Abstract
The neurobiological and neurochemical mechanisms underlying the pathophysiology of bipolar disorder are complex and not yet fully understood. From circadian disruption to neuroinflammation, many pathways and signaling molecules are important contributors to bipolar disorder development, some specific to a disease subtype or a cycling episode. Pharmacological agents for bipolar disorder have shown only partial efficacy, including mood stabilizers and antipsychotics. The purinergic hypothesis for bipolar disorder emerges in this scenario as a promising target for further research and drug development, given its role in neurotransmission and neuroinflammation that results in behavioral and mood regulation. Here, we review the basic concepts of purinergic signaling in the central nervous system and its contribution to bipolar disorder pathophysiology. Allopurinol and novel P2X7 receptor antagonists are promising candidates for treating bipolar disorder. We further explore currently available pharmacotherapies and the emerging new purinergic targets for drug development in bipolar disorder.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The new generation of P2X7 receptor antagonists represents a potential breakthrough in treatments for bipolar disorder. |
There is a promising antimanic effect of allopurinol but additional well-designed research on the topic is required. |
Modulation of the P2X4, A1, A2A, and P2Y1 receptors are possible new targets encouraged to be further explored for drug development in bipolar disorder. |
1 Introduction
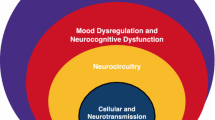
Bipolar disorder (BD) is a major neuropsychiatric condition with complex and multicomponent pathophysiology, involving changes in a wide range of neurocircuitries and signaling pathways [1]. Patients with BD experience different symptoms within the disease spectrum, cycling from severe depression to substantial euphoria, known as mania. It has been well established that genetic and epigenetic factors, metabolic and biochemical pathways, structural and functional brain alterations, and social and environmental triggers may contribute to the disorder’s onset, development, and progression [2]. Many molecular hypotheses have emerged to explain its vast neurobiological spectrum, including changes in neurotransmission systems such as the γ-aminobutyric acid (GABA)ergic, glutamatergic, and dopaminergic systems [3,4,5,6].
BD affects about 39.5 million people worldwide [7]. It is a severe, chronic, and debilitating disease in which patients exhibit an overall impairment in autonomy and cognitive and psychosocial functioning [8]. The many facets of BD and such a broad umbrella of symptoms and phenotypes often lead to misdiagnosis, resulting in delayed initiation of appropriate treatments [9, 10]. Current therapeutic approaches rely mainly on managing and preventing manic and depressive episodes with mood stabilizers, adjunctive antipsychotics, and/or antidepressants; however, long-term treatment is still challenging and with limited effectiveness [11]. Hence, it is of great relevance for BD management that new pharmacotherapies are developed, aiming to stabilize mood, restrain disease progression, protect against neurodegeneration, minimize dangerous behavior and suicide attempts, attenuate side effects, increase life expectancy, and improve overall quality of life.
From the neurobiological perspective, the purinergic system has gained considerable attention given that adenosine and adenosine 5′-triphosphate (ATP) are signaling molecules that modulate neurotransmission and neuroinflammation pathways linked to behavioral and mood regulation mechanisms relevant for BD [12]. Therefore, in this review we explore the role of purinergic signaling in BD pathophysiology and provide an overview of current and potential new purinergic targets for drug development.
2 Purinergic System in the CNS
ATP is a nucleotide stored intracellularly, and its signaling is vital for the energy production of all cellular processes. ATP reaches the extracellular space by different mechanisms, including: (1) Ca2+-dependent exocytosis [13]; (2) connexin hemichannels and pannexin channels, according to its concentration gradient; (3) cell membrane damage from injured cells [14]; and (4) P2X7 receptor (P2X7R)-induced transmembrane pore after sustained activation. The latter mechanism, however, is still debated [15, 16]. In the central nervous system (CNS), ATP can be physiologically released from neurons [17], astrocytes [18], and microglial cells [19] by exocytosis. In addition, ATP is classified as a neurotransmitter and can also be co-released with acetylcholine, noradrenaline, GABA, dopamine, and glutamate [20, 21].
Extracellular ATP acts on purinergic receptors P2X (P2XR) and P2Y (P2YR), inducing several intracellular signaling cascades. P2X(1-7)R are ionotropic receptors that elicit Ca2+ and Na+ influx, and K+ efflux under activation [22]. P2XR can occur as homomeric or heteromeric assemblies and consist of three subunits [22]. P2Y(1, 2, 4, 6, 11, 12, 13 or 14)R are metabotropic G-protein-coupled receptors sensitive to ATP, adenosine 5′-diphosphate (ADP), uridine 5′-tri- or diphosphate (UTP or UDP, respectively), or UDP-glucose, which will either activate or inhibit adenylyl cyclase, or activate phospholipase C [23]. These receptors are present in neurons, astrocytes, microglial cells, and oligodendrocytes [23]. In the brain, the majority of P2XR and P2YR are expressed in the hippocampus where they can regulate glutamate release [24]. The P2Y1R activation induces dopamine release in the rat striatum [25], the medial prefrontal cortex, and the nucleus accumbens [26]. The P2X7R activation also facilitates glutamate, GABA, and nitric oxide release [27,28,29,30], and negatively modulates serotonin levels [31]. It also regulates N-methyl-d-aspartate receptor (NMDAR) expression and basal levels of brain-derived neurotrophic factor in the hippocampus.
ATP is hydrolyzed into ADP, adenosine 5'-monophosphate (AMP), and adenosine by ectoenzymes that precisely control extracellular purine concentration. These cell surface enzymes are part of the family named ectonucleotidases, which mainly comprises the ecto-nucleoside triphosphate diphosphohydrolases (ENTPDases), pyrophosphohydrolases/phosphodiesterases (NPP), and ecto-5′-nucleotidase. ENTPD1, 2, and 3 (also known as CD39, CD39L2, and CD39L3, respectively) hydrolyze ATP and ADP into AMP [32]. NPPs hydrolyze ATP directly into AMP, generating pyrophosphate [33]. The final ectonucleotidase in the chain, ecto-5′-nucleotidase (also known as CD73), hydrolyzes AMP into adenosine [33]. Adenosine is inactivated by adenosine deaminase (ADA), generating inosine, which is further metabolized into hypoxanthine, xanthine, and uric acid (UA) (Fig. 1a). Inosine can modulate inflammation, neuroprotection, pain, and cognition [34], while UA is associated with sleep, locomotion, cognition, impulsivity, and mood [35,36,37]. Remarkably, this fine-tuning regulation by ectonucleotidases is strictly necessary as both ATP and adenosine can act as neuromodulators and frequently have counteracting effects.
Purinergic signaling in bipolar disorder (BD). a Overview of physiological purine metabolism. Adenosine 5′-triphosphate (ATP) is hydrolyzed by ectonucleoside triphosphate diphosphohydrolases (ENTPDases) or ecto-nucleoside pyrophosphohydrolases/phosphodiesterases (NPPs) into adenosine 5'-monophosphate (AMP), which is hydrolyzed into adenosine (ADO) by ecto-5′-nucleotidase. Adenosine deaminase (ADA) converts adenosine into inosine (INO), further metabolized into hypoxanthine (HXAN), xanthine (XAN), and uric acid (UA). b Proposed mechanisms in purinergic dysfunction contributing to BD pathophysiology. It is described that P2X7 receptor (P2X7R) activation drives neuroinflammation, oxidative stress, and gliosis in preclinical studies. Few reports scrutinized the direct role of P1 receptors in BD; however, it is known that A1 receptor (A1R) is primarily neuroprotective and its activation promotes an antidepressant-like effect, whereas A2A receptor (A2AR) is mainly proinflammatory and its inhibition may promote impulsivity, which can be associated with suicidal behavior. A1R-A2AR heteromeric interaction modulates glutamate activity and induces hyperactivation of N-methyl-d-aspartate receptor (NMDAR), which is exacerbated in BD pathology. Additionally, heteromeric formation between adenosine A2A and dopamine D2 receptors (A2AR-D2R) in basal ganglia regulates corticostriatal dopamine neurotransmission, which is hyperactive in patients with BD. c P2X7R single nucleotide polymorphisms (SNPs) associated with BD. The SNP rs208294 promotes gain of function of the P2X7R, and is associated with familial BD, increased illness time, and comorbidities with other mood disorders. The SNP rs3751143 promotes loss of function of P2X7R, and patients with BD possess the allele that preserves P2X7R function. d Proposed purinergic-based treatments for BD. Allopurinol is a promising therapeutic strategy; it can decrease UA levels and increase ADO availability, both dysregulated in patients with BD. Dipyridamole also acts on rising ADO levels and consequently modulates P1 receptors, showing beneficial effects in patients with BD. P2X7R antagonism has been proven effective in preclinical studies, and there are promising novel P2X7R antagonists able to cross the blood–brain barrier that could be explored in clinical trials. − indicates lower levels compared to healthy controls, = indicates equal levels compared to healthy controls, + indicates a subtle increase in levels compared to healthy controls, ++ indicates a moderate increase in levels compared to healthy controls, +++ indicates a high increase in levels compared to healthy controls, DA dopamine, ENT equilibrative nucleoside transporter, MDD major depressive disorder, NT5E ecto-5′-nucleotidase, PNP purine nucleoside phosphorylase, XO xanthine oxidase. Figure created with BioRender.com
Adenosine, in its turn, exerts multiple brain functions through the adenosine/P1 receptors, which are classified as A1R, A2AR, A2BR, and A3R. Adenosine receptors are metabotropic G-protein-coupled receptors that mainly activate or inhibit adenylyl cyclase [38]. The A1R is the most abundant P1 receptor expressed in the CNS [38]. Adenosine is well known for exerting neuroprotective properties in the CNS, mediated by A1R activation and A2AR inhibition [39]. The A2AR also mediates several essential functions in brain homeostasis, such as neurotransmitter release. A2AR is mainly expressed in dopaminergic areas, such as the striatum, nucleus accumbens, and olfactory tuberculum [38]. In the striatopallidal GABAergic neurons in the striatum, A2AR interacts with the dopamine D2 receptor (D2R), forming a heterodimer that results in decreased D2R affinity to dopamine when A2AR is activated [40] (Fig. 1b). Moreover, it is well accepted that adenosine can modulate spontaneous locomotor activity through striatal A2AR that interacts with D2R and dopamine D1 receptor (D1R) of the mesolimbic dopamine circuits [41,42,43]. In addition, A2AR interact with metabotropic glutamate 5 receptor in the striatum [44, 45] and hippocampus [46]. A2AR stimulation also facilitates glutamate release [39] and GABA release [47] from the hippocampus [48], whereas A1R counteracts A2AR effects by inhibiting glutamatergic neurotransmission [49, 50]. As adenosine receptors interact and modulate glutamate and dopamine receptor activity, pathological adenosinergic signaling has become a relevant hypothesis for psychiatric disorders [51,52,53], especially BD and schizophrenia [54,55,56].
