Abstract
Introduction
At the time of dapagliflozin’s approval in Europe (2012) to treat patients with type 2 diabetes mellitus, concerns regarding acute liver injury and severe complications of urinary tract infection (sUTI) led to two post-authorization safety (PAS) studies of these outcomes to monitor the safety of dapagliflozin in real-world use.
Objective
To investigate the incidence of hospitalization for acute liver injury (hALI) or sUTI (pyelonephritis or urosepsis) among patients initiating dapagliflozin compared with other glucose-lowering drugs (GLDs).
Methods
These two noninterventional cohort studies identified initiators of dapagliflozin and comparator GLDs in November 2012–February 2019 using data from three longitudinal, population-based data sources: Clinical Practice Research Datalink (UK), the HealthCore Integrated Research Database (USA), and the Medicare database (USA). Outcomes (hALI and sUTI) were identified with electronic algorithms. Incidence rates were estimated by exposure group. Incidence rate ratios (IRRs) were calculated comparing dapagliflozin to comparator GLDs, using propensity score trimming and stratification to address confounding. The sUTI analyses were conducted separately by sex.
Results
In all data sources, hALI and sUTI incidence rates were generally lower in dapagliflozin initiators than comparator GLD initiators. The adjusted IRR (95% confidence interval) pooled across data sources for hALI was 0.85 (0.59–1.24) and for sUTI was 0.76 (0.60–0.96) in females and 0.74 (0.56–1.00) in males. Findings from sensitivity analyses were largely consistent with the primary analyses.
Conclusions
These real-world studies do not suggest increased risks of hALI or sUTI, and they suggest a potential decreased risk of sUTI with dapagliflozin exposure compared with other GLDs.
Similar content being viewed by others
The results of these two post-authorization safety studies of dapagliflozin to assess the risk of hospitalization for acute liver injury (hALI) and the risk of severe complications of urinary tract infection (sUTI), including pyelonephritis and urosepsis, did not suggest increased risks of hALI and sUTI in patients initiating dapagliflozin compared with those initiating comparator glucose-lowering drugs. |
These findings contributed to the removal of liver injury and urinary tract infection as important identified risks in the dapagliflozin risk-management plan in Europe. |
1 Introduction
In clinical trials, dapagliflozin has been shown to be effective in lowering blood glucose levels, body weight, and blood pressure in patients with type 2 diabetes mellitus (T2DM) compared with placebo [1,2,3,4,5]. Dapagliflozin promotes urinary glucose excretion by selectively inhibiting human renal sodium-glucose cotransporter 2 (SGLT2), the major transporter responsible for renal glucose reabsorption. Dapagliflozin was initially approved for the treatment of T2DM by the European Medicines Agency (EMA) in November 2012 and by the US Food and Drug Administration (FDA) in January 2014 [6, 7]. At the time of the initial approval of dapagliflozin to treat T2DM in Europe, four EMA-endorsed pharmacoepidemiological post-authorization safety (PAS) studies were initiated to monitor the safety of dapagliflozin in real-world use [8]. In this report, we describe the results of 2 of these studies: an evaluation of the risk of acute liver injury (EUPAS 12110 [9], NCT02695095 [10]), and an evaluation of the risk of severe complications of urinary tract infection (sUTI) including urosepsis and pyelonephritis (EUPAS 12113 [11], NCT02695173 [12]). Other PAS studies include an assessment of the risk of acute kidney injury [13,14,15], and an assessment of cancer, including specific evaluations of bladder cancer and female invasive breast cancer, which is ongoing at the time of this report [16, 17].
As with other SGLT2 inhibitors, dapagliflozin is minimally metabolized in the liver [18]. In the Phase 3 clinical program for dapagliflozin, the proportions of patients with elevated liver function tests or adverse events of hepatic disorder were similar between the dapagliflozin and placebo groups; however, one patient in the dapagliflozin arm experienced a case of “possible” drug-induced liver injury (DILI) [8]. While this case of possible DILI was later revealed to be a case of autoimmune hepatitis (after the approval of dapagliflozin by the EMA) [19], at the time of regulatory review, the signal was sufficient to prompt investigation into DILI in dapagliflozin initiators in a larger population. Drug-induced liver injury occurs infrequently and therefore is rarely detected in clinical studies, although it is one of the most common forms of drug toxicity and the most common single cause of safety-related drug marketing withdrawals in the last several decades [20]. In addition, dapagliflozin was the first SGLT2 inhibitor to be approved worldwide and therefore the safety profile of SGLT2 inhibitors as a class was not yet characterized. These reasons, and the concerns raised with the one “possible” case of DILI during the Phase 3 trial prior to dapagliflozin approval, led to the inclusion of liver injury in the post-marketing safety monitoring program for dapagliflozin.
Patients with T2DM experience a higher incidence of urinary tract infections than patients without T2DM, with women experiencing higher incidence than men [21]. Possible mechanisms for the increased risk of urinary tract infections in patients with diabetes include glucosuria, diabetes-associated bladder dysfunction, and immune dysfunction related to hyperglycemia [22]. Serious complications of urinary tract infections, such as pyelonephritis and urosepsis, may also be more common in patients with diabetes [22]. Because dapagliflozin’s mechanism of action results in glucosuria, urinary tract infections have been rigorously evaluated in clinical trials. Pooled results of safety data from 12 clinical trials of dapagliflozin showed a small increased incidence of any urinary tract infection in patients treated with 5 mg dapagliflozin (5.7%) or 10 mg dapagliflozin (4.3%) compared with placebo (3.7%) [23]. In longer-term pooled analyses of these trials, there was no increased incidence of pyelonephritis [24]. Due to the increased risk of urinary tract infection among those with T2DM and also among users of dapagliflozin, the post-marketing safety monitoring program for dapagliflozin included an assessment of pyelonephritis and urosepsis, serious conditions that may develop as complications of urinary tract infection, which often require hospitalization and may be life threatening.
We present the results from two large PAS studies, one assessing hospitalization for acute liver injury (hALI) and the other assessing sUTI (hospitalization or emergency department visit for pyelonephritis and/or urosepsis), that were conducted to address potential safety concerns at the time of approval of dapagliflozin in Europe. Specifically, the study objectives were to assess the incidence of hALI or sUTI in patients with T2DM newly treated with dapagliflozin compared with those initiating another glucose-lowering drug (GLD) in a real-world setting.
