Abstract
Background
Real-world studies on fremanezumab, an anti-calcitonin gene-related peptide monoclonal antibody for migraine prevention, are few and with limited follow-up.
Objective
We aimed to evaluate the long-term (up to 52 weeks) effectiveness and tolerability of fremanezumab in high-frequency episodic migraine and chronic migraine.
Methods
This s an independent, prospective, multicenter cohort study enrolling outpatients in 17 Italian Headache Centers with high-frequency episodic migraine or chronic migraine and multiple preventive treatment failures. Patients were treated with fremanezumab 225 mg monthly. The primary outcomes included changes from baseline (1 month before treatment) in monthly headache days, response rates (reduction in monthly headache days from baseline), and persistence in medication overuse at months 3, 6, and 12 (all outcome timeframes refer to the stated month). Secondary outcomes included changes from baseline in acute medication intake and disability questionnaires scores at the same timepoints. A last observation carried forward analysis was also performed.
Results
A total of 90 patients who received at least one dose of fremanezumab and with a potential 12-month follow-up were included. Among them, 15 (18.0%) patients discontinued treatment for the entire population, a reduction in monthly headache days compared with baseline was reported at month 3, with a significant median [interquartile range] reduction in monthly headache days (− 9.0 [11.5], p < 0.001). A statistically different reduction was also reported at month 6 compared with baseline (− 10.0 [12.0]; p < 0.001) and at 12 months of treatment (− 10.0 [14.0]; p < 0.001). The percentage of patients with medication overuse was significantly reduced compared with baseline from 68.7% (57/83) to 29.6% (24/81), 25.3% (19/75), and 14.7% (10/68) at 3, 6, and 12 months of treatment, respectively (p < 0.001). Acute medication use (days and total number) and disability scores were also significantly reduced (p < 0.001). A ≥ 50% response rate was achieved for 51.9, 67.9, and 76.5% of all patients at 3, 6, and 12 months, respectively. Last observation carried forward analyses confirmed these findings. Fremanezumab was well tolerated, with just one patient discontinuing treatment because of adverse events.
Conclusions
This study provides evidence for the real-world effectiveness of fremanezumab in treating both high-frequency episodic migraine and chronic migraine, with meaningful and sustained improvements in multiple migraine-related variables. No new safety issue was identified.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Evaluating anti-calcitonin gene-related peptide monoclonal antibodies on long-term real-world treatment is of paramount importance. |
Monthly fremanezumab showed effectiveness and tolerability in patients with drug-resistant severe migraine over 54 weeks of treatment. |
Further studies specifically designed to evaluate a multi-assessed late response are needed. |
1 Introduction
Fremanezumab is a fully humanized (IgG2Δa) monoclonal antibody (mAb) that targets the calcitonin gene-related peptide (CGRP) [anti-CGRP mAb] [1]. It is approved in Europe and the USA for the preventive treatment of both episodic migraine (EM) and chronic migraine (CM). The drug is available in monthly (225-mg) and quarterly (675-mg) dosages that have been shown to be effective and well tolerated in three randomized, double-blind, placebo-controlled phase III trials (i.e., HALO CM, HALO EM, and FOCUS) [2,3,4]. These studies enrolled patients with EM and CM, with or without medication overuse, and inadequate responses to two to four previous migraine preventive treatment classes. The long-term efficacy and safety of fremanezumab have also been demonstrated in a 12-week extension of the FOCUS trial [5].
Despite the rising number of real-world studies on other available mAbs against CGRP (ligand) or its receptor (calcitonin-like receptor/receptor-activating modifying protein 1), such as erenumab and galcanezumab [6], research on fremanezumab is sparse. So far, only three real-world studies with short follow-up periods (up to 12 or 24 weeks) [7,8,9] and a retrospective chart review in the USA [10] have been conducted. Two large studies are underway, including the pan-European PEARL study [11] involving more than 11 countries, and the multicenter FINESSE study, which is being conducted in Austria and Germany [12]. However, long-term results for both studies are not expected until the end of 2023–24.