Both ATP and adenosine are immunomodulators that act during brain inflammatory processes in opposite directions [57]. ATP acts as a damage-associated molecular pattern (DAMP) when released by injured or stressed cells, triggering proinflammatory cascades [58, 59], whereas adenosine acts as an immunosuppressant [60]. As a DAMP, ATP activates nuclear factor-κB signaling and consequently upregulates proinflammatory cytokines and NOD-, LRR-, and pyrin domain-containing protein 3 (NLRP3) inflamassome [61]. P2X7R activation is an essential step in the NLRP3 cascade. It activates caspase-1 and converts pro-interleukin-1β and pro-interleukin-18 into their mature forms, increasing their release [61, 62]. The microglial P2X7R is the major known modulator of inflammation among P2 receptors. Its activation by millimolar ATP concentration elicits proinflammatory and immunostimulatory effects, promoting the production and release of proinflammatory cytokines, including interleukin-1β, interleukin-6, and tumor necrosis factor [57, 63]. This effect activates microglial cells and induces the release of additional ATP to the extracellular space. As a feedback loop, exacerbated ATP levels in the extracellular space will establish an excitotoxic microenvironment [64]. Consequently, primarily via P2X7R activation, the purinergic system has been strongly associated with neurodegenerative processes and neuropsychiatric disorders with a neuroinflammatory and excitotoxic component, including BD [51, 65].
3 Pathophysiology and Treatment Strategies for BD
3.1 ATPergic Signaling and Genetic Predisposition to BD
The P2X7R has emerged as a promising target to study the genetic predisposition in BD as its gene is highly polymorphic [66]. Genome-wide association studies have identified the region 12q23-q24 as a locus with genes influencing susceptibility to BD [67,68,69]. Furthermore, P2X7R and P2X4R genes are located on chromosome 12 in close proximity, at 12q24.31 and 12q24.32, respectively [66, 70]. Similar functions that trigger proinflammatory cascades [71] and evidence for a P2X4-P2X7 heteromeric formation were found [72, 73], although this association is still questioned [74, 75].
A massive effort has been directed to understand the role of P2X7R single nucleotide polymorphisms (SNPs) in BD. However, the current evidence for the involvement of the majority of the studied targets is controversial, including the P2X7R SNP rs2230912 [76,77,78,79,80,81,82,83] and rs1718119 [84]. A study conducted with British individuals did not detect any association between nine promising P2X7R SNPs (rs591874, rs208293, rs1186055, rs208298, rs503720, rs1718133, rs1718119, rs2230912, and rs1621388) and BD susceptibility [80]. P2X7R SNPs that have not been refuted yet are the rs208294 and the rs3751143. The rs208294 coding for His155Tyr promoted the gain of function of the P2X7R. It was associated with familial major depressive disorder (MDD) and BD, including increased illness time and comorbid anxiety, alcoholism, psychotic symptoms, and suicide attempts [78]. On the contrary, the rs3751143 coding for Glu496Ala promoted the loss of function of the P2X7R. The decreased 1513C allele frequency and the tendency of increased 1513 AA/AC genotype were found in patients with BD, suggesting that P2X7R functionality is preserved in these patients compared to healthy individuals [85] (Fig. 1c). Linkage disequilibrium, functional effects, and haplotype block structure (regions with high linkage disequilibrium) might explain these controversial findings within the genome [86]. Some authors have described haplotype blocks in the P2X7R gene [66, 87], which might partially explain the failure of previous association studies. Nevertheless, preclinical studies strongly support the beneficial effect of the P2X7R inhibition, which will be discussed in the upcoming sections.
To our knowledge, no studies have found an association between functional SNPs in the P2X4R gene and BD susceptibility [76]. Furthermore, no preclinical or clinical study directly evaluated the modulation of P2X4R in BD. Nonetheless, growing preclinical evidence indicates the role of P2X4R in modulating dopamine transmission. Mice deficient in the P2X4R gene presented with increased striatal tyrosine hydroxylase, dopamine transporter, and D1R and D2R expression. Remarkably, both deletion and activation of the P2X4R induced impairment in prepulse inhibition, whereas selective D1R and D2R antagonists reverted this deficit [88, 89].
Moreover, P2X4R knockout mice also exhibit alterations in the subunit expression of glutamate receptors, such as NMDAR and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors, and GABAA receptors in several brain regions [90, 91]. Behaviorally, other reports corroborate that P2X4R knockout mice present deficits in sensorimotor gating and social behavior, including increased ethanol intake [90, 91]; however, no anxiety-like behavior or altered locomotor activity were found [90]. In addition, a recent study showed that increased P2X4R density in the knock-in mice hippocampus induced synaptic deficits, anxiolytic-like behaviors, and impaired spatial memory processing [92]. Corroborating these findings, ivermectin, a potent P2X4R positive allosteric modulator, induced anxiolytic-like and depressive-like behaviors in mice [93]. These data support the hypothesis that P2X4R may modulate dopaminergic, glutamatergic, and GABAergic neurotransmission, suggesting its participation in reward mechanisms and ethanol abuse with particular relevance to BD pathogenesis and progression.
3.2 The Purinergic Hypothesis for BD: A Look Into Hyperuricemia
Whilst the purinergic hypothesis for BD has been mostly explored in the past two decades after being revisited by Machado-Vieira et al. [94], the link between components of the purinergic system and mood fluctuation was described more than a century ago [95]. The first insights date from 1846 owing to the accidental discovery of lithium salts as mood stabilizers for patients with gout and hyperuricemia, which are conditions known by the increased levels of peripheral UA [95]. Elevated amounts of UA were then firstly reported in 1968 by Anumonye et al. in the urine, but not in the blood, of patients with BD, including those receiving lithium treatment [96].
Current knowledge indicates that blood levels of UA in patients with BD, during mania, depression, or remission, are higher than in healthy controls [97] (Fig. 1d). While higher levels of peripheral UA are associated with manic and hypomanic episodes, lower levels are observed during depressive episodes [98,99,100,101]. Still, a decrease in UA levels during mania indicates lower severity of the episode; however, such a correlation was not observed during a depressive episode, as measured by the Young Mania Rating Scale and Hamilton Depression Rating Scale, respectively [97]. Of note, patients with MDD have shown the lowest levels of UA when compared to patients with BD or healthy subjects. These findings indicate an emerging role of UA as a biomarker for BD [102], potentially able to distinguish BD and MDD [103,104,105,106]. However, notwithstanding the current evidence, the UA-based discrimination between BD phases or between BD and MDD was only partially supported when further analyzed using a meta-analytical approach [107].
UA levels are also enhanced in metabolic syndrome, a prevalent (approximately 37%) comorbidity in patients with BD, especially in those receiving antipsychotic treatment [108,109,110]. Still, the effect of BD on hyperuricemia seems mostly direct, being only partially mediated by metabolic abnormalities [111]. From the pharmacotherapy perspective, psychotropic and antipsychotic drugs commonly considered in the psychiatric clinic for BD management might have different effects on serum UA levels. For example, it has been shown that lithium [96], carbamazepine [112], phenytoin [112], aripiprazole [113], a combination of zotepine and mood stabilizers (lithium or sodium valproate) [114], and a combination of quetiapine and sodium valproate [115] are likely to reduce peripheral UA levels. In contrast, sodium valproate monotherapy [112], phenobarbital [112], haloperidol [116], and risperidone [117] may increase UA levels.
3.3 Adenosinergic Dysfunction and Its Impact on Other Neurotransmission Systems
Increased UA levels might reflect an abnormal purine turnover with a consequent reduction in adenosine levels [36]. Peripheral adenosine levels were found reduced in patients with BD during the euthymic phase, with lower levels linked to higher functional impairment [118]. The authors suggested that, at low levels, adenosine would not exert its neuroprotective role, possibly impacting immune response and neuroinflammation [118].
The purinergic system, mainly via adenosine, can also regulate circadian rhythms, modulating the physiological response to light [53, 119]. It has been recently proposed that downstream signaling of A1R and A2AR antagonism controls clock genes PER1 and PER2 activity both in vitro and in vivo via Ca2+-extracellular-regulated kinase-AP-1 pathway [119]. Although the causal mechanisms involved in the connection between circadian rhythm disruption and mood disorders are yet to be reasoned [120], sleep cycle impairment is highly prominent in most patients with BD, being clinically associated with disease onset and development [121,122,123,124,125,126]. Thus, further understanding on the role of adenosinergic signaling in the context of mood control can be an attractive approach with potential therapeutic implications for BD.
Most evidence of adenosine receptor dysregulation in mood disorders comes from MDD [53, 127]. Their role in BD can be hypothesized from the therapeutic effect of carbamazepine, the first anti-seizure drug used for BD back in the 1970s. Carbamazepine is currently considered a second-line mood stabilizer with limited applicability for treating acute mania and mixed episodes or for maintenance and preventive therapy [128,129,130,131]. Its mechanism of action includes the antagonism of A1R, which results in long-term mRNA upregulation and an increased number of A1R receptors. This was shown to directly potentiate phospholipase C activity in primary astrocytes isolated from low-rich adenosinergic regions of the rat brain [132]. Of note, A1R activation has proven to exert antidepressant-like effects in preclinical studies, potentially linked to glutamatergic modulation [53, 133].
As mentioned above, adenosine-mediated neuroprotection is mainly attributed to A1R activation and A2AR blockade [39]. The evidence of the A1R-A2AR heterodimer formation on striatal glutamatergic terminals [134] raises attention to the regulatory effect of different concentrations of adenosine over glutamate-mediated excitatory activity, which is enhanced in patients with BD [135] (Fig. 1b). A dopaminergic signaling imbalance has also been extensively discussed as a major contributor to mood alterations, especially in BD [136]. The capability of adenosine receptors to form heterodimers with dopamine receptors becomes especially relevant in this context, as A2AR-D2R heterodimers in the basal ganglia regulate corticostriatal dopamine neurotransmission, found hyperactive in patients with BD [137, 138] (Fig. 1b). Adenosine-dopamine might also interact to modulate glutamatergic neurons in the hippocampus [53], although there is no evidence pointing to such a mechanism specifically in BD. The most promising hypothesis by which adenosinergic-dopaminergic interactions might control mood suggests the balance between excitatory (glutamate) and inhibitory (GABA) neurotransmission along with heteromeric formation, as recently reviewed [127]. Further research is still necessary to determine any mechanistic causality and clinical relevance and applicability of targeting adenosinergic-dopaminergic heteromers as a therapeutic approach for BD.
