Abstract
Background
Pharmacological treatment is common in practice and widely used for the management of insomnia. However, evidence comparing the relative effectiveness, safety, and certainty of evidence among drug classes and individual drugs for insomnia are still lacking. This study aimed to determine the relative effectiveness, safety, and tolerability of drugs for insomnia.
Methods
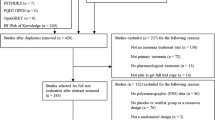
In this systematic review and network meta-analysis we systematically searched PubMed, Embase, Cochrane Central Register of Controlled Trials, PsycINFO, and ClinicalTrials.gov, from inception to January 10, 2022 to identify randomized controlled trials that compared insomnia drugs with placebo or an active comparator in adults with insomnia. We conducted random-effects frequentist network meta-analyses to summarize the evidence, and used the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach to assess the certainty, categorize interventionsand present the findings.
Results
A total of 148 articles met our eligibility criteria; these included 153 trials which enrolled 46,412 participants and assessed 36 individual drugs from eight drug classes. Compared with placebo, both subjectively and objectively measured total sleep time were significantly improved with non-benzodiazepine (subjective: mean difference [MD] 25.07, 95% confidence interval [CI] 15.49–34.64, low certainty; objective: MD 22.34, 95% CI 7.64–37.05, high certainty), antidepressants (subjective: MD 54.40, 95% CI 34.96–75.83, low certainty; objective: MD 35.64, 95% CI 13.05–58.24, high certainty), and orexin receptor antagonists (subjective: MD 21.62, 95% CI 0.84–42.40, high certainty; objective: MD 31.81, 95% CI 2.66–60.95, high certainty); of which doxepin, almorexant, suvorexant, and lemborexant were among the relatively effective drugs with relatively good tolerability and lower risks of any adverse events (AEs). Both subjectively and objectively measured sleep onset latency were significantly shortened with non-benzodiazepines (subjective: MD − 10.12, 95% CI − 13.84 to − 6.40, moderate certainty; objective: MD − 12.11, 95% CI − 19.31 to − 4.90, moderate certainty) and melatonin receptor agonists (subjective: MD − 7.73, 95% CI − 15.21 to − 0.26, high certainty; objective: MD − 7.04, 95% CI − 12.12 to − 1.95, moderate certainty); in particular, zopiclone was among the most effective drugs with a lower risk of any AEs but worse tolerability. Non-benzodiazepines could significantly decrease both subjective and objective measured wake time after sleep onset (subjective: MD − 16.67, 95% CI − 21.79 to − 11.56, moderate certainty; objective: MD − 13.92, 95% CI − 22.71 to − 5.14, moderate certainty).
Conclusions
Non-benzodiazepines probably improve total sleep time, sleep onset latency, and wake time after sleep onset. Other insomnia drug classes and individual drugs also showed potential benefits in improving insomnia symptoms. However, the choice of insomnia drugs should be based on the phenotype of insomnia presented, as well as each drug’s safety and tolerability.
Protocol registration PROSPERO (CRD42019138790).





Similar content being viewed by others
References
Morin CM, Vézina-Im LA, Ivers H, et al. Prevalent, incident, and persistent insomnia in a population-based cohort tested before (2018) and during the first-wave of COVID-19 pandemic (2020). Sleep. 2022;45(1):zsab258. https://doi.org/10.1093/sleep/zsab258.
Ge L, Guyatt G, Tian J, et al. Insomnia and risk of mortality from all-cause, cardiovascular disease, and cancer: systematic review and meta-analysis of prospective cohort studies. Sleep Med Rev. 2019;48: 101215. https://doi.org/10.1016/j.smrv.2019.101215.
Laugsand LE, Vatten LJ, Platou C, Janszky I. Insomnia and the risk of acute myocardial infarction: a population study. Circulation. 2011;124:2078–81. https://doi.org/10.1161/CIRCULATIONAHA.111.025858.
Troxel WM, Buysse DJ, Matthews KA, et al. Sleep symptoms predict the development of the metabolic syndrome. Sleep. 2010;33(12):1633–40. https://doi.org/10.1093/sleep/33.12.1633.
Vgontzas AN, Liao D, Bixler EO, et al. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. 2009;32:491–7. https://doi.org/10.1093/sleep/32.4.491.
Kleinman NL, Brook RA, Doan JF, et al. Health benefit costs and absenteeism due to insomnia from the employer’s perspective: a retrospective, case-control, database study. J Clin Psychiatry. 2009;70(8):1098–104. https://doi.org/10.4088/JCP.08m04264.
Leger D, Scheuermaier K, Philip P, et al. SF-36: evaluation of quality of life in severe and mild insomniacs compared with good sleepers. Psychosom Med. 2001;63(1):49–55. https://doi.org/10.1097/00006842-200101000-00006.
Walsh JK. Clinical and socioeconomic correlates of insomnia. J Clin Psychiatry. 2004;65(Suppl 8):13–9.
Bolge SC, Doan JF, Kannan H, Baran RW. Association of insomnia with quality of life, work productivity, and activity impairment. Qual Life Res. 2009;18(4):415–22. https://doi.org/10.1007/s11136-009-9462-6.
Kessler RC, Berglund PA, Coulouvrat C, et al. Insomnia, comorbidity, and risk of injury among insured Americans: results from the America Insomnia Survey. Sleep. 2012;35(6):825–34. https://doi.org/10.5665/sleep.1884.
Ford ES, Wheaton AG, Cunningham TJ, et al. Trends in outpatient visits for insomnia, sleep apnea, and prescriptions for sleep medications among US adults: findings from the National Ambulatory Medical Care survey 1999–2010. Sleep. 2014;37(8):1283–93. https://doi.org/10.5665/sleep.3914.
Lee MH, Choi JW, Lee J, et al. Trends in prescriptions for sedative-hypnotics among Korean adults: a nationwide prescription database study for 2011–2015. Soc Psychiatry Psychiatr Epidemiol. 2019;54(4):477–84. https://doi.org/10.1007/s00127-018-1615-x.
Zhu H, Li M, Pan B, et al. A critical appraisal of clinical practice guidelines on insomnia using the RIGHT statement and AGREE II instrument. Sleep Med. 2022;100:244–53. https://doi.org/10.1016/j.sleep.2022.08.023.
Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675–700. https://doi.org/10.1111/jsr.12594.
Sateia MJ, Buysse DJ, Krystal AD, et al. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017;13(2):307–49. https://doi.org/10.5664/jcsm.6470.