Long-term effectiveness and safety data on anti-CGRP mAbs, including fremanezumab, are needed to further assess and orient their use, especially given that preliminary evidence reveals discrepancies among these drugs [13, 14]. Indeed, according to the European Headache Federation guidelines, switching from one anti-CGRP mAb to another is an option, even though there are still inadequate data on its potential advantages [15]. Furthermore, predictors of response and time to response for anti-CGRP/receptor mAbs have yet to be well established in a real-world setting [1]. In this multicenter prospective study, we aimed to evaluate the long-term (up to 52 weeks) effectiveness, safety, and tolerability of monthly fremanezumab in patients with high-frequency EM (HFEM) or CM in Italy. Moreover, we aimed to investigate the potential predictors of treatment response at different timepoints.
2 Methods
2.1 Study Design and Ethics
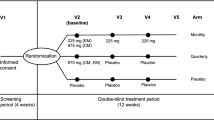
In 2019, the ‘Italian Headache Registry’ (Registro Italiano per le Cefalee, RICe) was established to evaluate primary headache disorders epidemiology in Italy. The study received ethics approval on 20 March, 2019. RICe currently involves 52 Italian headache centers (any level of care), and all patients attending these centers are proposed to be inserted in the registry. Consenting patients inserted in the registry are followed up at each visit. Among the aims that pushed the creation of the registry, there is the possibility to conduct specific observational projects joining involved centers. An additional observational protocol regarding fremanezumab was approved on 14 November, 2019. Hence, we conducted an independent (investigator-initiated), prospective, multicenter cohort study involving patients treated with fremanezumab in centers who joined the project (17 centers). The study consisted of a 12-month treatment period with a 1-month baseline (run-in) period. All consecutive outpatients who received at least one administration of monthly or quarterly fremanezumab between July 2020 and June 2022 were enrolled in the study and provided informed consent to participate in RICe. All procedures were performed according to clinical practice and all patients were included in the dataset regardless of having withdrawn from treatment for any reason. Patients were then assessed for effectiveness and safety based on a minimum follow-up of 12 months (Fig. 1). The study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
2.2 Patient Features and Variables Collected
The study recruited adult patients diagnosed with HFEM (8–14 migraine headache days/month) or CM according to the International Classification of Headache Disorders Third Edition criteria [16], with or without medication overuse (MO), who started fremanezumab treatment during the study period. For patients with MO, prior detoxication strategies were not mandatory. To access fremanezumab, according to Italian regulations, patients had to report previous failures of at least three preventive treatments among tricyclic antidepressants, beta-blockers, antiepileptic drugs, and onabotulinumtoxinA (for CM), owing to a lack of efficacy or tolerability. We included only patients treated with fremanezumab, 225 mg monthly (Fig. 1).
Baseline status was captured using diaries. Throughout the treatment phase, patients recorded their monthly headache days (MHDs) and acute medication use, including the absolute number of acute medications (AMNs) and days with at least one analgesic (AMDs, acute medication days) per month, in a headache diary. A headache day was defined as any day on which a patient reported any type of headache, and response rates were assessed based on the reduction in MHDs of 30, 50, 75, or 100%. For this study, a month was defined as 30 days.
In addition, patients completed the Headache Impact Test (HIT-6) questionnaire monthly and the Migraine Disability Assessment (MIDAS) questionnaire every 3 months. Both questionnaires are largely used in migraine studies [17, 18]. Any adverse events (AEs) experienced during treatment were also reported. Demographic information, migraine characteristics (such as the presence of aura, disease duration, and onset of migraine), previous failures with drug classes (including beta-blockers, tricyclic antidepressants, antiepileptic drugs, and onabotulinumtoxinA), and current concomitant preventive and acute symptomatic treatments were collected. Patients were allowed to use other preventive medications according to clinical practice. All variables were documented electronically and extracted using the RICe registry.
2.3 Outcomes and Analysis
The primary outcomes consisted of the absolute change from baseline in MHDs, response rates (≥ 30, ≥ 50, ≥ 75, and 100% reduction in MHDs), and persistence in MO at month 3, 6, and 12 compared to baseline. Monthly headache days were selected instead of monthly migraine days according to data availability in clinical practice settings. Secondary outcomes included the absolute changes from baseline in the overall number of acute medications used and days with at least one analgesic used, as well as scores on the MIDAS and HIT-6 questionnaires at the same timepoints. All patients with potentially 12 months of follow-up were included in the study, regardless of treatment discontinuation because of AEs, ineffectiveness, or loss to follow-up (Fig. 1). A last observation carried forward (LOCF) analysis was performed because of the absence of follow-up data after discontinuation for patients who stopped anti-CGRP mAbs for any reason, assuming no further changes. Finally, predictors of a ≥ 50% response (on MHDs) were evaluated at 3, 6, and 12 months of treatment using demographic and clinical baseline variables. All outcome timeframes refer to the stated month. All analyses were conducted on the entire population and then separately on patients with HFEM and CM.