Finally, one of the clinical features of BD that has received less attention from the molecular perspective is the substantially increased suicide risk among patients. It is expected that 30–50% of patients with BD will attempt suicide once in their lifetime, and 15–20% will commit suicide [139]. Although there is a lack of evidence directly linking purinergic signaling to suicidal behavior, some hypotheses have been recently proposed. A reduction in adenosinergic signaling through the inhibition of A2AR is thought to play a role in suicidal behavior by promoting impulsivity, a common trait in patients with BD [140]. Interestingly, UA levels have also been positively correlated with impulsive traits during a manic episode [100]. An expanded hypothesis has also proposed a role for neuroinflammation and glutamate-derived excitotoxicity mediated by P2X7R activation and A1R-A2AR heterodimer response to accumulated adenosine resulting from hyperactivation of the NMDAR and decreased activity of the enzyme ADA [141].
4 Current Therapeutic Strategies for BD Targeting the Purinergic Signaling
4.1 Lithium, The Gold Standard Mood Stabilizer
Lithium is still the first-line therapy for BD, even with its mechanism of action remaining only partially understood [142, 143]. A systematic review and meta-analysis, including seven clinical trials reports on the efficacy and effectiveness of lithium, revealed that it remains the most efficient long-term treatment option for preventing overall mood switches, especially for managing manic episodes [144]. Purinergic signaling has been suggested as one of the systems mediating the biological effects of lithium, either as a neuroprotective or a nephrotoxic drug [145,146,147,148]. It was previously shown that lithium increases ATP and AMP hydrolysis, and is neuroprotective against ATP-induced cellular death by acting on P2X7R in rat hippocampal slices [149]. More recently, an in vitro study conducted in murine neuronal and microglial cell lines corroborated the neuroprotective action of lithium against ATP-induced cell death and revealed a neuronal rather than a microglial response for this effect [145]. Molecular studies using a multinuclear, multi-dimensional, solid-state, nuclear magnetic resonance approach have shown that lithium binds to ATP [150, 151], suggesting a direct mode of action via a lithium-ATP complex in which its consequences should be further explored in vitro and in vivo.
4.2 The P2X7R Antagonism
P2X7R antagonism has been shown as a promising BD therapeutic candidate in preclinical models of mania. In addition to the translational limitations of modeling bipolar disorder in animals, amphetamine-induced hyperactive locomotion is still the most accepted and widely used model to mimic manic-like behavior, helping with the investigation of the molecular basis of mania. Both the pharmacological blockade and the genetic deletion of the P2X7R were demonstrated to be effective in preventing the hyperlocomotion induced by amphetamine [152,153,154,155]. Still, it was demonstrated that this receptor plays a role in the sustained neuroinflammation observed in a preclinical model of mania [152], and the observed behavioral effects on amphetamine-induced hyperlocomotion might be via dopaminergic and astrogliosis modulation [153] (Fig. 1d).
Despite the preclinical potential herein described, to our knowledge, there is no clinical trial currently investigating antagonists of P2X7R in patients with BD. The slow progression in this field might be due to the inherent challenges to developing brain penetrant P2X7R antagonists [155,156,157,158]. A few compounds have been identified, including JNJ-54175446 [159] and JNJ-55308942 [160], as well as P2X7R positron emission tomography-computed tomography-identified ligands, which can potentially accelerate the transition into clinical drug development for neuropsychiatric disorders [161]. The first investigational P2X7R antagonists have completed phase I trials. In a randomized single-ascending dose study in 77 healthy human subjects, JNJ-54175446 in doses from 0.5 to 600 mg showed a safe and successful dose-dependent response, attenuating the P2X7R-mediated interleukin-1β release from isolated peripheral blood cells (indicating P2X7R antagonism) [162]. The compound demonstrated a robust brain target engagement by using positron emission tomography imaging for P2X7R [163]. In addition, by using an oral dexamphetamine challenge model in 64 healthy male individuals in a randomized, double-blind, placebo-controlled, multiple ascending dose trial for the P2X7R antagonist JNJ-54175446, it was demonstrated that this compound was well tolerated and effective in suppressing ex vivo lipopolysaccharide-induced release of cytokines (an indicator of P2X7R antagonism). A proof-of-concept study also showed increased locomotion and mood-elevating effects of 50–450 mg JNJ-54175446 administration over a baseline oral dexamphetamine (20 mg) challenge paradigm in a randomized, double-blinded, placebo-controlled, multiple ascending dose, crossover trial in 64 healthy male subjects [164]. The potential mood-modulating outcome observed can be considered of great relevance in the context of BD, although no specific trial addressing these patients has been proposed yet. Additionally, future trials should seek stronger external validity, enlarging the sample size, and minimizing stratification per age, sex, or other unjustified exclusion criteria.
Taken together, these studies reveal an interesting potential for clinical antagonism of P2X7R, which has been explored in different CNS disorders, such as amyotrophic lateral sclerosis [165] and MDD. A randomized, placebo-controlled, double-blind trial is currently recruiting patients with MDD to primarily evaluate the effect of 50 mg/day JNJ-54175446 on depressive symptoms scores after 8 weeks of treatment compared to baseline (ClinicalTrials.gov Identifier: NCT04116606).
However, to our knowledge, no ongoing clinical trials are being conducted with any of the novel compounds for BD. At this stage, we can only speculate on the reasons: one possibility is related to pharmaceutical interests, given that MDD is still the most disabling psychiatric disease causing substantial social and economic impact; other than that it might also rely on the fact that the current evidence supporting the role of P2X7R in mood disorders is much more robust towards MDD. This should be taken as an encouragement for further investigation and validation of emerging hypotheses addressing BD through a purinergic perspective.
4.3 The Adenosine and UA Balance
Notably, drugs that increase adenosine levels, such as dipyridamole and allopurinol, have been investigated as adjuvant purinergic modulators for the treatment of BD [54, 166]. Dipyridamole is an antiplatelet and antithrombotic drug with a complex mechanism of action, including the inhibition of cellular adenosine reuptake [167, 168]. Allopurinol, in its turn, is an urate-lowering drug primarily acting in decreasing purine degradation through the inhibition of xanthine oxidase, thus treating hyperuricemia (high UA levels) [169]. Allopurinol has been used in different clinical contexts that include: (1) the management of patients with signs and symptoms of primary or secondary gout (acute attacks, tophi, joint destruction, UA lithiasis, and/or nephropathy) [170]; (2) the management of patients with leukemia, lymphoma, and malignancies who are experiencing elevations of serum and urinary UA levels due to the cancer therapy [171]; and (3) the management of patients with recurrent calcium oxalate kidney and urinary calculi whose daily UA excretion exceeds 800 mg/day in male patients and 750 mg/day in female patients [172, 173]. Although no direct evidence has confirmed a causal correlation, an allopurinol-driven UA reduction is thought to result in increased adenosine levels [54].
The first case report exploring the therapeutic potential of allopurinol in BD found an improvement in manic symptoms and a decrease in peripheral UA levels in two treatment-resistant patients with mania associated with hyperuricemia [174]. A double-blind, randomized, placebo-controlled trial including 41 patients with BD with moderate-to-severe mania evaluated the effect of allopurinol (300 mg/day), lithium, and haloperidol compared to placebo for 8 weeks, observing an improvement of manic symptoms induced by allopurinol [175]. Similarly, a double-blind, randomized, placebo-controlled study investigated the use of a higher dose of allopurinol (600 mg/day, n = 60) and dipyridamole (200 mg/day, n = 60) compared to placebo (n = 60) in addition to lithium for 4 weeks. This study demonstrated that allopurinol not only improves manic symptoms in comparison to dipyridamole and placebo, but also correlates with decreased plasma UA levels [176]. Likewise, 50 in-patients with acute mania received allopurinol (600 mg/day) or placebo in addition to sodium valproate (15–20 mg/kg) for 4 weeks in a randomized, placebo-controlled, double-blind trial, resulting in a similar antimanic action of allopurinol that was correlated with UA levels [177] (Fig. 1d).
In contrast, a nation-wide population-based longitudinal study in Denmark used a regression analysis to investigate new drug candidates for BD but no association between allopurinol and a positive outcome was found [178]. Additionally, a small double-blind, randomized, placebo-controlled trial pilot on 27 patients with BD investigated the addition of allopurinol or placebo to the BD standard treatments [179]. The study did not find any effect of allopurinol on manic symptoms but revealed a greater therapeutic response in patients restricted to caffeine [179]. These findings suggest that caffeine intake should be both better monitored and specifically addressed in future studies involving adenosinergic compounds for mood [179]. In addition, a large multi-center placebo-controlled trial performed with 180 patients with BD in acute manic episodes over 6 weeks with allopurinol (300 mg/day) or placebo added to the standard BD treatment also showed no antimanic effect of allopurinol [180]. However, it is essential to note that these two studies share a few limitations, including the heterogeneity of the concurrent treatment that patients were submitted to, which makes isolating the effect of allopurinol challenging. Furthermore, it should be considered that Fan et al. had a very small sample size [179] and Weiser et al. used the lowest dose of allopurinol [180], which might have limited the efficacy of the drug.
Nevertheless, a systematic review and meta-analysis have combined all the randomized controlled trials that used allopurinol and dipyridamole as adjuvant therapies in BD. This study promisingly revealed an overall significant reduction in manic symptoms in participants receiving the purinergic modulators compared with placebo [54] (Fig. 1d). Subsequently, further systematic reviews and meta-analyses of randomized controlled trials focusing on allopurinol administration revealed a small-to-moderate effect size along with existent but limited beneficial effects of allopurinol as an add-on treatment for BD [181, 182]. It must be critically observed that the efficacy might be related to the primary antimanic medication regimen, with lithium showing the most promising combination [182]. Finally, a recent meta-review and critical appraisal of the existing meta-analyses of randomized placebo-controlled trials have classified the current evidence as of low quality, confirming a higher efficacy of allopurinol over placebo on attenuating manic symptoms [183]. Considering the limited evidence so far, the potential benefit of allopurinol as an adjunctive treatment for mania requires further investigation.
