Abstract
Agents in development for the prevention or treatment of Clostridioides difficile infection can be split into three broad categories: antibiotics, microbiome restoration, and vaccines. Given the extensive list of agents currently in development, this narrative review will focus on agents that have progressed into late-stage clinical trials, defined as having a Phase III clinical trial registered on ClinicalTrials.gov. These agents include one antibiotic (ridinilazole), three live biotherapeutic products (LBPs) (CP101, RBX2660, and SER109), and two toxoid vaccines (PF06425090 and a second toxoid vaccine). As new prevention and treatment strategies enter the market, clinicians and administrators will need knowledge of these products to make rational decisions on how best to adopt them into clinical practice.
Similar content being viewed by others
Prevention and management of Clostridioides difficile infection (CDI) includes minimal disruption or restoration of the healthy gut microbiome. |
Emerging treatment options for CDI include narrow-spectrum antibiotics that minimize microbiome disruption, second-generation microbiome restoration, and vaccines for primary CDI prevention. |
1 Introduction
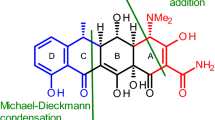
Clostridioides difficile is an anaerobic, Gram-positive, toxin-producing, spore-forming bacteria, and the causative organism of C. difficile infection (CDI). The pathogenesis of CDI is mediated by two toxins: C. difficile toxins A and B [1]. Toxin A is an enterotoxin that affects gut epithelial integrity and stimulates inflammation in the bowel. Toxin B exerts direct cytotoxic effects on colonic tissues. The inflammatory response that ensues causes the signs and symptoms associated with CDI: diarrhea, abdominal pain, leukocytosis, and pseudomembranous colitis [2, 3]. Since CDI is caused by a bacteria the standard of care for CDI treatment includes antibiotic therapy. The necessity of antibiotics in treating CDI was demonstrated by the failure of tolevamer, a nonantibiotic, toxin-binding polymer, as stand-alone therapy [4]. Accordingly, all CDI treatment regimens continue to rely on an antibiotic backbone.
One limitation of antibiotics is their inability to kill spores. C. difficile spores are ubiquitous in the environment and their ingestion and subsequent germination into vegetative, toxin-producing cells causes CDI in at-risk hosts [5]. While several antibiotics, including fidaxomicin, CRS3123, and ramoplanin, have demonstrated the ability to inhibit C. difficile sporulation and/or adhere to the exosporium layer of spores, killing vegetative cells as they germinate, no antibiotic has demonstrated the ability to kill intact spores [6,7,8,9,10]. The persistence of C. difficile spores following antibiotic therapy contributes to CDI recurrence, which occurs in approximately 15–25% of patients and represents a major burden in care [11,12,13,14]. A strategy to prevent CDI recurrence has been a focus of new treatment strategies.
C. difficile infection prevention requires a healthy gut microbiome. An intact, diverse gut microbiome provides humans with colonization resistance against pathogenic organisms, including C. difficile [15]. Disruption of the microbiota, usually through receipt of antibiotics, allows C. difficile spores to colonize the gut and germination to toxin-producing vegetative cells to occur. Thus, an ideal antibiotic for the treatment of CDI will selectively kill C. difficile while sparing other species present in the gut, including other Clostridium species. Intestinal bile acids are also thought to play a key role in this complex pathophysiology. Briefly, primary bile acids promote C. difficile spore germination while secondary bile acids inhibit vegetative C. difficile growth [16]. Certain bacterial species that populate the healthy gut microbiome are responsible for transforming primary bile acids into beneficial secondary bile acids. Thus, dysbiosis often leads to a reduction in secondary bile acids and an abundance of primary bile acids. This growing appreciation for the role of the microbiome has led to an ongoing search for ultra-narrow-spectrum agents for treating CDI, paired with strategies to expedite microbiome restoration following CDI.
Patients remain at risk for CDI for as long as microbiome dysbiosis persists, and restoration can take up to a year following antibiotic cessation [17]. Additionally, all existing C. difficile-active antibiotics cause further dysbiosis, albeit to varying degrees [18,19,20]. To help restore microbiome diversity, a variety of microbial-containing products have been utilized, including probiotics and fecal microbiota transplantation (FMT). Recently, a new category of live biotherapeutic products (LBPs) or “second-generation FMT” products has been created for the prevention of CDI recurrence, which undergo significant screening and processing to improve their standardization and safety [21, 22]. Notably, as with traditional FMT, antibiotic therapy is still necessary prior to therapy with an LBP, and as such, these products are considered adjunctive therapy in the treatment of CDI.
The CDI developmental pipeline can thus be split into three broad categories: antibiotics, microbiome therapeutics, and vaccines. Given the extensive list of agents in development across these categories, this narrative review aims to discuss agents that have progressed into late-stage clinical trials, which we define as having a Phase III clinical trial registered on ClinicalTrials.gov.
2 Antibiotics
Clinical practice guidelines have historically recommended oral vancomycin and/or metronidazole for most patients [23,24,25,26]. However, following the Food and Drug Administration (FDA) approval of fidaxomicin in 2011, many clinical practice guidelines have considered fidaxomicin equivalent, if not preferred, to oral vancomycin in most scenarios [27,28,29,30,31]. Although these three antibiotics serve as the mainstays of CDI therapy, other antibiotics have also been used off-label to treat CDI, including bacitracin, nitazoxanide, rifaximin, and tigecycline [32]. Of these, only rifaximin and tigecycline have been included in guideline recommendations [27,28,29, 31]. Two antibiotics not available in the USA, fusidic acid and teicoplanin, have been studied for use in CDI as well [32]. Lastly, several antibiotics in development specifically for CDI have notably failed to make it to market, including cadazolid, LFF571, ramoplanin, and surotomycin [33].
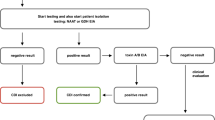
Fortunately, the developmental pipeline of antibiotics for CDI continues to develop. Currently, there are six antibiotics undergoing clinical trials in humans with CDI: ridinilazole (ongoing Phase III), MGBBP3 (completed Phase II), CRS3123 (ongoing Phase II), DNV3837/DNV3681 (ongoing Phase II), and ibezapolstat (ongoing Phase II). As it is the only antibiotic to progress to Phase III clinical trials, ridinilazole will be discussed in depth below.
2.1 Ridinilazole
Ridinilazole (Summit Therapeutics, Inc.) is a narrow-spectrum antibiotic that is being developed specifically for CDI. It has undergone two Phase II trials (ClinicalTrials.gov identifiers: NCT02092935 and NCT02784002), one of which has been published [34]. Ridinilazole has also been compared to vancomycin in two identical Phase III trials of adults with CDI: Ri-CoDIFy 1 (NCT03595553) and Ri-CoDIFy 2 (NCT03595566) [35, 36].
In its Phase II trial, patients aged 18–90 years with CDI were randomized to receive oral ridinilazole 200 mg twice daily or oral vancomycin 125 mg four times daily for 10 days [34]. Of the 69 patients in the modified intention to treat (mITT) population, which included only patients with free C. difficile toxin in their stool as identified via an enzyme immunoassay (EIA) or a cell culture cytotoxicity neutralization assay, 50.7% were aged < 65 years, 76.8% had non-severe CDI, and 87.0% had no history of CDI in the past year. The primary efficacy endpoint was sustained clinical response (SCR), defined as clinical cure without CDI recurrence within 30 days after the end of antibiotic therapy. In the mITT population, SCR occurred in 66.7% (24/36) of patients who received ridinilazole and 42.4% (14/33) of patients who received vancomycin (treatment difference 21.1%; 90% confidence interval [CI], 3.1–39.1; p = 0.0004). Thus, the investigators deemed ridinilazole superior to vancomycin.
