half of patients receiving fenfluramine in the EU EAP were able to either reduce the dose of, or discontinue, a concomitant ASM [37]. Real-world data on the effectiveness of fenfluramine in patients with LGS are duly awaited. Additional evidence for the real-world benefits on QOL from the perspective of caregivers/family members of patients with DEEs (which may not be captured in clinical trials) is also desirable, as this will further assist in determining the full impact of fenfluramine therapy [54].
As set out in a therapeutic algorithm prepared at a recent International DS Consensus, fenfluramine, like stiripentol and clobazam, is considered a second-line therapy behind first-line valproate [53]. Cannabidiol, another novel adjunctive ASM with a distinct mechanism of action (modulation of intracellular calcium and adenosine-mediated signalling [1, 2]), is regarded as a third-line therapy [53]. This placement of fenfluramine relative to stiripentol and cannabidiol concurs with the results of two network meta-analyses of ≥ 2 of these adjunctive ASMs, which have been performed in the absence of direct head-to-head trials [55, 56]. One found fenfluramine and stiripentol to be comparably effective and both more effective than cannabidiol, while fenfluramine was better tolerated than stiripentol followed by cannabidiol with respect to serious TEAEs [55]. The other also found fenfluramine to be more effective than cannabidiol, as well as better tolerated with respect to somnolence [56]. Pharmacoeconomic considerations may also favour fenfluramine over cannabidiol (with clobazam) for the treatment of seizures associated with DS, as the former extendedly dominated the latter in a cost-effectiveness analysis conducted in the UK [57], where fenfluramine (like cannabidiol/clobazam) has been recommended for adjunctive use by the National Institute of Health and Care Excellence in accordance with its EU-approved indication [58]. Currently, there is no standard treatment algorithm for LGS [6] and no relevant cost-effectiveness data for fenfluramine.
In conclusion, adjunctive fenfluramine is a novel and effective treatment for pharmacoresistant seizures associated with DS and LGS that may also improve aspects of everyday EF in some patients.
Data Selection Fenfluramine: 195 records identified
Duplicates removed | 5 |
Excluded during initial screening (e.g. press releases; news reports; not relevant drug/indication; preclinical study; reviews; case reports; not randomized trial) | 29 |
Excluded during writing (e.g. reviews; duplicate data; small patient number; nonrandomized/phase I/II trials) | 103 |
Cited efficacy/tolerability articles | 24 |
Cited articles not efficacy/tolerability | 34 |
Search Strategy: EMBASE, MEDLINE and PubMed from 1946 to present. Clinical trial registries/databases and websites were also searched for relevant data. Key words were Fenfluramine, ZX-008, 3-trifluoromethyl-N-ethylamphetamine, Lennox-Gastaut Syndrome, Dravet syndrome, severe myoclonic epilepsy, polymorphic epilepsy. Records were limited to those in English language. Searches last updated 12 May 2023 | |
Change history
01 July 2023
A Correction to this paper has been published: https://doi.org/10.1007/s40265-023-01919-z
References
Strzelczyk A, Schubert-Bast S. Expanding the treatment landscape for Lennox-Gastaut syndrome: current and future strategies. CNS Drugs. 2021;35(1):61–83.
Strzelczyk A, Schubert-Bast S. A practical guide to the treatment of Dravet Syndrome with anti-seizure medication. CNS Drugs. 2022;36(3):217–37.
Samanta D. Changing landscape of Dravet syndrome management: an overview. Neuropediatrics. 2020;51(2):135–45.
Sills GJ, Rogawski MA. Mechanisms of action of currently used antiseizure drugs. Neuropharmacology. 2020;168: 107966.
Sourbron J, Lagae L. Serotonin receptors in epilepsy: novel treatment targets? Epilepsia Open. 2022;7(2):231–46.
Samanta D. Fenfluramine: a review of pharmacology, clinical efficacy, and safety in epilepsy. Children (Basel). 2022;9(8):1159.
Martin P, Reeder T, Sourbron J, et al. An emerging role for sigma-1 receptors in the treatment of developmental and epileptic encephalopathies. Int J Mol Sci. 2021;22(16):1–27.
Zogenix. Fintepla: summary of product characteristics. 2023. https://www.ema.europa.eu/. Accessed 28 Apr 2023.
Zogenix. Fintepla (fenfluramine) oral solution, CIV: US prescribing information. 2023. https://dailymed.nlm.nih.gov/. Accessed 28 Apr 2023.
