Abstract
Background
Pitolisant, a selective histamine 3 receptor antagonist/inverse agonist, is indicated for the treatment of excessive daytime sleepiness or cataplexy in adults with narcolepsy. The efficacy and safety of pitolisant have been demonstrated in randomized placebo-controlled trials. When evaluating the results of randomized placebo-controlled trials, the clinical impact of a treatment can be assessed using effect size metrics that include Cohen’s d (the standardized mean difference of an effect) and number needed to treat (NNT; number of patients that need to be treated to achieve a specific outcome for one person).
Objective
The objective of this study was to evaluate the clinical impact of pitolisant for the reduction in excessive daytime sleepiness or cataplexy in adults with narcolepsy.
Methods
This post hoc analysis incorporated data from two 7-week or 8-week randomized placebo-controlled trials (HARMONY 1, HARMONY CTP). Study medication was individually titrated, with a maximum possible pitolisant dose of 35.6 mg/day. Efficacy was assessed using the Epworth Sleepiness Scale (ESS) and weekly rate of cataplexy (HARMONY CTP only). Cohen’s d was derived from the least-squares mean difference between treatment groups (pitolisant vs placebo), and NNTs were calculated from response rates. Treatment response was defined for excessive daytime sleepiness in two ways: (a) reduction in ESS score ≥ 3 or final ESS score ≤ 10 and (b) final ESS score ≤ 10. Treatment response was defined for cataplexy as a ≥ 25%, ≥ 50%, or ≥ 75% reduction in weekly rate of cataplexy.
Results
The analysis population included 61 patients in HARMONY 1 (pitolisant, n = 31; placebo, n = 30) and 105 patients in HARMONY CTP (pitolisant, n = 54; placebo, n = 51). For pitolisant vs placebo, Cohen’s d effect size values were 0.61 (HARMONY 1) and 0.86 (HARMONY CTP) based on changes in ESS scores, and 0.86 (HARMONY CTP) based on changes in weekly rate of cataplexy. NNTs for pitolisant were 3–5 for the treatment of excessive daytime sleepiness and 3–4 for the treatment of cataplexy.
Conclusions
The results of this analysis demonstrate the robust efficacy of pitolisant for the reduction in both excessive daytime sleepiness and cataplexy. These large effect sizes and low NNTs provide further evidence supporting the strength of the clinical response to pitolisant in the treatment of adults with narcolepsy.
Clinical Trial Registration
ClinicalTrials.gov identifiers: NCT01067222 (February 2010), NCT01800045 (February 2013).
Similar content being viewed by others
When evaluating the results of randomized controlled trials, the clinical impact of a treatment can be assessed using effect size metrics such as Cohen’s d and number needed to treat (NNT). |
In conjunction with the primary results from placebo-controlled studies, the large Cohen’s d values and low NNTs observed in this analysis demonstrate the robust efficacy of pitolisant for the reduction in both excessive daytime sleepiness and cataplexy in adults with narcolepsy. |
The strength of this evidence suggests that pitolisant should be considered as a first-line treatment in adult patients with narcolepsy. |
1 Introduction
Narcolepsy is a chronic, debilitating neurological disorder characterized by symptoms that are indicative of sleep–wake state instability (e.g., excessive daytime sleepiness [EDS], cataplexy, hypnagogic hallucinations, sleep paralysis, disrupted night-time sleep) [1, 2]. In patients with narcolepsy, EDS is typically characterized by repeated episodes of an irrepressible need to sleep, and/or unintended lapses into drowsiness or sleep but may also manifest with automatic behaviors and lapses in attention [2, 3]. Excessive daytime sleepiness is required for the diagnosis of narcolepsy; cataplexy (the sudden, brief loss of muscle tone usually triggered by emotion) and other manifestations of rapid eye movement sleep dysregulation (e.g., hypnagogic hallucinations, sleep paralysis) also occur in some patients [3]. There are two phenotypes of narcolepsy: narcolepsy type 1, which is diagnosed based on the presence of cataplexy attacks and/or low levels of hypocretin in cerebrospinal fluid, and narcolepsy type 2, in which cataplexy is absent [3]. Narcolepsy type 1 is caused by the selective loss of hypocretin-producing neurons in the lateral hypothalamus, whereas the pathophysiology of narcolepsy type 2 is less well understood [4]. Narcolepsy type 1 is associated with genetic (e.g., human leukocyte antigen DQB1*06:02) and environmental (e.g., infection) factors that may activate immunologic pathways, leading to the destruction of hypocretin-producing neurons [2, 5].