2 Methods
2.1 Study Population and Study Design
Two noninterventional, population-based studies were conducted concurrently, each using secondary data from three real-world longitudinal claims databases. The Clinical Practice Research Datalink (CPRD) in the UK is an electronic primary healthcare medical records database with linkage to hospital data through the Hospital Episode Statistics database; the HealthCore Integrated Research Database (HIRD) is an administrative claims database in the USA including commercially insured individuals; and the US Medicare research database includes information on federally funded fee-for-service insurance claims. The study period, which varied across the data sources, started on the date that dapagliflozin became available in each country after regulatory approval; ended on the date of the most recently available data at the time of data extraction; and included November 2012 through December 2018 for CPRD, January 2014 through February 2019 for the HIRD, and January 2014 through December 2017 for Medicare.
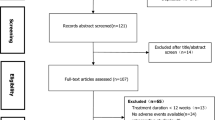
The study design, with inclusion and exclusion criteria for each PAS study cohort, is illustrated in Fig. 1. The study population comprised adult patients initiating dapagliflozin or an eligible comparator GLD (eligible comparator GLD classes and drug substances are listed in Table 1), with or without concomitant use of other GLDs (other than non-dapagliflozin SGLT2 inhibitors) or insulin. Because dapagliflozin was recommended as a second-line therapy for T2DM at the time of the study [25, 26], only drugs that were also considered second-line GLD treatment were eligible comparator GLDs. Metformin monotherapy and monotherapy with a sulfonylurea were not considered eligible comparators, as these are typically used as first-line therapy. Additionally, monotherapy with insulin was not considered as a comparator. However, combination therapy of an eligible comparator GLD with metformin, a sulfonylurea, or insulin were considered as eligible comparators.
Study design, cohort eligibility, and inclusion criteria. CPRD Clinical Practice Research Datalink, GLD glucose-lowering drug, GOLD General Practitioner Online Database of the CPRD, hALI hospitalization for acute liver injury, HIRD HealthCore Integrated Research Database, SGLT2 sodium-glucose cotransporter 2, sUTI severe complications of urinary tract infection (pyelonephritis or urosepsis), T1DM type 1 diabetes mellitus. Schematic based on the framework of graphical representation for visualizing longitudinal study designs proposed by Schneeweiss et al [50]. The light blue box represents the assessment window for use of the index study medication, the orange boxes represent the assessment windows for the exclusion criteria, the dark blue boxes represent the assessment windows for covariate variables, and the green box represents the follow-up period. aCPRD, registered in an up-to-standard participating general medical practice. HIRD, complete pharmacy and medical coverage in a health insurance plan with no enrollment gaps greater than 30 days; Medicare, enrolled in fee-for-service insurance in Parts A (hospital insurance), B (medical insurance), and D (prescription drug coverage). bCPRD, ages < 18 years; HIRD, ages < 18 or > 64 years; Medicare, ages < 65 years. cMedicare, enrolled because of disability or end-stage renal disease; nonresident of a US state or the District of Columbia; enrolled in managed care coverage. dApplicable only to the cohorts assessing the hALI outcome. eApplicable only to the cohorts assessing the sUTI outcome. fBody mass index, smoking history, and alcohol use were available in CPRD GOLD data but were not available in HIRD or Medicare. gDiscontinuation of the study medication (30 days after the end of the days’ supply of the last consecutive prescription or dispensing), hALI or sUTI event, death, end of patient-specific data or eligibility in each data source or end of the study period, initiation of an SGLT2 inhibitor, diagnosis of T1DM
This study used an active-comparator, new-user design, which enhances comparability of treatment groups by selecting patients at comparable stages in the disease trajectory [27]. “New use” was defined as the first recorded prescription or dispensing of dapagliflozin or an eligible comparator GLD within the study period, with no prior recorded prescription for that medication when all available lookback data before the first prescription or dispensing were assessed (a minimum lookback period of 180 days was required for study eligibility). The date of new use of an eligible treatment was considered the index date, and the period of time a patient continuously remained on the eligible treatment was defined as a treatment episode. A given patient could contribute more than one non-overlapping treatment episode within the study period for different eligible medications. Eligible comparator GLD treatment episodes were matched to dapagliflozin treatment episodes based on calendar year of the index date, age, sex, and geographic region. The comparator GLD to dapagliflozin matching ratio was 6:1 in CPRD and 15:1 in the HIRD and Medicare.
2.2 Exposure Assessment
The primary exposure of interest for each PAS study was the initiation of dapagliflozin or an eligible comparator GLD. Medication use was identified from written prescription records in CPRD GOLD (General Practitioner Online Database) by using Gemscript codes and from pharmacy dispensing records in the HIRD and Medicare by using Generic Product Identifiers (GPI) and National Drug Codes (NDCs), respectively.
Exposure time at risk was defined as the period starting the day after the index date until 30 days after the end of the days’ supply of the last consecutive prescription/dispensing in the treatment episode; this definition is based upon the assumption that any potential risk of each of the outcomes of interest would increase shortly after therapy initiation, remain increased during treatment, and then decrease gradually after treatment discontinuation. The duration of each prescription/dispensing was defined as the days’ supply of the medication plus 30 days. If there was more than one consecutive prescription or dispensing for the index medication separated by gaps of 30 days or fewer, the prescriptions/dispensings were concatenated into one treatment episode; the duration of the treatment episode included the gaps between the prescriptions/dispensings and ended 30 days after the end of the days’ supply of the last prescription/dispensing. A detailed description of the treatment episodes is available in ‘Methods and Results’, Section 1.1, of Online Resource 1.
2.3 Outcome Assessment
Electronic case-finding algorithms tailored to each data source were used to identify each of the outcomes, hALI and sUTI (Table 2). Case-finding algorithms were validated through clinical review of a sample of up to 125 cases for each outcome. In the CPRD electronic medical records database, validation was performed by clinical review of chronological patient profiles and by completed questionnaires from general practitioners. In the HIRD and Medicare claims databases, validation was performed by clinician review of medical records. The algorithm-identified cases in the validation samples were classified as either confirmed cases or non-cases according to guidance published by an FDA Working Group [20] and criteria proposed by Navarro and Senior [28] for hALI cases and according to clinical definitions for pyelonephritis [29] or urosepsis [30] for sUTI cases.
