Abstract
Introduction and Objective
The recent rise in acute kidney injury (AKI) incidence, with approximately 30% attributed to potentially preventable adverse drug events (ADEs), poses challenges in evaluating drug-induced AKI due to polypharmacy and other risk factors. This study seeks to consolidate knowledge on the drugs with AKI potential from four distinct sources: (i) bio(medical) peer-reviewed journals; (ii) spontaneous reporting systems (SRS); (iii) drug information databases (DIDs); and (iv) NephroTox website. By harnessing the potential of these underutilised sources, our objective is to bridge gaps and enhance the understanding of drug-induced AKI.
Methods
By searching Medline, studies with lists of drugs with AKI potential established through consensus amongst medical experts were selected. A final list of 63 drugs was generated aggregating the original studies. For these 63 drugs, the AKI reporting odds ratios (RORs) using three SRS databases, the average frequency of ADEs from four different DIDs and the number of published studies identified via NephroTox was reported.
Results
Drugs belonging to the antivirals, antibacterials, and non-steroidal anti-inflammatory pharmacological classes exhibit substantial consensus on AKI potential, which was also reflected in strong ROR signals, frequent to very frequent AKI-related ADEs and a high number of published studies reporting adverse kidney events as identified via NephroTox. Renin-angiotensin aldosterone system inhibitors and diuretics also display comparable signal strengths, but this can be attributed to expected haemodynamic changes. More variability is noted for proton-pump inhibitors.
Conclusions
By integrating four disjointed sources of knowledge, we have created a novel, comprehensive resource on drugs with AKI potential, contributing to kidney safety improvement efforts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This study integrates knowledge from four previously underutilised sources on 63 drugs with acute kidney injury (AKI) potential into one overarching resource. |
The sources included display high concordance for drugs with very strong agreement amongst experts regarding AKI potential and higher variability for drugs with moderate agreement. |
This novel and comprehensive resource is designed to raise awareness, aid in nephrotoxin stewardship and inform future research on endeavours pertaining to drug-induced AKI. |
1 Introduction
Acute kidney injury (AKI) is a sudden decline in kidney function. It is identified by the increase of serum creatinine concentrations or reduced urinary output within seven days [1]. Over the past decades, AKI has risen into prominence due to its increasing world-wide prevalence [2]. Approximately 20% of hospitalised adults are reported to experience an AKI episode during their hospital stay [3, 4]. Additionally, AKI has been associated with both short- and long-term risk of poor outcomes, leading to a higher healthcare demand [5, 6].
Acute kidney injury can arise from diverse aetiologies, including sepsis, cardiac surgery, acute liver failure, amongst others [7]. Drugs are estimated to account for 19–26% of all cases of AKI in hospitalised patients [8] and recent appeals to improve kidney safety highlight the urgency to mitigate drug-induced acute kidney injury (DAKI) [9]. However, drugs which may cause AKI and the strength of the causal relationship between various drugs and AKI remain a subject of debate [10]. Challenges in identifying DAKI are exacerbated by escalating trends of polypharmacy, the prevalence of multi-morbidity patterns and an ageing population in high-income countries [11, 12]. Furthermore, there is still room for exploration for reliable and specific in vitro models [13], DAKI biomarkers [14] and further studies defining DAKI sub-phenotypes [15].
A number of studies have gathered existing evidence about the potential of drugs to cause AKI using expert consensus [16,17,18,19] observational data [20, 21], previously published studies [21,22,23] and databases of spontaneous reporting systems (SRS) [24,25,26,27]. This has resulted in various enumerations of active substances associated with AKI. However, most of these studies have been conducted in the USA, leaving a gap in knowledge regarding regions with similar socioeconomic standards. Furthermore, the potential of drug information databases (DIDs) containing summaries of product characteristics remains underutilised despite its promise in offering valuable insights on the potential of drugs to cause AKI [28].
This study expands beyond the conventional scope, incorporating previously untapped knowledge sources on drugs that may cause AKI such as SRS databases, DIDs and NephroTox, a database that aggregates nephrotoxicity studies. Through this integration, we harness the potential of these sources, aiming to provide a comprehensive, multi-source overview of fragmented knowledge. To achieve our objective, we retrieved information about drugs with AKI potential and approved in the Netherlands according to the Medicines Evaluation Board from four different knowledge sources: (i) Medline; (ii) three SRS databases; (iii) four DIDs; and (iv) the NephroTox website. This approach led us to hypothesise that it could culminate in the development of a rigorous catalogue of drugs exhibiting AKI potential. By broadening the horizon of knowledge sources and delving into the nuanced aspects required for a thorough understanding of the potential of drugs to cause AKI, we sought to bridge gaps in existing knowledge. This contribution aligns with the standardisation of nephrotoxin surveillance and efforts in AKI prevention and detection.
2 Methods
We utilised expert consensus studies obtained using a Medline query, to select the drugs with AKI potential (knowledge retrieval step) and subsequently characterised the AKI potential of the selected drugs using SRS databases, DIDs and NephroTox. Below, we provide a detailed description of knowledge retrieval, pre-processing, and analyses by source and an overview of the methods in Figure 1. Information about drugs with AKI potential obtained from these four sources were compiled to generate the final resource. Finally, contextualisation with existing evidence is provided to support interpretation of the different data sources collected and consolidate the knowledge gathered.
Workflow for generating drugs with AKI potential resource by assembling four knowledge sources: Medline (in blue), SRS databases (in green), DIDs (in orange), NephroTox (in red). AKI acute kidney injury, avg average, DID drug information database, FK Farmacotherapeutisch Kompas, ICSR individual case safety report, IM Informatorium Medicamentorum, INN international non-proprietary name, MedDRA® Medical Dictionary for Regulatory Activities, ROR reporting odds ratio, SIDER Side Effect Resource, SMQ standardised MedDRA® query, SRS spontaneous reporting system
2.1 Knowledge Sources
2.1.1 Expert Consensus Lists of Drugs with AKI Potential
As a starting point, we searched Medline (from January 1, 2013 to July 1, 2024) to identify peer-reviewed publications in which a list of drugs with AKI potential was presented based on consensus among medical experts. We used combinations of the Medical Subject Headings (MeSH) Major Topic descriptors (see Electronic Supplementary Material #1, Table 1). One researcher (J.E.L.) screened the titles, abstracts and full texts using the following inclusion and exclusion criteria: (i) focussed on AKI phenotype or related terms; (ii) the publication should have been issued after 2012, when the Kidney Disease: Improving Global Outcomes (KDIGO) Clinical Practice Guideline for AKI [1] was published; (iii) the target population should be adults only; (iv) focussed on hospital drug utilisation; (v) provided information on how corresponding primary literature was retrieved; and (vi) medical professionals (i.e., medical doctors, pharmacists, nurses, etc.) should be involved in the assessment of the evidence with consensus amongst the reviewers for the generation of the list. To limit selection bias, a second reviewer (J.E.K.) was consulted on the occasions where the first reviewer (J.E.L.) was uncertain about the appropriateness of an article. The second reviewer also verified the final list of included articles. For an illustration of the process, see Electronic Supplementary Material #1, Fig. 1.