Since stool samples were collected from patients enrolled in the Phase II trial at several time-points, a secondary analysis was performed on patients who provided at least three stool samples and did not receive standard-of-care CDI treatment (i.e., fidaxomicin, metronidazole, or vancomycin) prior to enrollment [37]. Mean alpha diversity measurements, which are used to estimate microbiota richness within a sample, were significantly lower in vancomycin- versus ridinilazole-treated patients (n = 22 in each arm). Furthermore, beta diversity measurements, used to estimate the similarity between samples, suggested that while gut microbiota diversity at the beginning and end of vancomycin therapy was significantly different, the same was not true for ridinilazole. This change in gut microbiota diversity in vancomycin-treated patients corresponded with a significant increase in primary bile acids and a decrease in secondary bile acids over the 10 days of treatment [38]. It is hypothesized that this difference in the propensity for ridinilazole and vancomycin to cause further gut dysbiosis is the reason for the observed difference in the rate of SCR in the Phase II trial [37].
Ridinilazole has also been compared to vancomycin in two identical Phase III trials of adults (Ri-CoDIFy 1 and Ri-CoDIFy 2) [35, 36]. A total of 759 patients aged ≥ 18 years with CDI between both trials were randomized to receive either oral ridinilazole 200 mg twice daily or oral vancomycin 125 mg four times daily for 10 days [39]. Like the Phase II trial, the primary efficacy endpoint was SCR and only patients with free C. difficile toxin in their stool were included. Notably, among the mITT population (n = 745), 56.6% were aged < 65 years, 69.9% had non-severe CDI, and 82.8% had no history of CDI in the past year [40]. While the rate of CDI recurrence was lower in those who received ridinilazole (8.1%) versus vancomycin (17.3%; p = 0.0002), the study did not meet its primary endpoint for superiority of SCR. Results from the microbiome and bile acid analyses largely mirrored what was observed in the Phase II trial [37, 38, 40]. Briefly, mean alpha diversity measurements and the relative abundance of secondary bile acids were significantly lower in vancomycin- versus ridinilazole-treated patients at the end of antibiotic therapy [40]. Treatment-emergent adverse effects primarily consisted of gastrointestinal adverse effects such as diarrhea, nausea, and abdominal pain, and adverse effects leading to the discontinuation of study treatment was uncommon in both treatment arms (0.8% vs 2.9% in those who received ridinilazole and vancomycin, respectively). While these results are encouraging, an additional clinical trial will likely be necessary before the FDA considers ridinilazole for approval [41].
Recruitment is ongoing for a trial in which ridinilazole is being compared to vancomycin in adolescents aged 12–17 years with CDI (Ri-CoDIFy 3 [NCT04802837]) [42]. Notably, this is only the second randomized controlled trial conducted in adolescents with CDI to date [43]. As the topline results from Ri-CoDIFy 1 and Ri-CoDIFy 2 suggest that additional trials are needed, it is unlikely that a new antibiotic for CDI will be available in the next two years.
3 Live Biotherapeutic Products (LBPs)
A growing appreciation for the role of the microbiome in the development of and recovery from CDI has led to increased interest in microbiome-based therapies. Live biotherapeutic products (LBPs) are defined by the FDA as non-vaccine biological products that contain live organisms and are applicable to the prevention, treatment, or cure of a disease or condition in human beings [21]. Live biotherapeutic products seeking FDA-approval for the prevention of CDI recurrence include a variety of human donor-derived products. As the intent of LBPs is to restore dysbiosis and prevent future CDI episodes, which historically occur in up to 15–25% of patients, these products are to be administered following antibiotic therapy as they do not have antimicrobial activity against C. difficile.
Live biotherapeutic products are unique from previous microbiome-based strategies, such as probiotics and FMT. Probiotics, a term broadly used to describe any live microorganism(s) that confers a health benefit when administered in adequate amounts, usually refers to foods or dietary supplements available over the counter and, as such, are not strictly regulated by the FDA [22, 44, 45]. This has created a landscape in which there are many products available, often with discrepancies between labeled and actual contents, including a critical lack of viable microorganisms [46]. Accordingly, many of the studies analyzing the use of probiotics as primary or secondary prevention of CDI are of low-quality and have failed to demonstrate a consistent benefit [47,48,49]. Clinical practice guidelines therefore do not recommend the use of probiotics in the management of CDI [30, 31, 50].
Fecal microbiota transplantation refers to the administration of healthy donor stool to a diseased host’s intestinal tract via enema, colonoscopy, sigmoidoscopy, or nasogastric tube, and faces similar limitations due to its unstandardized nature [51, 52]. Sources of donor stool have ranged from a family member or friend with some degree of survey-based health screening to stool banks that conduct rigorous laboratory screening and provide accompanying stool characterization. Although the stool may be diluted with a liquid, like saline, there is minimal to no manipulation or processing prior to administration. The FDA regulation of FMT has varied since its development for modern use in the early 2000s, although at present, it is considered a biological product recommended to be administered under an investigational new drug application [53, 54]. There is robust evidence demonstrating the benefit of FMT in treating multiply recurrent or refractory CDI, and it is recommended in such cases in all major clinical practice guidelines [30, 31, 50, 55]. However, safety concerns have arisen over the past five years due to the transmission of multi-drug–resistant bacteria and potentially other pathogenic organisms, underscoring the need for standardization and comprehensive product screening [56, 57]. In contrast to LBPs, FMT still generally refers to the procedure rather than a specific product and is considered a treatment during acute infection rather than solely for the prevention of recurrence.
Live biotherapeutic products are, by definition, FDA-regulated as drugs and therefore their contents must be highly standardized and produced using good manufacturing practices [21]. Additionally, rigorous clinical trials meeting FDA standards and demonstrating both safety and efficacy will be required prior to approval. There are three LBPs that are in the process of recruiting for or have completed Phase III trials; each will be briefly discussed here. Of note, much of the information regarding these three agents remains proprietary and unavailable for inclusion in this review. Details of each product are also available in Table 1.
3.1 CP101
CP101 (Finch Therapeutics) is an oral capsule comprising lyophilized healthy donor stool [58, 59]. Following collection and screening from individual donors, the stool is processed, and the resulting material is lyophilized by mixing it with a 5% trehalose solution cryoprotectant prior to encapsulation [59]. The dosing regimen uniquely only requires a one-time dose of one capsule, without any need for bowel preparation. CP101 has completed and presented results from two Phase II trials: PRISM3 (NCT03110133) [60,61,62] and PRISM-EXT (NCT03497806) [63, 64], which is an extension trial including those patients experiencing recurrence in PRISM3. Enrollment for a Phase III trial, PRISM4 (NCT05153499)[65], began in late 2021, but was halted by the FDA in Spring 2022 due to updated Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV)-2-related donor screening and manufacturing requirements, enrollment restarted in late 2022 [66, 67].
