Abstract
Introduction
Adverse events of radiopharmaceuticals may be underreported or remain undetected. Patients can provide information about these adverse events to enable healthcare professionals to detect, understand, and manage them more efficiently.
Objective
In this study, we aimed to (a) determine the type, causality, and frequency of patient-reported adverse events of radiopharmaceuticals and to (b) assess the onset, outcome, and follow-up of these adverse events from the patient’s perspective.
Methods
We performed a prospective cohort study of 1002 patients who underwent a nuclear medicine examination. Using a validated questionnaire, we collected patient-reported information on adverse events that occurred immediately after administration of the radiopharmaceutical as well as those that occurred later. Adverse events were analysed, coded and assessed for causality by two independent researchers.
Results
A total of 187 (18.7%) patients reported 379 adverse events. Most patient-reported adverse events of radiopharmaceuticals belonged to the ‘general disorder and administration site conditions’ (42.0%) and ‘nervous system disorders’ (16.9%) system organ classes. Of the patient-reported adverse events, 43.0% were possibly or probably causally related to radiopharmaceuticals. We found the frequency of patient-reported adverse drug reactions to diagnostic radiopharmaceuticals to be 2.8%. No important medical events were related to the administrations of diagnostic radiopharmaceuticals. Most adverse events (80.0%) occurred shortly after administration of the radiopharmaceutical and were resolved within a few hours. Some events (20.0%) emerged after patients had left the nuclear medicine department, took longer to resolve, and sometimes prompted the patient to consult a healthcare professional.
Conclusion
Adverse reactions to diagnostic radiopharmaceuticals can occur, and the frequency reported by patients was found to be 2.8%, which is higher than reported in the existing literature. We hope that the results of this study increase awareness of these adverse reactions among patients and healthcare professionals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The frequency of patient-reported adverse reactions to diagnostic radiopharmaceuticals was found to be 2.8%, which is higher than reported in the existing literature. |
Most patient-reported adverse events related to radiopharmaceuticals were ‘general disorder and administration site conditions’ and ‘nervous system disorders’. |
Most adverse events (80.0%) occurred shortly after administration of the radiopharmaceutical and were resolved within a few hours. |
1 Introduction
Radiopharmaceuticals are essential for medical imaging and therapy in nuclear medicine. Adverse events with the use of radiopharmaceuticals can occur, although it is assumed in literature that they are rare in comparison with other pharmaceuticals. This can be attributed to a low dose—mostly in the order of micrograms—and the absence of pharmacologic effects for most radiopharmaceuticals. Furthermore, radiopharmaceuticals are used infrequently in individual patients with a short duration of use, often only being administered once or a small number of times in a lifetime [1,2,3]. Several studies have been performed to determine the frequency of adverse events in radiopharmaceuticals. Recently, in a systematic review, we reported a median frequency of 1.63 adverse events per 100,000 administrations based on 22 studies of diagnostic radiopharmaceuticals [4]. However, most of these studies retrieved their data from voluntary reports of adverse events from hospitals or pharmacovigilance centres.
Due to underreporting, which is inherent to voluntary reporting, an underestimation of the true frequency of adverse events in radiopharmaceuticals may occur [4,5,6]. Reasons for the underreporting of adverse events have been well described for other drugs and include aspects such as the reporter’s lack of time, unclear causal relationship with the drug, uncertainty about the way to report, and inadequate awareness of the benefits of reporting [7, 8]. Adverse events that occur after the use of radiopharmaceuticals may also remain undetected because such events may occur after the patient has left the nuclear medicine department and there is usually no follow-up contact between this department and the patient.
Besides reports by healthcare professionals, patients themselves are a valuable source of information and there is a growing interest in patient-reported data concerning adverse events [9, 10]. In comparison with healthcare professionals, patients tend to report different adverse events, including those that were previously unknown, and they also provide detailed accounts of known adverse events, including adverse changes in quality of life [11,12,13,14,15]. Furthermore, patients are able to disclose adverse events that occur with a later onset, which is useful to detect adverse events that occur after the patient has left the nuclear medicine department. Nevertheless, studies on the adverse events of radiopharmaceuticals from the perspective of the patient are scarce. To the best of our knowledge, only one study has assessed adverse events in radiopharmaceuticals from the perspective of the patient and described one patient who reported mild adverse events among 55 patients who received [99mTc]Tc-medronic acid [16].