Although hypocretin-based therapies such as hypocretin-2 receptor agonists are currently in clinical development [6, 7], at present, there are no approved agents that restore hypocretin function in patients with narcolepsy [8]. Available treatments are symptom driven and are thought to modulate various neurotransmitter systems that regulate wakefulness and sleep (e.g., norepinephrine, serotonin, dopamine, histamine, γ-aminobutyric acid) or play a role in the pathophysiology of cataplexy (e.g., norepinephrine, serotonin) [8,9,10,11]. Histamine, a wake-promoting neurotransmitter produced by neurons that originate in the tuberomammillary nucleus of the posterior hypothalamus, plays an important role in the regulation of sleep and wakefulness [12, 13]. Preclinical research has demonstrated that histamine is essential for normal sleep–wake behavior; in addition, histamine may stabilize sleep–wake transitions [12, 14]. Binding of histamine at postsynaptic histamine 1 receptors in the brain promotes wakefulness and suppresses sleep [12, 15]. Histamine binding at presynaptic histamine 3 (H3) autoreceptors decreases the synthesis and release of histamine [16,17,18], and histamine binding at presynaptic H3 heteroreceptors inhibits the release of other neurotransmitters (e.g., norepinephrine, serotonin, acetylcholine, dopamine) [17, 19].
Pitolisant, a selective H3 receptor antagonist/inverse agonist, is a first-in-class medication with a novel mechanism of action for the treatment of patients with narcolepsy [20, 21]. Pitolisant blocks the inhibitory effect of histamine on endogenous histamine release and increases the synthesis and release of histamine in the brain [16, 22, 23]. Pitolisant also increases the release of other neurotransmitters (e.g., norepinephrine, dopamine, acetylcholine) in the cerebral cortex [23, 24]. Thus, the mechanism of action for pitolisant in the treatment of narcolepsy is thought to involve both direct effects via the histaminergic system and indirect effects via other neurotransmitter systems [10, 11]. Pitolisant is approved by the US Food and Drug Administration for the treatment of EDS or cataplexy in adult patients with narcolepsy [25] and by the European Medicines Agency for the treatment of narcolepsy with or without cataplexy in adults [26]. The efficacy of pitolisant for reducing EDS and cataplexy in adults with narcolepsy has been demonstrated in randomized placebo-controlled trials (RCTs) [25, 27, 28] with additional information on safety and efficacy provided by a long-term open-label study [29].
When evaluating the clinical relevance of RCT results, response to treatment can be quantified using metrics such as effect size; Cohen’s d, for example, reflects the magnitude of the drug–placebo difference for an outcome measure [30]. Number needed to treat (NNT) is a derived statistic calculated from observed response rates; it can provide additional information regarding the number of patients that are likely to benefit from a treatment intervention [30, 31]. NNT suggests the number of patients that need to be treated with one agent (e.g., study medication) instead of another (e.g., placebo) to obtain a positive clinical outcome for one additional person [30, 31]. Information about the effect sizes of narcolepsy treatments may be useful for enhancing clinical decision making. The objective of this analysis was to evaluate the clinical impact of pitolisant for the treatment of EDS and cataplexy in adults with narcolepsy by using effect size metrics (Cohen’s d, NNT) to quantify the clinical relevance of RCT results and express them in a clinically meaningful way.
2 Methods
This post hoc analysis included data from two randomized, double-blind, placebo-controlled trials that evaluated the efficacy and safety of pitolisant in the treatment of adults with narcolepsy: HARMONY 1 (NCT01067222) and HARMONY CTP (NCT01800045) [27, 28]. HARMONY 1 was conducted at 24 centers in Europe between May 2009 and June 2010. HARMONY CTP was conducted at 16 centers in Europe between April 2013 and January 2015. The studies included a 1-week (HARMONY 1) or 2-week (HARMONY CTP) baseline period followed by a 7-week (HARMONY CTP) or 8-week (HARMONY 1) treatment period. Study conduct was consistent with Good Clinical Practice guidelines and the Declaration of Helsinki. Each study was approved by an institutional review board or independent ethics committee at each study site, and all patients provided written informed consent prior to study enrollment. The primary results of each study have been reported elsewhere [27, 28].