Sparks A, Cohen A, Arnold B, et al. Insomnia guideline. Kaiser Permanente; 2019. https://wa.kaiserpermanente.org/static/pdf/public/guidelines/insomnia.pdf. Accessed 1 July 2021.
Artiach González G, Isabel Díaz del Campo, et al. Clinical practice guidelines for the management of patients with insomnia in primary care. 2009.
Holbrook AM, Crowther R, Lotter A, et al. Meta-analysis of benzodiazepine use in the treatment of insomnia. CMAJ. 2000;162(2):225–33.
Huedo-Medina TB, Kirsch I, Middlemass J, et al. Effectiveness of non-benzodiazepine hypnotics in treatment of adult insomnia: meta-analysis of data submitted to the Food and Drug Administration. BMJ. 2012;345: e8343. https://doi.org/10.1136/bmj.e8343.
Rösner S, Englbrecht C, Wehrle R, et al. Antidepressants for insomnia in adults. Cochrane Database Syst Rev. 2018;5(5):CD010753. https://doi.org/10.1002/14651858.CD010753.pub2.
Xue T, Wu X, Chen S, et al. The efficacy and safety of dual orexin receptor antagonists in primary insomnia: a systematic review and network meta-analysis. Sleep Med Rev. 2022;61: 101573. https://doi.org/10.1016/j.smrv.2021.101573.
Xu H, Zhang C, Qian Y, et al. Efficacy of melatonin for sleep disturbance in middle-aged primary insomnia: a double-blind, randomised clinical trial. Sleep Med. 2020;76:113–9. https://doi.org/10.1016/j.sleep.2020.10.018.
McElroy H, O’Leary B, Adena M, et al. Comparative efficacy of lemborexant and other insomnia treatments: a network meta-analysis. J Manag Care Spec Pharm. 2021;27(9):1296–308. https://doi.org/10.18553/jmcp.2021.21011.
Ge L, Tian JH, Li YN, et al. Association between prospective registration and overall reporting and methodological quality of systematic reviews: a meta-epidemiological study. J Clin Epidemiol. 2018;93:45–55. https://doi.org/10.1016/j.jclinepi.2017.10.012.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4.
Ebrahim S, Johnston BC, Akl EA, et al. Addressing continuous data measured with different instruments for participants excluded from trial analysis: a guide for systematic reviewers. J Clin Epidemiol. 2014;67(5):560–70. https://doi.org/10.1016/j.jclinepi.2013.11.014.
Evidence Partners. 2011. Methodological resources. https://www.evidencepartners.com/resources/methodological-resources/.
Furukawa TA, Barbui C, Cipriani A, et al. Imputing missing standard deviations in meta-analyses can provide accurate results. J Clin Epidemiol. 2006;59(1):7–10. https://doi.org/10.1016/j.jclinepi.2005.06.006.
Rücker G, Schwarzer G, Krahn U. netmeta: network meta-analysis using Frequentist methods. https://cran.r-project.org/web/packages/netmeta/netmeta.pdf. Accessed 28 July 2019.
Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29:932–44. https://doi.org/10.1002/sim.3767.
Rücker G, Schwarzer G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol. 2015;15:58. https://doi.org/10.1186/s12874-015-0060-8.
Puhan MA, Schünemann HJ, Murad MH, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:g5630. https://doi.org/10.1136/bmj.g5630.
Brignardello-Petersen R, Bonner A, Alexander PE, et al. Advances in the GRADE approach to rate the certainty in estimates from a network meta-analysis. J Clin Epidemiol. 2018;93:36–44. https://doi.org/10.1016/j.jclinepi.2017.10.005.
Chaimai A, Caldwell DM, Li T, Higgins J, Salanti G. Chapter 11: undertaking network meta-analyses. In: Higgins J, Thomas J, Chandler J, et al, editors. Cochrane Handbook for Systematic Reviews of Interventions version 61. 2020. www.training.cochrane.org/handbook2020.
Brignardello-Petersen R, Florez ID, Izcovich A, et al. GRADE approach to drawing conclusions from a network meta-analysis using a minimally contextualised framework. BMJ. 2020;371:m3900. https://doi.org/10.1136/bmj.m3900.
De Crescenzo F, D’Alò GL, Ostinelli EG, et al. Comparative effects of pharmacological interventions for the acute and long-term management of insomnia disorder in adults: a systematic review and network meta-analysis. Lancet. 2022;400(10347):170–84. https://doi.org/10.1016/S0140-6736(22)00878-9.
Yue JL, Chang XW, Zheng JW, et al. Efficacy and tolerability of pharmacological treatments for insomnia in adults: a systematic review and network meta-analysis. Sleep Med Rev. 2023;68: 101746. https://doi.org/10.1016/j.smrv.2023.101746.
Choi H, Youn S, Um YH, et al. Korean Clinical Practice Guideline for the diagnosis and treatment of insomnia in adults. Psychiatry Investig. 2020;17(11):1048–59. https://doi.org/10.30773/pi.2020.0146.
Qaseem A, Kansagara D, Forciea MA, et al. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125–33. https://doi.org/10.7326/M15-2175.
Chinese Sleep Research Society. Guidelines for the diagnosis and treatment of insomnia in China. Chin Med J. 2017;6(27):1844–56.
Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84. https://doi.org/10.7326/M14-2385.
Li Y, Cao L, Zhang Z, et al. Reporting and methodological quality of COVID-19 systematic reviews needs to be improved: an evidence mapping. J Clin Epidemiol. 2021;135:17–28. https://doi.org/10.1016/j.jclinepi.2021.02.021.
Turner EH, Matthews AM, Linardatos E, et al. Selective publication of antidepressant trials and its influence on apparent efficacy. N Engl J Med. 2008;358:252–60. https://doi.org/10.1056/NEJMsa065779.
Kunz D, Dauvilliers Y, Benes H, et al. Long-term safety and tolerability of daridorexant in patients with insomnia disorder. CNS Drugs. 2023;37(1):93–106. https://doi.org/10.1007/s40263-022-00980-8.
Mignot E, Mayleben D, Fietze I, et al. Safety and efficacy of daridorexant in patients with insomnia disorder: results from two multicentre, randomised, double-blind, placebo-controlled, phase 3 trials. Lancet Neurol. 2022;21(2):125–39. https://doi.org/10.1016/S1474-4422(21)00436-1.