Early studies of CP101 focused on refining its formulation and establishing a dose in patients with 4–5 CDI recurrences [58, 59]. CP101 prevented 8-week CDI recurrence in 87.8% (43/49) of patients in a proof-of-concept study with a dosing protocol that evolved from using ~ 2.5 × 1012 bacteria contained in 24–27 capsules to ~ 2.1 to 2.5 × 1011 bacteria in 2–3 capsules [68]. Phase II trials proceeded with dosing of one capsule with ~ 6 × 1011 bacterial cells [62]. PRISM3 enrolled 198 patients aged ≥ 65 years with their first CDI recurrence or of any age with ≥ 2 recurrences [60]. Patients receiving CP101 had a higher rate of sustained clinical cure at 8 weeks, defined as absence of recurrence, versus placebo (74.5% [76/102] vs 61.5% [59/96]; p = 0.049), therefore meeting the trial’s primary efficacy endpoint. An increased alpha diversity in CP101 recipients compared to placebo was observed within 1 week of administration (p < 0.001) and this difference persisted through 8 weeks (p < 0.0001). The PRISM-EXT open-label extension trial observed a similar 8-week success rate of 80.3% (106/132) amongst its participants that were either directly enrolled (n = 82) or experienced CDI recurrence in either arm from PRISM3 (n = 50) [63]. Among those patients receiving a second dose of CP101 following recurrence in PRISM3, 70% (14/20) experienced 8-week treatment success and no safety concerns were noted [64]. Efficacy and safety have been reported from PRISM3 for up to 24 weeks of follow-up, with 73.5% and 59.4% (p = 0.0347) of CP101 and placebo participants, respectively, experiencing sustained clinical cure through week 24 [61].
3.2 RBX2660 (Rebyota)
RBX2660 (Rebyota) (Ferring Pharmaceuticals/Rebiotix, Inc.) is a microbiota suspension created from healthy donor stool to be administered as an enema [69,70,71]. Following a survey-based health screening and repeated infectious diseases blood and stool screenings, samples from individual donors are collected, pooled, and suspended in polyethylene glycol 3350 to create a single dose of RBX2660 containing ≥ 107 of live organisms/mL and 50 g of human stool/150 mL 0.9% saline. Each product undergoes a minimum 14-day quarantine in which repeated testing occurs prior to releasing each individual product. No bowel preparation is required prior to enema installation, but a washout period of 24–72 h is needed following the final CDI antibiotic dose. RBX2660 has completed a Phase III trial (PUNCH CD3; NCT03244644) [72] and the FDA approved RBX2660 for the prevention of CDI recurrence in individuals aged ≥ 18 years following antibiotic treatment for recurrent CDI on November 30, 2022 [73]. An additional, open-label Phase III trial (PUNCH CD3-OLS; NCT03931941) targeting inclusion of a more diverse and real-world patient population is also currently enrolling patients [74, 75].
RBX2660 has completed three Phase II trials: PUNCH CD (NCT01925417) [69], PUNCH Open Label (NCT02589847) [71], and PUNCH CD2 (NCT02299570) [76]. PUNCH CD was an open-label, non-comparative trial, demonstrating the safety and efficacy of RBX2660 in preventing CDI recurrence in 87.1% (27/31) of patients receiving two doses of RBX2660 in the 8 weeks following administration [69]. This was followed by the PUNCH Open Label trial. which compared patients receiving up to two doses of RBX2660 with a historical control group receiving antibiotics alone [71]. The primary efficacy endpoint of 8-week treatment success was met in 78.9% (112/142) of the RBX2660 cohort versus 30.7% (23/75) of the historical control group (p < 0.0001). RBX2660 responders were followed for an additional 24 months, at which time 90.7% (88/97) had not experienced another CDI episode. A final double-blinded, placebo-controlled, dose-ranging Phase II trial, PUNCH CD2, enrolled 89 patients who were randomized to receive two doses of RBX2660 given 7 days apart, one dose of RBX2660 followed by placebo 7 days later, or two doses of placebo given 7 days apart [76]. Although the primary efficacy endpoint of 8-week treatment success in participants receiving two doses of RBX2660 (60.9% [25/41]) versus two doses of placebo (45.5% [20/44]) was not met (p > 0.05), one dose of RBX2660 (66.7% [28/42]) demonstrated superiority over placebo (45.5% [20/44]; p = 0.048). Although the reason for the failure of two doses versus placebo is unknown, the investigators noted 13 participants were declared failures prior to receiving the second dose of either RBX2660 (n = 5) or placebo (n = 8), which was permitted to be administered sooner than 7 days after the first dose if patients experienced continued symptoms [76]. This may have prematurely assigned some patients as failures who would have responded to a second dose, thereby decreasing power to detect a difference between two doses and placebo.
Given these results, the Phase III trial was designed using a single dose of RBX2660 [72]. PUNCH CD3 is a randomized, double-blinded, placebo-controlled trial in which 262 patients with at least one CDI recurrence were randomized to receive RBX2660 or placebo. Treatment success at 8-weeks post-dose was observed in 71.2% (126/177) of RBX2660 recipients and 62.4% (53/85) of placebo recipients in the mITT population. However, due to recruiting difficulties associated with the COVID-19 pandemic, the FDA allowed the use of a Bayesian analysis to assess the primary endpoint of 8-week treatment success that incorporated patients receiving one dose of RBX2660 from the PUNCH CD2 trial and patients from the PUNCH CD3 trial. This a priori analysis demonstrated a model-estimated treatment success rate of 70.6% with RBX2660 versus 57.5% with placebo (estimated treatment effect, 13.1%) and a posterior probability of superiority of 99.1%, exceeding the 97.5% threshold that was chosen [72]. Rates of adverse events were similar between RBX2660 and placebo through 6-month follow-up, and there were no severe adverse events deemed related to RBX2660 or its rectal administration. Interim results from the PUNCH CD3-OLS Phase III trial, which includes patients with irritable bowel disease and irritable bowel syndrome, showed safety and efficacy in a real-world population with 75% (45/60) of patients experiencing 8-week treatment success [74]. Of the 27 patients without recurrence who reached the 6-month follow-up period, 74.1% (n = 20) remained CDI-free. Treatment success rates across all five Phase II and III trials, including a total of 629 patients receiving RBX2660, have ranged from 50 to 79% [75].
Multiple secondary analyses from Phase II and III trials have also been published showcasing a range of additional benefits associated with RBX2660. Several analyses have demonstrated beneficial microbiome changes in patients responding to RBX2660 that were absent in those patients who responded to placebo [77,78,79,80,81]. RBX2660-responders displayed post-treatment microbiome profiles more similar to that of RBX2660, with a predominance of Bacteroidia and Clostridia classes, while the microbiome profiles of placebo-responders did not differ from their pre-treatment profile [78]. Alpha diversity increased in both the RBX2660 and placebo groups without CDI recurrence [79]. Additionally, healthier bile acid compositions were observed in patients who received RBX2660 in PUNCH CD3 [81, 82]. Specifically, a decrease in primary bile acids, responsible for spore germination, and increases in secondary bile acids, which inhibit vegetative C. difficile growth, were observed after treatment. These findings suggest a recovery of the gut microbiome and subsequent restoration of bile acid homeostasis, which provides a mechanistic explanation for the higher treatment success rates observed in RBX2660-treated patients. In the PUNCH CD, CD2, and CD3 trials, RBX2660 was also associated with decreased antimicrobial resistance (AMR) gene content for at least 6 months following administration [77, 79, 83]. Vancomycin-resistant Enterococcus (VRE) stool colonization was specifically assessed in the PUNCH CD study, where 72.7% (8/11) of patients who tested positive for VRE prior to RBX2660 receipt converted to negative following therapy [84]. These additional investigations highlight the broader benefit of CDI management that includes a microbiome restoration strategy.
