Abstract
Introduction
The use of dipeptidyl peptidase-4 (DPP-4) inhibitors may be associated with an increased risk of gallbladder and bile duct disease among patients with type 2 diabetes.
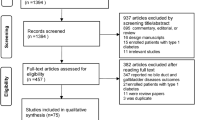
Methods
We conducted a population-based cohort study using an active comparator, new-user design. We used data from the United Kingdom Clinical Practice Research Datalink to identify patients newly treated with either a DPP-4 inhibitor or sodium-glucose cotransporter-2 (SGLT-2) inhibitor between January 2013 and December 2020. We fitted Cox proportional hazards models with propensity score fine stratification weighting to estimate the hazard ratio (HR) and its 95% confidence interval (CI) for incident gallbladder and bile duct disease associated with DPP-4 inhibitors compared to SGLT-2 inhibitors.
Results
DPP-4 inhibitors were associated with a 46% increased risk of gallbladder and bile duct disease (4.3 vs. 3.0 events per 1000 person-years, HR 1.46, 95% CI 1.17–1.83). At 6 months and 1 year, 745 and 948 patients, respectively, would need to be treated with DPP-4 inhibitors for one patient to experience a gallbladder or bile duct disease.
Conclusions
In this population-based cohort study, the use of DPP-4 inhibitors, when compared with SGLT-2 inhibitors, was associated with a moderately increased risk of gallbladder and bile duct disease among patients with type 2 diabetes. This outcome was still quite rare with a high number needed to harm at 6 months and 1 year.



Similar content being viewed by others
References
National Institute for Health and Care Excellence. Guideline: type 2 diabetes in adults: management. London: National Institute for Health And Care Excellence (Nice). Copyright National Institute For Health And Care Excellence; 2015.
American Diabetes Association. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes—2020. Diabetes Care. 2020;43(Supplement 1):S98–110.
Moran G, Bakhai C, Song S, Agwu J. Type 2 diabetes: summary of updated nice guidance. BMJ Br Med J. 2022. https://doi.org/10.1136/bmj.o775.
Bonora B, Avogaro A, Fadini G. Extraglycemic effects of Sglt2 inhibitors: a review of the evidence. Diabet Metab Syndr Obes. 2020;13:161–74.
Filippatos T, Panagiotopoulou T, Elisaf M. Adverse effects of Glp-1 receptor agonists. Rev Diabet Stud. 2014;11(3–4):202–30.
Lin Y, Wang T-H, Tsai M-L, Wu V-C, Tseng C-J, Lin M-S, et al. The cardiovascular and renal effects of glucagon-like peptide 1 receptor agonists in patients with advanced diabetic kidney disease. Cardiovasc Diabetol. 2023. https://doi.org/10.1186/s12933-023-01793-9.
Zhao X, Wang M, Wen Z, Lu Z, Cui L, Fu C, et al. Glp-1 receptor agonists: beyond their pancreatic effects. Front Endocrinol (Lausanne). 2021. https://doi.org/10.3389/fendo.2021.721135.
Faillie J, Yu O, Yin H, Hillaire-Buys D, Barkun A, Azoulay L. Association of bile duct and gallbladder diseases with the use of incretin-based drugs in patients with type 2 diabetes mellitus. JAMA Intern Med. 2016;176(10):1474–81.
He L, Wang J, Ping F, Yang N, Huang J, Li Y, et al. Association of glucagon-like peptide-1 receptor agonist use with risk of gallbladder and biliary diseases: a systematic review and meta-analysis of randomized clinical trials. JAMA Intern Med. 2022;182(5):513–9.
Nauck M, Muus Ghorbani M, Kreiner E, Saevereid H, Buse J. Effects of liraglutide compared with placebo on events of acute gallbladder or biliary disease in patients with type 2 diabetes at high risk for cardiovascular events in the leader randomized trial. Diabetes Care. 2019;42(10):1912–20.
Keller J, Trautmann M, Haber H, Tham L, Hunt T, Mace K, et al. Effect of exenatide on cholecystokinin-induced gallbladder emptying in fasting healthy subjects. Regul Pept. 2012;179(1–3):77–83.
He L, Wang J, Li Z, Li Y, Zhang H. Dipeptidyl peptidase 4 inhibitors and gallbladder or biliary diseases: data from the U.S. Food and Drug Administration adverse event reporting system. Diabetes Care. 2022;46(2):E72–3.