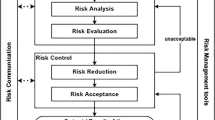
Knowledge about the true frequency of the occurrence of adverse events associated with the use of radiopharmaceuticals is limited but is needed to enable healthcare professionals to detect, understand, and manage the adverse events of radiopharmaceuticals efficiently. The current way of collecting safety data may provide us with information on possible safety signals but cannot provide more detailed knowledge of the frequency and impact on the patient of the adverse events of radiopharmaceuticals. For this reason, we recently developed, validated, and tested a questionnaire specifically designed to assess the adverse events of radiopharmaceuticals from the perspective of the patient [17]. This validated questionnaire was used to perform a study on a large group of patients who underwent a nuclear medicine examination, focusing especially on adverse events from the perspective of the patients.
The aim of this study was to (a) determine the type, causality, and frequency of patient-reported adverse events of radiopharmaceuticals and to (b) assess the onset, outcome, and follow-up of these adverse events from the patient’s perspective. Additionally, we compared the characteristics of the group that did not report adverse events with the group that did.
2 Methods
2.1 Study Design
We performed a prospective cohort study in patients undergoing a nuclear medicine examination at the Isala Hospital in Zwolle, a 1103-bed regional hospital in the Netherlands. Data were collected from November 2016 to November 2018. We obtained ethical exemption in writing from the Medical Ethics Committee of the Isala Hospital in Zwolle in the Netherlands (Reference number 16.08138), as this study did not require formal approval according to Dutch law. All patients gave their approval for the use of their data for this evaluation in agreement with Dutch privacy laws.
2.2 Patients
We invited patients who were scheduled for a nuclear medicine examination at the Isala Hospital to participate in this study. Patients received information by letter about the study 2 weeks before their visit to the nuclear medicine department. We informed patients in general terms that we intended to study their experience with the nuclear medicine examination, and we did not explicitly state the aim of the questionnaire. This approach will limit a social desirability bias, whereby patients would report adverse events in the direction of the perceived aim of the study. Patients could volunteer to participate on the day of their visit to the nuclear medicine department before their examination, and we did not ask patients about their reasons for not participating to avoid placing an additional burden on patients and staff. There were no non-participating patients who still participated after their examination. Patients who underwent a nuclear medicine examination and gave their signed approval for the use of their data for this study were included. Patients were excluded when data were missing that were required to initiate the web-based questionnaire, such as email address or date of birth, or when no radiopharmaceutical was used.
2.3 Data Collection
We used the questionnaire that we had developed, validated, and tested in our previous work [17]. The questionnaire in Dutch and an English translation can be found as supplementary material in the Electronic Supplement Material (ESM). Participants in the present study received a link to the web-based questionnaire (Researchmanager®; [18]) 7 days after their nuclear medicine examination. We sent a reminder after another 7 days in case patients had not completed the questionnaire, but access to the questionnaire was limited to 21 days after the nuclear medicine examination. These timespans were chosen for two reasons. First, we would expect possible adverse events to occur within a few days after the nuclear medicine examination. Second, longer recall periods may introduce bias due to patients forgetting information or patients bringing up information from other sequential doctor visits or examinations [4, 17]. In the questionnaire, we collected data from the patients about several aspects of their characteristics, health status, and occurrence of adverse events at several moments, as well as additional aspects when patients reported an adverse event (Table 1). We did not collect specific patient identifiers (such as their name and contact details) and there was also no need to contact patients for further clarification of the data collected. For each patient we added to the data the name of the radiopharmaceutical used and the radioactivity (in megabecquerel) obtained from the medical record system (Eridanos version 7.78, IC2it).