2.1 Patients
All patients were adults (aged ≥ 18 years) with a diagnosis of narcolepsy according to International Classification of Sleep Disorders, 2nd Edition criteria: narcolepsy with or without cataplexy in HARMONY 1 and narcolepsy with cataplexy in HARMONY CTP. Excessive daytime sleepiness was present in all patients, as documented by an Epworth Sleepiness Scale (ESS) score of ≥ 14 in HARMONY 1 or ≥ 12 in HARMONY CTP. All patients in HARMONY CTP also had three or more attacks of cataplexy per week at baseline. Key exclusion criteria included other conditions that may cause EDS (e.g., sleep apnea, periodic limb movement disorder, circadian rhythm sleep–wake disorders), substance abuse or dependence (within the past year), severe hepatic or renal impairment, and significant cardiovascular abnormality.
2.2 Treatment
This analysis included patients who were randomly assigned to receive pitolisant or placebo. Study medication was individually titrated over a 3-week period, with a possible maximum pitolisant dose of 35.6 mg/day; the dose administered at the beginning of week 4 remained stable for the remainder of the treatment period. Stimulants and other wake-promoting medications (e.g., amphetamines, methylphenidate, modafinil) were prohibited. Concomitant use of other anticataplectic mediations (e.g., sodium oxybate, antidepressants other than tricyclic antidepressants) was permitted if the dose had been stable for ≥ 1 month prior to screening and remained unchanged during the study.
2.3 Assessments
Excessive daytime sleepiness was assessed using the ESS: an eight-item, validated, patient-report questionnaire that assesses the propensity to doze off or fall asleep in real-world situations [32]. The total ESS score ranges from 0 to 24; scores ≤ 10 are considered to be within the normal range, scores > 10 are indicative of EDS, and scores ≥ 16 denote severe EDS [32, 33]. The ESS was administered at baseline and at scheduled study visits during the treatment period (weeks 2, 3, 7, and 8 in HARMONY 1; weeks 2, 3, 6, and 7 in HARMONY CTP). The weekly rate of cataplexy (WRC) attacks was calculated for the baseline period and weekly thereafter using information recorded in patient diaries. End-of-treatment assessments occurred at week 8 in HARMONY 1 and week 7 in HARMONY CTP.
2.4 Statistical Analysis
To evaluate the clinical impact of treatment, effect sizes were calculated using ESS scores (HARMONY 1, HARMONY CTP) and WRC (HARMONY CTP). Least-squares (LS) mean change from baseline was obtained from analysis of covariance models that included fixed effects for treatment and baseline and a random effect for study site. Cohen’s d was derived from the LS mean difference between treatment groups (pitolisant vs placebo). NNTs were calculated from response rates. For both studies, treatment response was defined for EDS in two ways: (a) reduction in ESS score ≥ 3 or final ESS score ≤ 10 and (b) final ESS score ≤ 10 (i.e., within the normal range). For HARMONY CTP, treatment response was defined for cataplexy as a ≥ 25%, ≥ 50%, or ≥ 75% reduction in WRC. The NNT was computed as the inverse of the drug–placebo difference in response rates rounded upward to the next higher whole number [31]. For the ESS score, the final value used in each analysis was the average of the last two study visits; for WRC, the final value was the average during the stable dose period in HARMONY CTP (weeks 4–7). All analyses used a last observation carried forward approach.
3 Results
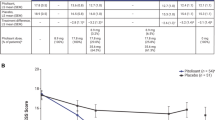
The analysis population included the intent-to-treat population from each study: 61 patients in HARMONY 1 (pitolisant, n = 31; placebo, n = 30) and 105 patients in HARMONY CTP (pitolisant, n = 54; placebo, n = 51). Baseline characteristics were similar across the two studies (Table 1). At baseline, the mean ESS score was 17.8 in the pitolisant group and 18.9 in the placebo group in HARMONY 1, and 17.4 and 17.3, respectively, in HARMONY CTP, which is representative of severe EDS [32]. In HARMONY CTP, the frequency of cataplexy attacks at baseline was 11.7 per week, on average, in the pitolisant group and 9.6 per week in the placebo group. Pitolisant was titrated to the maximum recommended dose (35.6 mg/day) in 61.3% of patients in HARMONY 1 and 64.8% of patients in HARMONY CTP. Concomitant anticataplectic medications were used by four patients (7.4%) in the pitolisant group (selective serotonin reuptake inhibitor, n = 3; sodium oxybate, n = 1) and eight patients (15.7%) in the placebo group (selective serotonin reuptake inhibitor, n = 1; serotonin and norepinephrine reuptake inhibitor, n = 5; norepinephrine reuptake inhibitor, n = 1; sodium oxybate, n = 1) in HARMONY CTP.