Tassniyom K, Paholpak S, Tassniyom S, Kiewyoo J. Quetiapine for primary insomnia: a double blind, randomized controlled trial. J Med Assoc Thai. 2010;93(6):729–34.
Lydiard RB, Lankford DA, Seiden DJ, et al. Efficacy and tolerability of modified-release indiplon in elderly patients with chronic insomnia: results of a 2-week double-blind, placebo-controlled trial. J Clin Sleep Med. 2006;2(3):309–15.
Murphy P, Moline M, Mayleben D, et al. Lemborexant, a dual orexin receptor antagonist (DORA) for the treatment of insomnia disorder: results from a Bayesian, adaptive, randomized, double-blind, placebo-controlled study. J Clin Sleep Med. 2017;13(11):1289–99. https://doi.org/10.5664/jcsm.6800.
Buxton OM, Pavlova MK, O’Connor SP, Wang W, Winkelman JW. Lack of change in glucose metabolism in eszopiclone-treated primary insomnia patients. Nat Sci Sleep. 2017;18(9):187–98. https://doi.org/10.2147/NSS.S130505.
Hajak G, Rodenbeck A, Voderholzer U, et al. Doxepin in the treatment of primary insomnia: a placebo-controlled, double-blind, polysomnographic study. J Clin Psychiatry. 2001;62(6):453–63. https://doi.org/10.4088/jcp.v62n0609.
Black J, Pillar G, Hedner J, Polo O, Berkani O, Mangialaio S, Hmissi A, Zammit G, Hajak G. Efficacy and safety of almorexant in adult chronic insomnia: a randomized placebo-controlled trial with an active reference. Sleep Med. 2017;36:86–94. https://doi.org/10.1016/j.sleep.2017.05.009.
Pinto LR Jr, Bittencourt LR, Treptow EC, et al. Eszopiclone versus zopiclone in the treatment of insomnia. Clinics (Sao Paulo). 2016;71(1):5–9. https://doi.org/10.6061/clinics/2016(01)02.
Roehrs TA, Roth T. Gender differences in the efficacy and safety of chronic nightly zolpidem. J Clin Sleep Med. 2016;12(3):319–25. https://doi.org/10.5664/jcsm.5574.
Herring WJ, Connor KM, Ivgy-May N, et al. Suvorexant in patients with insomnia: results from two 3-month randomized controlled clinical trials. Biol Psychiatry. 2016;79(2):136–48. https://doi.org/10.1016/j.biopsych.2014.10.003.
Michelson D, Snyder E, Paradis E, et al. Safety and efficacy of suvorexant during 1-year treatment of insomnia with subsequent abrupt treatment discontinuation: a phase 3 randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2014;13(5):461–71. https://doi.org/10.1016/S1474-4422(14)70053-5.
Ratti E, Carpenter DJ, Zamuner S, et al. Efficacy of vestipitant, a neurokinin-1 receptor antagonist, in primary insomnia. Sleep. 2013;36(12):1823–30. https://doi.org/10.5665/sleep.3208.
Roth T, Krystal A, Steinberg FJ, et al. Novel sublingual low-dose zolpidem tablet reduces latency to sleep onset following spontaneous middle-of-the-night awakening in insomnia in a randomized, double-blind, placebo-controlled, outpatient study. Sleep. 2013;36(2):189–96. https://doi.org/10.5665/sleep.2370.
Randall S, Roehrs TA, Roth T. Efficacy of eight months of nightly zolpidem: a prospective placebo-controlled study. Sleep. 2012;35(11):1551–7. https://doi.org/10.5665/sleep.2208.
Lankford A, Rogowski R, Essink B, et al. Efficacy and safety of doxepin 6 mg in a four-week outpatient trial of elderly adults with chronic primary insomnia. Sleep Med. 2012;13(2):133–8. https://doi.org/10.1016/j.sleep.2011.09.006.
Krystal AD, Lankford A, Durrence HH, et al. Efficacy and safety of doxepin 3 and 6 mg in a 35-day sleep laboratory trial in adults with chronic primary insomnia. Sleep. 2011;34(10):1433–42. https://doi.org/10.5665/SLEEP.1294.
Fan B, Kang J, He Y, et al. Efficacy and safety of suvorexant for the treatment of primary insomnia among Chinese: a 6-month randomized double-blind controlled study. 2017. Neurol. Asia. 2017;22(1):41–7.
Roth AJ, McCall WV, Liguori A. Cognitive, psychomotor and polysomnographic effects of trazodone in primary insomniacs. J Sleep Res. 2011;20(4):552–8. https://doi.org/10.1111/j.1365-2869.2011.00928.x.
Huang YS, Hsu SC, Liu SI, Chen CK. A double-blind, randomized, comparative study to evaluate the efficacy and safety of zaleplon versus zolpidem in shortening sleep latency in primary insomnia. Chang Gung Med J. 2011;34(1):50–6.
Uchimura N, Ogawa A, Hamamura M, et al. Efficacy and safety of ramelteon in Japanese adults with chronic insomnia: a randomized, double-blind, placebo-controlled study. Expert Rev Neurother. 2011;11(2):215–24. https://doi.org/10.1586/ern.10.197.
Ivgy-May N, Hajak G, van Osta G, et al. Efficacy and safety of esmirtazapine in adult outpatients with chronic primary insomnia: a randomized, double-blind placebo-controlled study and open-label extension. J Clin Sleep Med. 2020;16(9):1455–67. https://doi.org/10.5664/jcsm.8526.
Hajak G, Hedner J, Eglin M, et al. Gaboxadol Study 99775 Group. A 2-week efficacy and safety study of gaboxadol and zolpidem using electronic diaries in primary insomnia outpatients. Sleep Med. 2009;10(7):705–12. https://doi.org/10.1016/j.sleep.2008.09.010.
Uchiyama M, Hamamura M, Kuwano T, et al. Evaluation of subjective efficacy and safety of ramelteon in Japanese subjects with chronic insomnia. Sleep Med. 2011;12(2):119–26. https://doi.org/10.1016/j.sleep.2010.08.010.
Xu Z, Jiang X, Li W, et al. Propofol-induced sleep: efficacy and safety in patients with refractory chronic primary insomnia. Cell Biochem Biophys. 2011;60(3):161–6. https://doi.org/10.1007/s12013-010-9135-7.
