Abstract
Introduction
Macrolides are widely used during pregnancy; however, their fetal safety remains uncertain. We performed a meta-analysis to assess the relation between prenatal exposure to macrolides and occurrence of congenital malformations.
Methods
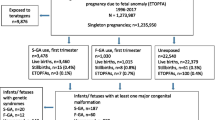
We searched MEDLINE, EMBASE, and other databases until June 12, 2019. We assessed the quality of the studies and checked for heterogeneity and publication bias. We performed three different analyses and compared the effect of macrolides with each of the following unexposed populations: Group 1: babies unexposed to any medicine before birth, Group 2: babies exposed to non-macrolide antibiotics/non-teratogens, and Group 3: mixed population of the first and second comparators.
Results
A weak association between macrolides and congenital malformation of any type was observed when macrolides were compared with the mixed population (ORgroup 3 1.06 [95% CI 1.01–1.10]). Subgroup analysis showed that this weak association is restricted to fetus exposure in the first trimester of pregnancy (OR 1.06 [95% CI 1.01–1.11]) and to cohort studies (OR 1.07 [95% CI 1.02–1.13]). Digestive system malformations were found to be slightly associated with prenatal exposure to macrolides (ORgroup 3 1.14 [95% CI 1.02–1.26]). The musculoskeletal system was also found to be potentially affected (ORgroup 2 1.21 [95% CI 1.08–1.35] and ORgroup 3 1.15 [95% CI 1.05–1.26]). European studies showed a slightly stronger association than American studies in these two comparisons.
Conclusions
Our study suggests a weak association between prenatal use of macrolides and congenital malformations, limited to exposure in early pregnancy, and musculoskeletal and digestive systems. In addition to studies with a larger control of confounding, risk–benefit research is needed to determine the usefulness of macrolides during pregnancy.



Similar content being viewed by others
References
World Health Organization. Congenital anomalies. World Health Organization. 2016. http://www.who.int/mediacentre/factsheets/fs370/en/. Accessed 19 Feb 2019.
Centers for Disease Control and Prevention. Birth Defects 2018. https://www.cdc.gov/ncbddd/birthdefects/facts.html. Accessed 19 Feb 2019.
Petrini J, Damus K, Russell R, Poschman K, Davidoff MJ, Mattison D. Contribution of birth defects to infant mortality in the United States. Teratology. 2002;66(Suppl 1):S3–6. https://doi.org/10.1002/tera.90002.
Kochanek KD, Murphy SL, Xu JQ, Arias E. Mortality in the United States, 2016. NCHS Data Brief. 2017. Report No.: 293.
Janz T, Navaneelan T, Pearson C. Deaths from congenital anomalies in Canada, 1974 to 2012. Health at a Glance. Statistics Canada. 2016. Catalogue No.: 82-624-X.
Christianson A, Howson CP, Modell B. Global report on birth defects. The hidden toll of dying and disabled children. White Plains (NY): March of Dimes Birth Defects Foundation. 2006. https://www.marchofdimes.org/global-report-on-birth-defects-the-hidden-toll-of-dying-and-disabled-children-full-report.pdf. Accessed 02 Apr 2019.
Adam MP, Polifka JE, Friedman JM. Evolving knowledge of the teratogenicity of medications in human pregnancy. Am J Med Genet C Semin Med Genet. 2011;157C(3):175–82. https://doi.org/10.1002/ajmg.c.30313.
Bookstaver PB, Bland CM, Griffin B, Stover KR, Eiland LS, McLaughlin M. A review of antibiotic use in pregnancy. Pharmacotherapy. 2015;35(11):1052–62. https://doi.org/10.1002/phar.1649.
Crider KS, Cleves MA, Reefhuis J, Berry RJ, Hobbs CA, Hu DJ. Antibacterial medication use during pregnancy and risk of birth defects: national birth defects prevention study. Arch Pediatr Adolesc Med. 2009;163(11):978–85. https://doi.org/10.1001/archpediatrics.2009.188.
Brauer R, Ruigómez A, Downey G, Bate A, Rodriguez LAG, Huerta C, et al. Prevalence of antibiotic use: a comparison across various European health care data sources. Pharmacoepidemiol Drug Saf. 2016;25(sup 1):11–20. https://doi.org/10.1002/pds.3831.
Lin KJ, Mitchell AA, Yau WP, Louik C, Hernandez-Diaz S. Safety of macrolides during pregnancy. Am J Obstet Gynecol. 2013;208(3):221. https://doi.org/10.1016/j.ajog.2012.12.023.
Santos F, Sheehy O, Perreault S, Ferreira E, Berard A. Trends in anti-infective drugs use in pregnancy. J Popul Ther Clin Pharmacol. 2012;19(3):e460–5.