2.1.2 SRS Databases
Access to anonymised individual case safety reports (ICSRs) about AKI-related adverse drug events (ADEs) was gained for three major international SRS databases [29], namely, EudraVigilance (EV) [30] curated by the European Medicines Agency (EMA), Database of Adverse Event Notifications (DAEN) [31] maintained by the Australian Therapeutic Goods Administration (TGA) and Canada Vigilance Adverse Reaction (CVAR) online database [32] from Health Canada (HC). The analyses focussed on the period between January 1, 2012 to December 31, 2022. For CVAR and DAEN, data were directly extracted from their corresponding websites in August 2023. An analysis covering the same time was requested to the EMA using EV and was performed between October and December 2023.
2.1.3 Drug Information Databases
In total we utilised four online DIDs—two were international and two were national (Dutch). The international DIDs were: the Side Effect Resource (SIDER) database of drugs and ADEs version 4.1 [33] and Micromedex® [34]. Informatorium Medicamentorum (IM) curated and maintained by the Royal Dutch Pharmacists Association (Koninklijke Nederlandse Maatschappij ter bevordering der Pharmacie, KNMP) [35], and the Farmacotherapeutisch Kompas (FK) curated and maintained by Zorginstituut Nederland [36] represented the Dutch DID resources.
2.1.4 NephroTox
NephroTox is an online resource aggregating studies available in PubMed® in which adverse kidney events due to drugs are reported [37]. It has an integrated search engine with its queries based on MeSH search strings. NephroTox was created by staff from the University of Basel headed by Prof. Dr. Med. Michael J. Mihatsch.
2.2 Pre-Processing and Information Retrieval
2.2.1 Drug Name Normalisation
For drug name standardisation, drugs with AKI potential were normalised to their corresponding international non-proprietary name (INN) based on drug brand name or active ingredients for each knowledge source, with manual mapping for CVAR and DAEN.
2.2.2 Expert Consensus Lists of Drugs with AKI Potential
One researcher (J.E.L.) extracted the drugs and information about their AKI potential from the included studies. Only drugs with certain to moderate AKI potential, as assessed via consensus by medical experts, were selected for comparison of the lists in this study. Drugs whose AKI potential was assessed as unlikely by experts were excluded from this comparison. Subsequently, the lists with drugs having certain to moderate AKI potential were compared by one researcher (J.E.L.) to assess agreement between the lists. Only drugs with high to moderate agreement between the lists were selected for further analysis using SRS databases, DIDs and NephroTox website in this study.
2.2.3 SRS Databases
The following inclusion for ICSRs were applied: (i) ICSRs submitted by healthcare professionals; and (ii) ICSRs were submitted in the jurisdiction of each regulatory authority. The exclusion criteria were: (i) ICSRs concerning patients aged < 18 years and > 110 years; (ii) ICSRs could only contain the INN of interest (i.e., one of the selected 63 drugs), ICSRs containing additional INNs besides the INN of interest were excluded to avoid drug-drug interaction signals; and (iii) drugs administered via non-systemic routes (e.g., topical creams, ophthalmological preparations). The ICSRs were de-duplicated.
To identify AKI-related ADEs in ICSRs (AKI ICSRs) of the selected drugs, the standardised Medical Dictionary for Regulatory Activities (MedDRA®) query (SMQ) v26.0 for Acute Renal Failure (SMQ code: 20000003) was used as the starting point for selecting relevant preferred terms (PT) (see Electronic Supplementary Material #1, Table 2), which hereinafter we refer to as AKI SMQ.
2.2.4 Drug Information Databases
To search for the selected drugs in SIDER and FK, we used Anatomical Therapeutic Chemical (ATC) codes for systemic administrations (see Electronic Supplementary Material #1, Table 3), and in IM and Micromedex® we used INN. To search for AKI-related ADEs of the selected drugs, in SIDER, which supports MedDRA® terminology, we used AKI SMQ PT descriptors and extracted them programmatically. In Micromedex®, FK and IM, MedDRA® terminology is not supported. Therefore, for each selected drug we extracted AKI-related ADE terms manually from the ‘Renal effects’ subsection in the medication safety section, and ‘Side-effects’ section, for Micromedex® and IM, respectively. For FK, web scraping using Python v3.2 with Beautiful Soup v4.8.1 package was performed to extract AKI-related ADEs from ‘Side-effects’ section. Subsequently, we manually mapped AKI-related ADE terms to MedDRA® AKI SMQ PT descriptors. For Dutch DIDs, MedDRA® v26.0 AKI PT descriptors were translated (see Electronic Supplementary Material #1, Table 4).
2.2.5 NephroTox
Each selected drug was entered using INN. In the instances where NephroTox integrated search engine failed to return hits due to the non-existence of MeSH term for the drug, the same query was executed manually in PubMed® replacing the drug MeSH term by its INN.
2.3 Knowledge Source Analyses
2.3.1 Expert Consensus Lists of Drugs with AKI Potential
The number of times drugs appeared in the included studies was tallied up to gauge the degree of agreement between the lists. Based on the total number of counts, drugs with AKI potential were classed into four agreement categories: very strong, strong, moderate and limited agreement amongst lists of drugs with AKI potential from expert consensus studies. Their corresponding pharmacological classes based on ATC nomenclature was reported and aggregated counts per class were provided. As mentioned earlier, we selected drugs with moderate to very strong agreement between the included lists for the subsequent analyses. For the selected drugs, we retrieved information about the AKI mechanism following the most recent expert-based recommendation for classifying drug-induced kidney diseases using functional and damage biomarkers [8]. In its turn, this classification system builds upon a framework initially established by the Acute Dialysis Quality Initiative (ADQI) group [38]. They identify two major mechanisms: kidney dysfunction (i.e., systemic, renal or glomerular haemodynamic effects) and/or kidney damage (i.e., structural or tubular damage). These mechanisms may co-occur or manifest separately and give place to four distinct subgroups, which enable a more nuanced interpretation of AKI diagnosis.
2.3.2 SRS Databases
For disproportionality analysis, the reporting odds ratio (ROR) was chosen as the disproportionality statistic for each selected drug using the contingency table described in Table 1 and Eqs. (1) and (2). This disproportionality measure has been shown to be advantageous over others [39] and it is the preferred method to EMA [40]. The ROR was calculated for each SRS database using the pre-processed ICSRs separately. A signal of disproportionate reporting was defined with the following criteria in line with EMA recommendations [40]: (i) the lower bound of the 95% confidence interval greater than 1; and (ii) the number of ICSRs per drug should be ≥ 5, except for those contained in the EMA additional monitoring list [41] for which ICSRs should be ≥ 3. For drugs with less than the specified number of ICSRs, the ROR was not reported.
