Abstract
Introduction/Objectives
An association between potentially inappropriate medication (PIM) use and adverse events has been established. However, PIM criteria for elderly patients and medical circumstance vary in different countries. We investigated the association between PIM use according to Japanese guidelines and unplanned hospitalization among elderly patients.
Design
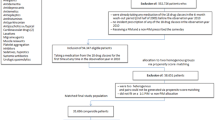
A case-crossover study was conducted.
Setting/Participants
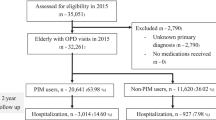
We used the Japanese Medical Data Vision database of 17.9 million people from 270 acute care hospitals across Japan. Records from 247,897 patients aged ≥ 65 years with unscheduled admissions between January 2009 and December 2015 were analyzed.
Measurements
We defined PIM use according to the Japanese Guidelines for Medical Treatment and Its Safety in the Elderly and used conditional logistic regression analysis to fit self-matched case-crossover models and compared each patient’s PIM use over five case periods (1, 2, 4, 8, and 12 weeks) prior to each unplanned hospitalization.
Results
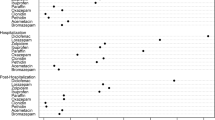
We found the highest odds ratios (ORs) of unscheduled admission related to PIM use in the 1-week case period [OR 4.15; 95% confidence interval (CI) 4.05–4.25], followed by the 2-week (OR 3.01; 95% CI 2.95–3.07), 4-week (OR 3.91; 95% CI 3.83–4.00), 8-week (OR 2.00; 95% CI 1.96–2.05), and 12-week case periods (OR 1.48; 95% CI 1.44–1.51).
Conclusions
Elderly patients commonly used PIMs, especially antidiabetics and diuretics. PIM use was associated with a 1.5- to 4-fold increase in the ORs of unplanned hospitalization among them.
Similar content being viewed by others
References
Ministry of Health Law. Estimates of National Medical Care Expenditure, FY. 2014. http://www.mhlw.go.jp/toukei/saikin/hw/k-iryohi/14/dl/kekka.pdf. Accessed 25 Jan 2017.
Bureau S. Population estimates by age (5 year age group) and Sex—August 1, 2016 (final estimates), January 1, 2017 (provisional estimates); 2018. http://www.e-stat.go.jp/SG1/estat/ListE.do?lid=000001168923. Accessed 20 Jan 2017.
Cabinet Office GOJ. Basic Policy on Economic and Fiscal Management and Reform 2015 (English version). Without economic revitalization, there can be no fiscal consolidation; 2018. http://www5.cao.go.jp/keizai-shimon/kaigi/cabinet/2015/2015_basicpolicies_en.pdf. Accessed 20 Jan 2017.
Routledge PA, O’Mahony MS, Woodhouse KW. Adverse drug reactions in elderly patients. Br J Clin Pharmacol. 2004;57:121–6.
Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5:345–51.
Hammond T, Wilson A. Polypharmacy and falls in the elderly: a literature review. Nurs Midwifery Stud. 2013;2:171–5.
Lindley CM, Tully M, Paramsothy V, et al. Inappropriate medication is a major cause of adverse drug reactions in elderly patients. Age Ageing. 1992;21:294–300.
Beers MH, Ouslander JG, Rollingher I, et al. Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA Division of Geriatric Medicine. Arch Intern Med. 1991;151:1825–32.
American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated Beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63:2227–46.
O’Mahony D, O’Sullivan D, Byrne S, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44:213–8.
Naugler CT, Brymer C, Stolee P, et al. Development and validation of an improving prescribing in the elderly tool. Can J Clin Pharmacol. 2000;7:103–7.
Laroche ML, Charmes JP, Merle L. Potentially inappropriate medications in the elderly: a French consensus panel list. Eur J Clin Pharmacol. 2007;63:725–31.
Rognstad S, Brekke M, Fetveit A, et al. The Norwegian General Practice (NORGEP) criteria for assessing potentially inappropriate prescriptions to elderly patients. A modified Delphi study. Scand J Prim Health Care. 2009;27:153–9.