2.4 Baseline Characteristics and Covariates
Baseline characteristics included demographic and lifestyle characteristics, comorbidities, comedications, and healthcare resource utilization and were assessed on or before the index date for each treatment episode. Baseline characteristics were assessed using all available lookback data, unless otherwise specified. Healthcare resource utilization variables (number of outpatient encounters to a general practice or outpatient clinic, number of hospitalizations, number of emergency department visits, and number of specialty care visits) and comedications were assessed in the 180 days before the index date. All measured baseline characteristics were considered for inclusion in propensity score (PS) modeling as covariates for confounding adjustment, as described below.
2.5 Statistical Analysis
Each of the outcomes, hALI and sUTI, were analyzed in separate outcome-specific cohorts in each data source. The sUTI outcome was analyzed separately for females and males. Data from CPRD and Medicare were analyzed by RTI Health Solutions, and the HIRD data were analyzed by HealthCore, Inc. After the inclusion and exclusion criteria and the matching were applied to generate each of the study cohorts, descriptive analyses were conducted of each cohort by treatment group by calculating frequencies and percentages for categorical variables and by calculating means and standard deviations or medians, interquartile ranges, or minimum and maximum values for continuous variables. The absolute standardized difference was used to assess the balance of baseline characteristics between the dapagliflozin and comparator GLD groups [31].
Potential confounding was addressed by using PS trimming and stratification to identify dapagliflozin and comparator GLD groups with balanced characteristics [32, 33]. The PS modeling approach is described in detail in ‘Methods and Results’, Section 1.2, of Online Resource 1. Briefly, the PSs, or the predicted probability of initiating treatment with dapagliflozin given the observed characteristics, were estimated for each treatment episode by fitting a multivariable logistic regression model, which included (1) dapagliflozin versus comparator GLD exposure as the dependent variable and (2) all baseline variables identified as potential confounders of the association between dapagliflozin and the outcome (hALI or sUTI) as independent variables [31]. All baseline variables were considered for inclusion in the PS models, and included demographic characteristics, lifestyle characteristics, calendar year of the index date, type of index medication (see ‘Methods and Results’, Section 1.5, of Online Resource 1, for a description of the type of index medication categories), number of years since the initial T2DM diagnosis, diabetes severity indicators, comedications, comorbidities, and healthcare utilization variables. Patients with an extreme PS (i.e., below the 2.5th percentile value of the dapagliflozin-exposed distribution and above the 97.5th percentile of the comparator GLD-exposed distribution) were trimmed (i.e., excluded from the analytic cohort). The remaining treatment episodes were ranked by PS value and divided into equally sized strata. Confounding control was assessed by evaluating the balance of covariates between treatment groups within each PS stratum using the absolute standardized difference values.
Incidence and comparative analyses were performed by using algorithm-identified hALI or sUTI events. Propensity score-adjusted incidence rates (IRs) of hALI and sUTI were estimated by first calculating crude IRs across the PS strata within each exposure group; then for each exposure group, the stratum-specific IR was standardized by using the person-years in the dapagliflozin group to estimate the standardized IR and variance, with the 95% confidence intervals (CIs) estimated by using the exact limits method [34].
Incidence rate ratios (IRRs) were calculated in each data source for each outcome by dividing the IR in the dapagliflozin group by the IR in the comparator GLD group, with the 95% CI estimated by using a Poisson distribution. Adjusted IRRs were estimated by calculating the IRR in each PS stratum and then combining the stratum-specific IRRs by using the Mantel-Haenszel method [35]. Database-specific adjusted IRR estimates were pooled to generate an overall adjusted IRR estimate and 95% CI also by using the Mantel-Haenszel method [35] (the detailed methods for the pooled analysis are provided in ‘Methods and Results’, Section 1.3, of Online Resource 1).
Sensitivity analyses were conducted and comprised (1) an extension of the risk window after the end of the medication's days' supply from 30 days to 90 days; (2) inclusion of only dipeptidyl peptidase-4 (DPP-4) inhibitors in the comparator GLD group; (3) inclusion of only glucagon-like peptide-1 (GLP-1) receptor agonists in the comparator GLD group; (4) inclusion of only patients new to the comparator GLD class (i.e., no previous use of a drug within the GLD class); and (5) inclusion of only the first treatment episode for an individual patient. A quantitative bias analysis was performed to assess the possible effect of potential unmeasured confounding variables of various strengths and prevalence on the effect estimate (the quantitative bias analysis is described in detail in ‘Methods and Results’, Section 1.4, of Online Resource 1) [36].
The study protocols for both PAS studies were reviewed and approved by the RTI International Institutional Review Board. For the CPRD and Medicare aspects, the UK Medicines Healthcare products Regulatory Agency’s Independent Scientific Advisory Committee (ISAC) and the US Centers for Medicare and Medicaid Services (CMS) Privacy Board approved the use of the respective data for these studies. The HealthCore-specific components were reviewed and approved by the New England Institutional Review Board. A waiver of informed consent was obtained, as data used in these studies were obtained from databases of anonymized medical records, claims, and pharmacy records and not directly from human subjects.
3 Results
3.1 Hospitalization for Acute Liver Injury Outcome
3.1.1 Baseline Characteristics
There were 129,520 potentially eligible treatment episodes (dapagliflozin or an eligible comparator GLD) in CPRD, 1,060,582 in the HIRD, and 2,474,817 in Medicare. After all inclusion and exclusion criteria and treatment-episode matching were applied, the final number of treatment episodes was 49,639 (dapagliflozin, 10,466; comparator GLD, 39,173) in CPRD, 212,580 (dapagliflozin, 17,187; comparator GLD, 195,393) in the HIRD, and 212,473 (dapagliflozin, 13,280; comparator GLD, 199,193) in Medicare (Table S1 in Online Resource 1).