2.4 Statistical Analysis and Missing Data
The study’s sample size was not determined based on statistical considerations. All consecutive out-patients who received at least one administration of monthly or quarterly fremanezumab from July 2020 to June 2022 were included. With shorter follow-ups, the sample size is comparable to or slightly lower than that of previous observational studies using fremanezumab [7,8,9]. We reported mean ± standard deviation or median interquartile range for continuous variables and number (percentage) for categorical data. The normality assumption was assessed using the Shapiro–Wilk test, and because the data were not normally distributed, a Wilcoxon signed-rank test was performed to evaluate pre-post changes in quantitative variables and an exact McNemar’s test was used for categorical-dependent variables. As few patients had missing data for the variables, years from migraine onset and years from chronicization onset at baseline, and HIT-6 score at 3 and 6 months, no imputation was performed for missing data, and the number of patients analyzed is reported in figure and table legends as appropriate. There were no other missing data.
We performed two different analyses. Because of the lack of follow-up data after discontinuance for patients who ceased anti-CGRP mAbs for any reason, a LOCF analysis was conducted, assuming no further changes. We performed a LOCF (see below) to investigate the influence of dropouts on an effectiveness analysis, and, as a second step, dropouts were treated as non-responders in the regression analysis. Predictors of a ≥ 50% response (on MHDs) were evaluated at 3, 6, and 12 months of treatment using demographic and clinical baseline data as the dependent variable.
A binary logistic regression (odds ratios and 95% confidence intervals) was performed to estimate a ≥ 50% response rate at 3, 6, and 12 months with selected variables significant in earlier analyses, or that were of clinical interest. For the regressions, patients who discontinued treatment were considered as non-responders. For all variables, a significance level of p < 0.05 was considered statistically significant, and the Bonferroni correction was used for multiple comparisons. SPSS software version 26.0 (SPSS Statistics; IBM Corp., Armonk, NY, USA) was used for all data analyses, and GraphPad Prism version 9.00 (La Jolla, CA, USA) was used to create the graphs.
3 Results
3.1 Baseline Characteristics
Overall, 90 patients reported in the RICe registry received at least one administration of fremanezumab between July 2020 and June 2022 (i.e., patients with 12 potential months of follow-up). For the analysis, seven patients were excluded for incomplete data (five patients) or using a quarterly dose of fremanezumab in order to standardize the population (two patients). Patients’ flowcharts are reported in Fig. 1. Finally, 83 patients (71.1% female, aged 56.2 ± 15.2 years) were included. At baseline, most patients had CM (67 [80.7%]), 16 had HFEM (19.3%), and 57 of the patients with HFEM (68.7%) were in MO. The mean duration of migraine was 38.1 ± 15.7 years. A history of aura was reported in four patients (4.8%). Clinical and demographic features are summarized in Table 1 for the overall population and separately for patients with CM and HFEM. All concomitant and prior treatments at baseline are reported in Table S1 of the Electronic Supplementary Material (ESM). Briefly, 85.6% of patients had at least three classes of preventive treatments documented as ineffective (42.2% with onabotulinumtoxinA), with a mean (standard deviation) of 4.0 ± 1.4 class failures (Table S1 of the ESM). Migraine-related variables were fully available during the treatment period; some missing data were reported only for HIT-6 total scores at 3 and 6 months of treatment, as highlighted in Table 2.
3.2 Effectiveness Analysis
Fifteen (15/83; 18.0%) patients discontinued treatment during the 12-month follow-up, with two (2.4%), six (7.2%), and seven (8.4%) patients before 3, 6, or 12 months of treatment, respectively (Fig. 1). The major cause for discontinuing monthly fremanezumab was ineffectiveness (n = 10/15; 66.6%), followed by lost to follow-up (n = 3/15; 20.0%), withdrawn because of the patient’s choice (n = 1/15; 6.6%), and a lack of tolerability (n = 1/15; 6.6%) [Fig. 1].