Large effect sizes, as measured using Cohen’s d, were observed for pitolisant in the treatment of EDS (Fig. 1) and cataplexy (Fig. 2). For changes in ESS scores from baseline to the end of treatment, the LS mean (standard error) difference for pitolisant vs placebo was − 3.1 (1.3) in HARMONY 1 (p = 0.022) and − 3.4 (0.8) in HARMONY CTP (p < 0.001). In a pooled analysis using data from both studies (pitolisant, n = 85; placebo, n = 81), the LS mean change in ESS score from baseline to end of treatment was − 5.6 in the pitolisant group and − 2.3 in the placebo group (LS mean treatment difference, − 3.3; p < 0.001; Cohen’s d = 0.73). For changes in WRC from baseline to the stable dose treatment period, the LS mean (standard error) difference for pitolisant vs placebo was − 6.2 (1.4) in HARMONY CTP (p < 0.001).
Response rates for EDS (Fig. 3) and WRC (Fig. 4) were consistently greater for pitolisant compared with placebo, regardless of how treatment response was defined. NNT values for pitolisant ranged from 3 to 5 in the treatment of EDS (Fig. 3). In a pooled analysis using ESS data from both studies, treatment response defined as an ESS score reduction ≥ 3 or a final ESS score ≤ 10 was observed in 68.3% of the pitolisant group vs 37.5% of the placebo group (NNT = 4). An ESS score of ≤ 10 (within the normal range) was noted at the end of treatment in 41.5% of patients receiving pitolisant vs 16.3% of patients receiving placebo (NNT = 4). For pitolisant in the treatment of cataplexy, NNT values ranged from 3 to 4 in HARMONY CTP (Fig. 4).
Number needed to treat (NNT) for pitolisant in the treatment of excessive daytime sleepiness in HARMONY 1 and HARMONY CTP for treatment response defined in two ways: a Epworth Sleepiness Scale score reduction ≥ 3 or final Epworth Sleepiness Scale score ≤ 10 and b final Epworth Sleepiness Scale score ≤ 10
4 Discussion
The statistical superiority of one intervention over another is commonly evaluated using statistical significance (p-value) in clinical trials; however, this does not necessarily reflect the clinical relevance of the intervention. Measures of effect size provide clinicians with metrics for appraising the magnitude of response in a clinical trial [30, 34]. This post hoc analysis used effect sizes (i.e., Cohen’s d, NNT) to capture the magnitude of response to pitolisant from the clinical trial results in the treatment of adult patients with narcolepsy. The therapeutic effects of pitolisant vs placebo resulted in large values for Cohen’s d (0.61 and 0.86 for EDS, 0.86 for cataplexy) and single-digit NNT values (3–5 for EDS, 3–4 for cataplexy). The primary efficacy analyses demonstrated a significantly greater mean change from baseline for pitolisant vs placebo on measures of EDS and cataplexy, which was important for establishing treatment efficacy [27, 28]. The findings of this analysis provide further evidence of the robust therapeutic effects of pitolisant in the treatment of EDS and cataplexy, with symptom reduction of a magnitude that was clinically meaningful for many patients.
Cohen’s d, one of the commonly used metrics of effect size, describes the standardized mean difference of an effect and can be used to compare across studies [30, 35]. The standard interpretation for Cohen’s d is that a value of 0.2 represents a small effect size, 0.5 a medium effect size, and 0.8 a large effect size [30, 34]. In this analysis, medium-to-large Cohen’s d values were observed for pitolisant in the treatment of EDS and cataplexy, and these values were similar to those reported for sodium oxybate for treatment of EDS in patients with narcolepsy [36]. It is important to note, however, that cross-study comparisons should be interpreted with caution because differences in study design (e.g., fixed dose vs flexible dose, variations in inclusion/exclusion criteria) may influence Cohen’s d values.