5 Limitations and Future Perspectives
The literature here discussed pointing to the role of purinergic signaling in BD pathophysiology and highlighting new potential therapeutic targets for drug development still relies mostly on basic and preclinical research. While in vitro studies bring to light cellular and molecular mechanisms involved in specific pathophysiological pathways linked to BD, their overall health impact and clinical relevance in the psychiatric clinic must be taken as minimal. Similarly, animal models are extremely limited in capturing the complexity of human diseases, particularly psychiatric disorders. Current animal models of mania fail on mimicking hypomanic and cycling states, and are mostly based on hyperlocomotion behavior, whereas manic behavior in humans is much more complex and involves several psychosocial, cognitive, and emotional facets. In addition, the difficulty of assertively assessing the neurobiological traits that distinguish bipolar depression from unipolar depression in preclinical models also limits the applicability and efficacy of potential drugs designed to target general aspects of a depressive episode in BD.
With these limitations in mind, the new generation of P2X7R antagonists configures the most promising new phase of accelerated discoveries to either monotherapies or adjunctive therapies for BD and related disorders that affect the CNS. The use of allopurinol as an add-on therapy for BD, while promising and relatively well explored, still has many roadblocks associated with study design, heterogeneity of primary BD medication, as well as the doses and length of administration, limiting consistent conclusions from being drawn. Future research should focus on additional well-designed translational approaches, with more robust and clinically-oriented preclinical studies followed by randomized multi-center clinical trials with larger sample sizes. Special attention should be directed towards identifying biomarkers for BD to be used both as diagnostic tools and disease-specific targets for drug development. Notably, new methods to manage suicidal behavior, neuroinflammation, and neurotransmission imbalance, especially dopaminergic dysfunction, are of great relevance for BD.
6 Conclusions
Although limited clinical data are currently available, extensive basic and preclinical research points to the purinergic system as an important modulator of mood in the context of BD. Here, we highlighted a few promising purinergic targets and compounds to be further explored, including the modulation of P2X4R, A1R, A2AR, and P2Y1R. We encourage future research aiming to clarify the applicability, safety, and efficacy of current and new purinergic-targeting candidates such as allopurinol, adenosinergic compounds, and the novel P2X7R antagonists as therapeutic approaches for BD.
References
Price JL, Drevets WC. Neurocircuitry of mood disorders. Neuropsychopharmacology. 2010;35:192–216. https://doi.org/10.1038/NPP.2009.104.
Scaini G, Valvassori SS, Diaz AP, Lima CN, Benevenuto D, Fries GR, et al. Neurobiology of bipolar disorders: a review of genetic components, signaling pathways, biochemical changes, and neuroimaging findings. Braz J Psychiatry. 2020;42:536–51. https://doi.org/10.1590/1516-4446-2019-0732.
Maletic V, Raison C. Integrated neurobiology of bipolar disorder. Front Psychiatry. 2014;5:98. https://doi.org/10.3389/FPSYT.2014.00098.
Sigitova E, Fišar Z, Hroudová J, Cikánková T, Raboch J. Biological hypotheses and biomarkers of bipolar disorder. Psychiatry Clin Neurosci. 2017;71:77–103. https://doi.org/10.1111/PCN.12476.
Nurnberger JI, Koller DL, Jung J, Edenberg HJ, Foroud T, Guella I, et al. Identification of pathways for bipolar disorder: a meta-analysis. JAMA Psychiat. 2014;71:657–64. https://doi.org/10.1001/JAMAPSYCHIATRY.2014.176.
Kim Y, Santos R, Gage FH, Marchetto MC. Molecular mechanisms of bipolar disorder: progress made and future challenges. Front Cell Neurosci. 2017;11:30. https://doi.org/10.3389/fncel.2017.00030.
GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137–50. https://doi.org/10.1016/S2215-0366(21)00395-3.
Rosa AR, Sánchez-Moreno J, Martínez-Aran A, Salamero M, Torrent C, Reinares M, et al. Validity and reliability of the Functioning Assessment Short Test (FAST) in bipolar disorder. Clin Pract Epidemiol Ment Health. 2007;3:5. https://doi.org/10.1186/1745-0179-3-5.
Perlis RH. Misdiagnosis of bipolar disorder. Am J Manag Care. 2005;11:S271–4.
Patel R, Shetty H, Jackson R, Broadbent M, Stewart R, Boydell J, et al. Delays before diagnosis and initiation of treatment in patients presenting to mental health services with bipolar disorder. PLoS ONE. 2015;10: e0126530. https://doi.org/10.1371/JOURNAL.PONE.0126530.
Fountoulakis KN, Kasper S, Andreassen O, Blier P, Okasha A, Severus E, et al. Efficacy of pharmacotherapy in bipolar disorder: a report by the WPA section on pharmacopsychiatry. Eur Arch Psychiatry Clin Neurosci. 2012;262(Suppl. 1):1–48. https://doi.org/10.1007/S00406-012-0323-X.
Jones GH, Vecera CM, Pinjari OF, Machado-Vieira R. Inflammatory signaling mechanisms in bipolar disorder. J Biomed Sci. 2021;28:45. https://doi.org/10.1186/s12929-021-00742-6.
Arcuino G, Lin JHC, Takano T, Liu C, Jiang L, Gao Q, et al. Intercellular calcium signaling mediated by point-source burst release of ATP. Proc Natl Acad Sci USA. 2002;99:9840–5. https://doi.org/10.1073/PNAS.152588599.
Illes P, Burnstock G, Tang Y. Astroglia-derived ATP modulates CNS neuronal circuits. Trends Neurosci. 2019;42:885–98. https://doi.org/10.1016/J.TINS.2019.09.006.
Di Virgilio F, Schmalzing G, Markwardt F. The elusive P2X7 macropore. Trends Cell Biol. 2018;28:392–404. https://doi.org/10.1016/J.TCB.2018.01.005.
Pelegrín P. Many ways to dilate the P2X7 receptor pore. Br J Pharmacol. 2011;163:908–11. https://doi.org/10.1111/J.1476-5381.2011.01325.X.
Pankratov Y, Lalo U, Verkhratsky A, North RA. Vesicular release of ATP at central synapses. Pflugers Arch. 2006;452:589–97. https://doi.org/10.1007/s00424-006-0061-x.
Zhang Z, Chen G, Zhou W, Song A, Xu T, Luo Q, et al. Regulated ATP release from astrocytes through lysosome exocytosis. Nat Cell Biol. 2007;9:945–53. https://doi.org/10.1038/ncb1620.
Imura Y, Morizawa Y, Komatsu R, Shibata K, Shinozaki Y, Kasai H, et al. Microglia release ATP by exocytosis. Glia. 2013;61:1320–30. https://doi.org/10.1002/GLIA.22517.
Burnstock G. Introduction to purinergic signalling in the brain. Adv Exp Med Biol. 2020;1202:1–12. https://doi.org/10.1007/978-3-030-30651-9_1.
Burnstock G. Historical review: ATP as a neurotransmitter. Trends Pharmacol Sci. 2006;27:166–76. https://doi.org/10.1016/j.tips.2006.01.005.
Burnstock G, Kennedy C. P2X receptors in health and disease. Adv Pharmacol. 2011. https://doi.org/10.1016/B978-0-12-385526-8.00011-4.
Jacobson KA, Delicado EG, Gachet C, Kennedy C, von Kügelgen I, Li B, et al. Update of P2Y receptor pharmacology: IUPHAR Review 27. Br J Pharmacol. 2020;177:2413–33. https://doi.org/10.1111/BPH.15005.
Rodrigues R, Almeida T, Richardson PJ, Oliveira CR, Cunha RA. Dual presynaptic control by ATP of glutamate release via facilitatory P2X1, P2X2/3, and P2X3 and inhibitory P2Y1, P2Y2, and/or P2Y4 receptors in the rat hippocampus. J Neurosci. 2005;25:6286–95. https://doi.org/10.1523/JNEUROSCI.0628-05.2005.
Zhang YX, Yamashita H, Ohshita T, Sawamoto N, Nakamura S. ATP increases extracellular dopamine level through stimulation of P2Y purinoceptors in the rat striatum. Brain Res. 1995;691:205–12. https://doi.org/10.1016/0006-8993(95)00676-H.
Koch H, Bespalov A, Drescher K, Franke H, Krügel U. Impaired cognition after stimulation of P2Y1 receptors in the rat medial prefrontal cortex. Neuropsychopharmacology. 2015;40:305–14. https://doi.org/10.1038/NPP.2014.173.
Codocedo JF, Godoy JA, Poblete MI, Inestrosa NC, Huidobro-Toro JP. ATP induces NO production in hippocampal neurons by P2X(7) receptor activation independent of glutamate signaling. PLoS ONE. 2013;8: e57626. https://doi.org/10.1371/JOURNAL.PONE.0057626.
Papp L, Vizi ES, Sperlágh B. Lack of ATP-evoked GABA and glutamate release in the hippocampus of P2X7 receptor-/- mice. NeuroReport. 2004;15:2387–91. https://doi.org/10.1097/00001756-200410250-00017.
Sperlágh B, Köfalvi A, Deuchars J, Atkinson L, Milligan CJ, Buckley NJ, et al. Involvement of P2X7 receptors in the regulation of neurotransmitter release in the rat hippocampus. J Neurochem. 2002;81:1196–211. https://doi.org/10.1046/J.1471-4159.2002.00920.X.
Sperlágh B, Vizi ES, Wirkner K, Illes P. P2X7 receptors in the nervous system. Prog Neurobiol. 2006;78:327–46. https://doi.org/10.1016/J.PNEUROBIO.2006.03.007.
Csölle C, Baranyi M, Zsilla G, Kittel Á, Gölöncsér F, Illes P, et al. Neurochemical changes in the mouse hippocampus underlying the antidepressant effect of genetic deletion of P2X7 receptors. PLoS ONE. 2013;8: e66547. https://doi.org/10.1371/JOURNAL.PONE.0066547.
Robson SC, Sévigny J, Zimmermann H. The E-NTPDase family of ectonucleotidases: structure function relationships and pathophysiological significance. Purinergic Signal. 2006;2:430. https://doi.org/10.1007/S11302-006-9003-5.
Roszek K, Czarnecka J. Is ecto-nucleoside triphosphate diphosphohydrolase (NTPDase)-based therapy of central nervous system disorders possible? Mini Rev Med Chem. 2015;15:5–20. https://doi.org/10.2174/1389557515666150219114416.
Nascimento FP, Macedo-Júnior SJ, Lapa-Costa FR, Cezar-dos-Santos F, Santos ARS. Inosine as a tool to understand and treat central nervous system disorders: a neglected actor? Front Neurosci. 2021;15:703783. https://doi.org/10.3389/FNINS.2021.703783/BIBTEX.
Lorenzi TM, Borba DL, Dutra G, Lara DR. Association of serum uric acid levels with emotional and affective temperaments. J Affect Disord. 2010;121:161–4. https://doi.org/10.1016/J.JAD.2009.05.023.