2.4 Drug Information Databases
For the selected drugs, the frequencies of their AKI-related ADEs were extracted from the four DIDs considered in this study. To remove redundancy, AKI-related ADEs referring to the same PT were averaged. Acute kidney injury-related ADEs expressed as ranges (e.g., 10–20%) were averaged and then rounded to the nearest integer. For SIDER, available placebo frequencies were also extracted. Acute kidney injury-related ADEs without an associated frequency, were labelled as ‘Post-marketing’ or ‘Unknown’ as pertinent. In the absence of an AKI-related ADE reported for a selected drug, the ‘Not applicable’ label was assigned. All AKI-related ADE frequencies were then standardised to a category ranging from 1 (rare) to 5 (very frequent) in line with Galeano et al [42] and averaged (see Electronic Supplementary Material #1, Table 5).
2.4.1 NephroTox
The search for each selected drug on the number of published studies reporting on adverse kidney events was done and completed on January 19, 2024. The results served as a surrogate for the prevalence of AKI for a selected drug.
3 Results
3.1 Expert Consensus Lists of Drugs with AKI Potential
In total, 5935 studies were identified. After screening, four studies met our inclusion criteria (see Electronic Supplementary Material #1, Table 6 and Electronic Supplementary Material #1, Fig. 1) [16,17,18,19]. Stottlemyer et al [19] had the list with highest count of drugs with AKI potential (n = 195). In Table 2, the agreement class assigned (after comparing the lists from expert consensus studies) to each selected drug with AKI potential is shown. The limited agreement category had the highest proportion of drugs with AKI potential (131/200; 66%) and drugs not approved in the Netherlands (20/131; 15%). Conversely, drugs with AKI potential categorised with very strong or strong agreement levels, each represented 12% separately. The method to generate consensus between experts as well as the literature sources consulted to extract drugs with AKI potential varied across the included studies. In fact, only two included studies provided detailed information on the processes to reach consensus. Stottlemyer et al [19] deployed the Delphi method within a substantial group of experienced clinicians and pharmacists. Griffin et al [17] annually evaluated a list of drugs with AKI potential by the Nephrotoxic Injury Negated Just-in Time Action subcommittee.
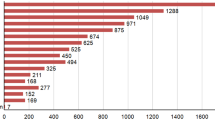
A total of 63 drugs with AKI potential was assigned moderate to very strong agreement after comparing the lists (see Electronic Supplementary Material #1, Table 7 and Electronic Supplementary Material #1, Fig. 2). These 63 drugs were selected for our subsequent analyses using SRS databases, DIDs and NephroTox. The most frequent pharmacological classes pertaining to the 63 drugs were: ‘antibacterials for systemic use’ (17.5%), ‘antivirals for systemic use’ (15.9%), and ‘anti-inflammatory and anti-rheumatic products, non-steroids – NSAIDs’ (11.1%) (see Fig. 2 and Electronic Supplementary Material #1, Table 8). Immunosuppressants, NSAIDs and antibacterials (pharmacological classes with more than one drug) show a high proportion of very strong agreement amongst experts for their AKI potential.
With respect to the suspected mechanism of AKI, the majority of drugs cause damage without dysfunction (n = 41; 65.1%) (see Table 3). Drugs displaying dysfunction without damage are in the minority (n = 9; 14.3%).
3.2 Disproportionality Analyses using SRS Databases
Between 2012 and 2022, there were a total of 2,973, 5,939 and 20,685 ICSRs in DAEN, CVAR and EV, respectively, where AKI-related PT was identified (see Electronic Supplementary Material #1, Tables 9–11). Acute kidney injury-related ICSRs tend to be more frequent amongst females and the median age is around 65 years across SRS databases. The most frequent PT descriptors from the AKI SMQ were: ‘acute kidney injury’, ‘renal failure’ and ‘blood creatinine increased’. Pre-processing steps and the whole suite of descriptive statistics for all and AKI-related ICSRs for each SRS (see Electronic Supplementary Material #1, Tables 9–11 and Tables 12–14).
When examining ROR signals (see Table 4 and Electronic Supplementary Material #2, Table 1), signals of variable strengths for AKI-related ADEs are observed across SRS databases for most drugs with AKI potential pertaining to antivirals, antibacterials, NSAIDs, immunosuppressants and diuretics. Notably, amongst renin-angiotensin aldosterone system (RAAS) acting agents and diuretics, strong signals are observed. Higher variability in ROR signals is noted across SRS databases for proton pump inhibitors (PPIs) (e.g., rabeprazole and pantoprazole).
3.3 Average AKI-related ADE Frequencies from DIDs
Across the four DIDs utilised, the PT descriptors ‘acute kidney injury’, ‘nephropathy toxic’ and ‘renal impairment’ were observed most frequently. In general, drugs in the antibacterial and antiviral pharmacological classes display the highest AKI-related ADE frequency, whereas PPIs fall at the lower end of the spectrum (see Table 4 and Electronic Supplementary Material #2, Table 1). High variability in average ADE frequencies is observed for NSAIDs. In Micromedex®, most drugs with AKI potential have frequent to very frequent average AKI-related ADEs. In contrast, Dutch DIDs (i.e., FK and IM) tend to display lower average AKI-related ADE frequencies (i.e., rare or very rare).
3.4 NephroTox
All 63 drugs have at least two published studies identified via the NephroTox in which kidney-related ADEs were reported. Antibacterials and antineoplastic agents have more than 250 such studies published, whereas drugs with AKI potential pertaining to the NSAIDs or RAAS inhibitors present a much greater variability.
3.5 Integration of Knowledge from the Four Sources
When bringing together the four sources of information into a single resource (see Table 4 and Electronic Supplementary Material #2, Table 1), specific patterns were identified. In general, drugs with AKI potential and very strong or strong agreement amongst experts lists exhibit moderate to strong ROR signals across SRS databases. Lower consistency is noted across DIDs, but it is common that at least one DID shows frequent or very frequent average AKI-related ADEs.
In the moderate agreement category, ROR signals across SRS databases show high variability. In fact, some drugs with AKI potential may exhibit weak or no association with AKI when analysing ROR signals. It is worth noting that drugs in the moderate agreement category show a higher prevalence of missing or unreported AKI-related ADE frequencies in DIDs compared to those that receive very strong or strong expert agreement. Reported average of AKI-related ADE frequencies in moderate category tend to be in the categories rare or very rare.
In NephroTox, the number of studies identified is lower in the moderate agreement category than in the very strong or strong agreement category.