Monthly headache days were significantly reduced by fremanezumab at 3, 6, and 12 months compared with baseline in the entire population, CM, or HFEM (Table 2; Fig. 2). In particular, for the entire population, a reduction in MHDs compared with baseline was reported at month 3, with a significant median [interquartile range] reduction in MHDs (− 9.0 [11.5], p < 0.001). A statistically different reduction was also reported at month 6 compared with baseline (− 10.0 [12.0]; p < 0.001) and at 12 months of treatment (− 10.0 [14.0]; p < 0.001) [Table 2; Fig. 2].
Number of monthly headache days, number of acute medications per month, and days with at least one analgesic use per month. The number of patients reported per group is shown in Table 2. Values reported are mean and 95% confidence interval. CM chronic migraine, HFEM high-frequency episodic migraine
A ≥ 50% response rate compared to baseline was achieved by 51.9, 67.9, and 76.5% of patients at 3, 6, and 12 months of treatment, respectively. Patients achieving a ≥ 75% response rate were 23.5, 34.6, and 36.8% at 3, 6, and 12 months of treatment, respectively. Two patients achieved 100% response at 3 months (2.5%), increasing to four (5.3%) at 6 months and five (7.4%) at 12 months of treatment (Fig. 3a; Table 3). Responder rates for patients with CM and HFEM are reported separately in Table 3 and Fig. 3a. Considering only patients who completed 12 months of treatment, six (8.8%) patients who were not responders at 6 months achieved a response status at 12 months, 46 (67.6%) persisted in response, 12 (17.6%) continued to be non-responders, and four (5.9%) lost the responder status.
Response rates in the overall population (a) and medication overuse in the cohort (b). Percentages are calculated on the total number of patients per follow-up as reported in Table 3. Values reported are mean and 95% confidence interval. CM chronic migraine
The percentage of patients with MO was significantly reduced compared with baseline from 68.7% (57/83) to 29.6% (24/81), 25.3% (19/75), and 14.7% (10/68) at 3, 6, and 12 months of treatment, respectively (p < 0.001) [Fig. 3b]. The subgroup of patients with CM showed similar reductions in MO (Fig. 3b). Disability questionnaire (MIDAS and HIT-6) scores were reduced (p < 0.001) compared with baseline at all follow-up timepoints, as reported in Fig. 4 and Table 2. AMDs and acute medications were significantly reduced at 3, 6, and 12 months of treatment compared with baseline (Fig. 2; Table 2). No difference between the various follow-ups (i.e., 3 vs 6 months; 3 vs 12 months, and 6 vs 12 months) was found.
Migraine Disability Assessment (MIDAS) and Headache Impact Test (HIT-6) total scores per month. The number of patients reported per group is shown in Table 2. CM chronic migraine, HFEM high-frequency episodic migraine
3.3 Clinical Predictors of Response
Univariate regressions with baseline-selected variables were performed to assess clinical predictors of a ≥ 50% response (in MHDs) in patients at 3, 6, and 12 months of follow-up (Table S5 of the ESM). Dropouts were considered as non-responders. No variables were significantly associated with a ≥ 50% response at any months of follow-up and, therefore, no multivariate regression analysis was carried out (Table S5 of the ESM).
3.4 Safety and Tolerability Analysis
No severe AEs have been reported throughout the study. A total of eight patients (9.6%) experienced at least one AE, with a total of ten AEs reported (Table S2 of the ESM). All events were mild and transient, and only one patient (1.2%) discontinued treatment because of no tolerability after 6 months for a local allergic reaction at the injection site, which, treated with cetirizine, achieved complete resolution. The most common AEs were constipation (7.2%) followed by injection-site reactions (3.6%) [Table S2 of the ESM].
3.5 Last Observation Carried Forward Analysis
The LOCF analysis, which included all patients (n = 83) at all follow-ups and assumed no further changes after dropout, showed that an increase in the response rate during treatment, although meaningfully elevated (a ≥ 50% response rate in the overall population of 63.8% at 12 months), was attenuated in comparison with the results obtained with the observed data analysis (Table S4 of the ESM). In the overall population, patients with a ≥ 30% response rate were 68.7, 72.3, and 69.9% at 3, 6, and 12 months of treatment, respectively, whereas 50.6, 61.4, and 63.8% of patients achieved a ≥ 50% response rate at the same timepoints (Table S4 of the ESM). The reduction in patients with MO was not modified in the LOCF analysis for both overall and CM populations.