Kim DS, Heo SI, Lee SH. Development of a list of potentially inappropriate drugs for the Korean elderly using the Delphi method. Healthc Inform Res. 2010;16:231–52.
Kojima T, Mizukami K, Tomita N, et al. Screening tool for older Persons’ appropriate prescriptions in Japanese: report of the Japan Geriatrics Society Working Group on “Guidelines for medical treatment and its safety in the elderly”. Geriatr Gerontol Int. 2016;16:983–1001.
Gallagher P, Ryan C, Byrne S, et al. STOPP (Screening Tool of Older Persons’ Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther. 2008;46:72–83.
Holt S, Schmiedl S, Thürmann PA. Potentially inappropriate medications in the elderly: the PRISCUS list. Dtsch Arztebl Int. 2010;107:543–51.
Gallagher P, Barry P, O’Mahony D. Inappropriate prescribing in the elderly. J Clin Pharm Ther. 2007;32:113–21.
Hill-Taylor B, Sketris I, Hayden J, et al. Application of the STOPP/START criteria: a systematic review of the prevalence of potentially inappropriate prescribing in older adults, and evidence of clinical, humanistic and economic impact. J Clin Pharm Ther. 2013;38:360–72.
Dalleur O, Spinewine A, Henrard S, et al. Inappropriate prescribing and related hospital admissions in frail older persons according to the STOPP and START criteria. Drugs Aging. 2012;29:829–37.
Hamilton H, Gallagher P, Ryan C, et al. Potentially inappropriate medications defined by STOPP criteria and the risk of adverse drug events in older hospitalized patients. Arch Intern Med. 2011;171:1013–9.
Kanaan AO, Donovan JL, Duchin NP, et al. Adverse drug events after hospital discharge in older adults: types, severity, and involvement of Beers criteria medications. J Am Geriatr Soc. 2013;61:1894–9.
Price SD, Holman CD, Sanfilippo FM, et al. Association between potentially inappropriate medications from the Beers criteria and the risk of unplanned hospitalization in elderly patients. Ann Pharmacother. 2014;48:6–16.
Price SD, Holman CD, Sanfilippo FM, et al. Are high-care nursing home residents at greater risk of unplanned hospital admission than other elderly patients when exposed to Beers potentially inappropriate medications? Geriatr Gerontol Int. 2014;14:934–41.
Albert SM, Colombi A, Hanlon J. Potentially inappropriate medications and risk of hospitalization in retirees: analysis of a US retiree health claims database. Drugs Aging. 2010;27:407–15.
Reich O, Rosemann T, Rapold R, et al. Potentially inappropriate medication use in older patients in Swiss managed care plans: prevalence, determinants and association with hospitalization. PLoS One. 2014;9:e105425.
Cahir C, Moriarty F, Teljeur C, et al. Potentially inappropriate prescribing and vulnerability and hospitalization in older community-dwelling patients. Ann Pharmacother. 2014;48:1546–54.
Price SD, Holman CD, Sanfilippo FM, et al. Does ongoing general practitioner care in elderly patients help reduce the risk of unplanned hospitalization related to Beers potentially inappropriate medications? Geriatr Gerontol Int. 2015;15:1031–9.
Lund B, Schroeder M, Middendorff G, et al. Effect of hospitalization on inappropriate prescribing in elderly Medicare beneficiaries. J Am Geriatr Soc. 2015;63:699–707.
Onatade R, Auyeung V, Scutt G, et al. Potentially inappropriate prescribing in patients on admission and discharge from an older peoples’ unit of an acute UK hospital. Drugs Aging. 2013;30:729–37.
van der Stelt CAK, Windsant-Van Den Tweel AV, Egberts ACG, et al. The association between potentially inappropriate prescribing and medication-related hospital admissions in older patients: a nested case control study. Drug Saf. 2016;39:79–87.