The NNT may be a particularly useful and clinically applicable measure when evaluating the effectiveness of therapeutic interventions, including treatments for neurological disorders [37]. Single-digit NNTs are considered to be clinically meaningful, with lower NNTs indicative of more robust treatment effects [30]. In this analysis, the NNT for achieving ESS score normalization with pitolisant was 4 (HARMONY 1) or 5 (HARMONY CTP), which is comparable to the NNTs observed in studies of other commonly used narcolepsy medications at approved doses (e.g., solriamfetol, armodafinil) [38, 39]. In addition to ESS score normalization, other thresholds have been used to identify a clinically meaningful change on the ESS (e.g., a > 20% or > 25% reduction in the total score [40, 41]). In the present analysis, an ESS score decrease of ≥ 3 (or an ESS score in the normal range) was used to define a clinically meaningful reduction in EDS, with an NNT of 3 (HARMONY CTP) or 5 (HARMONY 1) observed for pitolisant in attaining this outcome. A change in the frequency of cataplexy was evaluated using three different thresholds; for a reduction in WRC of ≥ 50% (which is consistent with a clinically meaningful change as identified in a separate analysis of narcolepsy study data [40]), the NNT for pitolisant was 3.
The NNT has been used to evaluate the effectiveness of treatments for other neurological disorders [42]. The NNTs reported for widely recognized standard-of-care treatments for epilepsy (e.g., topiramate, levetiracetam, sodium valproate, zonisamide, lamotrigine, gabapentin) and migraine (oral triptans) have been in the range of 4–12 [43,44,45], which is comparable to (or higher than) those observed in this analysis of pitolisant for the treatment of EDS and cataplexy.
Additional considerations when evaluating the clinical impact of a treatment for narcolepsy include the time to onset of a therapeutic response, effectiveness across the range of symptom severity, and safety/tolerability. In a post hoc analysis evaluating the time to onset of clinical response for pitolisant (up to a possible maximum dose of 35.6 mg/day), an initial response was observed for both EDS and cataplexy within 2–3 weeks of starting treatment, which is during the recommended titration period, with larger response rates observed as the dose of pitolisant was increased [46]. In a pooled post hoc analysis of patients with a high burden of symptoms at baseline (i.e., ESS score of ≥ 16 or WRC ≥ 15), the LS mean change in ESS score was significantly greater for pitolisant (− 6.1) vs placebo (− 2.3; p < 0.001) as was the LS mean change in WRC (− 14.5 vs − 0.1; p = 0.004), indicating that pitolisant was effective in the treatment of patients with more severe narcolepsy symptoms [47].
Pitolisant is generally well tolerated in patients with narcolepsy; across clinical trials, the most common adverse events (incidence ≥ 5% in pitolisant-treated patients and two or more times the rate with placebo) were insomnia (6% vs 2%), nausea (6% vs 3%), and anxiety (5% vs 1%), and the rate of discontinuation because of adverse events was comparable for pitolisant (3.9%) and placebo (3.5%) [25]. In addition, pitolisant demonstrated minimal to no potential for abuse in a clinical human abuse potential study [48] and was approved by the US Food and Drug Administration without being scheduled as a controlled substance. The 2 to 3 weeks’ time to the onset of therapeutic response, effectiveness across the range of symptom severity, and favorable safety and tolerability profile further corroborate the robust clinical impact of pitolisant in the treatment of narcolepsy [25, 47, 48].
This analysis has several limitations that should be noted. As this was a post hoc analysis, these outcomes were not prespecified and the studies were not powered to evaluate them. The data for this analysis were obtained from rigorously designed studies, and generalizability to patients in real-world treatment settings is unknown.
5 Conclusions
In conjunction with the primary results from RCTs, the results of this analysis demonstrate the robust efficacy of pitolisant for the reduction in both EDS and cataplexy in adults with narcolepsy. The large effect sizes and low NNTs observed in this analysis add to the evidence that the results of the pitolisant RCTs demonstrate clinically meaningful reductions in EDS and cataplexy. The strength of this evidence suggests that pitolisant should be considered as a first-line treatment in adult patients with narcolepsy.
References
Scammell TE. Narcolepsy. N Engl J Med. 2015;373:2654–62.
Bassetti CLA, Adamantidis A, Burdakov D, et al. Narcolepsy: clinical spectrum, aetiopathophysiology, diagnosis and treatment. Nat Rev Neurol. 2019;15:519–39.
American Academy of Sleep Medicine. The International Classification of Sleep Disorders. Darien: American Academy of Sleep Medicine; 2014.
Mahoney CE, Cogswell A, Koralnik IJ, et al. The neurobiological basis of narcolepsy. Nat Rev Neurosci. 2019;20:83–93.
Liblau RS, Vassalli A, Seifinejad A, et al. Hypocretin (orexin) biology and the pathophysiology of narcolepsy with cataplexy. Lancet Neurol. 2015;14:318–28.