3.3 SER109
SER109 (Seres Therapeutics, Inc.) is an oral capsule composed of live, purified Firmicutes bacterial spores derived from healthy donor stool, which were chosen based on their ability to metabolically compete with C. difficile for essential nutrients and/or modulate bile-acid profiles to reestablish colonization resistance [85,86,87]. SER109 is given as a regimen of four capsules once daily for 3 days, totaling ~ 3 × 107 spore colony-forming units. This is the only product discussed in this review that requires the administration of a bowel regimen consisting of 10 mg magnesium citrate given the night prior to the first dose to minimize presence of any residual CDI-active antibiotics [87]. The manufacturing process includes an ethanol-based, spore purification step intended to reduce the risk of transmission of other pathogens [85]. SER109 has completed Phase II (ECOSPOR; NCT02437487) [86] and Phase III (ECOSPOR III; NCT03183128)[87] trials, and has preliminary results from its open-label (ECOSPOR IV; NCT03183141) trial of those experiencing recurrence following SER109 receipt in ECOSPOR III [88, 89]. The manufacturer filed a BLA with the FDA in September 2022, which was assigned a priority review designation with a Prescription Drug User Fee Act (PDUFA) action date set as April 26, 2023 [90, 91].
In its dose-finding Phase Ib trial, up to 15 SER109 capsules per day were administered to patients with ≥ 3 episodes of CDI in the prior 12 months [85]. The primary endpoint, prevention of recurrence during the 8-week follow-up, was achieved in 86.7% (26/30) of patients. Additionally, 16S rRNA sequencing analysis demonstrated a sustained increase in microbiome diversity, including expansion of the Firmicutes and amplification of other beneficial phyla not contained in SER109, such as the Bacteroidetes, through 24 weeks post-administration. In ECOSPOR, 89 patients were enrolled and randomized in a 2:1 ratio to receive four capsules (~ 1 × 108 spores) of SER109 given one time or placebo [86]. SER109 failed to establish superiority over placebo as 44.1% (26/59) versus 53.3% (16/30) of patients receiving SER109 and placebo, respectively, experienced 8-week CDI recurrence (risk ratio (RR), 1.22; 95% CI, 0.79–1.88) [86]. A benefit was still observed in a preplanned subgroup analysis of those aged ≥ 65 years, in which 45.2% of patients receiving SER109 experienced recurrence versus 80% of those receiving placebo (RR, 1.8; 95% CI 1.1–2.8). Earlier engraftment, defined as the presence of SER109 species, was also associated with the prevention of recurrence (p < 0.05) and increased secondary bile acid concentrations (p < 0.0001). The failure to establish superiority in the overall cohort was attributed to the use of polymerase chain reaction (PCR) testing, leading to over enrollment of C. difficile-colonized patients, and underdosing of SER109.
To remedy these issues, ECOSPOR III used an increased dose of four SER109 capsules given once daily for 3 days and required a positive toxin assay for study entry [87]. Although enrollment of 188 patients was planned, the trial ended early with a sample size of 182 patients due to the coronavirus disease 2019 (COVID-19) pandemic. Of those, 88.6% (78/89) in the SER109 and 60.2% (56/93) in the placebo group experienced 8-week sustained clinical cure (p < 0.001); SER109 was superior to placebo in preventing CDI recurrence and was associated with a 0.32 relative risk (95% CI 0.18–0.58) of recurrent CDI. Although the numbers of Firmicute species increased in both SER109 and placebo recipients who did not experience recurrence, the number of SER109 species was higher among those receiving SER109 through Week 8. Additionally, although similar at baseline, there were higher concentrations of secondary bile acids in SER109 versus placebo recipients at all time points through Week 8. The overall rate of 8-week sustained clinical cure was 91.3% (240/263) in the open-label ECOSPOR IV extension trial, with similar SER109 response rates in those with one prior CDI recurrence (93.5%; 72/77) or two or more prior recurrences (90.3%, 168/186) [89]. No safety concerns were noted through 24 weeks post-dose in any clinical trials of SER109 [85,86,87, 89].
4 Approaches to CDI Prevention
As with any disease, prevention is the best medicine. Given the pathogenesis of CDI, two logical methods to prevent CDI would be to prevent or limit the infiltration of C. difficile toxins into the gut epithelium and the ensuing inflammatory response and/or to prevent the destruction of the healthy gut microbiome. The former is addressed through use of bezlotoxumab, a monoclonal antibody targeting C. difficile toxin B that was approved by the FDA in 2016 for the prevention of CDI recurrence in at-risk patients. Bezlotoxumab is administered as a one-time infusion, and as a form of passive immunity, it remains in the colon for several months (half-life of 19 days) and neutralizes toxin B during the highest-risk period of recurrence [92]. However, once bezlotoxumab is excreted, the patient is no longer protected. Thus, vaccination, a form of active immunity, is an attractive preventative option. Two vaccines have completed Phase III trials and are discussed in more depth below. Two additional vaccine candidates, VLA84 (Valneva Austria GmbH; NCT02316470) [93] and GSK2904545A (GlaxoSmithKline; NCT04026009) [94], are in early-stage clinical trials, but they will not be discussed in depth.
The second approach, preventing dysbiosis, requires more nuance as dysbiosis is often an unwanted consequence of antibiotic use. Therefore, we must preserve the intended effects of the antibiotic while preventing collateral damage. Unique strategies in development to prevent dysbiosis include ribaxamase (Synthetic Biologics, Inc.; NCT02563106), which is a β-lactamase used to inactivate β-lactams in the gut, and DAV132 (Da Volterra; NCT03710694), which is an activated charcoal product that prevents dysbiosis by binding to antibiotics, included non-β-lactams, in the colon [95, 96]. However, neither is currently being studied in Phase III clinical trials for CDI prevention and a full discussion of these agents is beyond the scope of this review.
4.1 PF06425090
PF06425090 (Pfizer Inc.) is a bivalent toxoid vaccine that contains detoxified versions of both toxin A and toxin B of C. difficile. It has undergone both Phase II (NCT02561195) and Phase III (NCT03090191) clinical trials [97, 98].
In its Phase II trial, patients were randomized in a 3:3:1 ratio to receive two different doses of PF06425090 or placebo in two different dosing regimens [97]. In all, 855 healthy adults aged 65 to 85 years were randomized, and the primary efficacy endpoint was serum toxin A and B neutralizing antibodies measured at 37 days or 7 months depending on the dosing regimen. Of the patients who were randomized to receive the dosing regimen chosen for Phase III clinical trials (200 mcg at 0, 1, and 6 months), 95.6% achieved the prespecified threshold level of toxin A neutralizing antibody compared to 1.9% of patients who received placebo. Furthermore, 87.3% and 7.5% of patients achieved the prespecified threshold level of toxin B neutralizing antibody in the vaccine and placebo groups, respectively.
In the Phase III CLOVER Trial, PF06425090 was compared to placebo in patients aged ≥50 years who received systemic antibiotics in the previous 12 weeks or were at an increased risk of future contact with the healthcare system [98]. Investigators randomized patients to PF06425090 (n = 8766) or placebo (n = 8769) and compared rates of CDI that occurred ≥14 days following dose two or three and within three years following dose three [15]. Vaccine efficacy after dose two and three was calculated to be 28.6% (96.4% CI − 28.4 to 61.0%) and 31% (96.4% CI −38.7 to 66.6%), respectively. Notably, the final analysis was performed after only 42 CDIs had occurred, which highlights the difficulty in designing a study with enough power to detect a difference between groups should one exist. According to a press release, the trial did not meet its pre-specified primary endpoint, although the full results have not been published [99]. Pre-specified secondary outcomes included medically attended CDI and CDI duration. While 11/25 patients sought medical attention for CDI in the placebo group, 0/17 patients sought medical attention for CDI in the vaccine group. Additionally, the median CDI duration was numerically shorter in the vaccine group (1 vs 4 days). No unanticipated safety concerns were identified. These findings are encouraging and may influence future study methodology decisions in this arena.