3.6 Data Quality Considerations
With regard to data quality, all SRS databases support PT descriptors from MedDRA® standards. In contrast, amongst DIDs, only SIDER uses MedDRA® PT descriptors. In Micromedex®, IM and FK, (AKI-related) ADEs are documented in various text formats that require custom extraction techniques (i.e., web scraping or standardisation and direct manual extraction). In addition, international DIDs like SIDER and Micromedex® have a higher level of missing AKI-related ADE frequencies and missing drugs compared to Dutch DIDs. In fact, no AKI-related ADE frequency was reported by SIDER for 21 of the 63 drugs with AKI potential. Concerning the ICSRs used for disproportionality analysis, the availability of data elements differed across SRS databases. Canada Vigilance Adverse Reaction and DAEN required manual drug name standardisation to INNs. In addition, CVAR had the lowest number of ICSRs per drug.
4 Discussion
We hypothesised that a comprehensive and multi-source overview of drugs with AKI potential, which integrates expert consensus, SRS databases, DIDs, and NephroTox, would lead to the generation and characterisation of a robust list of drugs with AKI potential. Our approach involved a wide-ranging effort in the field of DAKI, tapping into knowledge sources like SRS databases, DIDs or NephroTox that had remained underutilised in previous investigations. Through our analysis of four expert consensus studies on drugs with AKI potential, we found moderate to very strong agreement for 63 drugs. Disproportionality analyses conducted on three SRS databases largely showed consistency for these 63 drugs, likely because healthcare professionals tend to report what they know. As expected, higher variability in ROR signals was observed for drugs with moderate agreement. Average AKI ADE frequencies from the analysed DIDs exhibit lower levels of consistency with medical experts compared to ROR signals, albeit different reporting patterns can be identified in moderate compared to strong or very strong expert agreement levels. This underscores the effectiveness of our novel approach, extending beyond conventional methodologies, and focussing on previously underexplored dimensions of drugs with AKI potential.
4.1 Expert Consensus Lists of Drugs with AKI Potential
The 63 drugs with AKI potential that have surfaced from the four expert consensus studies, represent a broad spectrum of therapeutic agents, with antibacterials, antivirals and NSAIDs emerging as the most frequent pharmacological drug classes. Indeed, there is ample evidence that drugs belonging to these classes may cause AKI [22, 23, 43], which has also been reflected in clinical practice guidelines [1]. On the other hand, we identified 131 drugs with limited agreement between the lists presented in the four expert consensus studies. This limited agreement may arise from various factors, including differences in the primary sources used, the composition and background of the expert panels, methods for achieving consensus, and the lack of a standardised definition for what constitutes a drug with AKI potential.
While consensus-reaching processes involving expert knowledge should always be grounded in a robust scientific evidence base [44], this may not always be the case in the field of DAKI. In fact, the current evidence base for AKI potential of many drugs is often found to be weak and biased [19]. Even for drugs such as vancomycin, which have long been considered as nephrotoxic, it has been noted that stronger evidence is still required judging from currently available evidence [45, 46]. Against this backdrop, novel methods, like the target-trial emulation framework, hold the promise to improve the design of observational studies to better ascertain the AKI potential of drugs [47]. This can help to address, amongst other biases, those caused by insufficient adjustment for confounding factors, such as concurrent use of other medications, drug-drug interactions, and underlying acute states like multi-organ failure.
The above may also explain why drugs such as glibenclamide, metoclopramide or metformin, which do not seem to exhibit AKI potential based on the current evidence [34, 35], appear inconsistently across expert consensus lists. Here, we suspect that the expert consensus studies may have conflated AKI risk and non-AKI side effects resulting from drug accumulation due to inadequate dosing adjustments for kidney function. In fact, if the dose of these drugs is not adjusted for reduced kidney function, they can result in various other non-AKI side effects [48]. Second, some drugs like integrase strand transfer inhibitors (e.g., dolutegravir [49]) or tyrosine kinase inhibitors [50] (e.g., imatinib or sorafenib) can elicit an increase in serum creatinine without causing kidney damage or dysfunction (i.e., also referred to as pseudo-AKI) [8]. Current evidence suggests that drugs like these may be blocking the uptake of serum creatinine from the blood without altering the glomerular filtration rate by inhibiting the drug efflux transporters, such as organic cation transporter 2 (OCT2) and multidrug or toxin extrusion (MATE) transporters 1 organic cation transporters [49, 50].
4.2 Disproportionality Analyses using SRS Databases
We note that strong associations with AKI found for antiviral drugs like aciclovir [24, 26, 51, 52], antibacterials like gentamicin [25, 51], vancomycin [24,25,26] and colistin [25] or NSAIDs such as diclofenac [24, 26, 51, 52] and ibuprofen [26, 51, 52] are aligned with other pharmacovigilance studies using the FDA Event Reporting system (FAERS) database [25, 26], the Japanese Adverse Drug Event Report (JADER) database [24] and the French National Pharmacovigilance Database (FPVD) [51]. Interestingly, in our analysis, RAAS inhibitors exhibit significant ROR signals in practically all cases, which indicate strong associations with AKI. However, RAAS inhibitors should be considered nephroprotective, as a decrease in eGFR caused by RAAS inhibitors is considered an acceptable haemodynamic change and a sign that these drugs are ‘doing their job’ rather than a sign of AKI in the absence of severe bilateral renal artery stenosis, volume depletion or administration with a possible pharmacodynamic drug-drug interaction (i.e., triple whammy) [8]. This is similar for diuretics, which are not considered to cause AKI, and only become a concern when used excessively, leading to sustained volume depletion or contribute to a pharmacodynamic interaction. In fact, prudent use of diuretics to prevent volume overload has been associated with improvements in the kidney function [39].
Furthermore, we identified drug classes with high variability in ROR signals like PPIs. Indeed, PPIs are currently subject of discussions [21, 53], as their safety profile was recently challenged by epidemiological and histological studies [21, 53, 54]. In its turn, and as a limitation of disproportionality analyses, this could have led to ADE-stimulated reporting or masking effect and potentially end up biasing the signals. Thus, as a general remark, disproportionality studies should only be used for hypothesis generation and further causality studies are warranted to ascertain a relationship with AKI [39].
It should also be noted that in the disproportionality analyses we have discarded ICSRs associated with AKI containing more than one INN, which may be clinically relevant, thus leaving this exploration for future work. In addition, some signals in CVAR were not reportable due to low number of ICSRs, but these can be complemented with the signals present in the other SRS databases analysed.
4.3 Average AKI-related ADE Frequencies from DIDs
The higher variability in AKI-related ADE frequencies observed in DIDs compared to disproportionality analyses signals may be influenced by differences in content refresh rates. Drug information databases tend to be updated at longer time intervals in contrast to disproportionality signals, which can be tracked virtually continuously. This emphasises the need to consider the temporal aspect and diverse data sources when assessing the AKI potential of a drug [55, 56]. Consulting multiple information sources which adds value to our resource. The case of NSAIDs is of particular interest, as strong associations with AKI observed in most disproportionality analyses are not mirrored in DIDs. We speculate that this may be reflective of the low prevalence of NSAID-induced serious AKI events (estimated to be between 1 to 5%) [57], possibly due to the prescribers’ awareness of their AKI potential for patients at risk for AKI. As for the variability in AKI-related ADE frequencies observed between DIDs, the differences in the type of evidence considered and the critical appraisal of evidence may provide an explanation. Drug information databases do not account for specific populations and therefore they could provide wide ADE ranges. We have carried out manual mappings for the DIDs, which did not support MedDRA® terminology. Whilst we have provided a detailed account of this process, it is indeed an ongoing area for improvement.