2.4 Data Classification
After obtaining the data with the questionnaire, we standardised the names of the radiopharmaceuticals according to the Anatomical Therapeutic Chemical (ATC) classification system [21] and applying the International Consensus Radiochemistry Nomenclature Guidelines [22]. Adverse events reported by patients were manually coded using terminology from the Medical Dictionary for Regulatory Activities (MedDRA®) version 21.1 [23]. MedDRA® is the international medical terminology developed under the auspices of the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH). This terminology contains terms on five hierarchical levels: lowest level terms, preferred terms, high-level terms, high-level group terms, and system organ classes. The lowest level terms are connected in meaning to preferred terms, which represent unique medical concepts and can, therefore, be used for data representation. Although the preferred terms can be connected in meaning to multiple system organ classes, a primary system organ class is always allocated to the preferred term in the MedDRA® terminology. In our study, we used both the preferred terms and the corresponding primary system organ classes in our coding. With respect to the type of adverse events, we also screened for important medical events using the important medical event terms list drafted by the EudraVigilance Expert Working Group [24]. This list contains the preferred terms that are considered to be important by the European Medicines Agency, which comprise occurrences that may result in death, that are life-threating, require hospitalisation, result in disability, or are congenital defects. In other words, important medical events are those that may jeopardise the patient or require intervention to prevent a serious adverse event [25].
To assess the causal relationship between the radiopharmaceuticals and the adverse events, we used the algorithm of Silberstein [3], which was specifically developed to determine the likelihood of whether an adverse event is related to a radiopharmaceutical. Silberstein’s algorithm comprises four categories of causality: not related, unlikely, possible, and probable. Each category has several criteria based on aspects such as time sequence, response pattern to the suspected test material, and rechallenge. For the causality assessment, we used data obtained through the questionnaire on adverse events’ time of onset, the occurrence of adverse events during previous nuclear medicine examinations, the recovery status of the patient, and other possible causes of adverse events, such as the administration of interventional agents or as indicated by the patient. To determine whether previous conclusive reports had been made about the reported event or whether it was a known response pattern, we used data from our previously published systematic review of the literature [4] and the summaries of product characteristics (SmPCs).
To ensure clarity, adverse events with a possible or probable proven relationship (as determined with the algorithm of Silberstein) were further defined as adverse drug reactions (ADRs) as specified by the World Health Organization (WHO): “a response to a drug which is noxious and unintended, and which occurs at doses normally used in man for the prophylaxis, diagnosis, or therapy of disease, or for the modification of physiological function” [26, 27].
Two researchers (N.J. and N.S.) independently conducted extraction, coding into MedDRA® terms, screening for important medical events, and causality assessment. When the syntheses of the results were not in agreement, the results were discussed with a third researcher (E.v.P.) to resolve discrepancies.
2.5 Data Analysis
We used SPSS Statistics version 26 (IBM) to compare the characteristics of the group that did not report adverse events with those of the group that did. We determined the normality of the continuous data using the Shapiro–Wilk test in combination with the normal Q–Q plots. When normally distributed, data were compared using the independent t test, or when they were not normally distributed, the Mann–Whitney U test was used. For the nominal data of the characteristics, we used the Chi square test or Fisher’s exact test when the numbers were small. For all analyses, p values of < 0.05 were considered to be statistically significant. The other results were analysed descriptively using Microsoft Excel version 1808.
3 Results
3.1 Patient Characteristics
Out of the total 5497 patients invited, 1535 (27.9%) patients were considered for inclusion in this study. After excluding patients with no email address (n = 74), patients who were not retrieved from the medical record system (n = 3), and patients with a missing date of birth (n = 1), we sent out questionnaires to 1457 patients. Of these patients, 1147 (78.7%) completed the questionnaire. We excluded 145 patients as they did not use a radiopharmaceutical; some scans at the nuclear medicine department only made use of the computed tomography (CT) modality of the scanning equipment. This resulted in 1002 patients with questionnaires that were included (Fig. 1). The median age of the group of patients was 66 years (IQR 57–72), with men (52.7%) and women (47.3%) almost equally represented (Table 2). The most commonly used radiopharmaceuticals were [99mTc]Tc-oxidronic acid (n = 307, 30.6%), [99mTc]Tc-tetrofosmin (n = 253, 25.3%), [18F]fludeoxyglucose (n = 159, 15.9%) and [82Rb]Rb-chloride (n = 119, 11.9%; Table 3).
3.2 Patient-Reported Adverse Events
Of the 1002 patients surveyed, 187 (18.7%) reported 379 adverse events, with an average of 2.0 adverse events per patient. In the group that reported adverse events, there were significantly more women (55.1% versus 45.5%; p = 0.018), patients were younger (62 years old versus 66 years old; p = 0.005), had a higher BMI (27.1 kg/m2 versus 26.5 kg/m2; p = 0.042), and indicated more often that they had not had a nuclear medicine examination in the past (62.2% versus 46.9%; p = 0.001) than in the group that did not report adverse events. None of the other characteristics of the patients differed between the two groups (Table 2).