Ortiz R, Ulrich H, Zarate CA, Machado-Vieira R. Purinergic system dysfunction in mood disorders: a key target for developing improved therapeutics. Prog Neuropsychopharmacol Biol Psychiatry. 2015;57:117–31. https://doi.org/10.1016/J.PNPBP.2014.10.016.
Sutin AR, Cutler RG, Camandola S, Uda M, Feldman NH, Cucca F, et al. Impulsivity is associated with uric acid: evidence from humans and mice. Biol Psychiatry. 2014;75:31–7. https://doi.org/10.1016/J.BIOPSYCH.2013.02.024.
Fields RD, Burnstock G. Purinergic signalling in neuron-glia interactions. Nat Rev Neurosci. 2006;7:423–36. https://doi.org/10.1038/nrn1928.
Cunha RA. Neuroprotection by adenosine in the brain: from A1 receptor activation to A2A receptor blockade. Purinergic Signal. 2005;1:111–34. https://doi.org/10.1007/S11302-005-0649-1.
Ferré S. Adenosine-dopamine interactions in the ventral striatum. Implications for the treatment of schizophrenia. Psychopharmacology. 1997;133:107–20. https://doi.org/10.1007/s002130050380.
Barraco RA, Martens KA, Parizon M, Normile HJ. Adenosine A2a receptors in the nucleus accumbens mediate locomotor depression. Brain Res Bull. 1993;31:397–404. https://doi.org/10.1016/0361-9230(93)90233-2.
Barraco RA, Coffin VL, Altman HJ, Phillis JW. Central effects of adenosine analogs on locomotor activity in mice and antagonism of caffeine. Brain Res. 1983;272:392–5. https://doi.org/10.1016/0006-8993(83)90591-7.
Collins LE, Galtieri DJ, Collins P, Jones SK, Port RG, Paul NE, et al. Interactions between adenosine and dopamine receptor antagonists with different selectivity profiles: effects on locomotor activity. Behav Brain Res. 2010;211:148–55. https://doi.org/10.1016/J.BBR.2010.03.003.
Domenici MR, Pepponi R, Martire A, Tebano MT, Potenza RL, Popoli P. Permissive role of adenosine A2A receptors on metabotropic glutamate receptor 5 (mGluR5)-mediated effects in the striatum. J Neurochem. 2004;90:1276–9. https://doi.org/10.1111/J.1471-4159.2004.02607.X.
Rodrigues RJ, Alfaro TM, Rebola N, Oliveira CR, Cunha RA. Co-localization and functional interaction between adenosine A2A and metabotropic group 5 receptors in glutamatergic nerve terminals of the rat striatum. J Neurochem. 2005;92:433–41. https://doi.org/10.1111/j.1471-4159.2004.02887.x.
Tebano MT, Martire A, Rebola N, Pepponi R, Domenici MR, Grò MC, et al. Adenosine A2A receptors and metabotropic glutamate 5 receptors are co-localized and functionally interact in the hippocampus: a possible key mechanism in the modulation of N-methyl-D-aspartate effects. J Neurochem. 2005;95:1188–200. https://doi.org/10.1111/J.1471-4159.2005.03455.X.
Cunha RA, Ribeiro JA. Purinergic modulation of [3H]GABA release from rat hippocampal nerve terminals. Neuropharmacology. 2000;39:1156–67. https://doi.org/10.1016/S0028-3908(99)00237-3.
Diógenes MJ, Fernandes CC, Sebastião AM, Ribeiro JA. Activation of adenosine A2A receptor facilitates brain-derived neurotrophic factor modulation of synaptic transmission in hippocampal slices. J Neurosci. 2004;24:2905–13. https://doi.org/10.1523/JNEUROSCI.4454-03.2004.
Lopes LV, Cunha RA, Kull B, Fredholm BB, Ribeiro JA. Adenosine A2A receptor facilitation of hippocampal synaptic transmission is dependent on tonic A1 receptor inhibition. Neuroscience. 2002;112:319–29. https://doi.org/10.1016/S0306-4522(02)00080-5.
Masino SA, Diao L, Illes P, Zahniser NR, Larson GA, Johansson B, et al. Modulation of hippocampal glutamatergic transmission by ATP is dependent on adenosine a(1) receptors. J Pharmacol Exp Ther. 2002;303:356–63. https://doi.org/10.1124/JPET.102.036731.
Cheffer A, Castillo ARG, Corrêa-Velloso J, Gonçalves MCB, Naaldijk Y, Nascimento IC, et al. Purinergic system in psychiatric diseases. Mol Psychiatry. 2018;23:94–106. https://doi.org/10.1038/mp.2017.188.
Pasquini S, Contri C, Merighi S, Gessi S, Borea PA, Varani K, et al. Adenosine receptors in neuropsychiatric disorders: fine regulators of neurotransmission and potential therapeutic targets. Int J Mol Sci. 2022;23:1219. https://doi.org/10.3390/ijms23031219.
van Calker D, Biber K, Domschke K, Serchov T. The role of adenosine receptors in mood and anxiety disorders. J Neurochem. 2019;151:11–27. https://doi.org/10.1111/JNC.14841.
Hirota T, Kishi T. Adenosine hypothesis in schizophrenia and bipolar disorder: a systematic review and meta-analysis of randomized controlled trial of adjuvant purinergic modulators. Schizophr Res. 2013;149:88–95. https://doi.org/10.1016/j.schres.2013.06.038.
Moody CL, Funk AJ, Devine E, Devore Homan RC, Boison D, McCullumsmith RE, et al. Adenosine kinase expression in the frontal cortex in schizophrenia. Schizophr Bull. 2020;46:690–8. https://doi.org/10.1093/schbul/sbz086.
Boison D, Singer P, Shen HY, Feldon J, Yee BK. Adenosine hypothesis of schizophrenia: opportunities for pharmacotherapy. Neuropharmacology. 2012;62:1527–43. https://doi.org/10.1016/j.neuropharm.2011.01.048.
Illes P, Rubini P, Ulrich H, Zhao Y, Tang Y. Regulation of microglial functions by purinergic mechanisms in the healthy and diseased CNS. Cells. 2020;9:1108. https://doi.org/10.3390/cells9051108.
Ratajczak MZ, Mack A, Bujko K, Domingues A, Pedziwiatr D, Kucia M, et al. ATP-Nlrp3 inflammasome-complement cascade axis in sterile brain inflammation in psychiatric patients and its impact on stem cell trafficking. Stem Cell Rev Rep. 2019;15:497–505. https://doi.org/10.1007/S12015-019-09888-1.
Franklin TC, Xu C, Duman RS. Depression and sterile inflammation: essential role of danger associated molecular patterns. Brain Behav Immun. 2018;72:2–13. https://doi.org/10.1016/J.BBI.2017.10.025.
Jin K, Mao C, Chen L, Wang L, Liu Y, Yuan J. Adenosinergic pathway: a hope in the immunotherapy of glioblastoma. Cancers. 2021;13:1–21. https://doi.org/10.3390/CANCERS13020229.
Bernier LP. Purinergic regulation of inflammasome activation after central nervous system injury. J Gen Physiol. 2012;140:575. https://doi.org/10.1085/JGP.201210875.
He Y, Taylor N, Fourgeaud L, Bhattacharya A. The role of microglial P2X7: modulation of cell death and cytokine release. J Neuroinflammation. 2017;14:135. https://doi.org/10.1186/S12974-017-0904-8.
Andrejew R, Oliveira-Giacomelli Á, Ribeiro DE, Glaser T, Arnaud-Sampaio VF, Lameu C, et al. The P2X7 receptor: central hub of brain diseases. Front Mol Neurosci. 2020;13:124. https://doi.org/10.3389/FNMOL.2020.00124/BIBTEX.
Gubert C, Fries GR, de Aguiar BW, Rosa AR, Busnello JV, Ribeiro L, et al. The P2X7 purinergic receptor as a molecular target in bipolar disorder. Neuropsychiatr Neuropsychol. 2013;8:1–7.
Burnstock G, Ulrich H. Purinergic signaling in embryonic and stem cell development. Cell Mol Life Sci. 2011;68:1369–94. https://doi.org/10.1007/s00018-010-0614-1.
Fuller SJ, Stokes L, Skarratt KK, Gu BJ, Wiley JS. Genetics of the P2X7 receptor and human disease. Purinergic Signal. 2009;5:257–62. https://doi.org/10.1007/S11302-009-9136-4.
Morissette J, Villeneuve A, Bordeleau L, Rochette D, Laberge C, Gagné B, et al. Genome-wide search for linkage of bipolar affective disorders in a very large pedigree derived from a homogeneous population in quebec points to a locus of major effect on chromosome 12q23-q24. Am J Med Genet. 1999;88:567–87.
Shink E, Morissette J, Sherrington R, Barden N. A genome-wide scan points to a susceptibility locus for bipolar disorder on chromosome 12. Mol Psychiatry. 2005;10:545–52. https://doi.org/10.1038/SJ.MP.4001601.
Curtis D, Kalsi G, Brynjolfsson J, McInnis M, O’Neill J, Smyth C, et al. Genome scan of pedigrees multiply affected with bipolar disorder provides further support for the presence of a susceptibility locus on chromosome 12q23-q24, and suggests the presence of additional loci on 1p and 1q. Psychiatr Genet. 2003;13:77–84. https://doi.org/10.1097/01.YPG.0000056684.89558.D2.
Garcia-Guzman M, Soto F, Gomez-Hernandez JM, Lund PE, Stühmer W. Characterization of recombinant human P2X4 receptor reveals pharmacological differences to the rat homologue. Mol Pharmacol. 1997;51:109–18. https://doi.org/10.1124/MOL.51.1.109.
Suurväli J, Boudinot P, Kanellopoulos J, Rüütel BS. P2X4: a fast and sensitive purinergic receptor. Biomed J. 2017;40:245–56. https://doi.org/10.1016/J.BJ.2017.06.010.
Guo C, Masin M, Qureshi OS, Murrell-Lagnado RD. Evidence for functional P2X4/P2X7 heteromeric receptors. Mol Pharmacol. 2007;72:1447–56. https://doi.org/10.1124/MOL.107.035980.
Schneider M, Prudic K, Pippel A, Klapperstück M, Braam U, Müller CE, et al. Interaction of purinergic P2X4 and P2X7 receptor subunits. Front Pharmacol. 2017;8:860. https://doi.org/10.3389/FPHAR.2017.00860/FULL.
Nicke A. Homotrimeric complexes are the dominant assembly state of native P2X7 subunits. Biochem Biophys Res Commun. 2008;377:803–8. https://doi.org/10.1016/J.BBRC.2008.10.042.