Pharmaceuticals and Medical Devices Agency. Fintepla Japanese precscribing information. 2022. https://www.pmda.go.jp/. Accessed 28 Apr 2023.
Schoonjans AS, Marchau F, Paelinck BP, et al. Cardiovascular safety of low-dose fenfluramine in Dravet syndrome: a review of its benefit-risk profile in a new patient population. Curr Med Res Opin. 2017;33(10):1773–81.
Odi R, Invernizzi RW, Gallily T, et al. Fenfluramine repurposing from weight loss to epilepsy: what we do and do not know. Pharmacol Ther. 2021;226: 107866.
Schoonjans AS, Ceulemans B. A critical evaluation of fenfluramine hydrochloride for the treatment of Dravet syndrome. Expert Rev Neurother. 2022;22(5):351–64.
Reeder T, Martin P, Sourbron J, et al. Dual activity of fenfluramine (Fintepla®) as a serotonin receptor agonist and positive sigma-1 receptor modulator: implication for disease modification in developmental and epileptic encephalopathies [poster no. 27C]. In: 76th AES Annual Meeting. 2022.
Fuller R, Snoddy H, Robertson D. Mechanisms of effects of d-fenfluramine on brain serotonin metabolism in rats: uptake inhibition versus release. Pharmacol Biochem Behav. 1988;30:715–21.
Rodríguez-Muñoz M, Sánchez-Blázquez P, Garzón J. Fenfluramine diminishes NMDA receptor-mediated seizures via its mixed activity at serotonin 5HT2A and type 1 sigma receptors. Oncotarget. 2018;9(34):23373–89.
Gentsch K, Heinemann U, Schmitz B, et al. Fenfluramine blocks low-Mg2+-induced epileptiform activity in rat entorhinal cortex. Epilepsia. 2005;41(8):925–8.
Sourbron J, Smolders I, de Witte P, et al. Pharmacological analysis of the anti epileptic mechanisms of fenfluramine in scn1a mutant zebrafish. Front Pharmacol. 2017;8:191.
Tupal S, Faingold CL. Serotonin 5-HT4 receptors play a critical role in the action of fenfluramine to block seizure-induced sudden death in a mouse model of SUDEP. Epilepsy Res. 2021;177: 106777.
Li J, Nelis M, Sourbron J, et al. Efficacy of fenfluramine and norfenfluramine enantiomers and various antiepileptic drugs in a zebrafish model of Dravet syndrome. Neurochem Res. 2021;46(9):2249–61.
Martin P, Maurice T, Gammaitoni A, et al. Fenfluramine modulates the anti-amnesic effects induced by sigma-1 receptor agonists and neuro(active)steroids in vivo. Epilepsy Behav. 2022;127(108526):1–13.
Gammaitoni A, Smith S, Boyd B. The lack of effect of food on the pharmacokinetics of ZX008 (Fenfluramine oral solution): results of a single-dose, two-period crossover study. Clin Ther. 2018;40(8):1338–46.
Boyd B, Smith S, Gammaitoni A, et al. A phase I, randomized, open-label, single-dose, 3-period crossover study to evaluate the drug-drug interaction between ZX008 (fenfluramine HCl oral solution) and a regimen of stiripentol, clobazam, and valproate in healthy subjects. Int J Clin Pharmacol Ther. 2019;57(1):11–9.
Lagae L, Sullivan J, Knupp K, et al. Fenfluramine hydrochloride for the treatment of seizures in Dravet syndrome: a randomised, double-blind, placebo-controlled trial. Lancet. 2019;394(10216):2243–54.
Nabbout R, Mistry A, Zuberi S, et al. Fenfluramine for treatment-resistant seizures in patients with Dravet syndrome receiving stiripentol-inclusive regimens: a randomized clinical trial. JAMA Neurol. 2020;77(3):300–8.
Sullivan J, Lagae L, Cross H, et al. Fenfluramine (Fintepla) in Dravet syndrome: results of a third randomized, placebo-controlled clinical trial (Study 3) [abstract no. 853 plus poster]. In: 76th AES Annual Meeting. 2020.
Sullivan J, Scheffer IE, Lagae L, et al. Fenfluramine HCl (Fintepla®) provides long-term clinically meaningful reduction in seizure frequency: analysis of an ongoing open-label extension study. Epilepsia. 2020;61(11):2396–404.
Sullivan J, Auvin S, Pringsheim M, et al. Long-term (2-year) safety and efficacy of adjunctive ZX008 (fenfluramine hydrochloride oral solution) for Dravet syndrome: interim results of an ongoing open-label extension study [abstract]. Neurology. 2020;94(15 Suppl):4684.