Krystal AD, Durrence HH, Scharf M, Jochelson P, Rogowski R, Ludington E, Roth T. Efficacy and safety of doxepin 1 mg and 3 mg in a 12-week sleep laboratory and outpatient trial of elderly subjects with chronic primary insomnia. Sleep. 2010;33(11):1553–61. https://doi.org/10.1093/sleep/33.11.1553.
Wade AG, Crawford G, Ford I, et al. Prolonged release melatonin in the treatment of primary insomnia: evaluation of the age cut-off for short- and long-term response. Curr Med Res Opin. 2011;27(1):87–98. https://doi.org/10.1185/03007995.2010.537317.
Ancoli-Israel S, Krystal AD, McCall WV, et al. A 12-week, randomized, double-blind, placebo-controlled study evaluating the effect of eszopiclone 2 mg on sleep/wake function in older adults with primary and comorbid insomnia. Sleep. 2010;33(2):225–34. https://doi.org/10.1093/sleep/33.2.225.
Walsh JK, Salkeld L, Knowles LJ, et al. Treatment of elderly primary insomnia patients with EVT 201 improves sleep initiation, sleep maintenance, and daytime sleepiness. Sleep Med. 2010;11(1):23–30. https://doi.org/10.1016/j.sleep.2009.07.012.
Luthringer R, Muzet M, Zisapel N, Staner L. The effect of prolonged-release melatonin on sleep measures and psychomotor performance in elderly patients with insomnia. Int Clin Psychopharmacol. 2009;24(5):239–49. https://doi.org/10.1097/YIC.0b013e32832e9b08.
Mayer G, Wang-Weigand S, Roth-Schechter B, et al. Efficacy and safety of 6-month nightly ramelteon administration in adults with chronic primary insomnia. Sleep. 2009;32(3):351–60. https://doi.org/10.1093/sleep/32.3.351.
Krystal AD, Erman M, Zammit GK, et al. Long-term efficacy and safety of zolpidem extended-release 12.5 mg, administered 3 to 7 nights per week for 24 weeks, in patients with chronic primary insomnia: a 6-month, randomized, double-blind, placebo-controlled, parallel-group, multicenter study. Sleep. 2008;31(1):79–90. https://doi.org/10.1093/sleep/31.1.79.
Walsh JK, Soubrane C, Roth T. Efficacy and safety of zolpidem extended release in elderly primary insomnia patients. Am J Geriatr Psychiatry. 2008;16(1):44–57. https://doi.org/10.1097/JGP.0b013e3181256b01.
Lemoine P, Nir T, Laudon M, Zisapel N. Prolonged-release melatonin improves sleep quality and morning alertness in insomnia patients aged 55 years and older and has no withdrawal effects. J Sleep Res. 2007;16(4):372–80. https://doi.org/10.1111/j.1365-2869.2007.00613.x.
Roth T, Seiden D, Sainati S, et al. Effects of ramelteon on patient-reported sleep latency in older adults with chronic insomnia. Sleep Med. 2006;7(4):312–8. https://doi.org/10.1016/j.sleep.2006.01.003.
Ivgy-May N, Ruwe F, Krystal A, Roth T. Esmirtazapine in non-elderly adult patients with primary insomnia: efficacy and safety from a randomized, 6-week sleep laboratory trial. Sleep Med. 2015;16(7):838–44. https://doi.org/10.1016/j.sleep.2015.04.001.
Ivgy-May N, Roth T, Ruwe F, Walsh J. Esmirtazapine in non-elderly adult patients with primary insomnia: efficacy and safety from a 2-week randomized outpatient trial. Sleep Med. 2015;16(7):831–7. https://doi.org/10.1016/j.sleep.2015.03.005.
Wade AG, Ford I, Crawford G, et al. Efficacy of prolonged release melatonin in insomnia patients aged 55–80 years: quality of sleep and next-day alertness outcomes. Curr Med Res Opin. 2007;23(10):2597–605. https://doi.org/10.1185/030079907X233098.
Walsh JK, et al. Efficacy and tolerability of indiplon in older adults with primary insomnia. Sleep Med. 2007;8(7–8):753–9.
Zammit G, Erman M, Wang-Weigand S, et al. Evaluation of the efficacy and safety of ramelteon in subjects with chronic insomnia. J Clin Sleep Med. 2007;3(5):495–504.
Walsh JK, Krystal AD, Amato DA, et al. Nightly treatment of primary insomnia with eszopiclone for six months: effect on sleep, quality of life, and work limitations. Sleep. 2007;30(8):959–68. https://doi.org/10.1093/sleep/30.8.959.
Hedner J, Yaeche R, Emilien G, et al. Zaleplon shortens subjective sleep latency and improves subjective sleep quality in elderly patients with insomnia. The Zaleplon Clinical Investigator Study Group. Int J Geriatr Psychiatry. 2000;15(8):704–12. https://doi.org/10.1002/1099-1166(200008)15:8%3c704::aid-gps183%3e3.0.co;2-s.
Scharf MB, Black J, Hull S, et al. Long-term nightly treatment with indiplon in adults with primary insomnia: results of a double-blind, placebo-controlled, 3-month study. Sleep. 2007;30(6):743–52. https://doi.org/10.1093/sleep/30.6.743.
Walsh JK, Perlis M, Rosenthal M, et al. Tiagabine increases slow-wave sleep in a dose-dependent fashion without affecting traditional efficacy measures in adults with primary insomnia. J Clin Sleep Med. 2006;2(1):35–41.
McCall WV, Erman M, Krystal AD, et al. A polysomnography study of eszopiclone in elderly patients with insomnia. Curr Med Res Opin. 2006;22(9):1633–42. https://doi.org/10.1185/030079906X112741.
Roth T, Soubrane C, Titeux L, Walsh JK, Zoladult Study Group. Efficacy and safety of zolpidem-MR: a double-blind, placebo-controlled study in adults with primary insomnia. Sleep Med. 2006;7(5):397–406. https://doi.org/10.1016/j.sleep.2006.04.008.
Wu R, Bao J, Zhang C, et al. Comparison of sleep condition and sleep-related psychological activity after cognitive-behavior and pharmacological therapy for chronic insomnia. Psychother Psychosom. 2006;75(4):220–8. https://doi.org/10.1159/000092892.
Scharf M, Erman M, Rosenberg R, et al. A 2-week efficacy and safety study of eszopiclone in elderly patients with primary insomnia. Sleep. 2005;28(6):720–7. https://doi.org/10.1093/sleep/28.6.720.