Craigie E, Birch RE, Unwin RJ, Wildman SS. The relationship between P2X4 and P2X7: a physiologically important interaction? Front Physiol. 2013;4:216. https://doi.org/10.3389/FPHYS.2013.00216.
Barden N, Harvey M, Gagné B, Shink E, Tremblay M, Raymond C, et al. Analysis of single nucleotide polymorphisms in genes in the chromosome 12Q24.31 region points to P2RX7 as a susceptibility gene to bipolar affective disorder. Am J Med Genet B Neuropsychiatr Genet. 2006;141B:374–82. https://doi.org/10.1002/AJMG.B.30303.
McQuillin A, Bass NJ, Choudhury K, Puri V, Kosmin M, Lawrence J, et al. Case-control studies show that a non-conservative amino-acid change from a glutamine to arginine in the P2RX7 purinergic receptor protein is associated with both bipolar- and unipolar-affective disorders. Mol Psychiatry. 2009;14:614–20. https://doi.org/10.1038/MP.2008.6.
Soronen P, Mantere O, Melartin T, Suominen K, Vuorilehto M, Rytsälä H, et al. P2RX7 gene is associated consistently with mood disorders and predicts clinical outcome in three clinical cohorts. Am J Med Genet B Neuropsychiatr Genet. 2011;156B:435–47. https://doi.org/10.1002/AJMG.B.31179.
Halmai Z, Dome P, Vereczkei A, Abdul-Rahman O, Szekely A, Gonda X, et al. Associations between depression severity and purinergic receptor P2RX7 gene polymorphisms. J Affect Disord. 2013;150:104–9. https://doi.org/10.1016/J.JAD.2013.02.033.
Green EK, Grozeva D, Raybould R, Elvidge G, Macgregor S, Craig I, et al. P2RX7: a bipolar and unipolar disorder candidate susceptibility gene? Am J Med Genet B Neuropsychiatr Genet. 2009;150B:1063–9. https://doi.org/10.1002/AJMG.B.30931.
Grigoroiu-Serbanescu M, Herms S, Mühleisen TW, Georgi A, Diaconu CC, Strohmaier J, et al. Variation in P2RX7 candidate gene (rs2230912) is not associated with bipolar I disorder and unipolar major depression in four European samples. Am J Med Genet B Neuropsychiatr Genet. 2009;150B:1017–21. https://doi.org/10.1002/AJMG.B.30952.
Czamara D, Müller-Myhsok B, Lucae S. The P2RX7 polymorphism rs2230912 is associated with depression: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2018;82:272–7. https://doi.org/10.1016/J.PNPBP.2017.11.003.
Feng WP, Zhang B, Li W, Liu J. Lack of association of P2RX7 gene rs2230912 polymorphism with mood disorders: a meta-analysis. PLoS ONE. 2014;9: e88575. https://doi.org/10.1371/JOURNAL.PONE.0088575.
Backlund L, Nikamo P, Hukic DS, Ek IR, Träskman-Bendz L, Landén M, et al. Cognitive manic symptoms associated with the P2RX7 gene in bipolar disorder. Bipolar Disord. 2011;13:500–8. https://doi.org/10.1111/j.1399-5618.2011.00952.x.
Gubert C, Andrejew R, Jacintho Moritz CE, Dietrich F, Vasconcelos-Moreno MP, dos Santos BTMQ, et al. Bipolar disorder and 1513A>C P2RX7 polymorphism frequency. Neurosci Lett. 2019;694:143–7. https://doi.org/10.1016/j.neulet.2018.11.055.
Wall JD, Pritchard JK. Haplotype blocks and linkage disequilibrium in the human genome. Nat Rev Genet. 2003;4:587–97. https://doi.org/10.1038/nrg1123.
Li H, Cvejic E, Gu B, Vollmer-Conna U, Hickie I, Wakefield D, et al. Regulation of the acute sickness response by the P2RX7 receptor. J Infect Dis. 2021;224:914–20. https://doi.org/10.1093/infdis/jiab027.
Khoja S, Shah V, Garcia D, Asatryan L, Jakowec MW, Davies DL. Role of purinergic P2X4 receptors in regulating striatal dopamine homeostasis and dependent behaviors. J Neurochem. 2016;139:134–48. https://doi.org/10.1111/jnc.13734.
Khoja S, Asatryan L, Jakowec MW, Davies DL. Dopamine receptor blockade attenuates purinergic P2X4 receptor-mediated prepulse inhibition deficits and underlying molecular mechanisms. Front Cell Neurosci. 2019;13:1–17. https://doi.org/10.3389/fncel.2019.00331.
Wyatt LR, Godar SC, Khoja S, Jakowec MW, Alkana RL, Bortolato M, et al. Sociocommunicative and sensorimotor impairments in male P2X4-deficient mice. Neuropsychopharmacology. 2013;38:1993–2002. https://doi.org/10.1038/npp.2013.98.
Wyatt LR, Finn DA, Khoja S, Yardley MM, Asatryan L, Alkana RL, et al. Contribution of P2X4 receptors to ethanol intake in male C57BL/6 mice. Neurochem Res. 2014;39:1127–39. https://doi.org/10.1007/S11064-014-1271-9.
Bertin E, Deluc T, Pilch KS, Martinez A, Pougnet JT, Doudnikoff E, et al. Increased surface P2X4 receptor regulates anxiety and memory in P2X4 internalization-defective knock-in mice. Mol Psychiatry. 2021;26:629–44. https://doi.org/10.1038/S41380-019-0641-8.
Bortolato M, Yardley MM, Khoja S, Godar SC, Asatryan L, Finn DA, et al. Pharmacological insights into the role of P2X 4 receptors in behavioural regulation: lessons from ivermectin. Int J Neuropsychopharmacol. 2013;16:1059–70. https://doi.org/10.1017/S1461145712000909.
Machado-Vieira R, Lara D, Souza D, Kapczinski F. Purinergic dysfunction in mania: an integrative model. Med Hypotheses. 2002;58:297–304.
Shorter E. The history of lithium therapy. Bipolar Disord. 2009;11(Suppl. 2):4–9. https://doi.org/10.1111/J.1399-5618.2009.00706.X.
Anumonye A, Reading HW, Knight F, Ashcroft GW. Uric-acid metabolism in manic-depressive illness and during lithium therapy. Lancet. 1968;1:1290–3. https://doi.org/10.1016/S0140-6736(68)92300-3.
Kesebir S, Süner O, Yaylaci E, Bayrak A, Turan C. Increased uric acid levels in bipolar disorder: is it trait or state? J Biol Regul Homeost Agents. 2013;27:981–8.
Machado-Vieira R. Purinergic system in the treatment of bipolar disorder: uric acid levels as a screening test in Mania. J Clin Psychopharmacol. 2012;32:735–6. https://doi.org/10.1097/JCP.0b013e318268391d.
dos Santos Oliveira PM, Santos V, Coroa M, Ribeiro J, Madeira N. Serum uric acid as a predictor of bipolarity in individuals with a major depressive episode. Bipolar Disord. 2019;21:235–43. https://doi.org/10.1111/BDI.12708.
Chatterjee SS, Ghosal S, Mitra S, Mallik N, Ghosal MK. Serum uric acid levels in first episode mania, effect on clinical presentation and treatment response: data from a case control study. Asian J Psychiatry. 2018;35:15–7. https://doi.org/10.1016/J.AJP.2018.04.030.
Muti M, Del Grande C, Musetti L, Marazziti D, Turri M, Cirronis M, et al. Serum uric acid levels and different phases of illness in bipolar I patients treated with lithium. Psychiatry Res. 2015;225:604–8. https://doi.org/10.1016/J.PSYCHRES.2014.11.038.
Machado-Vieira R, Salem H, Frey BN, Barbosa IG, Teixeira AL. Convergent lines of evidence support the role of uric acid levels as a potential biomarker in bipolar disorder. Expert Rev Mol Diagn. 2017;17:107–8. https://doi.org/10.1080/14737159.2017.1270758.
Lu Z, Wang Y, Xun G. Individuals with bipolar disorder have a higher level of uric acid than major depressive disorder: a case-control study. Sci Rep. 2021;11:18307. https://doi.org/10.1038/S41598-021-97955-4.
Kesebir S, Tatlidil Yaylaci E, Süner Ö, Gültekin BK. Uric acid levels may be a biological marker for the differentiation of unipolar and bipolar disorder: the role of affective temperament. J Affect Disord. 2014;165:131–4. https://doi.org/10.1016/j.jad.2014.04.053.
Meng X, Huang X, Deng W, Li J, Li T. Serum uric acid a depression biomarker. PLoS ONE. 2020;15: e0229626. https://doi.org/10.1371/JOURNAL.PONE.0229626.
Kim S, Rhee SJ, Song Y, Ahn YM. Comparison of serum uric acid in major depressive disorder and bipolar disorder: a retrospective chart review study. J Korean Med Sci. 2020;35: e222. https://doi.org/10.3346/JKMS.2020.35.E222.
Bartoli F, Crocamo C, Mazza MG, Clerici M, Carrà G. Uric acid levels in subjects with bipolar disorder: a comparative meta-analysis. J Psychiatr Res. 2016;81:133–9. https://doi.org/10.1016/J.JPSYCHIRES.2016.07.007.
de Magalhães ELG, Juvanhol LL, da Silva DCG, Ferreira FG, Roberto DMT, de Hinnig PF, et al. Uric acid: a new marker for metabolic syndrome? Results of a population-based study with adults. Nutr Metab Cardiovasc Dis. 2021;31:2077–80. https://doi.org/10.1016/j.numecd.2021.03.012.
Kanbay M, Jensen T, Solak Y, Le M, Roncal-Jimenez C, Rivard C, et al. Uric acid in metabolic syndrome: from an innocent bystander to a central player. Eur J Intern Med. 2016;29:3–8. https://doi.org/10.1016/j.ejim.2015.11.026.
Vancampfort D, Vansteelandt K, Correll CU, Mitchell AJ, De Herdt A, Sienaert P, et al. Metabolic syndrome and metabolic abnormalities in bipolar disorder: a meta-analysis of prevalence rates and moderators. Am J Psychiatry. 2013;170:265–74. https://doi.org/10.1176/appi.ajp.2012.12050620.
Bartoli F, Crocamo C, Gennaro GM, Castagna G, Trotta G, Clerici M, et al. Exploring the association between bipolar disorder and uric acid: a mediation analysis. J Psychosom Res. 2016;84:56–9. https://doi.org/10.1016/j.jpsychores.2016.03.014.