4.2 Unnamed, Bivalent Toxoid Vaccine
A second vaccine candidate (Sanofi Pasteur) has undergone both Phase II (NCT01230957) and III (NCT01887912) clinical trials [100, 101]. This vaccine is also a bivalent toxoid vaccine that contains formalin-inactivated C. difficile toxin A and toxin B.
In its Phase II trial, patients aged 40–75 years with impending hospitalization within 60 days of enrollment or current or impending residence in a long-term care facility or rehabilitation facility were included. A total of 661 patients were randomized to receive two different doses of the vaccine or placebo with or without an aluminum hydroxide (AlOH) adjuvant in three different dosing regimens [100]. The primary efficacy endpoint was the proportion of patients who achieved a prespecified serum toxin A and B neutralizing antibody threshold measured at 60 days after the first dose of vaccine. Of the patients in the per protocol population who were randomized to receive the dosing regimen chosen for Phase III clinical trials (100 mcg [toxin A and toxin B in a 3:2 ratio] with an AlOH adjuvant at 0, 7, and 30 days), seroconversion rates for toxin A and B were 97% and 92%, respectively, compared to 7.9% and 13.2% in the placebo group.
In the Phase III Cdiffense trial, the vaccine was compared to placebo in patients aged ≥ 50 years with at least two previous hospital stays (each ≥ 24 h in duration) and systemic antibiotic receipt in the previous 12 months or who were anticipating a hospitalization for ≥ 72 h for a variety of pre-specified elective surgeries within 60 days of enrollment [101]. Investigators randomized patients in a 2:1 ratio to receive the vaccine (n = 6201) or placebo (n = 3101) and compared rates of CDI developing within 3 years following dose three, as diagnosed by PCR or by visually observing pseudomembranous colitis by colonoscopy. Among the mITT population, which included all patients who received at least one injection, 50 patients were diagnosed with CDI: 34/6173 patients in the vaccine group and 16/3085 patients in the placebo group. This corresponded to a rate of 0.29 infections per 100 person-years and 0.28 infections per 100 person-years, respectively, and a vaccine efficacy of − 5.2% (95% CI − 10.4 to 43.5%). The independent data monitoring committee subsequently recommended that the study be terminated for futility.
5 Conclusion
The diversity in approaches to CDI management continues to grow with our understanding of CDI pathogenesis and the multiple factors contributing to its development. One LBP has been approved by the FDA and another has filed for approval at the time of this writing, representing an exciting new compliment to existing antibiotic therapies. Ultra-narrow–spectrum antibiotics and vaccines are also in development, but appear to be further from approval. The availability of several antibiotics, a monoclonal antibody, and LBPs will create a future in which clinicians will be faced with several competing strategies to treat CDI and prevent CDI recurrence.
References
Voth DE, Ballard JD. Clostridium difficile toxins: mechanism of action and role in disease. Clin Microbiol Rev. 2005;18(2):247–63.
Buonomo EL, Petri WA Jr. The microbiota and immune response during Clostridium difficile infection. Anaerobe. 2016;41:79–84.
Bartlett JG, Gerding DN. Clinical recognition and diagnosis of Clostridium difficile infection. Clin Infect Dis. 2008;15(46 Suppl 1):S12–8.
Johnson S, Louie TJ, Gerding DN, Cornely OA, Chasan-Taber S, Fitts D, et al. Vancomycin, metronidazole, or tolevamer for Clostridium difficile infection: results from two multinational, randomized, controlled trials. Clin Infect Dis. 2014;59(3):345–54.
Paredes-Sabja D, Shen A, Sorg JA. Clostridium difficile spore biology: sporulation, germination, and spore structural proteins. Trends Microbiol. 2014;22(7):406–16.
Kraus CN, Lyerly MW, Carman RJ. Ambush of Clostridium difficile spores by ramoplanin: activity in an in vitro model. Antimicrob Agents Chemother. 2015;59(5):2525–30.
Babakhani F, Bouillaut L, Gomez A, Sears P, Nguyen L, Sonenshein AL. Fidaxomicin inhibits spore production in Clostridium difficile. Clin Infect Dis. 2012;55(Suppl 2):S162–9.
Chilton CH, Crowther GS, Ashwin H, Longshaw CM, Wilcox MH. Association of fidaxomicin with C. difficile spores: effects of persistence on subsequent spore recovery, outgrowth and toxin production. PLoS ONE. 2016;11(8):1200.
Basseres E, Endres BT, Montes-Bravo N, Perez-Soto N, Rashid T, Lancaster C, et al. Visualization of fidaxomicin association with the exosporium layer of Clostridioides difficile spores. Anaerobe. 2021;69: 102352.
Ochsner UA, Bell SJ, O’Leary AL, Hoang T, Stone KC, Young CL, et al. Inhibitory effect of REP3123 on toxin and spore formation in Clostridium difficile, and in vivo efficacy in a hamster gastrointestinal infection model. J Antimicrob Chemother. 2009;63(5):964–71.
Louie TJ, Miller MA, Mullane KM, Weiss K, Lentnek A, Golan Y, et al. Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011;364(5):422–31.
Cornely OA, Crook DW, Esposito R, Poirier A, Somero MS, Weiss K, et al. Fidaxomicin versus vancomycin for infection with Clostridium difficile in Europe, Canada, and the USA: a double-blind, non-inferiority, randomised controlled trial. Lancet Infect Dis. 2012;12(4):281–9.
Guery B, Menichetti F, Anttila V-J, Adomakoh N, Aguado JM, Bisnauthsing K, et al. Extended-pulsed fidaxomicin versus vancomycin for Clostridium difficile infection in patients 60 years and older (EXTEND): a randomised, controlled, open-label, phase 3b/4 trial. Lancet Infect Dis. 2018;18(3):296–307.
Mikamo H, Tateda K, Yanagihara K, Kusachi S, Takesue Y, Miki T, et al. Efficacy and safety of fidaxomicin for the treatment of Clostridioides (Clostridium) difficile infection in a randomized, double-blind, comparative Phase III study in Japan. J Infect Chemother. 2018;24(9):744–52.
Britton RA, Young VB. Role of the intestinal microbiota in resistance to colonization by Clostridium difficile. Gastroenterology. 2014;146(6):1547–53.
Allegretti JR, Kearney S, Li N, Bogart E, Bullock K, Gerber GK, et al. Recurrent Clostridium difficile infection associates with distinct bile acid and microbiome profiles. Aliment Pharmacol Ther. 2016;43(11):1142–53.
Rashid MU, Zaura E, Buijs MJ, Keijser BJ, Crielaard W, Nord CE, et al. Determining the long-term effect of antibiotic administration on the human normal intestinal microbiota using culture and pyrosequencing methods. Clin Infect Dis. 2015;15(60 Suppl 2):S77-84.
Lewis BB, Buffie CG, Carter RA, Leiner I, Toussaint NC, Miller LC, et al. Loss of microbiota-mediated colonization resistance to Clostridium difficile infection with oral vancomycin compared with metronidazole. J Infect Dis. 2015;212(10):1656–65.
Louie TJ, Cannon K, Byrne B, Emery J, Ward L, Eyben M, et al. Fidaxomicin preserves the intestinal microbiome during and after treatment of Clostridium difficile infection (CDI) and reduces both toxin reexpression and recurrence of CDI. Clin Infect Dis. 2012;55(Suppl 2):S132–42.
Edlund C, Barkholt L, Olsson-Liljequist B, Nord CE. Effect of vancomycin on intestinal flora of patients who previously received antimicrobial therapy. Clin Infect Dis. 1997;25(3):729–32.