Finally, in the LOCF analysis, no significant changes were reported for MHDs, AMDs, acute medications, and disability questionnaire total scores (Table S3 of the ESM) compared with the observed data analysis. As reported for responder rates, the further, although slight, reduction between 6 and 12 months of treatment was not replicated in the LOCF analysis.
4 Discussion
In our prospective multicenter long-term study, we show that monthly fremanezumab is effective and well tolerated as a preventive treatment in patients with CM and HFEM for up to 12 months in a real-world setting. To the best of our knowledge, this is the first real-world study assessing the effectiveness of fremanezumab up to 12 months in patients with drug-resistant migraine. We are aware of a previous Italian study that evaluated the efficacy of fremanezumab with a 3- or 6-month follow-up (FRIEND study) [7, 8], as well as a Greek registry with an up to 3-month follow-up [9], and a retrospective US chart review study reporting data up to 6 months [10].
The characteristics of our cohort are comparable to those described in previous studies, both in terms of sex and distribution of other clinical variables, including prior preventive failures. However, as discussed below, our cohort exhibited a higher average age compared with previous studies (mean age 56.2 years, vs 39.7–48.9 years).
In line with previous real-world studies [8,9,10], we confirmed the effectiveness and tolerability of monthly fremanezumab in difficult-to-treat patients with HFEM and CM, with several preventive failures, including onabotulinumtoxin A. At variance with previous investigations, in our present study, most patients completed the 12 months of treatment, before the mandatory interruption according to the Italian regulations, with a low discontinuation rate (18.0%). This highlights a favorable clinical response to fremanezumab as an effective migraine preventive treatment, confirming the remarkable persistence in anti-CGRP mAb treatment, which substantially differs from persistence reported for standard oral preventive therapies [19].
Our findings confirm: an early improvement in migraine frequency, associated with a reduction in analgesic intake, calculated as the total number and days with acute medications, and disability scores; a progressive increase in response up to 6 months of treatment, which was maintained until the end of the 12-month observation period; and no evidence of increase in AEs. The response rate (≥ 50%) in our study is comparable to those obtained by other prospective studies, including the FRIEND studies in the overall population at 3 and 6 months (64.2 and 73.6% vs 51.9 and 67.9% in our study) [7, 8] and in a study of a Greek registry at 3 months in CM (62.6 vs 51.9%). However, their results show a slightly lower response rate for HFEM (83.5 vs 56.2%) [9]. Notably, although patients enrolled in previous observational studies had a higher burden of disease, a higher number of prior treatment failures and a higher rate of MO at baseline than those enrolled in RCTs [6], all real-world studies unanimously report superior improvements in migraine-related variables compared with those found in pivotal RCTs and their open-label extension (e.g., 6-month open-label FOCUS trial) [5, 6].
The reconciliation of outcomes between randomized controlled trials (RCTs) and observational studies is a noteworthy challenge within clinical medicine, as numerous factors may contribute to the disparity in results. These factors encompass selection bias, confounding factors, statistical power, and differential adherence and follow-up [20]. A Cochrane review [21] discovered little evidence that the results of observational studies and RCTs consistently differ. This underlines that observational studies may be an important addition to the clinician’s resources by complementing RCT data. Nevertheless, a thorough examination of the reasons underlying the apparent superiority of observational studies over RCTs in relation to anti-CGRP/receptor mAbs is worthy of further evaluation.
Fremanezumab showed consistency in its effectiveness and tolerability, as they were maintained over time, in observational studies with an increasing follow-up of treatment [7,8,9]. Our study enrolled drug-resistant patients who did not respond to or tolerate at least three preventive classes with 68.7% of patients with MO. We confirmed that fremanezumab, like other anti-CGRP/receptor mAbs, is effective in patients with MO, with a reversion of the overuse without other treatment, an effect that significantly affects patients daily quality of life [22].
This difficult-to-treat migraine population is usually poorly represented in clinical trials and is the most challenging to manage in clinical practice, for both acute and preventive treatment. Furthermore, our cohort was older compared with other real-world studies [7, 8, 10] and RCTs [3,4,5] with fremanezumab or erenumab (mean 46.7, interquartile range 45.7–49) [6]. In our cohort, no unexpected AEs were reported, the incidence of AEs was not age related, and age was not a predictive variable for achieving a response status at any timepoint, underlining the safety and effectiveness of fremanezumab.