4.4 NephroTox
By employing NephroTox, we found that most drugs with AKI potential are consistently present in published studies where adverse kidney events are reported. Following the method of Welch et al [26] to identify drugs with AKI potential, the drugs under investigation in this study are ‘known’ for their association with AKI potential.
4.5 Integration of Knowledge from the Four Sources
We envisage our resource as a tool to be used for aiding AKI potential assessment when developing expert consensus lists of drugs with AKI potential and also as decision support when prescribing drugs in routine care. In this respect, we have encountered a number of cases where our resource may have changed the opinion of the experts, had our resource been available to them at that time. For example, our resource shows that amoxicillin and beta-lactamase inhibitor (i.e., clavulanic acid) displays moderate agreement, but no AKI signal is detected using any of the three SRS databases and ADE frequencies in the DIDs included tend to be very low. Given this pattern, the inclusion of amoxicillin and beta-lactamase inhibitor on the list of drugs with AKI potential is up for discussion. Potentially, this could also be said for drugs like ioversol or sulfasalazine.
Finally, we acknowledge that the AKI potential of drugs may be confounded by multiple factors (e.g., polypharmacy patterns) that may obscure the underlying biological process. Therefore, formal causality assessments are needed to assess whether AKI was indeed caused by a drug [12]. Thus, our resource serves as a starting point to signal potential associations between drugs and AKI and prompts further studies on specific areas, rather than being a conclusive endpoint.
From a practical standpoint, successful attempts have been made to automate knowledge-based generation for identifying ADEs [58]. However, the automation of knowledge retrieval from the knowledge sources leveraged in this study may be challenging at different stages in the analysis pipeline due to difficulties in data extraction or parsing processes. For instance, access to EV ICSRs data is layered and drug name standardisation is required for DAEN or CVAR databases. In addition, some DIDs do not support MedDRA® terminology (i.e., FK, IM, Micromedex®) or display high data missingness (i.e., SIDER). The latter DID does not entail curation by medical experts as is the case for the other DIDs. Therefore, continued improvements in data collection policies and terminology standardisation are needed to ensure compliance with findability, accessibility, interoperability and reusability (FAIR) principles, which enable progress in research. Whilst automating the integration of sources remains unfeasible at present, it is imperative to closely monitor the accrual of evidence for drugs whose AKI potential remains uncertain.
4.6 Strengths and Limitations
This study has several strengths. First, the integration of diverse and disjointed, often underexplored, knowledge sources has facilitated a comprehensive investigation on drugs with AKI potential from different angles. Second, by combining pharmacovigilance data from different regulatory agencies and DIDs across multiple countries, our resource provides a thorough overview of 63 drugs with AKI potential. Third, besides Dutch information sources, we have also included Micromedex® as a globally recognised DID and assessed diverse SRS databases like EV, CVAR and DAEN. This, coupled with broad alignment with previous studies, strengthens the generalisability of our findings and helps to reveal areas that require further investigation. Our resource and its scope are relevant to capitalise on the strengths each knowledge source has to offer and mitigate their limitations, as highlighted in the literature [59].
Our study also has several limitations. Starting with our literature search, we only searched the Medline database and focussed on drugs approved in the Netherlands. However, we identified a sufficient number of high-quality, peer-reviewed studies, which allowed us to allocate more time to other information sources included in this study. The 63 drugs included in this study are also common in other countries [16,17,18,19]. Second, we have used as input existing expert consensus lists of drugs with AKI potential, which may have led to the omission of some drugs with known AKI potential. One such example worth mentioning here may be antitumour drugs like azacytidine, streptozocin, high-dose pemetrexed and pentostatin, which exhibit AKI potential based on current evidence [34,35,36]. Presumably, these drugs may have been overlooked in the process of gathering expert consensus in the included studies. Furthermore, by taking existing expert consensus lists of drugs with AKI potential as a starting point, our resource may be less likely to include new therapeutic agents with AKI potential. In addition, both disproportionality analyses and DIDs necessitate extended periods of time to accumulate sufficient data in order to prevent temporal biases [39, 60] and ultimately provide robust estimates. This illustrates the importance of conducting this type of exercise periodically, whilst recognising that domain knowledge retrieval automation may not always be suitable for new therapeutic agents. Fourth, in relation to disproportionality analyses, we have included all ICSRs, as information on formal causality assessment [61] was not available in the SRS databases used. It is important to note that disproportionality analyses only provide an indication about the reporting rate of an ADE and do not necessarily carry a causal consideration, so the signals found are merely associational and cannot be used as evidence for a causal relationship. Fifth, all knowledge sources have been pulled together into a single resource giving the appearance of being on an equal footing. Indeed, the number of studies identified via NephroTox may not be as relevant for assessing AKI potential as ADEs frequencies from DIDs or disproportionality analyses, because it is an aggregated statistic that does not consider the quality of evidence in the studies found. To remediate this, we have provided contextualisation and emphasised the most salient features of the resource components.
4.7 Future Research
We consider our resource as a stepping stone to consolidating a list of drugs with AKI potential. Thus, the characterisation of the 131 agents labelled as having limited agreement in our study using SRS databases, DIDs and NephroTox (as we did for the 63 drugs labelled as having at least moderate agreement), is left for future research. Indeed, sufficient data accrual and mechanistic considerations based on existing evidence should also play a role in the prioritisation for analysis of each of these drugs. With regard to antitumour drugs with AKI potential that we have not assessed in this study (e.g., azacytidine, high-dose pemetrexed, pentostatin, streptozocin), a potentially interesting approach to tackle this issue could be following the reverse process, that is, starting by mining information about AKI potential of drugs in the empirical data sources (like those we propose in our study) and involving experts to discuss the existing evidence at the end.
5 Conclusion
In conclusion, in this study, we have classed drugs with AKI potential according to expert consensus in the literature, resulting in a list of 63 drugs. We have enriched this with data mining algorithms, extracting insights from previously underexplored sources including three SRS databases, four DIDs and the NephroTox website. Through the integration of disparate knowledge sources, we have generated an exhaustive knowledge base on current understanding of AKI potential of drugs. Our resource highlights that AKI potential should be understood as a gradation which benefits from contextualising it using both expert-based knowledge and quantitative analyses from clinical and post-marketing settings. Embedded in the context of kidney safety improvement efforts, this paper is a step forward in advancing our understanding of DAKI, aid prescription practices and raises awareness of the ubiquity of drugs that might cause AKI.