Scheffer IE, Devinsky O, Perry MS, et al. Efficacy and tolerability of adjunctive Fintepla (fenfluramine HCl) in an open-label extension study of Dravet syndrome patients treated for up to 3 years [abstract no. 978 plus poster]. In: 74th AES Annual Meeting. 2020.
Sullivan J, Specchio N, Devinsky O, et al. Using a time-to-event analysis to measure treatment effect of fenfluramine (Fintepla®) on seizure-free days post-hoc analysis of two phase 3 studies in Dravet Syndrome [poster no. 385]. In: 14th EPNS Annual Meeting. 2022.
Sullivan J, Perry MS, Wheless JW, et al. Fenfluramine responder analyses and numbers needed to treat: translating epilepsy trial data into clinical practice. Eur J Paediatr Neurol. 2021;31:10–4.
Sullivan J, Specchio N, Devinsky O, et al. Fenfluramine significantly reduces day-to-day seizure burden by increasing number of seizure-free days and time between seizures in patients with Dravet syndrome: a time-to-event analysis. Epilepsia. 2022;63(1):130–8.
Devinsky O, Cross JH, Gil-Nagel A, et al. ZX008 (fenfluramine HCl oral solution) significantly reduces frequency of generalized tonic-clonic seizures in Dravet syndrome: pooled analysis from two phase 3 clinical trials [abstract no. 41 plus poster]. Ann Neurol. 2019;86(Suppl 23):S59-60.
Bishop KI, Isquith PK, Gioia GA, et al. Fenfluramine treatment is associated with improvement in everyday executive function in preschool-aged children (<5 years) with Dravet syndrome: a critical period for early neurodevelopment. Epilepsy Behav. 2023;138: 108994.
Lagae L, Auvin S, Knupp K, et al. Impact of fenfluramine on convulsive seizure frequency in young (< 6 years old) patients with dravet syndrome: a long-term open-label study [abstract no. 527]. Epilepsia. 2021;62(Suppl 3):282–3.
Bishop KI, Isquith PK, Gioia GA, et al. Improved everyday executive functioning following profound reduction in seizure frequency with fenfluramine: analysis from a phase 3 long-term extension study in children/young adults with Dravet syndrome. Epilepsy Behav. 2021;121(Pt A):1–9.
Guerrini R, Specchio N, Aledo-Serrano Á, et al. An examination of the efficacy and safety of fenfluramine in adults, children, and adolescents with Dravet syndrome in a real-world practice setting: a report from the fenfluramine European Early Access Program. Epilepsia Open. 2022;7(4):578–87.
Specchio N, Pietrafusa N, Doccini V, et al. Efficacy and safety of fenfluramine hydrochloride for the treatment of seizures in Dravet syndrome: a real-world study. Epilepsia. 2020;61(11):2405–14.
Strzelczyk A, Pringsheim M, Mayer T, et al. Efficacy, tolerability, and retention of fenfluramine for the treatment of seizures in patients with Dravet syndrome: compassionate use program in Germany. Epilepsia. 2021;62(10):2518–27.
Lagae L, Schoonjans AS, Gammaitoni AR, et al. A pilot, open-label study of the effectiveness and tolerability of low-dose ZX008 (fenfluramine HCl) in Lennox-Gastaut syndrome. Epilepsia. 2018;59(10):1881–8.
Knupp KG, Scheffer IE, Ceulemans B, et al. Efficacy and safety of fenfluramine for the treatment of seizures associated with Lennox-Gastaut syndrome: a randomized clinical trial. JAMA Neurol. 2022;79(6):554–64.
Knupp KG, Scheffer IE, Ceulemans B, et al. Fenfluramine provides clinically meaningful reduction in frequency of drop seizures in patients with Lennox-Gastaut syndrome: interim analysis of an open-label extension study. Epilepsia. 2023;64(1):139–51.
Bishop K, Isquith P, Gioia G, et al. Fenfluramine treatment improves everyday executive functioning in patients with Lennox-Gastaut syndrome: analysis from a phase 3 clinical trial [presentation]. In: 73rd AAN Annual Meeting. 2021.
Bishop K, Isquith P, Gioia G, et al. Fenfluramine (Fintepla®) treatment improves everyday executive functioning in patients with Lennox-Gastaut syndrome: analysis from a phase 3 clinical trial [abstract no. P12-8.004 plus poster]. Neurology. 2022;98(15 Suppl).