Moses R, Round E, Shentu Y, Golm G, Oneill EA, Gantz I, et al. A randomized clinical trial evaluating the safety and efficacy of sitagliptin added to the combination of sulfonylurea and metformin in patients with type 2 diabetes mellitus and inadequate glycemic control. J Diabetes. 2016;8(5):701–11.
Rosenstock J, Kahn S, Johansen O, Zinman B, Espeland M, Woerle H, et al. Effect of linagliptin vs glimepiride on major adverse cardiovascular outcomes in patients with type 2 diabetes: the Carolina randomized clinical trial. JAMA. 2019;322(12):1155–66.
Rosenstock J, Perkovic V, Johansen O, Cooper M, Kahn S, Marx N, et al. Effect of linagliptin vs placebo on major cardiovascular events in adults with type 2 diabetes and high cardiovascular and renal risk: the Carmelina randomized clinical trial. JAMA. 2019;321(1):69–79.
Scirica B, Bhatt D, Braunwald E, Steg P, Davidson J, Hirshberg B, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369(14):1317–26.
He L, Wang J, Ping F, Yang N, Huang J, Li W, et al. Dipeptidyl peptidase-4 inhibitors and gallbladder or biliary disease in type 2 diabetes: systematic review and pairwise and network meta-analysis of randomised controlled trials. BMJ. 2022;377:E068882.
Herrett E, Gallagher A, Bhaskaran K, Forbes H, Mathur R, Van Staa T, et al. Data resource profile: clinical practice research datalink (CPRD). Int J Epidemiol. 2015;44(3):827–36.
Wolf A, Dedman D, Campbell J, Booth H, Lunn D, Chapman J, et al. Data resource profile: clinical practice research datalink (CPRD) aurum. Int J Epidemiol. 2019;48(6):1740.
Herrett E, Thomas S, Schoonen W, Smeeth L, Hall A. Validation and validity of diagnoses in the general practice research database: a systematic review. Br J Clin Pharmacol. 2010;69(1):4–14.
Nf K, Se H, Pw R. Validity of diagnostic coding within the general practice research database: a systematic review. Br J Gen Pract. 2010;60(572):E128–36.
Jick H, Jick S, Derby L. Validation of information recorded on general practitioner based computerised data resource in the United Kingdom. Br Med J. 1991;302(6779):766–8.
Herbert A, Wijlaars L, Zylbersztejn A, Cromwell D, Hardelid P. Data resource profile: hospital episode statistics admitted patient care (HES APC). Int J Epidemiol. 2017;46(4):1093.
National Health Service. Hospital episode statistics (HES). Available from https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics.
Office for National Statistics. Deaths. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths.
Wexler D. Management of persistent hyperglycemia in type 2 diabetes mellitus. In: Nathan D, Mulder J, editors. Up to date. Waltham, MA: Up to date; 2021.
Wilkinson S, Douglas I, Stirnadel-Farrant H, Fogarty D, Pokrajac A, Smeeth L, et al. Changing use of antidiabetic drugs in the UK: trends in prescribing 2000–2017. BMJ Open. 2018;8(7):E022768.
Desai RJ, Franklin JM. Alternative approaches for confounding adjustment in observational studies using weighting based on the propensity score: a primer for practitioners. BMJ. 2019;367:L5657.
White I, Royston P. Imputing missing covariate values for the Cox model. Stat Med. 2009;28(15):1982–98.
Pizzimenti V, Giandalia A, Cucinotta D, Russo G, Smits M, Cutroneo P, et al. Incretin-based therapy and acute cholecystitis: a review of case reports and eudravigilance spontaneous adverse drug reaction reporting database. J Clin Pharm Ther. 2016;41(2):116–8.
Woronow D, Chamberlain C, Niak A, Avigan M, Houstoun M, Kortepeter C. Acute cholecystitis associated with the use of glucagon-like peptide-1 receptor agonists reported to the US Food And Drug Administration. JAMA Intern Med. 2022;182(10):1104–6.
Erlinger S. Gallstones in obesity and weight loss. Eur J Gastroenterol Hepatol. 2000;12(12):1347–52.