Roth T, Walsh JK, Krystal A, et al. An evaluation of the efficacy and safety of eszopiclone over 12 months in patients with chronic primary insomnia. Sleep Med. 2005;6(6):487–95. https://doi.org/10.1016/j.sleep.2005.06.004.
Zammit GK, McNabb LJ, Caron J, et al. Efficacy and safety of eszopiclone across 6-weeks of treatment for primary insomnia. Curr Med Res Opin. 2004;20(12):1979–91. https://doi.org/10.1185/174234304x15174.
Ancoli-Israel S, Walsh JK, Mangano RM, Fujimori M. Zaleplon, a novel nonbenzodiazepine hypnotic, effectively treats insomnia in elderly patients without causing rebound effects. Prim Care Companion J Clin Psychiatry. 1999;1(4):114–20. https://doi.org/10.4088/pcc.v01n0404.
Allain H, Arbus L, Schück S. Efficacy and safety of zolpidem administered as needed in primary insomnia: results of a double-blind, placebo-controlled study. Clin Drug Investig. 2001;21:391–400. https://doi.org/10.2165/00044011-200121060-00001.
Krystal AD, Walsh JK, Laska E, et al. Sustained efficacy of eszopiclone over 6 months of nightly treatment: results of a randomized, double-blind, placebo-controlled study in adults with chronic insomnia. Sleep. 2003;26(7):793–9. https://doi.org/10.1093/sleep/26.7.793.
Walsh JK. Zolpidem “as needed” for the treatment of primary insomnia: a double-blind, placebo-controlled study. Sleep Med Rev. 2002;6(Suppl 1):S7-10. https://doi.org/10.1016/s1087-0792(02)80002-8. (discussion S10-1, S31-3).
Morin CM, Bastien CH, Brink D, Brown TR. Adverse effects of temazepam in older adults with chronic insomnia. Hum Psychopharmacol. 2003;18(1):75–82. https://doi.org/10.1002/hup.454.
Riemann D, Voderholzer U, Cohrs S, et al. Trimipramine in primary insomnia: results of a polysomnographic double-blind controlled study. Pharmacopsychiatry. 2002;35(5):165–74. https://doi.org/10.1055/s-2002-34119.
Roehrs TA, Randall S, Harris E, et al. Twelve months of nightly zolpidem does not lead to rebound insomnia or withdrawal symptoms: a prospective placebo-controlled study. J Psychopharmacol. 2012;26(8):1088–95. https://doi.org/10.1177/0269881111424455.
Tsutsui S, Zolipidem Study Group. A double-blind comparative study of zolpidem versus zopiclone in the treatment of chronic primary insomnia. J Int Med Res. 2001;29(3):163–77. https://doi.org/10.1177/147323000102900303.
Krystal AD, Huang H, Zummo J, et al. A WASO sub-group analysis of a 6-month study of eszopiclone 3 mg. Sleep Med. 2012;13(6):691–6. https://doi.org/10.1016/j.sleep.2012.01.010.
Walsh JK, Roth T, Randazzo A, et al. Eight weeks of non-nightly use of zolpidem for primary insomnia. Sleep. 2000;23(8):1087–96.
Zhang H, Shen Y, Liu N, et al. Efficacy and safety of zaleplon in the treatment of insomnia: a randomized controlled trial. Chin J Clin Rehabil. 2004;8(18):3488–90.
Monti JM, Alvariño F, Monti D. Conventional and power spectrum analysis of the effects of zolpidem on sleep EEG in patients with chronic primary insomnia. Sleep. 2000;23(8):1075–84.
Roth T, Lines C, Vandormael K, et al. Effect of gaboxadol on patient-reported measures of sleep and waking function in patients with primary insomnia: results from two randomized, controlled, 3-month studies. J Clin Sleep Med. 2010;6(1):30–9.
Walsh JK, et al. Short-term efficacy of zaleplon in older patients with chronic insomnia. Clin Drug Investig. 2000;20(3):143–9.
Fry J, Scharf M, Mangano R, Fujimori M. Zaleplon improves sleep without producing rebound effects in outpatients with insomnia. Zaleplon Clinical Study Group. Int Clin Psychopharmacol. 2000;15(3):141–52. https://doi.org/10.1097/00004850-200015030-00003.
Elie R, Rüther E, Farr I, et al. Sleep latency is shortened during 4 weeks of treatment with zaleplon, a novel nonbenzodiazepine hypnotic. Zaleplon Clinical Study Group. J Clin Psychiatry. 1999;60(8):536–44. https://doi.org/10.4088/jcp.v60n0806.
Walsh JK, Fry J, Erwin CW, et al. Efficacy and tolerability of 14-day administration of zaleplon 5mg and 10mg for the treatment of primary insomnia. Clin Drug Investig. 1998;16(5):347–54.
Walsh JK, Erman M, Erwin CW, et al. Subjective hypnotic efficacy of trazodone and zolpidem in DSMIII–R primary insomnia. Hum Psychopharmacol Clin Exp. 1998;13(3):191–8.
Lahmeyer H, Wilcox CS, Kann J, Leppik I. Subjective efficacy of zolpidem in outpatients with chronic insomnia. Clin Drug Investig. 1997;13(3):134–44.
Monti JM, Monti D, Estévez F, Giusti M. Sleep in patients with chronic primary insomnia during long-term zolpidem administration and after its withdrawal. Int Clin Psychopharmacol. 1996;11(4):255–63. https://doi.org/10.1097/00004850-199612000-00007.
Mamelak M, Csima A, Buck L, Price V. A comparative study on the effects of brotizolam and flurazepam on sleep and performance in the elderly. J Clin Psychopharmacol. 1989;9(4):260–7.
Fleming DJ, Moldofsky H, Walsh JK. Comparison of the residual effects and efficacy of short-term zolpidem, flurazepam and placebo in patients with chronic insomnia. Clin Drug Investig. 1995;9(6):303–13.
Erman M, Guiraud A, Joish VN, Lerner D. Zolpidem extended-release 12.5 mg associated with improvements in work performance in a 6-month randomized, placebo-controlled trial. Sleep. 2008;31(10):1371–8.
Hartmann E, Lindsley JG, Spinweber C. Chronic insomnia: effects of tryptophan, flurazepam, secobarbital, and placebo. Psychopharmacology. 1983;80(2):138–42. https://doi.org/10.1007/BF00427957.
Hornyak M, Kopasz M, Rodenbeck A, et al. Influence of low‐dose doxepin on periodic leg movements in sleep in primary insomnia patients. Somnologie. 2005;9(2):111–5. https://doi.org/10.1111/j.1439-054X.2005.00050.x.