Polega S, Bishop K, Isquith P, et al. Fenfluramine treatment is associated with improvement in everyday executive function in adults with Lennox-Gastaut syndrome: post-hoc analysis of dose effects from a phase 3 trial rationale [abstract no. 3.411]. In: 76th AES Annual Meeting. 2022.
Scheffer I, Devinsky O, Thiele E, et al. Interim safety analysis of an ongoing open-label extension study of fenfluramine for Dravet syndrome [abstract no. 3.412]. In: 76th AES Annual Meeting. 2022.
Gil-Nagel A, Sullivan J, Ceulemans B, et al. Treatment with fenfluramine in patients with Dravet syndrome has no long-term effects on weight and growth. Epilepsy Behav. 2021;122(108212):1–6.
Lai WW, Galer BS, Wong PC, et al. Cardiovascular safety of fenfluramine in the treatment of Dravet syndrome: analysis of an ongoing long-term open-label safety extension study. Epilepsia. 2020;61(11):2386–95.
Agarwal A, Farfel GM, Gammaitoni AR, et al. Long-term cardiovascular safety of fenfluramine in patients with Dravet syndrome treated for up to 3 years: findings from serial echocardiographic assessments. Eur J Paediatr Neurol. 2022;39:35–9.
DeGiorgio CM, Curtis A, Hertling D, et al. Sudden unexpected death in epilepsy: risk factors, biomarkers, and prevention. Acta Neurol Scand. 2019;139(3):220–30.
Cross JH, Galer BS, Gil-Nagel A, et al. Impact of fenfluramine on the expected SUDEP mortality rates in patients with Dravet syndrome. Seizure. 2021;93:154–9.
Marchese F, Cappelletti S, Filippini M, et al. Comorbidities in Dravet syndrome and Lennox-Gastaut syndrome. Comp Clin Med. 2021;3:2167–79.
Wirrell EC, Hood V, Knupp KG, et al. International consensus on diagnosis and management of Dravet syndrome. Epilepsia. 2022;63(7):1761–77.
Jensen MP, Gammaitoni AR, Galer BS, et al. Fenfluramine treatment for Dravet syndrome: real-world benefits on quality of life from the caregiver perspective. Epilepsy Res. 2022;185: 106976.
Devi N, Madaan P, Asrar MM, et al. Comparative short-term efficacy and safety of add-on anti-seizure medications in Dravet syndrome: an indirect treatment comparison. Seizure. 2021;91:316–24.
Linley W, Hawkins N, Schwenkglenks M, et al. Comparative effectiveness of fenfluramine vs cannabidiol for the treatment of seizures in Dravet syndrome (DS): a network meta-analysis (NMA) [abstract no. 324]. Epilepsia. 2021;62(Suppl 3):154.
Weston G, Pinsent A, Adams E, et al. A cost-effectiveness analysis of fenfluramine for the treatment of seizures for patients with Dravet syndrome (DS) in the UK setting [abstract no. PND33]. Value Health. 2021;24(Suppl 1):S164–5.
Wijnen B, Witlox W, Wolff R, et al. Fenfluramine for treating Dravet syndrome: an evidence review group perspective of a NICE Single Technology Appraisal. Pharmacoeconomics. 2023;41(1):33–42.
Acknowledgments
During the peer review process, the manufacturer of fenfluramine was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Authorship and Conflict of interest
James E. Frampton is a salaried employee of Adis International Ltd/Springer Nature, and declares no relevant conflicts of interest. All authors contributed to the review and are responsible for the article content.
Ethics approval, Consent to participate, Consent to publish, Availability of data and material, Code availability
Not applicable.
Additional information
The manuscript was reviewed by: L. Lagae, Department of Paediatric Neurology, University of Leuven, Leuven, Belgium; S. Lattanzi, Department of Experimental and Clinical Medicine, Marche Polytechnic University, Ancona, Italy; D. Mandelbaum, Departments of Neurology and Pediatrics, Alpert Medical School of Brown University, Providence, RI, USA; T. Martino, Neuroscience department, SC Ospedaliera of Neurology and Stroke Unit, Policlinico Riuniti of Foggia, Italy; M. Mula, St George's University Hospitals NHS Foundation Trust, London, UK.
The original article has been revised due to retrospective open choice order.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Frampton, J.E. Fenfluramine: A Review in Dravet and Lennox-Gastaut Syndromes. Drugs 83, 923–934 (2023). https://doi.org/10.1007/s40265-023-01881-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-023-01881-w