Pi-Sunyer X, Astrup A, Fujioka K, Greenway F, Halpern A, Krempf M, et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N Engl J Med. 2015;373(1):11–22.
Gallwitz B. Clinical use of Dpp-4 inhibitors. Front Endocrinol (Lausanne). 2019. https://doi.org/10.3389/fendo.2019.00389.
Marzioni M, Alpini G, Saccomanno S, Candelaresi C, Venter J, Rychlicki C, et al. Glucagon-like peptide-1 and its receptor agonist exendin-4 modulate cholangiocyte adaptive response to cholestasis. Gastroenterology. 2007;133(1):244–55.
Chen B, Zhao W, Dong J, Sima H. Expression of Glp-1r protein and its clinical role in intrahepatic cholangiocarcinoma tissues. Mol Biol Rep. 2014;41(7):4313–20.
Marzioni M, Alpini G, Saccomanno S, Candelaresi C, Venter J, Rychlicki C, et al. Exendin-4, a glucagon-like peptide 1 receptor agonist protects cholangiocytes from apoptosis. Gut. 2009;58(7):990–7.
Nexøe-Larsen C, Sørensen P, Hausner H, Agersnap M, Baekdal M, Brønden A, et al. Effects of liraglutide on gallbladder emptying: a randomized, placebo-controlled trial in adults with overweight or obesity. Diabetes Obes Metab. 2018;20(11):2557–64.
Gether I, Nexøe-Larsen C, Knop F. New avenues in the regulation of gallbladder motility-implications for the use of glucagon-like peptide-derived drugs. J Clin Endocrinol Metab. 2019;104(7):2463–72.
Rehfeld J, Knop F, Asmar A, Madsbad S, Holst J, Asmar M. Cholecystokinin secretion is suppressed by glucagon-like peptide-1: clue to the mechanism of the adverse gallbladder events of Glp-1-derived drugs. Scand J Gastroenterol. 2018;53(12):1429–32.
Shaddinger B, Young M, Billiard J, Collins D, Hussaini A, Nino A. Effect of albiglutide on cholecystokinin-induced gallbladder emptying in healthy individuals: a randomized crossover study. J Clin Pharmacol. 2017;57(10):1322–9.
Gebhard R, Prigge W, Ansel H, Schlasner L, Ketover S, Sande D, et al. The role of gallbladder emptying in gallstone formation during diet-induced rapid weight loss. Hepatology. 1996;24(3):544–8.
Pauletzki J, Althaus R, Holl J, Sackmann M, Paumgartner G. Gallbladder emptying and gallstone formation: a prospective study on gallstone recurrence. Gastroenterology. 1996;111(3):765–71.
LaMorte WW. Biliary motility and abnormalities associated with cholesterol cholelithiasis. Curr Opin Gastroenterol. 1993;9(5):810–6.
Smits M, Tonneijck L, Muskiet M, Hoekstra T, Kramer M, Diamant M, et al. Biliary effects of liraglutide and sitagliptin, a 12-week randomized placebo-controlled trial in type 2 diabetes patients. Diabetes Obes Metab. 2016;18(12):1217–25.
Han T, Zhang S, Tang W, Jiang Z. Bile acids in serum and bile of patients with cholesterol gallstone. World J Gastroenterol. 1998;4(1):82–4.
Lund J, Richardson D, Stürmer T. The active comparator, new user study design in pharmacoepidemiology: historical foundations and contemporary application. Curr Epidemiol Rep. 2015;2(4):221–8.
Yoshida K, Solomon D, Kim S. Active-comparator design and new-user design in observational studies. Nat Rev Rheumatol. 2015;11(7):437–41.
Hawthorne G, Hrisos S, Stamp E, Elovainio M, Francis J, Grimshaw J, et al. Diabetes care provision in UK primary care practices. PLoS ONE. 2012;7(7):E41562.
Williams D, Baxter H, Airey C, Ali S, Turner B. Diabetes UK funded surveys of the structural provision of primary care diabetes services in the UK. Diabet Med. 2002;19(Suppl 4):21–6.
Sharma M, Nazareth I, Petersen I. Trends in incidence, prevalence and prescribing in type 2 diabetes mellitus between 2000 and 2013 in primary care: a retrospective cohort study. BMJ Open. 2016;6(1):E010210.