Of the patients who reported adverse events, 153 reported that 303 (80.0%) adverse events occurred shortly after the administration of the radiopharmaceutical and 51 patients reported that 76 (20.0%) adverse events occurred within 1 week after leaving the nuclear medicine department. We found that 58.9% of the patient-reported adverse events were related to two system organ classes (Fig. 2): ‘general disorders and administration site conditions’ (42.0%) and ‘nervous system disorders’ (16.9%). The five most frequently reported adverse events were a hot feeling (n = 47), a sense of oppressed breathing (n = 26), chest discomfort (n = 24), headache (n = 20) and fatigue (n = 18).
Of the patient-reported adverse events, 163 (43.0%) in 96 patients were determined to be possibly (n = 123; 32.5%) or probably (n = 40; 10.6%) causally related and further determined as adverse drug reactions. Another 216 (57.0%) patient-reported adverse events in 91 patients were determined to be unrelated (n = 177; 46.7%) or unlikely to be related (n = 39; 10.3%; Table 3). Of the 163 patient-reported adverse drug reactions, 11 adverse drug reactions in four patients were related to two therapeutic radiopharmaceuticals ([223Ra]Ra-dichloride and [131I]sodium iodine) and 152 adverse drug reactions in 92 patients were related to diagnostic radiopharmaceuticals (Table 3). Of patients injected with [99mTc]Tc-tetrofosmin, 119 adverse drug reactions in 71 patients were attributed to adenosine, which is used as a stressing agent with myocardial perfusion imaging [28]. Of these 71 patients, seven patients reported both adverse drug reactions mentioned in the SmPC of adenosine and those not mentioned in the SmPC of adenosine. After excluding patients with adverse drug reactions that were related to adenosine, the frequency of patients with adverse drug reactions related to diagnostic radiopharmaceuticals became 2.8% (28/993; Table 3).
The diagnostic radiopharmaceuticals that were most frequently associated with patient-reported adverse drug reactions were [99mTc]Tc-tetrofosmin and [99mTc]Tc-oxidronic acid (Table 3). A detailed overview of adverse drug reactions in which standardised terminology according to MedDRA® is used for all radiopharmaceuticals can be found in Table 4. Two reactions in two patients were considered to be important medical events. These two events were respiratory distress with myocardial perfusion imaging using [99mTc]Tc-tetrofosmin and adenosine, and were considered to be related to the use of adenosine. Both of these patients reported this to the hospital staff. One of the patients was reassured by the hospital staff and was given instructions for relaxation. He recovered within 2 min. The other patient indicated that she was not treated by the hospital staff and recovered within 10 min. When excluding these two patients with an important medical event related to adenosine, no important medical events were related to the administration of diagnostic radiopharmaceuticals (0.0%; 0/993).
3.3 Onset, Outcome and Follow-Up of Adverse Events From the Patient’s Perspective
Among the patients who reported an adverse event that occurred after the administration of the radiopharmaceuticals, 143 patients reported that the onset of the adverse event was shortly after administration with a median time of 1 min after administration (interquartile range [IQR]: 0.1–5 min). Of the group of patients who reported an adverse event that occurred after the administration of the radiopharmaceuticals, 138 (90.2%) made a full recovery and the median time to recover was 15 min (IQR: 2–120 min). Twelve patients (7.8%) indicated that they partly recovered and three patients (2.0%) had not yet recovered at the time of the last notification of their status. The adverse events of the patients who reported not to have recovered were found to be unrelated or unlikely to be related to the radiopharmaceutical. The patients reported the adverse events to the hospital staff in 77.1% of cases and indicated that in 8.5% of the cases, they received treatment (Table 5).