The reduction in MHDs and other migraine-related variables occurred mainly after the first 3 months of treatment, followed by a slightly further decrease in the following 3 months (6 months). As confirmed by the sensitivity analysis, no further significant improvement was observed at months 6 and 12 of treatment. Although, in principle, a longer treatment might lead to a better response rate, in line with previous studies [1, 6], both observed data and sensitivity analyses suggest a ceiling effect of anti-CGRP mAb effectiveness. Several clinical and demographic predictors were identified in different studies (e.g., migraine burden at baseline, years of migraine, allodynia, triptan use, body mass index), as discussed in [23], but results are usually inconsistent among them, and there is no current evidence for robust clinical predictors of response to mAbs. No predictors of response (≥50% in MHD reduction) have been identified in our cohort at any follow-up. It should be noted that some variables reported in other real-world studies (e.g., autonomic symptoms, triptans effectiveness, mood disorders) were not collected in this population [24]. Fremanezumab was well tolerated as all AEs were mild and transient and no serious AEs were reported. Few AEs occurred during the first 6 months of treatment. Only in one case, because of a transient local allergic reaction, treatment was discontinued at month 6.
Several strengths characterize our study. This is the first study reporting 12 months follow-up of fremanezumab treatment in clinical practice, enrolling patients usually under-represented in RCTs. In fact, our cohort consisted of patients with HFEM and CM who did not respond or tolerate at least three previous preventive treatments, and most of them with MO. Further strengths include the use of different analyses on acute medication use (including days and total number of acute medications used) and on disability questionnaires, and a sensitivity analysis to adjust effectiveness results for missing data and dropouts. There are, however, some limitations, including the use of only MHDs instead of distinguishing MHDs from monthly migraine days. Some patients (Table S1 of the ESM) received concomitant preventive therapy (regardless of clinical indication) during fremanezumab. However, as no preventive treatment was initiated shortly before or after fremanezumab, and considering the high burden of disease at baseline, it is unlikely that this would have impacted on the results. We also did not record the number of patients with MO who underwent detoxication procedures, which might have contributed to the efficacy of fremanezumab. Furthermore, being an open-label study, we cannot rule out the potential placebo effect and the cyclical exacerbations and relative remissions of migraine over time. Finally, our analyses included only patients treated with monthly fremanezumab, and results may not apply to the quarterly regimen.
5 Conclusions
This study provides evidence in support of the real-world effectiveness of monthly fremanezumab in treating both HFEM and CM, which complements and extends its effectiveness shown in previous studies. Moreover, the present results add to the currently limited data on the use of fremanezumab in real-world settings. Our study shows sustained improvements in multiple variables, including migraine frequency, acute medication use, and disability questionnaires, in a population of patients with difficult-to-treat migraine with treatment failures to multiple preventive medications. Considering the cyclical nature of migraine and the lack of long-term data on fremanezumab over 12 months, further studies are needed to evaluate effectiveness and safety long term.
References
Al-Hassany L, Goadsby PJ, Danser AHJ, MaassenVanDenBrink A. Calcitonin gene-related peptide-targeting drugs for migraine: how pharmacology might inform treatment decisions. Lancet Neurol. 2022;21(3):284–94.
Bigal ME, Walter S, Rapoport AM. Fremanezumab as a preventive treatment for episodic and chronic migraine. Expert Rev Neurother. 2019;19(8):719–28.
Silberstein SD, Dodick DW, Bigal ME, Yeung PP, Goadsby PJ, Blankenbiller T, et al. Fremanezumab for the preventive treatment of chronic migraine. N Engl J Med. 2017;377(22):2113–22.
Ferrari MD, Diener HC, Ning X, Galic M, Cohen JM, Yang R, et al. Fremanezumab versus placebo for migraine prevention in patients with documented failure to up to four migraine preventive medication classes (FOCUS): a randomised, double-blind, placebo-controlled, phase 3b trial. Lancet. 2019;394(10203):1030–40.