Kallen BA, Otterblad Olausson P, Danielsson BR. Is erythromycin therapy teratogenic in humans? Reprod Toxicol. 2005;20(2):209–14. https://doi.org/10.1016/j.reprotox.2005.01.010.
Lund M, Pasternak B, Davidsen RB, Feenstra B, Krogh C, Diaz LJ, et al. Use of macrolides in mother and child and risk of infantile hypertrophic pyloric stenosis: nationwide cohort study. BMJ. 2014;348:g1908. https://doi.org/10.1136/bmj.g1908.
Dinur AB, Koren G, Matok I, Wiznitzer A, Uziel E, Gorodischer R, et al. Fetal safety of macrolides. Antimicrob Agents Chemother. 2013;57(7):3307–11. https://doi.org/10.1128/AAC.01691-12.
Andersen JT, Petersen M, Jimenez-Solem E, Broedbaek K, Andersen NL, Torp-Pedersen C, et al. Clarithromycin in early pregnancy and the risk of miscarriage and malformation: a register based nationwide cohort study. PLoS One. 2013;8(1):e53327. https://doi.org/10.1371/journal.pone.0053327.
Fan H, Li L, Wijlaars L, Gilbert RE. Associations between use of macrolide antibiotics during pregnancy and adverse child outcomes: a systematic review and meta-analysis. PLoS One. 2019;14(2):e0212212. https://doi.org/10.1371/journal.pone.0212212.
Prospero International Prospective Register of Systematic Reviews. 2017. https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=55131.
Wells GA, Shea B, O’Connell D, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 19 Feb 2019.
Rothman KJ, Greenland S, Lash TL. Measure of effect and measures of association. Modern epidemiology. 3rd ed. Philadelphia: Lippincott, Williams and Wilkins; 2008. p. 61.
Takkouche B, Cadarso-Suárez C, Spiegelman D. Evaluation of old and new tests of heterogeneity in epidemiologic meta-analysis. Am J Epidemiol. 1999;150(2):206–15.
Kallen B, Danielsson BR. Fetal safety of erythromycin. An update of Swedish data. Eur J Clin Pharmacol. 2014;70(3):355–60. https://doi.org/10.1007/s00228-013-1624-3.
Mahon BE, Rosenman MB, Kleiman MB. Maternal and infant use of erythromycin and other macrolide antibiotics as risk factors for infantile hypertrophic pyloric stenosis. J Pediatr. 2001;139(3):380–4. https://doi.org/10.1067/mpd.2001.117577.
Wolfgang P, Schloemp S, Sterzik K, Stoz F, editors. Does roxithromycin affect embryo development? 33rd Annual Conference of the European Teratology Society; 3–7 Sep, 2005; Haarlem, The Netherlands: Reproductive Toxicology.
Lê Nguyên T, Araujo M, Hurault-Delarue C, Lacroix I, Damase-Michel C, Sommet A. Teratogenic risk of macrolides during the first trimester of pregnancy: a study with two complementary approaches within the EFEMERIS database. Clin Ther. 2017;39(8):e11–2.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Costa-Bouzas J, Takkouche B, Cadarso-Suárez C, Spiegelman D. HEpiMA: software for the identification of heterogeneity in meta-analysis. Comput Methods Programs Biomed. 2001;64:101–7.
Bar-Oz B, Weber-Schoendorfer C, Berlin M, Clementi M, Di Gianantonio E, de Vries L, et al. The outcomes of pregnancy in women exposed to the new macrolides in the first trimester: a prospective, multicentre, observational study. Drug Saf. 2012;35(7):589–98. https://doi.org/10.2165/11630920-000000000-00000.
Romoren M, Lindbaek M, Nordeng H. Pregnancy outcome after gestational exposure to erythromycin—a population-based register study from Norway. Br J Clin Pharmacol. 2012;74(6):1053–62. https://doi.org/10.1111/j.1365-2125.2012.04286.x.
Cooper WO, Hernandez-Diaz S, Arbogast PG, Dudley JA, Dyer SM, Gideon PS, et al. Antibiotics potentially used in response to bioterrorism and the risk of major congenital malformations. Paediatr Perinat Epidemiol. 2009;23(1):18–28. https://doi.org/10.1111/j.1365-3016.2008.00978.x.
Bar-Oz B, Diav-Citrin O, Shechtman S, Tellem R, Arnon J, Francetic I, et al. Pregnancy outcome after gestational exposure to the new macrolides: a prospective multi-center observational study. Eur J Obstet Gynecol Reprod Biol. 2008;141(1):31–4. https://doi.org/10.1016/j.ejogrb.2008.07.008.
Chun JY, Han JY, Ahn HK, Choi JS, Koong MK, Nava-Ocampo AA, et al. Fetal outcome following roxithromycin exposure in early pregnancy. J Matern Fetal Neonatal Med. 2006;19(3):189–92. https://doi.org/10.1080/14767050500439657.