References
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2(1).
Cerdá J, et al. The contrasting characteristics of acute kidney injury in developed and developing countries. Nat Clin Pract Nephrol. 2008;4(3):138–53. https://doi.org/10.1038/ncpneph0722.
Hoste EAJ, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41(8):1411–23. https://doi.org/10.1007/s00134-015-3934-7.
Susantitaphong P, et al. World incidence of AKI: a meta-analysis. Clin J Am Soc Nephrol. 2013;8(9):1482–93. https://doi.org/10.2215/CJN.00710113.
Coca SG, et al. Long-term risk of mortality and other adverse outcomes after acute kidney injury: a systematic review and meta-analysis. Am J Kidney Dis. 2009;53(6):961–73. https://doi.org/10.1053/j.ajkd.2008.11.034.
Fischer MJ, et al. Uncomplicated acute renal failure and hospital resource utilization: a retrospective multicenter analysis. Am J Kidney Dis. 2005;46(6):1049–57. https://doi.org/10.1053/j.ajkd.2005.09.006.
Mehta RL, et al. Recognition and management of acute kidney injury in the International Society of Nephrology 0by25 Global Snapshot: a multinational cross-sectional study. Lancet. 2016;387(10032):2017–25. https://doi.org/10.1016/S0140-6736(16)30240-9.
Karimzadeh I, et al. Moving toward a contemporary classification of drug-induced kidney disease. Crit Care. 2023;27(1):435. https://doi.org/10.1186/s13054-023-04720-2.
Kane-Gill SL. Nephrotoxin stewardship. Crit Care Clin. 2021;37(2):303–20. https://doi.org/10.1016/j.ccc.2020.11.002.
Awdishu L, Mehta RL. The 6R’s of drug induced nephrotoxicity. BMC Nephrol. 2017;18(1):124. https://doi.org/10.1186/s12882-017-0536-3.
Hoste EAJ, et al. Global epidemiology and outcomes of acute kidney injury. Nat Rev Nephrol. 2018;14(10):607–25. https://doi.org/10.1038/s41581-018-0052-0.
Yousif ZK, et al. Clinical characteristics and outcomes of drug-induced acute kidney injury cases. Kidney Int Rep. 2023;8(11):2333–44. https://doi.org/10.1016/j.ekir.2023.07.037.
Irvine AR, et al. A systematic review of in vitro models of drug-induced kidney injury. Curr Opin Toxicol. 2021;27:18–26. https://doi.org/10.1016/j.cotox.2021.06.001.
Ostermann M, et al. Recommendations on acute kidney injury biomarkers from the acute disease quality initiative consensus conference: a consensus statement. JAMA Netw Open. 2020;3(10): e2019209. https://doi.org/10.1001/jamanetworkopen.2020.19209.
Vaara ST, et al. Subphenotypes in acute kidney injury: a narrative review. Crit Care. 2022;26(1):251. https://doi.org/10.1186/s13054-022-04121-x.
Arias Pou P, et al. Improvement of drug prescribing in acute kidney injury with a nephrotoxic drug alert system. Eur J Hosp Pharm. 2019;26(1):33–8. https://doi.org/10.1136/ejhpharm-2017-001300.
Griffin BR, et al. Nephrotoxin exposure and acute kidney injury in adults. Clin J Am Soc Nephrol. 2023;18(2):163–72. https://doi.org/10.2215/CJN.0000000000000044.
Schreier DJ, et al. Nephrotoxin exposure in the 3 years following hospital discharge predicts development or worsening of chronic kidney disease among acute kidney injury survivors. Am J Nephrol. 2022;53(4):273–81. https://doi.org/10.1159/000522139.
Stottlemyer BA, et al. Expert consensus on the nephrotoxic potential of 195 medications in the non-intensive care setting: a modified Delphi method. Drug Saf. 2023;46(7):677–87. https://doi.org/10.1007/s40264-023-01312-5.
Yasrebidekom IAR, et al. Acute kidney injury associated with nephrotoxic drugs in critically ill patients: a multicenter cohort study using electronic health record data. Clin Kidney J. 2023;16(12):2549–58. https://doi.org/10.1093/ckj/sfad160.
Zhang Y, et al. The association between proton pump inhibitor use and risk of post-hospitalization acute kidney injury: a multicenter prospective matched cohort study. BMC Nephrol. 2023;24(1):150. https://doi.org/10.1186/s12882-023-03211-4.
Campbell RE, Chen CH, Edelstein CL. Overview of antibiotic-induced nephrotoxicity. Kidney Int Rep. 2023;8(11):2211–25. https://doi.org/10.1016/j.ekir.2023.08.031.
Klomjit N, Ungprasert P. Acute kidney injury associated with non-steroidal anti-inflammatory drugs. Eur J Intern Med. 2022;101:21–8. https://doi.org/10.1016/j.ejim.2022.05.003.
Hosohata K, et al. Surveillance of drugs that most frequently induce acute kidney injury: a pharmacovigilance approach. J Clin Pharm Ther. 2019;44(1):49–53. https://doi.org/10.1111/jcpt.12748.
Patek TM, et al. Comparing acute kidney injury reports among antibiotics: a pharmacovigilance study of the FDA adverse event reporting system (FAERS). Drug Saf. 2020;43(1):17–22. https://doi.org/10.1007/s40264-019-00873-8.
Welch HK, Kellum JA, Kane-Gill SL. Drug-associated acute kidney injury identified in the United States food and drug administration adverse event reporting system database. Pharmacotherapy. 2018;38(8):785–93. https://doi.org/10.1002/phar.2152.
Wu B, et al. Proton pump inhibitors associated acute kidney injury and chronic kidney disease: data mining of US FDA adverse event reporting system. Sci Rep. 2021;11(1):3690. https://doi.org/10.1038/s41598-021-83099-y.
Malec SA, Boyce RD. Exploring novel computable knowledge in structured drug product labels. AMIA Jt Summits Transl Sci Proc. 2020;2020:403–12.
Emanuel R, et al. Evolving roles of spontaneous reporting systems to assess and monitor drug safety. In: Charmy SK, Manan S, Rajvi Manthan P, editors. Pharmacovigilance. Rijeka: IntechOpen; 2018. p. Ch. 2.
EudraVigilance—European database of suspected adverse drug reaction reports. https://www.adrreports.eu/en/index.html. Accessed 15 Dec 2023.
Database of Adverse Event Notifications (DAEN)—medicines. https://daen.tga.gov.au/medicines-search/. Accessed 5 Dec 2023.
Canada Vigilance adverse reaction online database. https://www.canada.ca/en/health-canada/services/drugs-health-products/medeffect-canada/adverse-reaction-database.html. Accessed 19 May 2023.