Ring HA, Heller AJ, Marshall WJ, Johnson AL, Reynolds EH. Plasma uric acid in patients receiving anticonvulsant monotherapy. Epilepsy Res. 1991;8:241–4. https://doi.org/10.1016/0920-1211(91)90070-V.
Koller D, Almenara S, Mejía G, Saiz-Rodríguez M, Zubiaur P, Román M, et al. Metabolic effects of aripiprazole and olanzapine multiple-dose treatment in a randomised crossover clinical trial in healthy volunteers: association with pharmacogenetics. Adv Ther. 2021;38:1035–54. https://doi.org/10.1007/S12325-020-01566-W.
Chan HY, Jou SH, Juang YY, Chang CJ, Chen JJ, Chen CH, et al. A single-blind, comparative study of zotepine versus haloperidol in combination with a mood stabilizer for patients with moderate-to-severe mania. Psychiatry Clin Neurosci. 2010;64:162–9. https://doi.org/10.1111/J.1440-1819.2010.02066.X.
Chen JX, Zhang LG, Liu KZ, Chen HM, Zhou SJ, Wang N, et al. Patients with drug-naive bipolar disorder in remission after 8 weeks of treatment had decreased serum uric acid concentrations. Front Psychiatry. 2019;10:767. https://doi.org/10.3389/FPSYT.2019.00767.
Yao JK, Reddy R, Van Kammen DP. Reduced level of plasma antioxidant uric acid in schizophrenia. Psychiatry Res. 1998;80:29–39. https://doi.org/10.1016/S0165-1781(98)00051-1.
Vanwong N, Srisawasdi P, Ngamsamut N, Nuntamool N, Puangpetch A, Chamkrachangpada B, et al. Hyperuricemia in children and adolescents with autism spectrum disorder treated with risperidone: the risk factors for metabolic adverse effects. Front Pharmacol. 2017;7:527. https://doi.org/10.3389/FPHAR.2016.00527.
Gubert C, Jacintho Moritz CE, Vasconcelos-Moreno MP, Quadros dos Santos BTM, Sartori J, Fijtman A, et al. Peripheral adenosine levels in euthymic patients with bipolar disorder. Psychiatry Res. 2016;246:421–6. https://doi.org/10.1016/J.PSYCHRES.2016.10.007.
Jagannath A, Varga N, Dallmann R, Rando G, Gosselin P, Ebrahimjee F, et al. Adenosine integrates light and sleep signalling for the regulation of circadian timing in mice. Nat Commun. 2021;12:2113. https://doi.org/10.1038/S41467-021-22179-Z.
Bechtel W. Circadian rhythms and mood disorders: are the phenomena and mechanisms causally related? Front Psychiatry. 2015;6:118.
Gold AK, Sylvia LG. The role of sleep in bipolar disorder. Nat Sci Sleep. 2016;8:207–14. https://doi.org/10.2147/NSS.S85754.
Lewis KS, Gordon-Smith K, Forty L, Di Florio A, Craddock N, Jones L, et al. Sleep loss as a trigger of mood episodes in bipolar disorder: individual differences based on diagnostic subtype and gender. Br J Psychiatry. 2017;211:169–74. https://doi.org/10.1192/BJP.BP.117.202259.
Wehr TA. Sleep loss: a preventable cause of mania and other excited states. J Clin Psychiatry. 1989;50 Suppl.:8–16.
Plante DT, Winkelman JW. Sleep disturbance in bipolar disorder: therapeutic implications. Am J Psychiatry. 2008;165:830–43. https://doi.org/10.1176/APPI.AJP.2008.08010077.
Yang S, Van Dongen HPA, Wang K, Berrettini W, Bućan M. Assessment of circadian function in fibroblasts of patients with bipolar disorder. Mol Psychiatry. 2009;14:143–55. https://doi.org/10.1038/MP.2008.10.
McCarthy MJ, Wei H, Marnoy Z, Darvish RM, McPhie DL, Cohen BM, et al. Genetic and clinical factors predict lithium’s effects on PER2 gene expression rhythms in cells from bipolar disorder patients. Transl Psychiatry. 2013;3: e318. https://doi.org/10.1038/TP.2013.90.
Gonçalves MCB, Glaser T, de Oliveira SLB, Ulrich H. Adenosinergic-dopaminergic signaling in mood disorders: a mini-review. J Caffeine Adenosine Res. 2020;10:94–103. https://doi.org/10.1089/caff.2020.0009.
Baldessarini RJ, Tondo L, Vázquez GH. Pharmacological treatment of adult bipolar disorder. Mol Psychiatry. 2019;24:198–217. https://doi.org/10.1038/S41380-018-0044-2.
Grunze A, Amann BL, Grunze H. Efficacy of carbamazepine and its derivatives in the treatment of bipolar disorder. Med Kaunas Lith. 2021;57:433. https://doi.org/10.3390/MEDICINA57050433.
Chen CH, Lin SK. Carbamazepine treatment of bipolar disorder: a retrospective evaluation of naturalistic long-term outcomes. BMC Psychiatry. 2012;12:47. https://doi.org/10.1186/1471-244X-12-47.
Yatham LN, Kennedy SH, Parikh SV, Schaffer A, Bond DJ, Frey BN, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018;20:97–170. https://doi.org/10.1111/bdi.12609.
Biber K, Fiebich BL, Gebicke-Härter P, Van Calker D. Carbamazepine-induced upregulation of adenosine A1-receptors in astrocyte cultures affects coupling to the phosphoinositol signaling pathway. Neuropsychopharmacology. 1999;20:271–8. https://doi.org/10.1016/S0893-133X(98)00059-1.
Marek GJ. Activation of adenosine1 receptors induces antidepressant-like, anti-impulsive effects on differential reinforcement of low-rate 72-s behavior in rats. J Pharmacol Exp Ther. 2012;341:564–70. https://doi.org/10.1124/JPET.112.191718.
Ferre S, Ciruela F, Borycz J, Solinas M, Quarta D, Antoniou K, et al. Adenosine A1–A2A receptor heteromers: new targets for caffeine in the brain. Front Biosci. 2008;13:2391–9. https://doi.org/10.2741/2852.
Shen J, Tomar JS. Elevated brain glutamate levels in bipolar disorder and pyruvate carboxylase-mediated anaplerosis. Front Psychiatry. 2021;12: 640977. https://doi.org/10.3389/FPSYT.2021.640977.
Ashok AH, Marques TR, Jauhar S, Nour MM, Goodwin GM, Young AH, et al. The dopamine hypothesis of bipolar affective disorder: the state of the art and implications for treatment. Mol Psychiatry. 2017;22:666–79. https://doi.org/10.1038/MP.2017.16.
Marchand WR, Yurgelun-Todd D. Striatal structure and function in mood disorders: a comprehensive review. Bipolar Disord. 2010;12:764–85. https://doi.org/10.1111/J.1399-5618.2010.00874.X.
Martini C, Tuscano D, Trincavelli ML, Cerrai E, Bianchi M, Ciapparelli A, et al. Upregulation of A2A adenosine receptors in platelets from patients affected by bipolar disorders under treatment with typical antipsychotics. J Psychiatr Res. 2006;40:81–8. https://doi.org/10.1016/J.JPSYCHIRES.2004.12.008.
Dome P, Rihmer Z, Gonda X. Suicide risk in bipolar disorder: a brief review. Med Kaunas Lith. 2019;55:403. https://doi.org/10.3390/MEDICINA55080403.
Bartoli F, Clerici M, Carrà G. Purinergic system and suicidal behavior: exploring the link between adenosine A2A receptors and depressive/impulsive features. Mol Psychiatry. 2020;25:512–3. https://doi.org/10.1038/S41380-018-0057-X.
Gonçalves MCB, Corrêa-Velloso J, Naaldijk Y, Cheffer A, Ulrich H. Purinergic modulation of pathways associated to suicidal behavior. Mol Psychiatry. 2020;25:514–6. https://doi.org/10.1038/S41380-018-0088-3.
Alda M. Lithium in the treatment of bipolar disorder: pharmacology and pharmacogenetics. Mol Psychiatry. 2015;20:661–70. https://doi.org/10.1038/MP.2015.4.
Licht RW, Rasmus Licht CW. Lithium: still a major option in the management of bipolar disorder. CNS Neurosci Ther. 2012;18:219–26. https://doi.org/10.1111/J.1755-5949.2011.00260.X.
Severus E, Taylor MJ, Sauer C, Pfennig A, Ritter P, Bauer M, et al. Lithium for prevention of mood episodes in bipolar disorders: systematic review and meta-analysis. Int J Bipolar Disord. 2014;2:15. https://doi.org/10.1186/s40345-014-0015-8.
Gubert C, Andrejew R, Figueiro F, Bergamin L, Kapczinski F, Magalhães da PVS, et al. Lithium-induced neuroprotective activity in neuronal and microglial cells: a purinergic perspective. Psychiatry Res. 2021;295:113562. https://doi.org/10.1016/J.PSYCHRES.2020.113562.
Wilot LC, Da Silva RS, Ferreira OJ, Bonan CD, Sarkis JJF, Rocha E, et al. Chronic treatment with lithium increases the ecto-nucleotidase activities in rat hippocampal synatosomes. Neurosci Lett. 2004;368:167–70. https://doi.org/10.1016/j.neulet.2004.07.002.
Zhang Y, Nelson RD, Carlson NG, Kamerath CD, Kohan DE, Kishore BK. Potential role of purinergic signaling in lithium-induced nephrogenic diabetes insipidus. Am J Physiol Renal Physiol. 2009;296:F1194–201. https://doi.org/10.1152/ajprenal.90774.2008.
Anand A, McClintick JN, Murrell J, Karne H, Nurnberger JI, Edenberg HJ. Effects of lithium monotherapy for bipolar disorder on gene expression in peripheral lymphocytes. Complex Psychiatry. 2016;2:115–23. https://doi.org/10.1159/000446348.
Wilot LC, Bernardi A, Frozza RL, Marques AL, Cimarosti H, Salbego C, et al. Lithium and valproate protect hippocampal slices against ATP-induced cell death. Neurochem Res. 2007;32:1539–46. https://doi.org/10.1007/s11064-007-9348-3.
Haimovich A, Goldbourt A. How does the mood stabilizer lithium bind ATP, the energy currency of the cell: Insights from solid-state NMR. Biochim Biophys Acta Gen Subj. 2020;1864:1–10. https://doi.org/10.1016/J.BBAGEN.2019.129456.
Briggs KT, Giulian GG, Li G, Kao JPY, Marino JP. A molecular model for lithium’s bioactive form. Biophys J. 2016;111:294–300. https://doi.org/10.1016/J.BPJ.2016.06.015.