Sarkar M, Woodland C, Koren G, Einarson AR. Pregnancy outcome following gestational exposure to azithromycin. BMC Pregnancy Childbirth. 2006;6:18. https://doi.org/10.1186/1471-2393-6-18.
Einarson A, Phillips E, Mawji F, D’Alimonte D, Schick B, Addis A, et al. A prospective controlled multicentre study of clarithromycin in pregnancy. Am J Perinatol. 1998;15(9):523–5. https://doi.org/10.1055/s-2007-994053.
Cooper WO, Griffin MR, Arbogast P, Hickson GB, Gautam S, Ray WA. Very early exposure to erythromycin and infantile hypertrophic pyloric stenosis. Arch Pediatr Adolesc Med. 2002;156(7):647–50. https://doi.org/10.1001/archpedi.156.7.647.
Wilton LV, Pearce GL, Martin RM, Mackay FJ, Mann RD. The outcomes of pregnancy in women exposed to newly marketed drugs in general practice in England. Br J Obstet Gynaecol. 1998;105(8):882–9.
Muanda FT, Sheehy O, Berard A. Use of antibiotics during pregnancy and the risk of major congenital malformations: a population based cohort study. Br J Clin Pharmacol. 2017;83(11):2557–71. https://doi.org/10.1111/bcp.13364.
Czeizel AE, Rockenbauer M, Olsen J, Sorensen HT. A case–control teratological study of spiramycin, roxithromycin, oleandomycin and josamycin. Acta Obstet Gynecol Scand. 2000;79(3):234–7.
Louik C, Werler MM, Mitchell AA. Erythromycin use during pregnancy in relation to pyloric stenosis. Am J Obstet Gynecol. 2002;186(2):288–90. https://doi.org/10.1067/mob.2002.119718.
Czeizel AE, Rockenbauer M, Sorensen HT, Olsen J. A population-based case–control teratologic study of oral erythromycin treatment during pregnancy. Reprod Toxicol. 1999;13(6):531–6. https://doi.org/10.1016/s0890-6238(99)00046-5.
Bulska M, Szcześniak P, Pięta-Dolińska A, Oszukowski P, Orszulak-Michalak D. The placental transfer of erythromycin in human pregnancies with group B streptococcal infection. Ginekol Pol. 2015;86(1):33–9.
Danielsson BR, Skold AC, Azarbayjani F. Class III antiarrhythmics and phenytoin: teratogenicity due to embryonic cardiac dysrhythmia and reoxygenation damage. Curr Pharm Des. 2001;7(9):787–802.
Gorelik E, Masarwa R, Perlman A, Rotshild V, Muszkat M, Matok I. Systematic review, meta-analysis, and network meta-analysis of the cardiovascular safety of macrolides. Antimicrob Agents Chemother. 2018;62(6):89. https://doi.org/10.1128/AAC.00438-18.
Canfield MA, Mai CT, Wang Y, O’Halloran A, Marengo LK, Olney RS, et al. The association between race/ethnicity and major birth defects in the United States, 1999–2007. Am J Public Health. 2014;104(9):e14–23. https://doi.org/10.2105/AJPH.2014.302098.
Goossens H. Antibiotic consumption and link to resistance. Clin Microbiol Infect. 2009;15:12–5. https://doi.org/10.1111/j.1469-0691.2009.02725.x.
Hollier LM, Leveno KJ, Kelly MA, MCIntire DD, Cunningham FG. Maternal age and malformations in singleton births. Obstet Gynecol. 2000;96(5 Pt 1):701–6. https://doi.org/10.1016/s0029-7844(00)01019-x.
Author information
Authors and Affiliations
Contributions
Conception and design of the study: BT and ME; Conceptualization of the manuscript and review and synthesis of the literature: NM; Data extraction: NM and HT; Coordination and supervision of data extraction and analysis: BT and AF; All authors made substantial contribution to the interpretation of data, critically reviewed the manuscript, and approved its submission for publication.
Corresponding author
Ethics declarations
Funding Source
No specific funding for this work. Dr. Takkouche’s and Dr. Figueiras’ work is funded by a Grant from the Regional Ministry of Education, Universities and Vocational Training, Santiago de Compostela, Spain, ED431C 2018/20.
Conflict of interest
Narmeen Mallah, Hamid Reza Tohidinik, Mahyar Etminan, Adolfo Figueiras, and Bahi Takkouche declare that they have no conflict of interest.
Data Sharing
All data generated or analyzed during this study are included in this published article and its Supplementary Information File (Online Resource 1, see ESM).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mallah, N., Tohidinik, H.R., Etminan, M. et al. Prenatal Exposure to Macrolides and Risk of Congenital Malformations: A Meta-Analysis. Drug Saf 43, 211–221 (2020). https://doi.org/10.1007/s40264-019-00884-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-019-00884-5