Food and Drug Administration (FDA). Early clinical trials with live biotherapeutic products: chemistry, manufacturing, and control information. 2016. https://www.fda.gov/files/vaccines,%20blood%20%26%20biologics/published/Early-Clinical-Trials-With-Live-Biotherapeutic-Products--Chemistry--Manufacturing--and-Control-Information--Guidance-for-Industry.pdf. Accessed 12 Jan 2023.
Cordaillat-Simmons M, Rouanet A, Pot B. Live biotherapeutic products: the importance of a defined regulatory framework. Exp Mol Med. 2020;52(9):1397–406.
Cohen SH, Gerding DN, Johnson S, Kelly CP, Loo VG, McDonald LC, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31(5):431–55.
Gerding DN, Johnson S, Peterson LR, Mulligan ME, Silva J Jr. Clostridium difficile-associated diarrhea and colitis. Infect Control Hosp Epidemiol. 1995;16(8):459–77.
Surawicz CM, Brandt LJ, Binion DG, Ananthakrishnan AN, Curry SR, Gilligan PH, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108(4):478–98 (quiz 99).
Bauer MP, Kuijper EJ, van Dissel JT. European Society of Clinical Microbiology and Infectious Diseases (ESCMID): treatment guidance document for Clostridium difficile infection (CDI). Clin Microbiol Infect. 2009;15(12):1067–79.
Debast SB, Bauer MP, Kuijper EJ, European Society of Clinical M, Infectious D. European Society of Clinical Microbiology and Infectious Diseases: update of the treatment guidance document for Clostridium difficile infection. Clin Microbiol Infect. 2014;20(Suppl 2):1–26.
McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018;66(7):e1–48.
Johnson S, Lavergne V, Skinner AM, Gonzales-Luna AJ, Garey KW, Kelly CP, et al. Clinical Practice Guideline by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA): 2021 Focused Update Guidelines on Management of Clostridioides difficile infection in adults. Clin Infect Dis. 2021;73(5):e1029–44.
Kelly CR, Fischer M, Allegretti JR, LaPlante K, Stewart DB, Limketkai BN, et al. ACG clinical guidelines: prevention, diagnosis, and treatment of Clostridioides difficile Infections. Am J Gastroenterol. 2021;116(6):1124–47.
van Prehn J, Reigadas E, Vogelzang EH, Bouza E, Hristea A, Guery B, et al. European Society of Clinical Microbiology and Infectious Diseases: 2021 update on the treatment guidance document for Clostridioides difficile infection in adults. Clin Microbiol Infect. 2021;27(Suppl 2):S1–21.
Beinortas T, Burr NE, Wilcox MH, Subramanian V. Comparative efficacy of treatments for Clostridium difficile infection: a systematic review and network meta-analysis. Lancet Infect Dis. 2018;18(9):1035–44.
Carlson TJ, Gonzales-Luna AJ. Antibiotic treatment pipeline for Clostridioides difficile infection (CDI): A wide array of narrow-spectrum agents. Curr Infect Dis Rep. 2020;22(8):20. https://doi.org/10.1007/s11908-020-00730-1.
Vickers RJ, Tillotson GS, Nathan R, Hazan S, Pullman J, Lucasti C, et al. Efficacy and safety of ridinilazole compared with vancomycin for the treatment of Clostridium difficile infection: a phase 2, randomised, double-blind, active-controlled, non-inferiority study. Lancet Infect Dis. 2017;17(7):735–44.
A phase 3, randomized, double-blind, active controlled study to compare the efficacy and safety of ridinilazole (200 mg, bid) for 10 days with vancomycin (125 mg, qid) for 10 days in the treatment of Clostridium difficile infection (CDI). https://ClinicalTrials.gov/show/NCT03595553. Accessed 21 Sep 2022.
A phase 3, randomized, double-blind, active controlled study to compare the efficacy and safety of ridinilazole (200 mg, bid) for 10 days with vancomycin (125 mg, qid) for 10 days in the treatment of Clostridium difficile infection (CDI). https://ClinicalTrials.gov/show/NCT03595566. Accessed 21 Sep 2022.
Thorpe CM, Kane AV, Chang J, Tai A, Vickers RJ, Snydman DR. Enhanced preservation of the human intestinal microbiota by ridinilazole, a novel Clostridium difficile-targeting antibacterial, compared to vancomycin. PLoS ONE. 2018;13(8): e0199810.
Qian X, Yanagi K, Kane AV, Alden N, Lei M, Snydman DR, et al. Ridinilazole, a narrow spectrum antibiotic for treatment of Clostridioides difficile infection, enhances preservation of microbiota-dependent bile acids. Am J Physiol Gastrointest Liver Physiol. 2020;319(2):G227–37.
Summit Therapeutics, Inc. Summit Therapeutics announces topline results for phase III Ri-CoDIFy study for C. difficile infection. 2021. https://www.summittxinc.com/app/uploads/2021/12/2021_PR_1220_TLR-Announcement-_-FINAL.pdf. Accessed 21 Sep 2022.
Okhuysen PC. “Ri-CoDIFy—A phase 3, randomized, double-blind study to evaluate the efficacy and safety of ridinilazole compared with vancomycin for the treatment of Clostridioides difficile infection”. ID Week. Washington, D.C. October 20, 2022.
Summit Therapeutics, Inc. Summit Therapeutics provides update on ridinilazole. 2022; Available from: https://www.summittxinc.com/app/uploads/2022/07/2022_PR_0714_Ridinilazole-Update-_-FINAL-1.pdf. Accessed 21 Sep 2022.
A randomized, double-blind, active controlled study to evaluate the safety and tolerability of ridinilazole compared with vancomycin and to assess the pharmacokinetics of ridinilazole in adolescent subjects (aged 12 to <18 years) with Clostridioides difficile infection. https://ClinicalTrials.gov/show/NCT04802837. Accessed 21 Sep 2022.
Wolf J, Kalocsai K, Fortuny C, Lazar S, Bosis S, Korczowski B, et al. Safety and efficacy of fidaxomicin and vancomycin in children and adolescents with clostridioides (Clostridium) difficile infection: a phase 3, multicenter, randomized, single-blind clinical trial (SUNSHINE). Clin Infect Dis. 2020;71(10):2581–8.
Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11(8):506–14.
Freedman SB, Schnadower D, Tarr PI. The probiotic conundrum: regulatory confusion, conflicting studies, and safety concerns. JAMA. 2020;323(9):823–4.
Mazzantini D, Calvigioni M, Celandroni F, Lupetti A, Ghelardi E. Spotlight on the compositional quality of probiotic formulations marketed worldwide. Front Microbiol. 2021;12: 693973.
Goldenberg JZ, Yap C, Lytvyn L, Lo CK, Beardsley J, Mertz D, et al. Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Cochrane Database Syst Rev. 2017;12:CD006095.
Allen SJ, Wareham K, Wang D, Bradley C, Sewell B, Hutchings H, et al. A high-dose preparation of lactobacilli and bifidobacteria in the prevention of antibiotic-associated and Clostridium difficile diarrhoea in older people admitted to hospital: a multicentre, randomised, double-blind, placebo-controlled, parallel arm trial (PLACIDE). Health Technol Assess. 2013;17(57):1–140.
Barker AK, Duster M, Valentine S, Hess T, Archbald-Pannone L, Guerrant R, et al. A randomized controlled trial of probiotics for Clostridium difficile infection in adults (PICO). J Antimicrob Chemother. 2017;72(11):3177–80.
McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018;66(7):987–94.