Baseline characteristics for the treatment groups in the full hALI cohort (i.e., after matching and before PS trimming) are presented in Table 3. The mean age of patients at the index date was 57 years for the dapagliflozin group and 59 years for comparator GLD group in CPRD, 52 and 70 years for both treatment groups in the HIRD and Medicare, respectively. In CPRD (the only data source with available information on body mass index), more dapagliflozin users were obese or severely obese (74%) than comparator GLD users (61%). In all three data sources, a higher proportion of dapagliflozin users than comparator GLD users had concomitant insulin use on the index date, and dapagliflozin initiators were more likely to have used three or more other classes of GLD medications in the year before the index date. The proportion with one or more dispensing/prescription for a drug with a known association with liver injury (for the list of drugs, see Table S2 in Online Resource 1) as well as the prevalence of most baseline medical conditions were similar across the dapagliflozin and comparator GLD groups within each data source.
Propensity score trimming and stratification were effective in achieving balance between the treatment groups for the variables included in the PS models (Fig. S1 in Online Resource 1). For the included covariates, most absolute standardized differences were below 0.10, corresponding to small differences in the distribution of the variable between the dapagliflozin and comparator GLD groups. The baseline characteristics for the hALI cohort after PS trimming are presented in Table S3 in Online Resource 1.
3.1.2 Incidence and Comparative Analyses
The incidence and comparative analyses were performed by using hALI events identified by the case-finding algorithm, which, in CPRD, included more than 20 but fewer than 25 events combined across both treatment groups (CPRD policy does not allow values of 1 to 4 to be reported, which in this case, applies to the small number of hALI events identified in the dapagliflozin group; a range is given to prevent back calculation of the small number of events in the dapagliflozin group). There were 186 and 202 total hALI events in the HIRD and Medicare, respectively. Table 4 presents the number of hALI events, exposure time, and adjusted IRs by exposure group for each data source. The estimated PS-adjusted IR of hALI per 1000 person-years for dapagliflozin and comparator GLD treatment episodes, respectively, was 0.37 (95% CI 0.10–0.93) and 0.62 (95% CI 0.27–1.11) in CPRD, 1.36 (95% CI 0.74–2.28) and 1.83 (95% CI 1.55–2.15) in the HIRD, and 1.92 (95% CI 1.02–3.29) and 1.70 (95% CI 1.42–2.02) in Medicare.
The adjusted IRR estimates were below the null value of 1.0 in CPRD, and the HIRD and was slightly above the null value in Medicare (Fig. 2). The overall adjusted hALI IRR estimate (pooled across all data sources) was 0.85 (95% CI 0.59–1.24). The 95% CIs were wide for all adjusted IRR estimates because of a small number of hALI events.
3.1.3 Sensitivity and Bias Analyses
The adjusted IRR results from all sensitivity analyses for hALI in the HIRD and Medicare were generally similar to the primary analysis and, in CPRD, were variable because of a small number of hALI events (Fig. S2 in Online Resource 1). The assessment of the potential impact of possible unmeasured confounders indicates that it is unlikely that an unmeasured hypothetical confounder would mask a harmful association of hALI with dapagliflozin (the results from this analysis are described in detail in ‘Methods and Results’, Section 1.4 and Fig. S7, of Online Resource 1).
The electronic algorithms had low to moderate validity in identifying true cases of hALI in each of the three data sources [37,38,39]; however, simulation analyses to assess the impact of potential outcome misclassification indicated that it is unlikely that an increased risk of hALI associated with dapagliflozin, if it exists, is being masked by outcome misclassification that differs between the treatment groups (data on file with the corresponding author).
3.2 Severe Complication of Urinary Tract Infection Outcome
3.2.1 Baseline Characteristics
After all inclusion and exclusion criteria and treatment-episode matching were applied, the final number of treatment episodes in the sUTI female cohort was 26,315 (dapagliflozin, 5508; comparator GLD, 20,807) in CPRD, 135,299 (dapagliflozin, 10,544; comparator GLD, 124,755) in the HIRD, and 200,976 (dapagliflozin, 12,561; comparator GLD, 188,415) in Medicare; the final number of treatment episodes selected into the male cohort was 36,805 (dapagliflozin, 7610; comparator GLD, 29,195) in CPRD, 160,828 (dapagliflozin, 13,091; comparator GLD, 147,737) in the HIRD, and 204,519 (dapagliflozin, 12,783; comparator GLD, 191,736) in Medicare (Table S4 in Online Resource 1).
Baseline characteristics for the full sample of patients in the sUTI cohorts (i.e., after matching and before PS trimming) are presented in Table 5. The mean age at the index date was similar among males and females within each data source. Among both females and males, the mean age in CPRD was approximately 57 years in the dapagliflozin group and approximately 59 years in the comparator GLD group; the mean age in the HIRD was approximately 52 years for both treatment groups, and in Medicare it was approximately 72 years for both treatment groups. In CPRD, the proportion of users who were obese or severely obese was higher in dapagliflozin users (79% of females, 72% of males) than in comparator GLD users (67% of females, 58% of males). In all data sources for females and males, the prevalence of insulin use at the index date was higher for the dapagliflozin group than the comparator GLD group, and dapagliflozin initiators were more likely to have used 3 or more other classes of GLD medications in the year before the index date. For females and males, a history of kidney disease of all types (acute and chronic) was more common in the comparator GLD group than the dapagliflozin group, but the prevalence of chronic or recurring urinary tract infections was similar between the two treatment groups. Other medical conditions were similarly distributed between the dapagliflozin and comparator GLD groups.
Similar to the hALI cohorts, PS trimming and stratification were very effective in achieving balance between the treatment groups for the variables in the PS models in both the female and male sUTI cohorts in all the data sources; most PS-stratified values of the absolute standardized difference were below 0.10 (Fig. S3 in Online Resource 1). The baseline characteristics for the sUTI sample after PS trimming are presented in Table S5 in Online Resource 1.
3.2.2 Incidence and Comparative Analyses
The total number of algorithm-identified sUTI events for the incidence and comparative analyses in females was 27 in CPRD, 450 in the HIRD, and 904 in Medicare, and in males it was 25 in CPRD, 230 in the HIRD, and 584 in Medicare. Across the data sources in both females and males, the PS-adjusted IR estimates per 1000 person-years was consistently lower in the dapagliflozin group than in the comparator GLD group (Table 6).