Gubert C, Fries GR, Pfaffenseller B, Ferrari P, Coutinho-Silva R, Morrone FB, et al. Role of P2X7 receptor in an animal model of mania induced by D-amphetamine. Mol Neurobiol. 2016;53:611–20. https://doi.org/10.1007/s12035-014-9031-z.
Gubert C, Andrejew R, Leite CE, Moritz CEJ, Scholl J, Figueiro F, et al. P2X7 purinergic receptor is involved in the pathophysiology of mania: a preclinical study. Mol Neurobiol. 2020;57:1347–60. https://doi.org/10.1007/s12035-019-01817-0.
Csölle C, Andó RD, Kittel Á, Gölöncsér F, Baranyi M, Soproni K, et al. The absence of P2X7 receptors (P2rx7) on non-haematopoietic cells leads to selective alteration in mood-related behaviour with dysregulated gene expression and stress reactivity in mice. Int J Neuropsychopharmacol. 2013;16:233. https://doi.org/10.1017/S1461145711001933.
Bhattacharya A, Biber K. The microglial ATP-gated ion channel P2X7 as a CNS drug target. Glia. 2016;64:1772–87. https://doi.org/10.1002/glia.23001.
Bhattacharya A. Recent advances in CNS P2X7 physiology and pharmacology: focus on neuropsychiatric disorders. Front Pharmacol. 2018;9:30. https://doi.org/10.3389/FPHAR.2018.00030.
Rech JC, Bhattacharya A, Letavic MA, Savall BM. The evolution of P2X7 antagonists with a focus on CNS indications. Bioorg Med Chem Lett. 2016;26:3838–45. https://doi.org/10.1016/j.bmcl.2016.06.048.
Gunosewoyo H, Kassiou M. P2X purinergic receptor ligands: recently patented compounds. Expert Opin Ther Pat. 2010;20:625–46. https://doi.org/10.1517/13543771003702424.
Letavic MA, Savall BM, Allison BD, Aluisio L, Andres JI, De Angelis M, et al. 4-Methyl-6,7-dihydro-4H-triazolo[4,5-c]pyridine-based P2X7 receptor antagonists: optimization of pharmacokinetic properties leading to the identification of a clinical candidate. J Med Chem. 2017;60:4559–72. https://doi.org/10.1021/ACS.JMEDCHEM.7B00408.
Chrovian CC, Soyode-Johnson A, Peterson AA, Gelin CF, Deng X, Dvorak CA, et al. A dipolar cycloaddition reaction to access 6-methyl-4,5,6,7-tetrahydro-1H-[1,2,3]triazolo[4,5-c]pyridines enables the discovery synthesis and preclinical profiling of a P2X7 antagonist clinical candidate. J Med Chem. 2018;61:207–23. https://doi.org/10.1021/ACS.JMEDCHEM.7B01279.
Wei L, Syed Mortadza SA, Yan J, Zhang L, Wang L, Yin Y, et al. ATP-activated P2X7 receptor in the pathophysiology of mood disorders and as an emerging target for the development of novel antidepressant therapeutics. Neurosci Biobehav Rev. 2018;87:192–205. https://doi.org/10.1016/J.NEUBIOREV.2018.02.005.
Timmers M, Ravenstijn P, Xi L, Triana-Baltzer G, Furey M, Van Hemelryck S, et al. Clinical pharmacokinetics, pharmacodynamics, safety, and tolerability of JNJ-54175446, a brain permeable P2X7 antagonist, in a randomised single-ascending dose study in healthy participants. J Psychopharmacol (Oxf). 2018;32:1341–50. https://doi.org/10.1177/0269881118800067.
Koole M, Schmidt ME, Hijzen A, Ravenstijn P, Vandermeulen C, Van Weehaeghe D, et al. 18 F-JNJ-64413739, a novel PET ligand for the P2X7 ion channel: radiation dosimetry, kinetic modeling, test-retest variability, and occupancy of the P2X7 antagonist JNJ-54175446. J Nucl Med. 2019;60:683–90. https://doi.org/10.2967/JNUMED.118.216747.
Recourt K, van der Aart J, Jacobs G, de Kam M, Drevets W, van Nueten L, et al. Characterisation of the pharmacodynamic effects of the P2X7 receptor antagonist JNJ-54175446 using an oral dexamphetamine challenge model in healthy males in a randomised, double-blind, placebo-controlled, multiple ascending dose trial. J Psychopharmacol Oxf Engl. 2020;34:1030–42. https://doi.org/10.1177/0269881120914206.
Ruiz-Ruiz C, Calzaferri F, García AG. P2X7 receptor antagonism as a potential therapy in amyotrophic lateral sclerosis. Front Mol Neurosci. 2020;13:93. https://doi.org/10.3389/FNMOL.2020.00093.
Bishnoi RJ. Clinical potential of allopurinol in the treatment of bipolar disorder. Indian J Psychol Med. 2014;36:218–20. https://doi.org/10.4103/0253-7176.131008.
Harker LA, Kadatz RA. Mechanism of action of dipyridamole. Thromb Res. 1983;4:39–46. https://doi.org/10.1016/0049-3848(83)90356-0.
German DC, Kredich NM, Bjornsson TD. Oral dipyridamole increases plasma adenosine levels in human beings. Clin Pharmacol Ther. 1989;45:80–4. https://doi.org/10.1038/CLPT.1989.12.
Pacher P, Nivorozhkin A, Szabó C. Therapeutic effects of xanthine oxidase inhibitors: renaissance half a century after the discovery of allopurinol. Pharmacol Rev. 2006;58:87–114. https://doi.org/10.1124/PR.58.1.6.
Qurie A, Goyal A, Musa R. Allopurinol. Treasure Island: StatPearls Publishing; 2022.
Krakoff IH. Use of allopurinol in preventing hyperuricemia in leukemia and lymphoma. Cancer. 1966;19:1489–96. https://doi.org/10.1002/1097-0142(196611)19:11%3c1489::AID-CNCR2820191105%3e3.0.CO;2-F.
Grover PK, Ryall RL. Allopurinol for stones: right drug—wrong reasons. Am J Med. 2007;120:380. https://doi.org/10.1016/j.amjmed.2006.08.017.
Pak CYC, Poindexter JR, Peterson RD, Koska J, Sakhaee K. Biochemical distinction between hyperuricosuric calcium urolithiasis and gouty diathesis. Urology. 2002;60:789–94. https://doi.org/10.1016/s0090-4295(02)01908-8.
Machado-Vieira R, Lara DR, Souza DO, Kapczinski F. Therapeutic efficacy of allopurinol in mania associated with hyperuricemia. J Clin Psychopharmacol. 2001;21:621–2. https://doi.org/10.1097/00004714-200112000-00017.
Akhondzadeh S, Milajerdi MR, Amini H, Tehrani-Doost M. Allopurinol as an adjunct to lithium and haloperidol for treatment of patients with acute mania: a double-blind, randomized, placebo-controlled trial. Bipolar Disord. 2006;8:485–9. https://doi.org/10.1111/J.1399-5618.2006.00363.X.
Machado-Vieira R, Soares JC, Lara DR, Luckenbaugh DA, Busnello JV, Marca G, et al. A double-blind, randomized, placebo-controlled 4-week study on the efficacy and safety of the purinergic agents allopurinol and dipyridamole adjunctive to lithium in acute bipolar mania. J Clin Psychiatry. 2008;69:1237–45. https://doi.org/10.4088/JCP.V69N0806.
Jahangard L, Soroush S, Haghighi M, Ghaleiha A, Bajoghli H, Holsboer-Trachsler E, et al. In a double-blind, randomized and placebo-controlled trial, adjuvant allopurinol improved symptoms of mania in in-patients suffering from bipolar disorder. Eur Neuropsychopharmacol. 2014;24:1210–21. https://doi.org/10.1016/J.EURONEURO.2014.05.013.
Kessing LV, Rytgaard HC, Gerds TA, Berk M, Ekstrøm CT, Andersen PK. New drug candidates for bipolar disorder: a nation-wide population-based study. Bipolar Disord. 2019;21:410–8. https://doi.org/10.1111/BDI.12772.
Fan A, Berg A, Bresee C, Glassman LH, Rapaport MH. Allopurinol augmentation in the outpatient treatment of bipolar mania: a pilot study. Bipolar Disord. 2012;14:206–10. https://doi.org/10.1111/J.1399-5618.2012.01001.X.
Weiser M, Burshtein S, Gershon AA, Marian G, Vlad N, Grecu IG, et al. Allopurinol for mania: a randomized trial of allopurinol versus placebo as add-on treatment to mood stabilizers and/or antipsychotic agents in manic patients with bipolar disorder. Bipolar Disord. 2014;16:441–7. https://doi.org/10.1111/BDI.12202.
Bartoli F, Crocamo C, Clerici M, Carra G. Allopurinol as add-on treatment for mania symptoms in bipolar disorder: systematic review and meta-analysis of randomised controlled trials. Br J Psychiatry J Ment Sci. 2017;210:10–5. https://doi.org/10.1192/BJP.BP.115.180281.
Chen AT, Malmstrom T, Nasrallah HA. Allopurinol augmentation in acute mania: a meta-analysis of placebo-controlled trials. J Affect Disord. 2018;226:245–50. https://doi.org/10.1016/J.JAD.2017.09.034.
Bartoli F, Cavaleri D, Bachi B, Moretti F, Riboldi I, Crocamo C, et al. Repurposed drugs as adjunctive treatments for mania and bipolar depression: a meta-review and critical appraisal of meta-analyses of randomized placebo-controlled trials. J Psychiatr Res. 2021;143:230–8. https://doi.org/10.1016/J.JPSYCHIRES.2021.09.018.
Acknowledgments
Maria Carolina Bittencourt Gonçalves is a Sadhguru Center for a Conscious Planet Fellow. Roberta Andrejew has a doctoral fellowship from Fundação de Amparo à Pesquisa do Estado de São Paulo (Project No. 2019/24553-5). Carolina Gubert is a Hereditary Disease Foundation Fellow.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the preparation of this article. Open Access funding enabled and organized by CAUL and its Member Institutions.
Conflict of interest/competing interests
The authors have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Authors’ contributions
Conceptualization, CG; literature search, MCBG, RA, and CG; writing, original draft, MCBG, RA, and CG; writing, review and editing, MCBG, RA, and CG; figure, MCBG and RA; supervision, CG. All authors approved the final version of the manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gonçalves, M.C.B., Andrejew, R. & Gubert, C. The Purinergic System as a Target for the Development of Treatments for Bipolar Disorder. CNS Drugs 36, 787–801 (2022). https://doi.org/10.1007/s40263-022-00934-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-022-00934-0