Ashina M, Cohen JM, Galic M, Campos VR, Barash S, Ning X, et al. Efficacy and safety of fremanezumab in patients with episodic and chronic migraine with documented inadequate response to 2 to 4 classes of migraine preventive medications over 6 months of treatment in the phase 3b FOCUS study. J Headache Pain. 2021;22(1):68.
Pavelic AR, Wober C, Riederer F, Zebenholzer K. Monoclonal antibodies against calcitonin gene-related peptide for migraine prophylaxis: a systematic review of real-world data. Cells. 2022;12(1):143.
Barbanti P, Egeo G, Aurilia C, d’Onofrio F, Albanese M, Cetta I, et al. Fremanezumab in the prevention of high-frequency episodic and chronic migraine: a 12-week, multicenter, real-life, cohort study (the FRIEND study). J Headache Pain. 2022;23(1):46.
Barbanti P, Egeo G, Aurilia C, Torelli P, Finocchi C, d’Onofrio F, et al. Early and sustained efficacy of fremanezumab over 24-weeks in migraine patients with multiple preventive treatment failures: the multicenter, prospective, real-life FRIEND2 study. J Headache Pain. 2023;24(1):30.
Argyriou AA, Dermitzakis EV, Xiromerisiou G, Rallis D, Soldatos P, Litsardopoulos P, et al. Efficacy and safety of fremanezumab for migraine prophylaxis in patients with at least three previous preventive failures: prospective, multicenter, real-world data from a Greek registry. Eur J Neurol. 2023;30(5):1435–42.
Driessen MT, Cohen JM, Patterson-Lomba O, Thompson SF, Seminerio M, Carr K, et al. Real-world effectiveness of fremanezumab in migraine patients initiating treatment in the United States: results from a retrospective chart study. J Headache Pain. 2022;23(1):47.
Ashina M, Amin FM, Kokturk P, Cohen JM, Konings M, Tassorelli C, et al. PEARL study protocol: a real-world study of fremanezumab effectiveness in patients with chronic or episodic migraine. Pain Manag. 2021;11(6):647–54.
Straube A, Broessner G, Gaul C, Hamann X, Kraya T, Schauerte I, et al. Fremanezumab for preventive treatment in migraine: the FINESSE study (P16–2.001). Neurology. 2022;98(18 Suppl):1678.
Iannone LF, Burgalassi A, Vigani G, Tabasso G, De Cesaris F, Chiarugi A, et al. Switching anti-CGRP(R) monoclonal antibodies in multi-assessed non-responder patients and implications for ineffectiveness criteria: a retrospective cohort study. Cephalalgia. 2023;43(4):3331024231160519.
Overeem LH, Peikert A, Hofacker MD, Kamm K, Ruscheweyh R, Gendolla A, et al. Effect of antibody switch in non-responders to a CGRP receptor antibody treatment in migraine: a multi-center retrospective cohort study. Cephalalgia. 2022;42(4–5):291–301.
Sacco S, Amin FM, Ashina M, Bendtsen L, Deligianni CI, Gil-Gouveia R, et al. European Headache Federation guideline on the use of monoclonal antibodies targeting the calcitonin gene related peptide pathway for migraine prevention: 2022 update. J Headache Pain. 2022;23(1):67.
Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211.
Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) questionnaire to assess headache-related disability. Neurology. 2001;56(6 Suppl. 1):S20–8.
Yang M, Rendas-Baum R, Varon SF, Kosinski M. Validation of the Headache Impact Test (HIT-6) across episodic and chronic migraine. Cephalalgia. 2011;31(3):357–67.
Hepp Z, Dodick DW, Varon SF, Chia J, Matthew N, Gillard P, et al. Persistence and switching patterns of oral migraine prophylactic medications among patients with chronic migraine: a retrospective claims analysis. Cephalalgia. 2017;37(5):470–85.
Ross J. Randomized clinical trials and observational studies are more often alike than unlike. JAMA Intern Med. 2014;174:10.
Anglemyer A, Horvath HT, Bero L. Healthcare outcomes assessed with observational study designs compared with those assessed in randomized trials. Cochrane Database Syst Rev. 2014;2014(4):MR000034.
Alpuente A, Torres-Ferrus M, Terwindt GM. Preventive CGRP-targeted therapies for chronic migraine with and without medication-overuse headache. Cephalalgia. 2023;43(3):1–11.