For both females and males, when the IRs of sUTI were compared between the dapagliflozin group and the comparator GLD group, the adjusted IRR estimates were below the null value of 1.0 for all data sources, although the CIs were wide in CPRD due to the small number of sUTI events (Fig. 3). The overall adjusted sUTI IRR estimate pooled across all data sources was similar for females (0.76 [95% CI 0.60–0.96]) and males (0.74 [95% CI 0.56–1.00]).
3.2.3 Sensitivity and Bias Analyses
The adjusted IRR results of most sensitivity analyses were consistent with those of the primary analyses of sUTI for both males and females (Fig. S4 in Online Resource 1). The assessment of potential unmeasured confounders for the sUTI analysis had similar results to those for the hALI analysis (the results from this analysis are described in detail in ‘Methods and Results’, Section 1.4 and Fig. S8, in Online Resource 1).
The case-finding algorithms had moderate validity in identifying true cases of sUTI in each of the three data sources [37,38,39], and, similar to hALI, simulation analyses indicate that it is unlikely that a potential increased risk of sUTI associated with dapagliflozin, if it exists, is being masked by misclassification of sUTI that differs between the treatment groups (data on file with the corresponding author).
4 Discussion
Safety labeling for new prescription drugs is often based on a limited number of events observed in the relatively short time frame of clinical trials. Compared with clinical trials, PAS studies, such as those reported here, can be conducted over longer time spans and with larger base populations that are fully representative of the target population and can clarify the magnitude of these outcomes in the treated populations in a real-world setting.
The two large observational PAS studies reported here, comprising three healthcare databases with 3–6 years of observation per database, found no increased risk of hALI or sUTI associated with dapagliflozin exposure compared with other GLD medications. The assessment of hALI included over 28,000 person-years of dapagliflozin exposure, and the assessment of sUTI included over 17,000 and 22,000 person-years of dapagliflozin exposure in females and males, respectively; however, because of a small number of hALI and sUTI events, the database-specific IRR estimates were imprecise, with wide CIs. For hALI, the pooled adjusted IRR estimate was 0.85 (95% CI 0.59–1.24), while for sUTI, the pooled adjusted IRR estimate was 0.76 (95% CI 0.60–0.96) for females and 0.74 (95% CI 0.56–1.00) for males. The pooled adjusted IRR point estimates for both outcomes were below the null value of 1.0, suggesting a decrease in risk associated with dapagliflozin exposure compared with other GLD medications. However, the 95% CI estimates are imprecise and compatible with the null value.
There is scant published literature reporting risk of acute liver injury associated with SGLT2 inhibitors. In prelicensure clinical studies, no SGLT2 inhibitor medications (canagliflozin, dapagliflozin, empagliflozin, ertugliflozin) were associated with acute liver injury [18]. The Dapagliflozin Effect on CardiovascuLAR Events (DECLARE) trial – a randomized, double-blind, placebo-controlled, Phase 3 trial of dapagliflozin in patients with T2DM and with either known cardiovascular disease or two or more risk factors for cardiovascular disease in addition to T2DM – assessed 17,160 patients during a median of 4.2 years with about 30,000 person-years of exposure to dapagliflozin. As part of the evaluation of secondary outcomes, the occurrence of hepatic events was reported to be similar in the dapagliflozin group compared with the placebo group (hazard ratio [HR], 0.92; 95% CI 0.68–1.25) [40, 41]. This estimate is similar to the pooled adjusted IRR estimate for hALI in the current study (0.85; 95% CI 0.59–1.24). The metabolism of SGLT2 inhibitors in the liver is minimal and could partially explain the relative lack of reporting of hepatotoxicity with dapagliflozin [18].
Overall, for both males and females, we found no increased risk for severe complications (pyelonephritis and/or urosepsis) of urinary tract infection associated with dapagliflozin, and instead, the results suggested a decreased risk when compared with other GLDs. In a previous analysis of safety data pooled from 13 placebo-controlled trials of dapagliflozin of up to 24 weeks’ duration, the occurrence of urinary tract infections (as adverse events or serious adverse events) was slightly higher with dapagliflozin (4.7%) than with placebo (3.5%), with a higher frequency in women than men in both treatment groups [42]. Similarly, a recent meta-analysis of clinical trials assessing safety outcomes in users of SGLT2 inhibitors reported that dapagliflozin users had an increased risk of urinary tract infection compared with users of other non-SGLT2 inhibitor comparator treatments (relative risk: 1.42; 95% CI 1.07–1.87) [43]. However, urinary tract infections associated with dapagliflozin use are typically mild and respond well to standard of care treatment [22, 23, 44]. In the large, Phase 3 DECLARE trial, the incidence of urinary tract infections that occurred as serious adverse events or led to treatment discontinuation was similar in the dapagliflozin (1.5%) and placebo (1.6%) groups (HR, 0.93; 95% CI 0.73–1.18) [40, 41]. Published population-based observational studies using real-world data have demonstrated similar or lower rates of urinary tract infection outcomes with SGLT2 inhibitors as a group compared with other second-line or later-line therapy (DPP-4 inhibitors or GLP-1 receptor agonists) [45,46,47,48,49]. One study, performed in two US healthcare claims databases, assessed a composite outcome (hospitalization for primary urinary tract infection, sepsis with urinary tract infection, or pyelonephritis) similar to our outcome of sUTI, and found no increased risk associated with SGLT2 inhibitors compared with DPP-4 inhibitors (HR, 0.57; 95% CI 0.29–1.14) or GLP-1 receptor agonists (HR, 0.52; 95% CI 0.28–0.97) [45]. Similarly, another study that used data from Canadian healthcare administrative databases and CPRD reported no increased risk of urosepsis when comparing new users of SGLT2 inhibitors to new users of DPP-4 inhibitors (pooled adjusted HR: 0.58; 95% CI 0.42–0.80), and this finding was consistent when dapagliflozin was assessed alone (HR, 0.63; 95% CI 0.36–1.12) [46]. Our study builds on these previous studies by examining the effects of dapagliflozin alone compared with other GLDs on pyelonephritis and urosepsis, providing separate estimates for females and males across three large population-based data sources in the UK and the USA. Mild and uncomplicated urinary tract infections were not the focus of our study.