Roth T, Wright KP Jr, Walsh J. Effect of tiagabine on sleep in elderly subjects with primary insomnia: a randomized, double-blind, placebo-controlled study. Sleep. 2006;29(3):335–41. https://doi.org/10.1093/sleep/29.3.335.
He XG, Wang LN, Zhang BH, et al. Intervention effect of melatonin on elderly patients with primary insomnia. Chin J Clin Rehab. 2005;9(12):73–5.
Allain H, Coz FL, Borderies P, et al. Use of zolpidem 10 mg as a benzodiazepine substitute in 84 patients with insomnia. Hum Psychopharmacol Clin Exp. 1998;13(8):551–9.
Leppik G, Barbara, Roth-Schechter, et al. Double-blind, placebo-controlled comparison of zolpidem, triazolam, and temazepam in elderly patients with insomnia. Drug Dev Res. 1997;3(40):230–8. https://doi.org/10.1002/(SICI)1098-2299(199703)40:33.0.CO;2-L.
Dockhorn RJ, Dockhorn DW. Zolpidem in the treatment of short-term insomnia: a randomized, double-blind, placebo-controlled clinical trial. Clin Neuropharmacol. 1996;19(4):333–40. https://doi.org/10.1097/00002826-199619040-00006.
Dehlin O, Rubin B, Rundgren A. Double-blind comparison of zopiclone and flunitrazepam in elderly insomniacs with special focus on residual effects. Curr Med Res Opin. 1995;13(6):317–24. https://doi.org/10.1185/03007999509110492.
Rosenberg J, Ahlstrøm F. Randomized, double blind trial of zolpidem 10 mg versus triazolam 0.25 mg for treatment of insomnia in general practice. Scand J Prim Health Care. 1994;12(2):88–92. https://doi.org/10.3109/02813439409003681.
Scharf MB, Roth PB, Dominguez RA, Ware JC. Estazolam and flurazepam: a multicenter, placebo-controlled comparative study in outpatients with insomnia. J Clin Pharmacol. 1990;30(5):461–7. https://doi.org/10.1002/j.1552-4604.1990.tb03486.x.
Ngen CC, Hassan R. A double-blind placebo-controlled trial of zopiclone 7.5 mg and temazepam 20 mg in insomnia. Int Clin Psychopharmacol. 1990;5(3):165–71. https://doi.org/10.1097/00004850-199007000-00001.
Tamminen T, Hansen PP. Chronic administration of zopiclone and nitrazepam in the treatment of insomnia. Sleep. 1987;10(Suppl 1):63–72.
Klimm HD, Dreyfus JF, Delmotte M. Zopiclone versus nitrazepam: a double-blind comparative study of efficacy and tolerance in elderly patients with chronic insomnia. Sleep. 1987;10(Suppl 1):73–8. https://doi.org/10.1093/sleep/10.suppl_1.73.
Jovanovic UJ, Dreyfus JF. Polygraphical sleep recordings in insomniac patients under zopiclone or nitrazepam. Pharmacology. 1983;27(Suppl 2):136–45. https://doi.org/10.1159/000137920.
Zhou CL, Xie HJ, Wang LQ, Tang XF. Clinical observation of paroxetine in the treatment of chronic primary insomnia in the elderly. Chin J Gerontol. 2002;3(21):185–7.
Kärppä M, Yardley J, Pinner K, et al. Long-term efficacy and tolerability of lemborexant compared with placebo in adults with insomnia disorder: results from the phase 3 randomized clinical trial SUNRISE 2. Sleep. 2020;43(9):zsaa123. https://doi.org/10.1093/sleep/zsaa123.
Dauvilliers Y, Zammit G, Fietze I, et al. Daridorexant, a new dual orexin receptor antagonist to treat insomnia disorder. Ann Neurol. 2020;87(3):347–56. https://doi.org/10.1002/ana.25680.
Rosenberg R, Murphy P, Zammit G, et al. Comparison of lemborexant with placebo and zolpidem tartrate extended release for the treatment of older adults with insomnia disorder: a phase 3 randomized clinical trial. JAMA Netw Open. 2019;2(12): e1918254. https://doi.org/10.1001/jamanetworkopen.2019.18254.
Yan X, Huang S, Ma C, et al. A randomized, double-blind, double-dummy, multicenter, controlled trial on brotizolam intervention in outpatients with insomnia. Int J Psychiatry Clin Pract. 2013;17(4):239–43. https://doi.org/10.3109/13651501.2012.735242.
Morin CM, Koetter U, Bastien C, et al. Valerian-hops combination and diphenhydramine for treating insomnia: a randomized placebo-controlled clinical trial. Sleep. 2005;28(11):1465–71. https://doi.org/10.1093/sleep/28.11.1465.
Wade AG, Ford I, Crawford G, et al. Nightly treatment of primary insomnia with prolonged release melatonin for 6 months: a randomized placebo-controlled trial on age and endogenous melatonin as predictors of efficacy and safety. BMC Med. 2010;8:51. https://doi.org/10.1186/1741-7015-8-51.
Sivertsen B, Omvik S, Pallesen S, et al. Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: a randomized controlled trial. JAMA. 2006;295(24):2851–8. https://doi.org/10.1001/jama.295.24.2851.
Morin CM, Colecchi C, Stone J, et al. Behavioral and pharmacological therapies for late-life insomnia: a randomized controlled trial. JAMA. 1999;281(11):991–9. https://doi.org/10.1001/jama.281.11.991.
Jacobs GD, Pace-Schott EF, Stickgold R, Otto MW. Cognitive behavior therapy and pharmacotherapy for insomnia: a randomized controlled trial and direct comparison. Arch Intern Med. 2004;164(17):1888–96. https://doi.org/10.1001/archinte.164.17.1888.
Lankford DA, Corser BC, Zheng YP, et al. Effect of gaboxadol on sleep in adult and elderly patients with primary insomnia: results from two randomized, placebo-controlled, 30-night polysomnography studies. Sleep. 2008;31(10):1359–70.
Perlis ML, McCall WV, Krystal AD, Walsh JK. Long-term, non-nightly administration of zolpidem in the treatment of patients with primary insomnia. J Clin Psychiatry. 2004;65(8):1128–37. https://doi.org/10.4088/jcp.v65n0816. (PMID: 15323600).