Of the patients who reported an adverse event that occurred within 1 week after leaving the nuclear medicine department, 48 reported an onset of adverse events at a median time of 22 h (IQR: 4–39) after administration. Of the group of patients who reported an adverse event that occurred within 1 week after leaving the nuclear medicine department, 60.8% made a full recovery and the median time to recover was 2 days (IQR: 1–3 days). Twelve patients (23.5%) indicated that they had partly recovered and eight patients (15.7%) indicated that they had not yet recovered at the time of the last notification of their status. In four of the eight patients who had not recovered, the adverse events were found to be possibly or probably related to the radiopharmaceutical. One patient indicated at the time of the last notification that he still experienced diarrhoea and fatigue after the administration of [223Ra]Ra-dichloride. One patient still suffered from musculoskeletal chest pain, listlessness, fatigue, and headache after the administration of [223Ra]Ra-dichloride. One patient still had urticaria and pruritus after the administration of [99mTc]Tc-tetrofosmin. Finally, one patient still suffered from malaise, nausea, and a cold feeling after the administration of [123I]sodium iodine. Other adverse events in patients who reported to have not recovered were found to be unlikely to be related or unrelated to the radiopharmaceutical. A majority of 72.5% of the patients did not contact a healthcare professional about the adverse event, and those who did mostly contacted the referring physician of the hospital or their general practitioner. Of all patients reporting an adverse event that occurred within 1 week after leaving the nuclear medicine department, five patients (9.8%) indicated that they had been treated (Table 5).
4 Discussion
In this study, we found that most patient-reported adverse events of radiopharmaceuticals belonged to the ‘general disorder and administration site conditions’ and ‘nervous system disorders’ system organ classes. Of the patient-reported adverse events, 43.0% were possibly or probably causally related to the radiopharmaceuticals. We found a frequency of patient-reported adverse drug reactions to diagnostic radiopharmaceuticals of 2.8%. No important medical events related to the administration of diagnostic radiopharmaceuticals were reported, although two important medical events were attributed to the use of adenosine in myocardial perfusion imaging. Most adverse events (80.0%) of radiopharmaceuticals occurred shortly after the administration of the radiopharmaceutical, and most of these patients recovered (90.2%) quickly with a median time of 15 min (interquartile range [IQR]: 2–120 min).
We found the frequency of patient-reported adverse drug reactions to diagnostic radiopharmaceuticals to be much higher than the median frequency of 0.0016% that we identified in our literature review [4], but it seems to correspond with one small study that assessed patient-reported adverse events in 55 patients who received the radiopharmaceutical [99mTc]Tc-medronic acid, in which a frequency of 1.8% was reported [16]. Our findings suggest underreporting of adverse events of radiopharmaceuticals in the literature. Such underreporting of adverse events is well known for other drugs, where a median underreporting rate as high as 94% has been identified [7]. Further research could determine the reasons for the underreporting of adverse events of radiopharmaceuticals and may identify possible areas for improvement in reporting.
The proportion of serious adverse drug reactions that we found in this study was lower than in our previously published systematic review of the literature [4]. Furthermore, there was a difference in the type of adverse events reported. Most of the reported adverse events in our study were ‘general disorders and administration site conditions’ (e.g., a hot feeling, a sense of oppressed breathing, chest discomfort, and fatigue), and ‘nervous system disorders’ (e.g., headache), while in our previously published systematic review of the literature, we found that most reported adverse events were ‘skin and subcutaneous tissue disorders’ (e.g., rash and pruritus), and ‘general disorders and administration site conditions’ (e.g., fever; [4]). From these results, it seems that patients tend to report different adverse events to healthcare professionals, which is in line with studies of other drugs [29].
This study focused on adverse events from the perspective of the patient. We are not aware of other large studies with this focus. Regarding the follow-up of adverse events, patients who experienced an adverse event of a radiopharmaceutical shortly after administration reported this event to the hospital staff in most cases (77.1%). This result is as expected, as patients are under close surveillance by the hospital staff at the nuclear medicine department, such as nuclear medicine technologists. As the hospital staff are likely the first to register an adverse event, they must be aware of this and be prepared to manage such events. Patients who experience an adverse event of a radiopharmaceutical after leaving the nuclear medicine department do not usually contact the nuclear medicine staff but may report to their family physician or other.
We believe that our study contributes to the area of drug safety of radiopharmaceuticals, in which little research has been conducted. The strengths of our study are that we used a validated and tested questionnaire, as well as a large group of patients. Besides the frequency and type of patient-reported adverse events of radiopharmaceuticals, we studied the outcome and follow-up of these adverse events from the perspective of the patient, which, according to our knowledge, has not been studied before.