An important strength of these studies is the large, population-based sample of dapagliflozin users, which comprised over 40,000 and 62,000 new dapagliflozin treatment episodes across the data sources for assessing hALI and sUTI, respectively. Matching and PS trimming and stratification were used to address confounding for observed covariates and resulted in well-balanced treatment groups; however, in observational studies that use data collected for other purposes (i.e., electronic medical record or health insurance billing claims), bias can occur from confounding factors that cannot be measured in the data source. Lifestyle variables (i.e., body mass index, smoking status, and alcohol use), which may have been potential confounding variables, were only available in the CPRD data and thus could not be directly accounted for in the HIRD or Medicare data. However, results from CPRD, which included lifestyle variables, were largely similar to those of the other two databases, and quantitative bias analyses suggested that unmeasured confounders would be required to be either quite strong or highly imbalanced between the treatment groups to mask a truly elevated association between dapagliflozin and either of the study outcomes. In CPRD, full prescription information, including prescriptions from specialists, is not available, and, therefore, it is possible that if initial prescriptions were provided by specialist physicians, rather than general practitioners, the first use of dapagliflozin or comparator GLD would not be properly captured. Similarly, inpatient administration of medications in the HIRD and Medicare was not captured. No databases recorded the use of over-the-counter medication. Furthermore, IRR estimates for each outcome in the individual data sources were imprecise due to the low number of hALI and sUTI events, particularly among dapagliflozin users.
5 Conclusions
Results from two large, robust multi-year real-world studies do not suggest an increased risk of hospitalization for acute liver injury (> 28,000 person-years of dapagliflozin exposure) or severe complications of urinary tract infection (about 40,000 person-years of dapagliflozin exposure) associated with new exposure to dapagliflozin compared with new exposure to other GLDs. The results from these PAS studies, combined with evidence from the DECLARE trial on dapagliflozin [40, 41], contributed to the removal of liver injury and urinary tract infection as important identified risks in the dapagliflozin risk management plan in Europe.
References
Bailey CJ, Gross JL, Hennicken D, Iqbal N, Mansfield TA, List JF. Dapagliflozin add-on to metformin in type 2 diabetes inadequately controlled with metformin: a randomized, double-blind, placebo-controlled 102-week trial. BMC Med. 2013;11:43.
Bailey CJ, Morales Villegas EC, Woo V, Tang W, Ptaszynska A, List JF. Efficacy and safety of dapagliflozin monotherapy in people with type 2 diabetes: a randomized double-blind placebo-controlled 102-week trial. Diabet Med. 2015;32(4):531–41.
Wilding JP, Woo V, Rohwedder K, Sugg J, Parikh S, Dapagliflozin 006 Study Group. Dapagliflozin in patients with type 2 diabetes receiving high doses of insulin: efficacy and safety over 2 years. Diabetes Obes Metab. 2014;16(2):124–36.
Wilding JP, Woo V, Soler NG, Pahor A, Sugg J, Rohwedder K, et al. Long-term efficacy of dapagliflozin in patients with type 2 diabetes mellitus receiving high doses of insulin: a randomized trial. Ann Intern Med. 2012;156(6):405–15.
Sjostrom CD, Johansson P, Ptaszynska A, List J, Johnsson E. Dapagliflozin lowers blood pressure in hypertensive and non-hypertensive patients with type 2 diabetes. Diab Vasc Dis Res. 2015;12(5):352–8.
European Medicines Agency. Forxiga. 2021. https://www.ema.europa.eu/en/medicines/human/EPAR/forxiga. Accessed 15 Apr 2022.
US Food and Drug Administration. FARXIGA® prescribing information. 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/202293s024lbl.pdf. Accessed 3 Jan 2022.
European Medicines Agency. Committee for Medicinal Products for Human Use (CHMP) Assessment Report: Forxiga, dapagliflozin; Procedure No.: EMEA/H/C/002322. 2012. https://www.ema.europa.eu/en/documents/assessment-report/forxiga-epar-public-assessment-report_en.pdf. Accessed 15 Apr 2022.
European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP). EUPAS12110: Comparison of the risk of acute liver injury between patients with type 2 diabetes exposed to dapagliflozin and those exposed to other antidiabetic treatments. European Union Electronic Register of Post-Authorisation Studies. 2021. https://www.encepp.eu/encepp/viewResource.htm?id=44089. Accessed 18 Jan 2022.
ClinicalTrials.gov. Acute Liver Injury in Patients on Dapagliflozin: NCT02695095. 2021. https://clinicaltrials.gov/ct2/show/NCT02695095. Accessed 6 Jul 2022.
European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP). EUPAS12113: Comparison of the Risk of Severe Complications of Urinary Tract Infections (UTI) Between Patients With Type 2 Diabetes Exposed to Dapagliflozin and Those Exposed to Other Antidiabetic Treatments. European Union Electronic Register of Post-Authorisation Studies. 2021. https://www.encepp.eu/encepp/viewResource.htm?id=44093. Accessed 18 Jan 2022.
ClinicalTrials.gov. Complications of UTI in Patients on Dapagliflozin: NCT02695173. 2021. https://clinicaltrials.gov/ct2/show/NCT02695173. Accessed 6 Jul 2022.
European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP). EUPAS11684: Comparison of the risk of acute kidney injury between patients with type 2 diabetes exposed to dapagliflozin and those exposed to other antidiabetic treatments. European Union Electronic Register of Post-Authorisation Studies. 2021. https://www.encepp.eu/encepp/viewResource.htm?id=44085. Accessed 6 Jul 2022.
ClinicalTrials.gov. Acute Kidney Injury in Patients on Dapagliflozin and Other Antidiabetic Medications: NCT02695082. 7 Dec 2021. https://clinicaltrials.gov/ct2/show/NCT02695082. Accessed 6 Jul 2022.
Johannes CB, Beachler DC, Layton JB, Danysh HE, Ziemiecki R, Arana A, et al. Post-authorization safety study of hospitalization for acute kidney injury in patients with type 2 diabetes exposed to Dapagliflozin in a real-world setting. Drug Saf. 2022. https://doi.org/10.1007/s40264-022-01263-3.