Barbanti P, Egeo G, Aurilia C, Altamura C, d’Onofrio F, Finocchi C, et al. Predictors of response to anti-CGRP monoclonal antibodies: a 24-week, multicenter, prospective study on 864 migraine patients. J Headache Pain. 2022;23(1):138.
Hong JB, Lange KS, Overeem LH, Triller P, Raffaelli B, Reuter U. A scoping review and meta-analysis of anti-CGRP monoclonal antibodies: predicting response. Pharmaceuticals (Basel). 2023;16(7):934.
Acknowledgments
The “Società Italiana per lo Studio delle Cefalee” (SISC) is acknowledged for the “Registro Italiano delle Cefalee (RICe)”. Figure 1 is created with Biorender.com. The Italian Headache Registry (RICe) Study Group: Marta Allena, Daria Brovia, Giorgio Liaci, Giorgio Tabasso, Giulia Vigani, Gabriele Garascia, Paolo Manganotti, Anna La Porta, Natascia Beretta, Stefano Tronci, Claudio Baiata.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
Open access funding provided by Università degli Studi di Firenze within the CRUI-CARE Agreement.
Conflict of interest
Pierangelo Geppetti received personal fees from Allergan, Eli Lilly, Novartis, Amgen, and TEVA; grants from Amgen, TEVA, Eli-Lilly, Allergan, and Chiesi; is on the Scientific Advisory Board for Endosome Therapeutics; and is a founding scientist of FloNext srl, Spinoff of the University of Florence. Francesco De Cesaris received personal fees from TEVA, Eli Lilly, and Novartis. Luigi Francesco Iannone received personal fees from Eli-Lilly and TEVA, and a travel grant from Lundbeck. Simona Sacco reports personal fees as a speaker or advisor from Abbott, Allergan-AbbVie, AstraZeneca, Eli Lilly, Lundbeck, Novartis, NovoNordisk, Pfizer, and Teva, and research grants from Novartis. Raffaele Ornello reports personal fees from Novartis, Eli Lilly, and Teva, and non-financial support from Novartis, Allergan, Eli Lilly, and Teva. Simona Guerzoni received personal fees from Allergan/AbbVie, Eli Lilly, Novartis, Teva, and Lundbeck. Carlo Baraldi received fees and honoraria from Eli-Lilly, TEVA, Allergan/AbbVie, Lundbeck, and Novartis. Grazia Sances received personal fees as a speaker or was on the Advisory Board for Eli-Lilly, Novartis, TEVA, Lundbeck, and Pfizer. Roberto De Icco received honoraria for scientific presentations from Eli-Lilly and Teva. Gloria Vaghi received travel grants from Lundbeck and TEVA. Marta Allena received personal fees as a speaker from Eli Lilly. N.G. received personal fees as a speaker from Eli Lilly. Valeria Caponnetto, Antonio Russo, Marcello Silvestro, Alessandro Tessitore, Cristina Tassorelli, Grazia Sances, Flavia Lo Castro, Simona Guerzoni, Maria Pia Prudenzano, Adriana Fallacara, Martino Gentile, Agnese Onofri, Andrea Burgalassi, Alberto Chiarugi, Antonio Granato, Alfonsina Casalena, Marina De Tommaso, Edoardo Mampreso, Paola Merlo, Gianluca Coppola, Stefania Battistini, Valentina Rebecchi, Innocenzo Rainero, Federica Nicoletta Sepe, and Giorgio Dalla Volta have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
The study was approved as a part of the Registro Italiano Cefalee (RICe) study by the local ethics committee (Studio RICe, 14591_oss and subsequent emendaments).
Consent to participate
Informed consent was obtained from each patient.
Consent for publication
Not applicable.
Availability of data and material
Data supporting the findings in the present study are reported in the article and in the supplementary materials. The raw data collected and analyzed are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
All authors critically reviewed the manuscript, agreed to be fully accountable for ensuring the integrity and accuracy of the work, and read and approved the final manuscript.
Additional information
The members of The Italian Headache Registry (RICe) Study Group are listed in Acknowledgements section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Caponnetto, V., Russo, A., Silvestro, M. et al. Long-Term Treatment Over 52 Weeks with Monthly Fremanezumab in Drug-Resistant Migraine: A Prospective Multicenter Cohort Study. CNS Drugs 37, 1069–1080 (2023). https://doi.org/10.1007/s40263-023-01050-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-023-01050-3