A point of attention is that in this study, we focused specifically on adverse events from the perspective of the patient. Although we used a validated and tested questionnaire, one can argue that patients may not be regarded as able to discriminate effectivity between symptoms attributed to the radiopharmaceutical, the disease, or the nuclear medicine examination. Nevertheless, the results of our study are of value to healthcare professionals, as they illustrate the way that patients experience radiopharmaceuticals. Other studies have shown that patients are interested in their own illnesses and treatment and that both they and healthcare professionals report adverse events. Importantly, patient reporting of adverse events does not replace the information obtained from the healthcare professional but is a useful complement [30,31,32]. Indeed, the results of our study demonstrate that patients report different adverse events and provide more detail on their experiences with these events in comparison with healthcare professionals.
A general limitation of studies using a questionnaire is the representativeness of the responders. Even though 1002 patients participated in this study, this was 18.2% of the 5497 patients approached. A potential for selection bias may exist and limits the applicability to a larger population. However, the age, gender ratio, and distribution of different types of nuclear medicine procedures of our population corresponds with the Dutch population undergoing a nuclear medicine examination as presented in two older studies [33, 34]. Furthermore, sending the questionnaire 7 days after the nuclear medicine examination may have led to underreporting or overreporting of adverse events or have affected the accuracy of reporting due to possible recall bias. Another limitation of this study is that we could not validate the exact times of the onset and recovery of the patients. The values presented in Table 5 are times according to the perception of the patients and might not correspond with actual times. However, these times were adequate to perform the causality assessment. Another study might include a quantitative approach to measure actual times. In addition, although we calculated a frequency, we did not control for confounding. Creating a control group could have been an option but this would have involved difficult practical and ethical aspects.
Using Silberstein’s algorithm together with the data that we obtained with the questionnaire, we were able to successfully conduct the causality assessment and establish that 43% of the patient-reported adverse events were possibly or probably related to radiopharmaceuticals. However, the assessment with Silberstein’s algorithm has two potential limitations that must be considered. One limitation is that only adverse events with a known response pattern are classified as possibly or probably related, leading to an exclusion of new adverse events. A sub-analysis of our data revealed that the classification would change from unlikely related to possibly or probably related for only five adverse events (paraesthesia with [18F]fludeoxyglucose; chromaturia, thirst, and feeling cold with [99mTc]Tc-oxidronic acid; ageusia with [123I]sodium iodine), which we considered to be acceptable. Another limitation is the inability of the algorithm to distinguish between adverse events due to the radiopharmaceutical or interventional drugs, such as adenosine, in our study. Although we overcame this limitation in our study by excluding the adverse drug reactions attributed to adenosine, it may be necessary to update Silberstein’s algorithm when using it in future research. In general, one should note that establishing a causal relationship between a suspected drug and an adverse event is difficult and that although algorithms are often used in pharmacovigilance, these cannot replace a thorough medical examination of an individual case.
The findings of this study have several practical implications. Our results imply that adverse events of radiopharmaceuticals as experienced by patients are more common than previously assumed and that nuclear medicine staff are likely to be the first to be informed about a potential adverse event. It is, therefore, important that the nuclear medicine staff are aware of potential adverse events and are prepared to counsel, respond, and manage these events. Furthermore, we suggest that nuclear medicine staff consistently inform patients about the adverse events of radiopharmaceuticals. It has been supposed that well informed patients may handle side effects better or may be less concerned about them than uninformed patients [35]. Patients may be instructed what to do when they experience an adverse event after leaving the nuclear medicine department. One final practical implication is that other healthcare professionals, such as the referring physician of the hospital or a patient’s general practitioner, should be aware that symptoms reported by a patient might be caused by a nuclear medicine examination, as they may be contacted by patients who are experiencing adverse events.
5 Conclusion
We studied the patient-reported adverse events of radiopharmaceuticals and found that most were ‘general disorders and administration site conditions’ and ‘nervous system disorders’. The reported frequency of patient-reported adverse drug reactions to diagnostic radiopharmaceuticals was 2.8%, which is considerably higher than previously suggested. None of the adverse drug reactions related to the administration of a diagnostic radiopharmaceutical were considered to be an important medical event. Most events occurred shortly after the administration of the radiopharmaceutical and were resolved within a few hours, while 20% of the events occurred later, and these took longer to resolve. This study will hopefully increase awareness of adverse events to radiopharmaceuticals among patients and healthcare professionals.