ClinicalTrials.gov. Cancer in Patients on Dapagliflozin and Other Antidiabetic Treatment: NCT02695121. 30 Jun 2022. https://clinicaltrials.gov/ct2/show/NCT02695121. Accessed 6 Oct 2022.
European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP). EUPAS12116: Comparison of the Risk of Cancer Between Patients With Type 2 Diabetes Exposed to Dapagliflozin and Those Exposed to Other Antidiabetic Treatments. European Union Electronic Register of Post-Authorisation Studies. 2017. https://www.encepp.eu/encepp/viewResource.htm?id=19751. Accessed 6 Oct 2022.
National Institute of Diabetes and Digestive and Kidney Diseases. Sodium glucose cotransporter-2 (SGLT-2) inhibitors. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet], 2018.
Bristol-Myers Squibb. Summary review for regulatory action: Farxiga (dapagliflozin)-Application Number 202293Orig1s000. 2013. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/202293Orig1s000SumR.pdf. Accessed 13 Dec 2021.
US Food and Drug Administration. Guidance for industry. Drug-induced liver injury: premarketing clinical evaluation. Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research. 2009. https://www.fda.gov/media/116737/download. Accessed 27 Sep 2022.
Nichols GA, Brodovicz KG, Kimes TM, Deruaz-Luyet A, Bartels DB. Prevalence and incidence of urinary tract and genital infections among patients with and without type 2 diabetes. J Diabetes Complications. 2017;31(11):1587–91.
Geerlings S, Fonseca V, Castro-Diaz D, List J, Parikh S. Genital and urinary tract infections in diabetes: impact of pharmacologically-induced glucosuria. Diabetes Res Clin Pract. 2014;103(3):373–81.
Johnsson KM, Ptaszynska A, Schmitz B, Sugg J, Parikh SJ, List JF. Urinary tract infections in patients with diabetes treated with dapagliflozin. J Diabetes Complic. 2013;27(5):473–8.
Ptaszynska A, Johnsson KM, Parikh SJ, de Bruin TW, Apanovitch AM, List JF. Safety profile of dapagliflozin for type 2 diabetes: pooled analysis of clinical studies for overall safety and rare events. Drug Saf. 2014;37(10):815–29.
Brown E, Heerspink HJL, Cuthbertson DJ, Wilding JPH. SGLT2 inhibitors and GLP-1 receptor agonists: established and emerging indications. Lancet. 2021;398(10296):262–76.
Shin JI. Second-line glucose-lowering therapy in type 2 diabetes mellitus. Curr Diab Rep. 2019;19(8):54.
Lund JL, Richardson DB, Sturmer T. The active comparator, new user study design in pharmacoepidemiology: historical foundations and contemporary application. Curr Epidemiol Rep. 2015;2(4):221–8.
Navarro VJ, Senior JR. Drug-related hepatotoxicity. N Engl J Med. 2006;354(7):731–9.
Patkar NM, Curtis JR, Teng GG, Allison JJ, Saag M, Martin C, et al. Administrative codes combined with medical records based criteria accurately identified bacterial infections among rheumatoid arthritis patients. J Clin Epidemiol. 2009;62(3):321–7 (7 e1-7).
Wagenlehner FM, Pilatz A, Naber KG, Weidner W. Therapeutic challenges of urosepsis. Eur J Clin Invest. 2008;38(Suppl 2):45–9.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–107.
Sturmer T, Rothman KJ, Avorn J, Glynn RJ. Treatment effects in the presence of unmeasured confounding: dealing with observations in the tails of the propensity score distribution–a simulation study. Am J Epidemiol. 2010;172(7):843–54.
Brookhart MA, Wyss R, Layton JB, Sturmer T. Propensity score methods for confounding control in nonexperimental research. Circ Cardiovasc Qual Outcomes. 2013;6(5):604–11.
Dobson AJ, Kuulasmaa K, Eberle E, Scherer J. Confidence intervals for weighted sums of Poisson parameters. Stat Med. 1991;10(3):457–62.
Rothman K, Greenland S, Lash TL. Modern Epidemiology. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008.
Lash TL, Fox MP, Fink AK. Unmeasured and unknown confounders. In: Applying quantitative bias analysis to epidemiologic data. New York: Springer Science and Business Media, LLC; 2009, p. 59–78.
Zhou CK, Dinh J, Danysh HE, Johannes C, Gutierrez L, Schmid R, et al. Validity of claims-based algorithms to identify acute kidney injury, acute liver injury, severe complications of urinary tract infections, breast cancer, and bladder cancer among patients with type 2 diabetes: a pilot study. Pharmacoepidemiol Drug Saf. 2019;28(S2):157–8.
Danysh HE, Gilsenan A, Arana A, Pladevall-Vila M, Layton JB, Ziemiecki R, et al. Validation of acute outcomes among patients with type 2 diabetes mellitus in the Clinical Practice Research Datalink. Pharmacoepidemiol Drug Saf. 2021;30(S1):393–4.
Danysh HE, Layton JB, Beachler DC, Arana A, Pladevall-Vila M, Schmid R, et al. Validation of acute outcomes among patients with type 2 diabetes mellitus in medicare: a pilot study. Pharmacoepidemiol Drug Saf. 2020;29(Suppl 3):396.
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–57.
Cahn A, Raz I, Bonaca M, Mosenzon O, Murphy SA, Yanuv I, et al. Safety of dapagliflozin in a broad population of patients with type 2 diabetes: analyses from the DECLARE-TIMI 58 study. Diabetes Obes Metab. 2020;22(8):1357–68.
Jabbour S, Seufert J, Scheen A, Bailey CJ, Karup C, Langkilde AM. Dapagliflozin in patients with type 2 diabetes mellitus: a pooled analysis of safety data from phase IIb/III clinical trials. Diabetes Obes Metab. 2018;20(3):620–8.
Donnan JR, Grandy CA, Chibrikov E, Marra CA, Aubrey-Bassler K, Johnston K, et al. Comparative safety of the sodium glucose co-transporter 2 (SGLT2) inhibitors: a systematic review and meta-analysis. BMJ Open. 2019;9(1): e022577.