Herrmann WM, Kubicki ST, Boden S, et al. Pilot controlled double-blind study of the hypnotic effects of zolpidem in patients with chronic “learned” insomnia: psychometric and polysomnographic evaluation. J Int Med Res. 1993;21(6):306–22. https://doi.org/10.1177/030006059302100602.
Takeda. 2007. NCT00492232. Facilitation of Zolpidem (≥10 mg) Discontinuation Through Use of Ramelteon in Subjects With Chronic Insomnia. https://clinicaltrials.gov/ct2/show/study/NCT00492232?rslt=With&type=Intr&cond=insomnia&age=12&draw=3.
Katz, 2011. NCT01489969. Sleep Laboratory Study to Investigate the Safety and Efficacy of Neu-P11 in Primary Insomnia Patients. https://clinicaltrials.gov/ct2/show/study/NCT01489969?rslt=With&type=Intr&cond=insomnia&age=12&draw=3.
NCT00548340. VEC-162 Study in Adult Patients With Primary Insomnia. https://clinicaltrials.gov/ct2/show/NCT00548340?rslt=With&type=Intr&cond=insomnia&age=12&draw=7&rank=59.
NCT01463098. A 2-Part Single Dose Study to Assess the Safety, Tolerability, Pharmacokinetics, and Pharmacodynamics of E2006. https://clinicaltrials.gov/ct2/show/results/NCT01463098?rslt=With&type=Intr&cond=insomnia&age=12&draw=11&rank=77.
Dorsey CM, Lee KA, Scharf MB. Effect of zolpidem on sleep in women with perimenopausal and postmenopausal insomnia: a 4-week, randomized, multicenter, double-blind, placebo-controlled study. Clin Ther. 2004;26(10):1578–86.
Rickels K, Morris RJ, Mauriello R, et al. Brotizolam, a triazolothienodiazepine, in insomnia. Clin Pharmacol Ther. 1986;40(3):293–9.
Scharf MB, Roth T, Vogel GW, Walsh JK. A multicenter, placebo-controlled study evaluating zolpidem in the treatment of chronic insomnia. J Clin Psychiatry. 1994;55(5):192–9.
Soares CN, Joffe H, Rubens R, et al. Eszopiclone in patients with insomnia during perimenopause and early postmenopause: a randomized controlled trial. Obstet Gynecol. 2006;108(6):1402–10.
Voshaar RC, van Balkom AJ, Zitman FG. Zolpidem is not superior to temazepam with respect to rebound insomnia: a controlled study. Eur Neuropsychopharmacol. 2004;14(4):301–6.
Roth T, Zammit GK, Scharf MB, Farber R. Efficacy and safety of as-needed, post bedtime dosing with indiplon in insomnia patients with chronic difficulty maintaining sleep. Sleep. 2007;30(12):1731–8. https://doi.org/10.1093/sleep/30.12.1731.
Cordingley GJ, Dean BC, Harris RI. A double-blind comparison of two benzodiazepine hypnotics, flunitrazepam and triazolam, in general practice. Curr Med Res Opin. 1984;8(10):714–9. https://doi.org/10.1185/03007998409110122.
Dahl LE, Dencker SJ, Lundin L, Kullingsjö H. Comparison of nitrazepam with triazolam in insomniac outpatients. Acta Psychiatr Scand. 1982;65(2):86–92. https://doi.org/10.1111/j.1600-0447.1982.tb00826.x.
Fabre LF Jr, Gross L, Pasigajen V, Metzler C. Multiclinic double-blind comparison of triazolam and flurazepam for seven nights in outpatients with insomnia. J Clin Pharmacol. 1977;17(7):402–9. https://doi.org/10.1002/j.1552-4604.1977.tb04623.x. (PMID: 18492).
Fillingim JM. Double-blind evaluation of the efficacy and safety of temazepam in outpatients with insomnia. Br J Clin Pharmacol. 1979;8(1):73S-77S. https://doi.org/10.1111/j.1365-2125.1979.tb00461.x.
Martinez HT, Serna CT. Short-term treatment with quazepam of insomnia in geriatric patients. Clin Ther. 1982;5(2):174–8.
McAlpine CJ, Ankier SI, Elliott CS. A multicentre hospital study to compare the hypnotic efficacy of loprazolam and nitrazepam. J Int Med Res. 1984;12(4):229–37. https://doi.org/10.1177/030006058401200402.
Ware JC, Walsh JK, Scharf MB, et al. Minimal rebound insomnia after treatment with 10-mg zolpidem. Clin Neuropharmacol. 1997;20(2):116–25. https://doi.org/10.1097/00002826-199704000-00002.
Allen RP, Mendels J, Nevins DB, et al. Efficacy without tolerance or rebound insomnia for midazolam and temazepam after use for one to three months. J Clin Pharmacol. 1987;27(10):768–75. https://doi.org/10.1002/j.1552-4604.1987.tb02994.x.
Anderson AA. Zopiclone and nitrazepam: a multicenter placebo controlled comparative study of efficacy and tolerance in insomniac patients in general practice. Sleep. 1987;10(Suppl 1):54–62. https://doi.org/10.1093/sleep/10.suppl_1.54.
Bayer AJ, Pathy MS. Clinical and psychometric evaluation of two doses of loprazolam and placebo in geriatric patients. Curr Med Res Opin. 1986;10(1):17–24. https://doi.org/10.1185/03007998609111088.
Cohn JB, Wilcox CS, Bremner J, Ettinger M. Hypnotic efficacy of estazolam compared with flurazepam in outpatients with insomnia. J Clin Pharmacol. 1991;31(8):747–50. https://doi.org/10.1002/j.1552-4604.1991.tb03771.x.
Dominguez RA, Goldstein BJ, Jacobson AF, Steinbook RM. Hypnotic efficacy of a modified triazolodiazepine, brotizolam. Clin Pharmacol Ther. 1985;37(6):674–9. https://doi.org/10.1038/clpt.1985.110.
Goldenberg F, Hindmarch I, Joyce CRB, Le Gal M, Partinen M, Pilate C. Zopiclone, sleep and health-related quality of life. Human Psychopharacol Clin Exp. 1994;9:245–51.
Gooneratne NS, Edwards AY, Zhou C, et al. Melatonin pharmacokinetics following two different oral surge-sustained release doses in older adults. J Pineal Res. 2012;52(4):437–45. https://doi.org/10.1111/j.1600-079X.2011.00958.x.