References
Hesslewood SR, Keeling DH. Frequency of adverse reactions to radiopharmaceuticals in Europe. Eur J Nucl Med. 1997;24:1179–82.
Silberstein EB. Prevalence of adverse events to radiopharmaceuticals from 2007 to 2011. J Nucl Med. 2014;55:1308–10.
Silberstein EB, Ryan J. Prevalence of adverse reactions in nuclear medicine: pharmacopeia committee of the society of nuclear medicine. J Nucl Med. 1996;37:185–92.
Schreuder N, Koopman D, Jager PL, Kosterink JGW, van Puijenbroek EP. Adverse events of diagnostic radiopharmaceuticals: a systematic review. Sem Nucl Med. 2019;49:382–410.
Pinto SR, Santos LFC, Dos Reis SRR, Bastos MK, Gomes VDS, Vieira TO, et al. Adverse reactions to radiopharmaceuticals: a survey based on clinical cases using criteria of systematic review. Ther Innov Regul Sci. 2018;52:109–13.
Santos-Oliveira R, Machado M. Pitfalls with radiopharmaceuticals. Am J Med Sci. 2011;342:50–3.
Hazell L, Shakir SA. Under-reporting of adverse drug reactions: a systematic review. Drug Saf. 2006;29:385–96.
Stergiopoulos S, Brown CA, Felix T, Grampp G, Getz KA. A survey of adverse event reporting practices among US healthcare professionals. Drug Saf. 2016;39:1117–27.
Stefanovic S, Wallwiener M, Karic U, Domschke C, Katic L, Taran FA, et al. Patient-reported outcomes (PRO) focused on adverse events (PRO-AEs) in adjuvant and metastatic breast cancer: clinical and translational implications. Support Care Cancer. 2017;25:549–58.
Gandhi TK, Weingart SN, Borus J, Seger AC, Peterson J, Burdick E, et al. Adverse drug events in ambulatory care. N Engl J Med. 2003;348:1556–64.
Jarernsiripornkul N, Kakaew W, Loalukkana W, Krska J. Adverse drug reaction monitoring: comparing doctor and patient reporting for new drugs. Pharmacoepidemiol Drug Saf. 2009;18:240–5.
Blenkinsopp A, Wilkie P, Wang M, Routledge PA. Patient reporting of suspected adverse drug reactions: a review of published literature and international experience. Br J Clin Pharmacol. 2007;63:148–56.
van Grootheest K, de Graaf L, de Jong-van den Berg LT. Consumer adverse drug reaction reporting: a new step in pharmacovigilance. Drug Saf. 2003;26:211–7.
van den Bemt PM, Egberts AC, Lenderink AW, Verzijl JM, Simons KA, van der Pol WS, et al. Adverse drug events in hospitalized patients. A comparison of doctors, nurses and patients as sources of reports. Eur J Clin Pharmacol. 1999;55:155–8.
Finer D, Albinson J, Westin L, Dukes G. Consumer reports on medicines—CRM: policy and practice. Int J Risk Saf Med. 2000;13:117–27.
Dos Santos Almeida R, Mamede M, Santos-Oliveira R. Pharmacovigilance of radiopharmaceuticals used for prostate and breast cancer in Brazil. Adverse Drug React Bull. 2013;283:1091–4.
Schreuder N, de Hoog Q, de Vries ST, Jager PL, Kosterink JGW, van Puijenbroek EP. Patient-reported adverse events of radiopharmaceuticals: development and validation of a questionnaire. Drug Saf. 2020;43:319–28.
Researchmanager. https://my-researchmanager.com/en/home-2/ Accessed 04 Jan 2019.
Euroqol research foundation. EQ-5D Instruments. https://euroqol.org/. Accessed 4 July 2019.
The EuroQol Group. EuroQol-a new facility for the measurement of health related quality of life. Health Policy. 1990;16:199–208.
WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment 2020. 23rd ed. Oslo: World Health Organisation; 2019.
Coenen HH, Gee AD, Adam M, Antoni G, Cutler CS, Fujibayashi Y, et al. Open letter to journal editors on: international consensus radiochemistry nomenclature guidelines. EJNMMI Radiopharm Chem. 2019. https://doi.org/10.1186/s41181-018-0047-y.
MedDRA Browser (2016 version 2.0). https://www.meddra.org/ Accessed 06 Feb 2019.