Kuhn M, et al. The SIDER database of drugs and side effects. Nucleic Acids Res. 2016;44(D1):D1075–9. https://doi.org/10.1093/nar/gkv1075.
Medication Safety. Adverse Effects. In: MicroMedex [Electronic version]. Greenwood Village: Truven Health Analytics; 2024. http://www.micromedexsolutions.com/.
KNMP Kennisbank. 2024. https://kennisbank.knmp.nl/. Accessed 1 July 2024.
Farmacotherapeutisch Kompas. 2024. https://www.farmacotherapeutischkompas.nl. Accessed 1 July 2024.
NephroTox. Data base for chemicals, drugs, poisons and other related medical interventions. 2022. http://www.nephrotox.com/. Accessed 1 July 2024.
McCullough PA, et al. Diagnosis of acute kidney injury using functional and injury biomarkers: workgroup statements from the tenth acute dialysis quality initiative consensus conference. In: Kellum JA, et al., editors. ADQI consensus on AKI biomarkers and cardiorenal syndromes. S.Karger AG; 2013. https://doi.org/10.1159/000349963.
Faillie JL. Case-non-case studies: principle, methods, bias and interpretation. Therapie. 2019;74(2):225–32. https://doi.org/10.1016/j.therap.2019.01.006.
Inspections, Human Medicines, Pharmacovigilance and Committees Division, Screening for adverse reactions in EudraVigilance. 2016.
List of medicines under additional monitoring. 2024. https://www.ema.europa.eu/en/human-regulatory-overview/post-authorisation/pharmacovigilance-post-authorisation/medicines-under-additional-monitoring/list-medicines-under-additional-monitoring. Accessed 20 Feb 2024.
Galeano D, Paccanaro A. Machine learning prediction of side effects for drugs in clinical trials. Cell Rep Methods. 2022;2(12): 100358. https://doi.org/10.1016/j.crmeth.2022.100358.
Izzedine H, Launay-Vacher V, Deray G. Antiviral drug-induced nephrotoxicity. Am J Kidney Dis. 2005;45(5):804–17. https://doi.org/10.1053/j.ajkd.2005.02.010.
Djulbegovic B, Guyatt G. Evidence vs consensus in clinical practice guidelines. JAMA. 2019;322(8):725–6. https://doi.org/10.1001/jama.2019.9751.
Mullaney SR. Vancomycin should be considered a nephrotoxic antimicrobial agent: CON. Kidney360. 2022;3(9):1488–90. https://doi.org/10.34067/KID.0007932021.
Murphy ME, Barreto EF. Vancomycin should be considered a nephrotoxic antimicrobial agent: PRO. Kidney360. 2022;3(9):1484–7. https://doi.org/10.34067/KID.0008032021.
Fu EL. Target trial emulation to improve causal inference from observational data: what, why, and how? J Am Soc Nephrol. 2023;34(8):1305–14. https://doi.org/10.1681/ASN.0000000000000152.
Munar MY, Singh H. Drug dosing adjustments in patients with chronic kidney disease. Am Fam Physician. 2007;75(10):1487–96.
Koteff J, et al. A phase 1 study to evaluate the effect of dolutegravir on renal function via measurement of iohexol and para-aminohippurate clearance in healthy subjects. Br J Clin Pharmacol. 2013;75(4):990–6. https://doi.org/10.1111/j.1365-2125.2012.04440.x.
Omote S, et al. Effect of tyrosine kinase inhibitors on renal handling of creatinine by MATE1. Sci Rep. 2018;8(1):9237. https://doi.org/10.1038/s41598-018-27672-y.
Pierson-Marchandise M, et al. The drugs that mostly frequently induce acute kidney injury: a case–noncase study of a pharmacovigilance database. Br J Clin Pharmacol. 2017;83(6):1341–9. https://doi.org/10.1111/bcp.13216.
Roughead EE, et al. Medicine-induced acute kidney injury findings from spontaneous reporting systems, sequence symmetry analysis and a case-control study with a focus on medicines used in primary care. Drug Saf. 2022;45(11):1413–21. https://doi.org/10.1007/s40264-022-01238-4.
Al-Aly Z, Maddukuri G, Xie Y. Proton pump inhibitors and the kidney: implications of current evidence for clinical practice and when and how to deprescribe. Am J Kidney Dis. 2020;75(4):497–507. https://doi.org/10.1053/j.ajkd.2019.07.012.
Muriithi AK, et al. Biopsy-proven acute interstitial nephritis, 1993–2011: a case series. Am J Kidney Dis. 2014;64(4):558–66. https://doi.org/10.1053/j.ajkd.2014.04.027.
Clauson KA, et al. Clinical decision support tools: analysis of online drug information databases. BMC Med Inform Decis Mak. 2007;7:7. https://doi.org/10.1186/1472-6947-7-7.
McConachie SM, et al. Evaluation of adverse drug reaction formatting in drug information databases. J Med Libr Assoc. 2020;108(4):598–604. https://doi.org/10.5195/jmla.2020.983.
Whelton A, Hamilton CW. Nonsteroidal anti-inflammatory drugs: effects on kidney function. J Clin Pharmacol. 1991;31(7):588–98. https://doi.org/10.1002/j.1552-4604.1991.tb03743.x.
Voss EA, et al. Accuracy of an automated knowledge base for identifying drug adverse reactions. J Biomed Inform. 2017;66:72–81. https://doi.org/10.1016/j.jbi.2016.12.005.
Fusaroli M, et al. Mapping strategies to assess and increase the validity of published disproportionality signals: a meta-research study. Drug Saf. 2023;46(9):857–66. https://doi.org/10.1007/s40264-023-01329-w.
Mountford CM, et al. Quality and usability of common drug information databases. Can J Hosp Pharm. 2010;63(2):130–7. https://doi.org/10.4212/cjhp.v63i2.898.
Behera SK, et al. Comparison of different methods for causality assessment of adverse drug reactions. Int J Clin Pharm. 2018;40(4):903–10. https://doi.org/10.1007/s11096-018-0694-9.