Li D, Wang T, Shen S, Fang Z, Dong Y, Tang H. Urinary tract and genital infections in patients with type 2 diabetes treated with sodium-glucose co-transporter 2 inhibitors: a meta-analysis of randomized controlled trials. Diabetes Obes Metab. 2017;19(3):348–55.
Dave CV, Schneeweiss S, Kim D, Fralick M, Tong A, Patorno E. Sodium-glucose cotransporter-2 inhibitors and the risk for severe urinary tract infections: a population-based cohort study. Ann Intern Med. 2019;171(4):248–56.
Fisher A, Fralick M, Filion KB, Dell’Aniello S, Douros A, Tremblay E, et al. Sodium-glucose co-transporter-2 inhibitors and the risk of urosepsis: a multi-site, prevalent new-user cohort study. Diabetes Obes Metab. 2020;22(9):1648–58.
Gadzhanova S, Pratt N, Roughead E. Use of SGLT2 inhibitors for diabetes and risk of infection: analysis using general practice records from the NPS MedicineWise MedicineInsight program. Diabetes Res Clin Pract. 2017;130:180–5.
Lega IC, Bronskill SE, Campitelli MA, Guan J, Stall NM, Lam K, et al. Sodium glucose cotransporter 2 inhibitors and risk of genital mycotic and urinary tract infection: a population-based study of older women and men with diabetes. Diabetes Obes Metab. 2019;21(11):2394–404.
Ueda P, Svanstrom H, Melbye M, Eliasson B, Svensson AM, Franzen S, et al. Sodium glucose cotransporter 2 inhibitors and risk of serious adverse events: nationwide register based cohort study. BMJ. 2018;363: k4365.
Schneeweiss S, Rassen JA, Brown JS, Rothman KJ, Happe L, Arlett P, et al. Graphical depiction of longitudinal study designs in health care databases. Ann Intern Med. 2019;170(6):398–406.
Research Data Assistance Center. Revenue center code (FFS). 2022. https://www.resdac.org/cms-data/variables/revenue-center-code-ffs. Accessed 15 Feb 2022.
Acknowledgments
In the preparation of this article, medical writing assistance was provided by S. Musetti and K. Lothman of RTI Health Solutions; editorial assistance was provided by J. Forbes of RTI Health Solutions; graphics assistance was provided by E. Gill of RTI Health Solutions; and critical review and feedback on the manuscript was provided by L. Gutierrez of RTI Health Solutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Sponsorship for the 2 described post-authorization safety studies, medical writing support, and the article-processing charge were provided by AstraZeneca.
Competing Interests
HED, CBJ, JBL, RZ, AA, BC, MPV, and AG are full-time employees of RTI Health Solutions, an independent nonprofit research organization, which was retained by AstraZeneca to conduct the research that is the subject of this manuscript. DCB is an employee of HealthCore, a wholly owned subsidiary of Anthem Inc, which was also retained by AstraZeneca to conduct this research. JD and LL were employees of HealthCore at the time these studies were conducted. RTI Health Solutions and HealthCore associates’ compensation is unconnected to the studies on which they work. PRH, HC, CK, and KJ are employees of AstraZeneca and hold shares and/or stock options in the company.
Authorship and Author Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article. HED contributed to project administration and resources (including data acquisition), interpretation of the results, writing of the original draft, and supervision. CBJ contributed to the study design, methodology, interpretation of the results, writing of the original draft, and supervision. DCB and JBL contributed to the study design, methodology, and interpretation of the results. RZ contributed to the methodology, data curation, and formal analysis. JD contributed to project administration and resources (including data acquisition), and the interpretation of the results. LL and BC contributed to data curation and formal analysis. AA and MPV contributed to the study design and methodology. PH and HC contributed to the methodology and interpretation of the results. CK and KJ contributed to interpretation of results. AG contributed to the conceptualization, study design, interpretation of the results, project administration and resources, and supervision. All authors critically reviewed the draft versions of the manuscript and approved the final version.
Compliance and Ethics Guidelines
The study protocols for both post-authorization safety studies were reviewed and approved by the RTI International Institutional Review Board (study ID 13887). For the CPRD and Medicare aspects, the UK Medicines Healthcare products Regulatory Agency’s (MHRA) Independent Scientific Advisory Committee (ISAC) and the US Centers for Medicare and Medicaid Services (CMS) Privacy Board approved the use of the respective data for these studies (ISAC protocol ID 15_220; CMS data use agreement RSCH-2018-51681). The HealthCore-specific components were reviewed and approved by the New England Institutional Review Board (study ID 120180081). A waiver of informed consent was obtained, as data used in these studies were obtained from databases of anonymized medical, claims, and pharmacy records and not directly from human subjects.
Data Availability
The CMS Privacy Board approved access to Medicare Research Identifiable Files for use in these studies under a data use agreement with RTI Health Solutions (https://resdac.org/). Data in CPRD are provided by patients and collected by the National Health Service (NHS) as part of patient care and support; the UK MHRA ISAC approved the use of CPRD GOLD and accompanying linkage data (including Hospital Episode Statistics [HES], death registration data from the Office for National Statistics [ONS; Copyright © 2019, reused with the permission of The Health & Social Care Information Centre. All rights reserved.], and data from the Index of Multiple Deprivation [IMD]) for these studies, and the data were obtained under a data license from the UK MHRA (https://www.cprd.com/). Data in the HIRD are provided by members of Anthem Inc. Data cannot be shared given privacy regulations. There was no active enrollment or active follow-up of study subjects, and no data were collected directly from individuals. Further information can be requested from each of the data entities as described above. The interpretation and conclusions of the studies described in this manuscript are those of the authors alone.
Code availability
Not applicable.
Consent to participate
Individual-level consent was not required for these analyses of secondary data from anonymized medical, claims, and pharmacy records and not directly from human subjects.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Danysh, H.E., Johannes, C.B., Beachler, D.C. et al. Post-Authorization Safety Studies of Acute Liver Injury and Severe Complications of Urinary Tract Infection in Patients with Type 2 Diabetes Exposed to Dapagliflozin in a Real-World Setting. Drug Saf 46, 175–193 (2023). https://doi.org/10.1007/s40264-022-01262-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-022-01262-4