European Medicines Agency. Important medical event terms list version 21.0. European Medicines Agency. 2018. https://www.ema.europa.eu/documents/other/important-medical-event-terms-list-version-210-ime-list_en.xls Accessed 06 Feb 2019.
European Medicines Agency. Inclusion/exclusion criteria for the “Important Medical Events” list. European Medicines Agency. 2019. http://www.ema.europa.eu/docs/en_GB/document_library/Other/2016/08/WC500212100.pdf. Accessed 25 Oct 2019.
World Health Organization. International Drug Monitoring, The Role of National Centres (Technical Report Series No. 498). Geneva: World Health Organisation; 1972.
World Health Organization. Safety of Medicines: a guide to detecting and reporting adverse drug reactions. World Health Organisation. 2002. whqlibdoc.who.int/hq/2002/WHO_EDM_QSM_2002.2.pdf, Accessed 25 Mar 2020.
Sanofi-Aventis Netherlands B.V. Adenocor—Summary of Product Characteristics (SPC). https://www.geneesmiddeleninformatiebank.nl/smpc/h16617_smpc.pdf. Accessed 25 Oct 2019.
Rolfes L, van Hunsel F, Wilkes S, van Grootheest K, van Puijenbroek E. Adverse drug reaction reports of patients and healthcare professionals-differences in reported information. Pharmacoepidemiol Drug Saf. 2015;24:152–8.
de Langen J, van Hunsel F, Passier A, de Jong-van den Berg L, van Grootheest K. Adverse drug reaction reporting by patients in the Netherlands: three years of experience. Drug Saf. 2008;31:515–24.
Rolfes L, van Hunsel F, van der Linden L, Taxis K, van Puijenbroek E. The Quality of Clinical Information in Adverse Drug Reaction Reports by Patients and Healthcare Professionals: a Retrospective Comparative Analysis. Drug Saf. 2017;40:607–14.
Inacio P, Cavaco A, Airaksinen M. The value of patient reporting to the pharmacovigilance system: a systematic review. Br J Clin Pharmacol. 2017;83:227–46.
Brugmans MJ, Buijs WC, Geleijns J, Lembrechts J. Population exposure to diagnostic use of ionizing radiation in The Netherlands. Health Phys. 2002;82(4):500–9.
Beentjes LB, Timmermans CW. Age and sex specific population doses (SED (somatic effective dose equivalent) and GSD (genetically significant dose equivalent)) due to nuclear medicine procedures in The Netherlands. Int J Rad Appl Instrum B. 1990;17(3):261–8.
Gandhi TK, Burstin HR, Cook EF, Puopolo AL, Haas JS, Brennan TA, et al. Drug complications in outpatients. J Gen Intern Med. 2000;15:149–54.
Acknowledgements
The authors would like to thank pharmacist Helin Tang for her help with the data collection. The authors would like to thank the EuroQol group for permitting them to use the EQ-5D instrument. Acknowledgement statement: The MedDRA® trademark is owned by the International Federation of Pharmaceutical Manufacturers and Associations on behalf of ICH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No financial support was received for the conduct of this study or preparation of this manuscript.
Conflict of interest
Nanno Schreuder is employed by GE Healthcare, however this work was part of his PhD trajectory at the University of Groningen. Niels A. Jacobs, Pieter L. Jager, Jos G.W. Kosterink, and Eugène P. van Puijenbroek have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Ethical exemption in writing was obtained from the Medical Ethics Committee of the Isala Hospital in Zwolle in the Netherlands (Reference number 16.08138), as this study did not require formal approval according to Dutch law.
Consent to participate
All patients gave their approval for the use of their data, in agreement with Dutch privacy laws.
Consent for publication
Not applicable.
Availability of data and material
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
Authors’ contributions
All authors contributed to the study conception and design. Data collection and analysis was performed by Nanno Schreuder and Niels A. Jacobs. The first draft of the manuscript was written by Nanno Schreuder and Niels A. Jacobs and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Schreuder, N., Jacobs, N.A., Jager, P.L. et al. Patient-Reported Adverse Events of Radiopharmaceuticals: A Prospective Study of 1002 Patients. Drug Saf 44, 211–222 (2021). https://doi.org/10.1007/s40264-020-01006-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-020-01006-2