Kales A, Bixler EO, Soldatos CR, et al. Quazepam and flurazepam: long-term use and extended withdrawal. Clin Pharmacol Ther. 1982;32(6):781–8. https://doi.org/10.1038/clpt.1982.236.
Kales A, Bixler EO, Soldatos CR, et al. Quazepam and temazepam: effects of short- and intermediate-term use and withdrawal. Clin Pharmacol Ther. 1986;39(3):345–52. https://doi.org/10.1038/clpt.1986.51.
Kales A, Bixler EO, Vela-Bueno A, et al. Comparison of short and long half-life benzodiazepine hypnotics: triazolam and quazepam. Clin Pharmacol Ther. 1986;40(4):378–86. https://doi.org/10.1038/clpt.1986.194.
Kales A, Manfredi RL, Vgontzas AN, et al. Rebound insomnia after only brief and intermittent use of rapidly eliminated benzodiazepines. Clin Pharmacol Ther. 1991;49(4):468–76. https://doi.org/10.1038/clpt.1991.55.
Leibowitz M, Sunshine A. Long-term hypnotic efficacy and safety of triazolam and flurazepam. J Clin Pharmacol. 1978;18(5–6):302–9. https://doi.org/10.1002/j.1552-4604.1978.tb02450.x.
Monti JM, Attali P, Monti D, Zipfel A, de la Giclais B, Morselli PL. Zolpidem and rebound insomnia—a double-blind, controlled polysomnographic study in chronic insomniac patients. Pharmacopsychiatry. 1994;27(4):166–75. https://doi.org/10.1055/s-2007-1014298.
Richardson G, Wang-Weigand S. Effects of long-term exposure to ramelteon, a melatonin receptor agonist, on endocrine function in adults with chronic insomnia. Hum Psychopharmacol. 2009;24(2):103–11. https://doi.org/10.1002/hup.993.
Shell WE, May LA, Bullias DH, et al. Sentra PM (a medical food) and trazodone in the management of sleep disorders. J Cent Nerv Syst Dis. 2012;4:65–72. https://doi.org/10.4137/JCNSD.S9381.
Wang-Weigand S, Watissée M, Roth T. Use of a post-sleep questionnaire-interactive voice response system (PSQ-IVRS) to evaluate the subjective sleep effects of ramelteon in adults with chronic insomnia. Sleep Med. 2011;12(9):920–3. https://doi.org/10.1016/j.sleep.2011.06.008.
Heidrich H, Ott H, Beach RC. Lormetazepam—a benzodiazepine derivative without hangover effect? A double-blind study with chronic insomniacs in a general practice setting. Int J Clin Pharmacol Ther Toxicol. 1981;191:11–7.
Begg EJ, Robson RA, Frampton CM, Campbell JE. A comparison of efficacy and tolerance of the short acting sedatives midazolam and zopiclone. N Z Med J. 1992;105(944):428–9.
Dement WC. Objective measurements of daytime sleepiness and performance comparing quazepam with flurazepam in two adult populations using the Multiple Sleep Latency Test. J Clin Psychiatry. 1991;52(Supplement):31–7.
Mauri MC, Gianetti S, Pugnetti L, Altamura AC. Quazepam versus triazolam in patients with sleep disorders: a double-blind study. Int J Clin Pharmacol Res. 1993;133:173–7.
Moon CA, Ankier SI, Hayes G. Early morning insomnia and daytime anxiety—a multicentre general practice study comparing loprazolam and triazolam. Br J Clin Pract. 1985;399:352–8.
Roger M, Attali P, Coquelin JP. Multicenter, double-blind, controlled comparison of zolpidem and triazolam in elderly patients with insomnia. Clin Ther. 1993;151:127–36.
Caldwell JR. Short-term quazepam treatment of insomnia in geriatric patients. Pharmacotherapeutica. 1982;34:278–82.
NCT00156533. Long term treatment with zolpidem: nightly and intermittent dosing. clinicaltrials.gov/ct2/show/NCT00156533.
NCT00177216. Characteristics of sleep patterns in young adults with and without insomnia. clinicaltrials.gov/ct2/show/NCT00177216.
NCT00383643. Xyrem sodium oxybate and ambien zolpidem tartrate in the treatment of chronic insomnia. clinicaltrials.gov/ct2/show/NCT00383643.
NCT00755495. Safety and efficacy of ramelteon and doxepin in subjects with chronic insomnia. clinicaltrials.gov/ct2/show/NCT00755495.
NCT00756002. Safety and efficacy study of ramelteon in subjects with chronic insomnia. clinicaltrials.gov/ct2/show/NCT00756002.
NCT03375203. A study to evaluate the efficacy, safety, and tolerability of JNJ-42847922 in participants with insomnia disorder. https://clinicaltrials.gov/ct2/show/NCT03375203.
NCT03545191. Study to assess the efficacy and safety of ACT-541468 in adult and elderly subjects with insomnia disorder. https://clinicaltrials.gov/ct2/show/NCT03545191.
NCT03575104. Study to assess the efficacy and safety of ACT-541468 in adult and elderly subjects suffering from difficulties to sleep. https://clinicaltrials.gov/ct2/show/NCT03575104.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This research received no specific grant from any funding agency.
Conflict of interest
BP, LG, JHT, GWD, XXL, YQZ, DRW, KHY, LYH, HHL, KLY, CT, YL, QW, HFZ, YG, ML, and JYL declare no competing interests.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
BP, LG, JHT, GWD, XXL, YQZ, DRW, and KHY conceived and designed the study. BP, LYH, HHL, KLY, CT, YL, QW, HFZ, YG, and ML screened and selected the articles. BP, LYH, HHL, KLY, JYL, QW, HFZ, YG, and ML extracted the data. BP, LYH, CT, YL, and QW assessed the risk of bias. BP, HHL, CT, and LYH analyzed the data. LG and KHY supervised the data analyses. BP, YL, QW, and LYH rated the certainty of evidence. BP, LG, JHT, GWD, and KHY interpreted the data. BP, LG, XXL, YQZ, and KHY drafted the manuscript. All authors had full access to all the data in the study, had read and approved the final version of the manuscript, and agree to be accountable for the work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pan, B., Ge, L., Lai, H. et al. The Comparative Effectiveness and Safety of Insomnia Drugs: A Systematic Review and Network Meta-Analysis of 153 Randomized Trials. Drugs 83, 587–619 (2023). https://doi.org/10.1007/s40265-023-01859-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-023-01859-8