Hoffmann DE, Palumbo FB, Ravel J, Rowthorn V, von Rosenvinge E. A proposed definition of microbiota transplantation for regulatory purposes. Gut Microbes. 2017;8(3):208–13.
Vindigni SM, Surawicz CM. Fecal microbiota transplantation. Gastroenterol Clin N Am. 2017;46(1):171–85.
Allegretti JR, Mullish BH, Kelly C, Fischer M. The evolution of the use of faecal microbiota transplantation and emerging therapeutic indications. Lancet. 2019;394(10196):420–31.
Food and Drug Administration (FDA). Enforcement policy regarding investigational new drug requirements for use of fecal microbiota for transplantation to treat clostridium difficile infection not responsive to standard therapies. FDA Guideance document Docket Number: FDA-2013-D-0811. 2016.
Kelly CR, Yen EF, Grinspan AM, Kahn SA, Atreja A, Lewis JD, et al. Fecal microbiota transplantation is highly effective in real-world practice: initial results from the FMT National Registry. Gastroenterology. 2021;160(1):183-92e3.
DeFilipp Z, Bloom PP, Torres Soto M, Mansour MK, Sater MRA, Huntley MH, et al. Drug-resistant E. coli bacteremia transmitted by fecal microbiota transplant. N Engl J Med. 2019;381(21):2043–50.
Food and Drug Amdinistration (FDA). Safety Alert Regarding Use of Fecal Microbiota for Transplantation and Additional Safety Protections Pertaining to SARS-CoV-2 and COVID-19. 2020 [cited November 22 2022]; Available from: https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/safety-alert-regarding-use-fecal-microbiota-transplantation-and-additional-safety-protections. Accessed 12 Jan 2023.
Hamilton MJ, Weingarden AR, Sadowsky MJ, Khoruts A. Standardized frozen preparation for transplantation of fecal microbiota for recurrent Clostridium difficile infection. Am J Gastroenterol. 2012;107(5):761–7.
Staley C, Hamilton MJ, Vaughn BP, Graiziger CT, Newman KM, Kabage AJ, et al. Successful resolution of recurrent Clostridium difficile infection using freeze-dried, encapsulated fecal microbiota; pragmatic cohort study. Am J Gastroenterol. 2017;112(6):940–7.
Khanna S, Kelly CR, Louie T, Fisher M, Hota S, Misra B, et al. S131. CP101, an investigational orally administered microbiome therapeutic, increases intestinal microbiome diversity and prevents recurrent C. difficile infection: results from a randomized, placebo-controlled trial. Am J Gastroenterol. 2021;116(1):S57-S.
Allegretti JR, Kelly CR, Louie T, Fisher M, Hota S, Misra B, et al. S145. Week 24 efficacy and safety data from PRISM3: a randomized, placebo-controlled trial evaluating CP101, an investigational orally administered microbiome therapeutic for the prevention of recurrent C. difficile infection. Am J Gastroenterol. 2021;116(1):S63–4.
Allegretti JR, Kelly CR, Louie T, Fisher M, Hota S, Misra B, et al. LB21 An investigational oral microbiome drug, CP101, for the prevention of recurrent Clostridioides difficile infection: a randomized, placebo-controlled, multi-center trial (PRISM3). United Eur Gastroenterol J. 2020;8(10):1270–1.
Allegretti JR, Kelly CR, Fischer M, Cohen T, Gerardin Y, Budree S, et al. 583: CP101, an investigational orally administered microbiome therapeutic, was effective for prevention of recurrent C. difficile infection: results from open-label PRISM-EXT trial. Gastroenterology. 2022;162(7):S-143.
Allegretti JR, Kelly CR, Fischer M, Cohen T, Budree S, Khanna S. Tu1519: CP101, an investigational microbiome therapeutic for the prevention of recurrent C. difficile infection: a combined analysis of the PRISM3 (Randomized Placebo-Controlled) and PRISM-EXT (Open-Label) trials. Gastroenterology. 2022;162(7):S-995-S6-6.
A Trial of CP101 for the Prevention of Recurrent CDI (PRISM4). 2022 [cited 2022 September 20]; Available from: https://clinicaltrials.gov/ct2/show/record/NCT05153499
Finch Therapeutics. Finch therapeutics provides an update on its phase 3 trial of CP101 in recurrent C. difficile infection. 2022. https://ir.finchtherapeutics.com/news-releases/news-release-details/finch-therapeutics-provides-update-its-phase-3-trial-cp101. Accessed 12 Jan 2023.
Finch Therapeutics. Finch therapeutics provides corporate updates and reports second Quarter 2022 Financial Results. 2022. https://ir.finchtherapeutics.com/news-releases/news-release-details/finch-therapeutics-provides-corporate-updates-and-reports-second. Accessed 12 Jan 2023.
Kelly CR, Khoruts A, Staley C, Sadowsky MJ, Abd M, Alani M, et al. Effect of fecal microbiota transplantation on recurrence in multiply recurrent Clostridium difficile infection: a randomized trial. Ann Intern Med. 2016;165(9):609–16.
Orenstein R, Dubberke E, Hardi R, Ray A, Mullane K, Pardi DS, et al. Safety and durability of RBX2660 (Microbiota Suspension) for recurrent Clostridium difficile infection: results of the PUNCH CD study. Clin Infect Dis. 2016;62(5):596–602.
Ray A, Jones C. Does the donor matter? Donor vs patient effects in the outcome of a next-generation microbiota-based drug trial for recurrent Clostridium difficile infection. Future Microbiol. 2016;11:611–6.
Orenstein R, Dubberke ER, Khanna S, Lee CH, Yoho D, Johnson S, et al. Durable reduction of Clostridioides difficile infection recurrence and microbiome restoration after treatment with RBX2660: results from an open-label phase 2 clinical trial. BMC Infect Dis. 2022;22(1):245.
Khanna S, Assi M, Lee C, Yoho D, Louie T, Knapple W, et al. Efficacy and safety of RBX2660 in PUNCH CD3, a Phase III, randomized, double-blind, placebo-controlled trial with a Bayesian primary analysis for the prevention of recurrent Clostridioides difficile infection. Drugs. 2022;82(15):1527–38.
U.S. Food & Drug Administration. Rebyota. 2022. https://www.fda.gov/vaccines-blood-biologics/vaccines/rebyota. Accessed 19 Dec 2022.
Kraft C, Khanna S, Assi M, Feuerstadt P, Harvey A, Bancke L. Sa611 interim analysis of a phase 3 open-label study indicates safety and efficacy of RBX2660, an investigational live biotherapeutic, in a “Real-world” population of patients with recurrent Clostridioides difficile infection. Gastroenterology. 2021;160(6):S-573.
Bancke L, Su X. 167. Efficacy of investigational microbiota-based live biotherapeutic RBX2660 in individuals with recurrent Clostridioides difficile infection: data from five prospective clinical studies. Open Forum Infect Dis. 2021;8(Supplement_1):S100–1.
Dubberke ER, Lee CH, Orenstein R, Khanna S, Hecht G, Gerding DN. Results from a randomized, placebo-controlled clinical trial of a RBX2660-a microbiota-based drug for the prevention of recurrent Clostridium difficile infection. Clin Infect Dis. 2018;67(8):1198–204.
Langdon A, Schwartz DJ, Bulow C, Sun X, Hink T, Reske KA, et al. Microbiota restoration reduces antibiotic-resistant bacteria gut colonization in patients with recurrent Clostridioides difficile infection from the open-label PUNCH CD study. Genome Med. 2021;13(1):28.