Acknowledgements
LEAPfROG consortium: The LEAPfROG consortium which aims to leverage real-world data, machine learning and knowledge representation methods to improve pharmacotherapy outcomes in patients with multi-morbidity, is a unique cross-sectional collaboration between patients, healthcare professionals, epidemiologists, medical informatics and computer science researchers, as well as partners from medical technology industry, regulatory bodies and healthcare insurance. It aims to develop data-driven computerized decisions support tools to support clinicians in data quality improvement, drug side-effects detection, and causal inference using data from electronic health records. The project focuses on clinically relevant use case of drug-induced kidney disease in people with chronic kidney disease. Principal investigator: Dr. Joanna E. Klopotowska. Work package (WP) leaders: Dr. Ronald Cornet (WP1), Prof. Dr. Annette ten Teije (WP2), Dr. Giovanni Cinà (WP3), Dr. Stephanie Medlock (WP4). Beneficiaries of the LEAPfROG consortium: Amsterdam University Medical Center, leadership and coordination; Vrije Universiteit Amsterdam, and Open University Heerlen.Ongoing LEAPfROG PhDs: Daniel Fernández-Llaneza, Romy M. P. Vos, Joris E. Lieverse. We would also like to thank the EMA for granting us Level 2A access for academia, as established in the EudraVigilance access policy. The LEAPfROG Consortium members include: The LEAPfROG Consortium has the following members in addition to all co-authors: Ameen Abu-Hanna (Amsterdam University Medical Center), Annemiek Dorgelo (Dutch Kidney Foundation/Nierstichting), Annette ten Teije (Vrije Universiteit Amsterdam), Birgit A. Damoiseaux (Amsterdam University Medical Center), Cornelis Boersma (Open Universiteit), Dave A. Dongelmans (Nationale Intensive Care Evaluatie foundation), David H. de Koning (Amsterdam University Medical Center), Erol S. Hofmans (College ter Beoordeling van Geneesmiddelen), Evelien Tiggelaar (Z-Index), Frank van Harmelen (Vrije Universiteit Amsterdam), Giovanni Cinà (Amsterdam University Medical Center), Gerty Holla (Amsterdam Economic Board), Hilda J. de Jong (PHARMO Institute for Drug Outcomes Research), Iacopo Vagliano (Amsterdam University Medical Center), Jan Pander (AstraZeneca), Jasper M. Boomker (Dutch Kidney Foundation/Nierstichting), Jurjen van der Schans (Open Universiteit), Kitty J. Jager (Amsterdam University Medical Center, European Renal Association-European Dialysis and Transplantation Association [ERA-EDTA] Registry), Linda Dusseljee-Peute (Amsterdam University Medical Center), Luuk B. Hilbrands (Radboud University Medical Centre), Marianne le Comte (Koninklijke Nederlandse Matschappij ter bevordering der Pharmacie [KNMP] Geneesmiddelen Informatie Centrum), Marieke A. R. Bak (Amsterdam University Medical Center), Mariette van den Hoven (Amsterdam University Medical Center), Martijn G. Kersloot (Castor), Menno Maris (Amsterdam University Medical Center), Nicolette F. de Keizer (Amsterdam University Medical Center), Otto R. Maarsingh (Amsterdam University Medical Center), Paul Blank (NWO), Piet Heingraaf (Pitts.AI), Ron Herings (Amsterdam University Medical Center), Ron J. Keizer (InsightRX), Ronald Cornet (Amsterdam University Medical Center), Ruben Boyd (IXA), Sebastiaan L. Knijnenburg (Castor), Sipke Visser (Digital Health Link), Stephanie Medlock (Amsterdam University Medical Center), Tjerk S. Heijmens Visser (CZ health insurance, Zorgverzekeraars Nederland), Vianda S. Stel (Amsterdam University Medical Center, ERA-EDTA Registry), Wanda Konijn (Nierpatiënten Vereniging Nederland).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
This study is part of a larger project called LEveraging real-world dAta to optimize PharmacotheRapy outcomes in multimOrbid patients by using machine learning and knowledGe representation methods (LEAPfROG project) funded by the Nederlandse Organisatie voor Wetenschappelijk Onderzoek (NWO; Dutch Research Council) under grant agreement KICH1.ST01.20.011 and co-funded in-cash by Dutch Kidney Foundation and National Intensive Care Evaluation (NICE) foundation, and in-kind by PHARMO Institute for Drug Outcomes Research, Castor, InsightRX, Z-Index, Digital Health Link. The funders had no role in the design of the study, the collection, analysis and interpretation of the data, or in writing the manuscript.
Conflict of interest
Daniel Fernández-Llaneza is a former employee of AstraZeneca and terminated his contract in February 2023. In the last 3 years, Dr. T.vG. has received lecture fees and consulting fees from Roche Diagnostics, Thermo Fisher, Vitaeris, Otsuka, CSL Behring, Astellas and Aurinia Pharma. In all cases money has been transferred to hospital accounts, and none has been paid to his personal bank accounts. Dr. T.vG. does not have employment or stock ownership at any of these companies, and neither does he have patents or patent applications. Dr. S.L.K-G. receives grant funding from the National Institute of Diabetes and Digestive and Kidney Diseases R01DK121730 and U01DK130010, the National Center for Complementary and Integrative Health U54AT008909 and the Jewish Healthcare Foundation. All other authors declared no competing interests for this work.
Availability of data and material
Some of the data supporting the findings of this study are not publicly available. Access to EV data is restricted based on conditions for access specified in EMA’s access policy (https://www.adrreports.eu/en/access_policy.html). Micromedex® and Informatorium Medicamentorum data was accessed through the hospital’s licence. All publications, DAEN and CVAR SRS databases data and SIDER and FK data are freely and publicly accessible.
Ethics approval
This study is part of a larger project called LEveraging real-world dAta to optimize PharmacotheRapy outcomes in multimOrbid patients by using machine learning and knowledGe representation methods (LEAPfROG project).The LEAPfROG project was exempted from requiring ethics approval (waiver W22_340 # 22.412) on September 2022, 22 by the Medical Ethics Committee of the Amsterdam University Medical Centre, University of Amsterdam, Amsterdam, The Netherlands, as it did not fall within the scope of the Dutch Medical Research Involving Human Subjects Act. The anonymised ICSR data elements of DAEN and CVAR are available as an online open source. In order to get an extended subset of ICSR data elements from EV (level 2A), a research request and a signed copy of a confidentiality undertaking were submitted to the EMA. These were then presented to the EV research committee, which granted access to the data. This does not affect the rights to publish the results.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Code is available upon reasonable request to the authors.
Author contributions (CRediT taxonomy)
Daniel Fernández-Llaneza: Conceptualisation, Methodology, Software, Validation, Formal analysis, Investigation, Data Curation; Writing—original draft, Visualisation; Romy M. P Vos: Conceptualisation, Methodology, Software, Validation, Formal analysis, Investigation, Data Curation; Writing—original draft, Visualisation; Joris E. Lieverse: Conceptualisation, Methodology, Validation, Formal analysis, Investigation, Data Curation; Writing – original draft, Visualisation; Helen R. Gosselt, Sandra L. Kane-Gill, Teun van Gelder: Methodology; Validation; Writing—review and editing; Joanna E. Klopotowska: Conceptualisation; Data Curation; Formal Analysis; Funding Acquisition; Methodology; Project Administration; Validation; Writing—review and editing. All authors and LEAPfROG consortium members gave final approval of the submitted version.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Fernández-Llaneza, D., Vos, R.M.P., Lieverse, J.E. et al. An Integrated Approach for Representing Knowledge on the Potential of Drugs to Cause Acute Kidney Injury. Drug Saf (2024). https://doi.org/10.1007/s40264-024-01474-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s40264-024-01474-w