Aune D, Vatten L. Diabetes mellitus and the risk of gallbladder disease: a systematic review and meta-analysis of prospective studies. J Diabetes Complications. 2016;30(2):368–73.
Chapman BA, Wilson IR, Frampton C, Chisholm R, Stewart N, Eagar G, et al. Prevalence of gallbladder disease in diabetes mellitus. Dig Dis Sci. 1996;41(11):2222–8.
Haffner S, Diehl A, Valdez R, Mitchell B, Hazuda H, Morales P, et al. Clinical gallbladder disease in NIDDM subjects. Relationship to duration of diabetes and severity of glycemia. Diabetes Care. 1993;16(9):1276–84.
Yuan S, Gill D, Giovannucci E, Larsson S. Obesity, type 2 diabetes, lifestyle factors, and risk of gallstone disease: a Mendelian randomization investigation. Clin Gastroenterol Hepatol. 2022;20(3):E529–37.
Bailey C, Day C, Bellary S. Renal protection with Sglt2 inhibitors: effects in acute and chronic kidney disease. Curr Diab Rep. 2022;22(1):39–52.
Karangelis D, Mazer C, Stakos D, Tzifa A, Loggos S, Verma S, et al. Cardio-protective effects of sodium-glucose co-transporter 2 inhibitors: focus on heart failure. Curr Pharm Des. 2021;27(8):1051–60.
Yanai H, Hakoshima M, Adachi H, Katsuyama H. Multi-organ protective effects of sodium glucose cotransporter 2 inhibitors. Int J Mol Sci. 2021;22(9):4416.
Pradhan R, Lu S, Yin H, Yu OHY, Ernst P, Suissa S, et al. Novel antihyperglycaemic drugs and prevention of chronic obstructive pulmonary disease exacerbations among patients with type 2 diabetes: population based cohort study. BMJ. 2022;379:E071380.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research was funded by a Foundation Scheme grant from the Canadian Institutes of Health Research (FDN-143328). SBS is the recipient of a doctoral training award from the Canadian Institutes of Health Research. LA is the recipient of a Distinguished Research Scholar Award from the Fonds de recherche du Québec—Santé and received a William Dawson Scholar award from McGill University. The study funder was not involved in the design of the study; the collection, analysis, and interpretation of data; and writing the report; and did not impose any restrictions regarding the publication of the report.
Conflict of Interests
This study was funded by the Canadian Institutes of Health Research. LA has received speaking and consulting fees from Pfizer and Roche for work unrelated to this project. OY was involved in an advisory board meeting for Novo Nordisk for work unrelated to this study. All other authors declare no conflicts of interest. LA is an Editorial Board member of Drug Safety. LA was not involved in the selection of peer reviewers for the manuscript nor any of the subsequent editorial decisions.
Ethics Approval
The study protocol was approved by the Research Data Governance of the CPRD (protocol 23_002543) and by the Research Ethics Board of the Jewish General Hospital, Montreal, Canada.
Data Availability
No data are available. This study is based on data from the CPRD obtained under license from the UK Medicines and Healthcare products Regulatory Agency. The data are provided by patients and collected by the UK National Health Service as part of their care and support. The interpretation and conclusions contained in this study are those of the authors alone. Because electronic health records are classified as “sensitive data” by the UK Data Protection Act, information governance restrictions (to protect patient confidentiality) prevent data sharing via public deposition. Data are available with approval through the individual constituent entities controlling access to the data. Specifically, the primary care data can be requested via application to the CPRD (https://www.cprd.com).
Code Availability
Codes may be made privately available upon reasonable request to the corresponding author.
Consent to Participate
Not applicable.
Consent to Publish
Not applicable.
Author Contributions
SBS wrote the manuscript, and all authors edited, critically reviewed, and approved the final version of the manuscript. All authors conceived and designed the study, analyzed and interpreted the data, approved the final version of the manuscript, and are accountable for its accuracy. SBS, HY, and LA performed the statistical analyses. LA acquired the data and supervised the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shapiro, S.B., Yin, H., Yu, O.H.Y. et al. Dipeptidyl Peptidase-4 Inhibitors and the Risk of Gallbladder and Bile Duct Disease Among Patients with Type 2 Diabetes: A Population-Based Cohort Study. Drug Saf (2024). https://doi.org/10.1007/s40264-024-01434-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s40264-024-01434-4