Masumoto S, Sato M, Maeno T, et al. Association between potentially inappropriate medications and anxiety in Japanese older patients. Geriatr Gerontol Int. 2017;17:2520–6.
Medical Data Vision Co., Ltd. Press release. 2016. https://www.mdv.co.jp/press/2016/. Accessed 3 Mar 2018.
Matsuda S, Ishikawa KB, Kuwabara K, et al. Development and use of the Japanese case-mix system. Eurohealth. 2008;14:25–30.
Maclure M, Mittleman MA. Should we use a case-crossover design? Annu Rev Public Health. 2000;21:193–221.
Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991;133:144–53.
Schmiedl S, Rottenkolber M, Szymanski J, et al. Preventable ADRs leading to hospitalization—results of a long-term prospective safety study with 6427 ADR cases focusing on elderly patients. Expert Opin Drug Saf. 2018;17:125–37.
Ní Chróinín D, Neto HM, Xiao D, et al. Potentially inappropriate medications (PIMs) in older hospital in-patients: prevalence, contribution to hospital admission and documentation of rationale for continuation. Australas J Ageing. 2016;35:262–5.
Schneeweiss S, Stürmer T, Maclure M. Case–crossover and case–time–control designs as alternatives in pharmacoepidemiologic research. Pharmacoepidemiol Drug saf. 1997;6:S51–9.
Hallas J, Pottegård A. Use of self-controlled designs in pharmacoepidemiology. J Intern Med. 2014;275:581–9.
Acknowledgements
This work was supported by both the Keihanshin Consortium for Fostering the Next Generation of Global Leaders in Research (K-CONNEX, Kyoto, Japan), established by the Human Resource Development Program for Science and Technology, and the Ministry of Education, Culture, Sports, Science and Technology (MEXT, Tokyo, Japan). We would like to thank Medical Data Vision (MDV) for generously providing the medical data and Editage (http://www.editage.jp) for English language editing. These contributors received no extra compensation.
Author information
Authors and Affiliations
Contributions
IS and KK had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: IS and KK. Acquisition, analysis, or interpretation of data: IS, KK, GK, and YY. Drafting of the manuscript: IS Critical revision of the manuscript for important intellectual content: IS, KK, GK, and YY. Statistical analysis: IS. Obtained funding: IS. Administrative, technical, or material support: IS, KK, GK, and YY. Study supervision: KK.
Corresponding author
Ethics declarations
Conflicts of Interest
Izumi Sato has received support from K-CONNEX and a grant from the Pfizer Health Research Foundation (Grant number 203150600035). Koji Kawakami received research funds from Dainippon Sumitomo Pharma, Olympus, Stella Pharma, Medical Platform Co., Novartis Pharmaceutical K.K., Bayer, and CMIC Inc. He has also received consultation fees from Olympus, Kyowa Hakko Kirin, Kaken Pharmaceutical, and Takeda Pharmaceutica, and lecture fees from Daiichi Sankyo, Eisai, Boehringer Ingelheim Japan Inc., Mitsubishi Tanabe Pharma, Abbie, Chugai, and Sanofi K.K. No other disclosures were reported. Yosuke Yamamoto and Genta Kato have no conflicts of interest that are directly relevant to the content of this study.
Funding
This work was supported by the Pfizer Health Research Foundation (Grant number 203150600035). This financial assistance was used to conduct the study described in the manuscript and to assist with the preparation of the manuscript.
Ethical Approval
The Institutional Review Board of Kyoto University approved the study protocol (approval R0541) on April 22, 2016. A collaborative research agreement was obtained from MDV.
Patient Consent
The requirement for written informed consent was waived because this was a retrospective study analyzing anonymized data.
Sponsor’s Role
The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sato, I., Yamamoto, Y., Kato, G. et al. Potentially Inappropriate Medication Prescribing and Risk of Unplanned Hospitalization among the Elderly: A Self-Matched, Case-Crossover Study. Drug Saf 41, 959–968 (2018). https://doi.org/10.1007/s40264-018-0676-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-018-0676-9