Blount KF, Shannon WD, Deych E, Jones C. Restoration of bacterial microbiome composition and diversity among treatment responders in a phase 2 trial of RBX2660: an investigational microbiome restoration therapeutic. Open Forum Infect Dis. 2019;6(4):ofz095.
Kwak S, Choi J, Hink T, Reske KA, Blount K, Jones C, et al. Impact of investigational microbiota therapeutic RBX2660 on the gut microbiome and resistome revealed by a placebo-controlled clinical trial. Microbiome. 2020;8(1):125.
Blount K, Jones C, Walsh D, Gonzalez C, Shannon WD. Development and validation of a novel microbiome-based biomarker of post-antibiotic dysbiosis and subsequent restoration. Front Microbiol. 2021;12: 781275.
Blount K, Hau H, Papzyan R, Fuchs B, Shannon B, Gonzalez C. Microbiome and bile acid restoration was consistent across three clinical trials of RBX2660 for recurrent Clostridioides difficile infection: a combined analysis. In: Presented at: Digestive Disease Week; 2022 May 21–24, 2022; San Diego, CA; 2022.
Papazyan R, Fuchs B, Blount K, Gonzalez C, Shannon B. 1039. rapid restoration of bile acid compositions after treatment with rbx2660 for recurrent Clostridioides difficile infection—results from the PUNCH CD3 Phase 3 Trial. Open Forum Infectious Dis. 2021;8(1):S610-S.
Hau H, Walsh D, Gonzalez C, Shannon B, Blount K. 129. Antimicrobial Resistance Genes Were Reduced Following Administration of Investigational Microbiota-Based Live Biotherapeutic RBX2660 to Individuals with Recurrent Clostridioides difficile Infection. Open Forum Infect Dis. 2021;8:S79.
Dubberke ER, Mullane KM, Gerding DN, Lee CH, Louie TJ, Guthertz H, et al. Clearance of vancomycin-resistant enterococcus concomitant with administration of a microbiota-based drug targeted at recurrent Clostridium difficile infection. Open Forum Infect Dis. 2016;3(3):ofw133.
Khanna S, Pardi DS, Kelly CR, Kraft CS, Dhere T, Henn MR, et al. A novel microbiome therapeutic increases gut microbial diversity and prevents recurrent Clostridium difficile infection. J Infect Dis. 2016;214(2):173–81.
McGovern BH, Ford CB, Henn MR, Pardi DS, Khanna S, Hohmann EL, et al. SER-109, an investigational microbiome drug to reduce recurrence after Clostridioides difficile infection: lessons learned from a phase 2 trial. Clin Infect Dis. 2021;72(12):2132–40.
Feuerstadt P, Louie TJ, Lashner B, Wang EEL, Diao L, Bryant JA, et al. SER-109, an oral microbiome therapy for recurrent Clostridioides difficile infection. N Engl J Med. 2022;386(3):220–9.
Seres Therapeutics Inc. Seres Therapeutics Announces Confirmatory Results From Investigational Microbiome Therapeutic SER-109 ECOSPOR IV Open-Label Study in Recurrent C. difficile Infection. 2022.
Khanna S, Feuerstadt P, Huang E, Oneto C, Pardi DS, Wang EE, et al. Oral 63 – An Open-Label Study (ECOSPOR IV) to Evaluate the Safety, Efficacy and Durability of SER-109, an Investigational Oral Microbiome Therapeutic, in Adults With Recurrent Clostridioides difficile Infection (rCDI). In: ACG 2022; 2022; Charlotte, NC.; 2022.
Seres Therapeutics Inc. Seres Therapeutics Announces Completion Of Rolling BLA Submission To FDA For Investigational Microbiome Therapeutic SER-109 For Recurrent C. difficile Infection. 2022.
Seres Therapeutics Inc. Seres Therapeutics Announces FDA Acceptance of Biologics License Application for Investigational Microbiome Therapeutic SER-109 for Recurrent C. difficile Infection for Priority Review. 2022.
Johnson S, Gerding DN. Bezlotoxumab. Clin Infect Dis. 2019;68(4):699–704.
Dose confirmation, immunogenicity and safety study of the Clostridium difficile vaccine candidate VLA84 in healthy adults aged 50 years and older: a randomized, controlled, observer-blind phase II study. 2014 [cited 2022 September 21]; Available from: https://ClinicalTrials.gov/show/NCT02316470
Safety and Immunogenicity Study of GSK's Clostridium Difficile Vaccine 2904545A When Administered in Healthy Adults Aged 18-45 Years and 50-70 Years. 2019 [cited 2022 September 21]; Available from: https://ClinicalTrials.gov/show/NCT04026009.
Kokai-Kun JF, Roberts T, Coughlin O, Le C, Whalen H, Stevenson R, et al. Use of ribaxamase (SYN-004), a beta-lactamase, to prevent Clostridium difficile infection in beta-lactam-treated patients: a double-blind, phase 2b, randomised placebo-controlled trial. Lancet Infect Dis. 2019;19(5):487–96.
Vehreschild M, Ducher A, Louie T, Cornely OA, Feger C, Dane A, et al. An open randomized multicentre Phase 2 trial to assess the safety of DAV132 and its efficacy to protect gut microbiota diversity in hospitalized patients treated with fluoroquinolones. J Antimicrob Chemother. 2022;77(4):1155–65.
Kitchin N, Remich SA, Peterson J, Peng Y, Gruber WC, Jansen KU, et al. A phase 2 study evaluating the safety, tolerability, and immunogenicity of two 3-dose regimens of a Clostridium difficile vaccine in healthy us adults aged 65 to 85 years. Clin Infect Dis. 2020;70(1):1–10.
A phase 3, placebo-controlled, randomized, observer-blinded study to evaluate the efficacy, safety, and tolerability of a Clostridium difficile vaccine in adults 50 years of age and older. https://ClinicalTrials.gov/show/NCT03090191. Accessed 21 Sept 2022.
Pfizer, Inc. Phase 3 CLOVER Trial for Pfizer’s investigationalClostridioides difficile vaccine indicates strong potential effect in reducing duration and severity of disease based on secondary endpoints. 2022. https://www.pfizer.com/news/press-release/press-release-detail/phase-3-clover-trial-pfizers-investigational-clostridioides. Accessed 21 Sep 2022.
de Bruyn G, Saleh J, Workman D, Pollak R, Elinoff V, Fraser NJ, et al. Defining the optimal formulation and schedule of a candidate toxoid vaccine against Clostridium difficile infection: A randomized Phase 2 clinical trial. Vaccine. 2016;34(19):2170–8.
de Bruyn G, Gordon DL, Steiner T, Tambyah P, Cosgrove C, Martens M, et al. Safety, immunogenicity, and efficacy of a Clostridioides difficile toxoid vaccine candidate: a phase 3 multicentre, observer-blind, randomised, controlled trial. Lancet Infect Dis. 2021;21(2):252–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding relevant to this review was provided to the authors or affiliated institutions.
Competing interests
AJGL and TJC have no competing interests to declare that are relevant to the content of this article. KWG has received research support from Acurx Pharmaceuticals, Summit Therapeutics, and Seres Therapeutics.
Author contributions
All authors on the submission made substantial contributions to the project: AJGL and TJC drafted the work and AJGL, TJC, and KWG revised it critically for important intellectual content. All authors have approved the version to be published and agree to be accountable for all aspects of the work.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gonzales-Luna, A.J., Carlson, T.J. & Garey, K.W. Emerging Options for the Prevention and Management of Clostridioides difficile Infection. Drugs 83, 105–116 (2023). https://doi.org/10.1007/s40265-022-01832-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-022-01832-x