Evans R, Tanaka S, Tanaka S, et al. A phase 1 single ascending dose study of a novel orexin 2 receptor agonist, TAK-925, in healthy volunteers (HV) and subjects with narcolepsy type 1 (NT1) to assess safety, tolerability, pharmacokinetics, and pharmacodynamic outcomes. Sleep Med. 2019;64:S105–6.
ClinicalTrials.gov. A study of TAK-994 in adults with type 1 and type 2 narcolepsy, study NCT04096560. https://clinicaltrials.gov/ct2/show/NCT04096560. Accessed 12 Nov 2021.
Pellitteri G, de Biase S, Valente M, et al. How treatable is narcolepsy with current pharmacotherapy and what does the future hold? Expert Opin Pharmacother. 2021;22:1517–20.
Barateau L, Dauvilliers Y. Recent advances in treatment for narcolepsy. Ther Adv Neurol Disord. 2019;12:1756286419875622.
Thorpy MJ. Recently approved and upcoming treatments for narcolepsy. CNS Drugs. 2020;34:9–27.
Thorpy MJ, Bogan RK. Update on the pharmacologic management of narcolepsy: mechanisms of action and clinical implications. Sleep Med. 2020;68:97–109.
Scammell TE, Jackson AC, Franks NP, et al. Histamine: neural circuits and new medications. Sleep. 2019;42:1–8.
Panula P, Nuutinen S. The histaminergic network in the brain: basic organization and role in disease. Nat Rev Neurosci. 2013;14:472–87.
Parmentier R, Ohtsu H, Djebbara-Hannas Z, et al. Anatomical, physiological, and pharmacological characteristics of histidine decarboxylase knock-out mice: evidence for the role of brain histamine in behavioral and sleep–wake control. J Neurosci. 2002;22:7695–711.
Haas HL, Sergeeva OA, Selbach O. Histamine in the nervous system. Physiol Rev. 2008;88:1183–241.
Schwartz JC. The histamine H3 receptor: from discovery to clinical trials with pitolisant. Br J Pharmacol. 2011;163:713–21.
Benarroch EE. Histamine in the CNS: multiple functions and potential neurologic implications. Neurology. 2010;75:1472–9.
Arrang JM, Garbarg M, Lancelot JC, et al. Highly potent and selective ligands for histamine H3-receptors. Nature. 1987;327:117–23.
Nieto-Alamilla G, Márquez-Gómez R, García-Gálvez AM, et al. The histamine H3 receptor: structure, pharmacology, and function. Mol Pharmacol. 2016;90:649–73.
de Biase S, Pellitteri G, Gigli GL, et al. Evaluating pitolisant as a narcolepsy treatment option. Expert Opin Pharmacother. 2021;22:155–62.
Lamb YN. Pitolisant: a review in narcolepsy with or without cataplexy. CNS Drugs. 2020;34:207–18.
Lin JS, Sergeeva OA, Haas HL. Histamine H3 receptors and sleep-wake regulation. J Pharmacol Exp Ther. 2011;336:17–23.
Ligneau X, Perrin D, Landais L, et al. BF2.649 [1-{ 3-[3-(4-chlorophenyl) propoxy] propyl} piperidine, hydrochloride], a nonimidazole inverse agonist/antagonist at the human histamine H3 receptor: preclinical pharmacology. J Pharmacol Exp Ther. 2007;320:365–75.
Lin JS, Dauvilliers Y, Arnulf I, et al. An inverse agonist of the histamine H3 receptor improves wakefulness in narcolepsy: studies in orexin-/- mice and patients. Neurobiol Dis. 2008;30:74–83.
Wakix® (pitolisant) tablets, for oral use. Package insert. Plymouth Meeting (PA): Harmony Biosciences, LLC; 2020.
Wakix®. Summary of product characteristics [SPC]. https://www.ema.europa.eu/documents/product-information/wakix-epar-product-information_en.pdf. Accessed 12 Nov 2021.
Dauvilliers Y, Bassetti C, Lammers GJ, et al. Pitolisant versus placebo or modafinil in patients with narcolepsy: a double-blind, randomised trial. Lancet Neurol. 2013;2:1068–75.
Szakacs Z, Dauvilliers Y, Mikhaylov V, et al. Safety and efficacy of pitolisant on cataplexy in patients with narcolepsy: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2017;16:200–7.
Dauvilliers Y, Arnulf I, Szakacs Z, et al. Long-term use of pitolisant to treat patients with narcolepsy: Harmony III study. Sleep. 2019;42:1–11.
Citrome L. Quantifying clinical relevance. Innov Clin Neurosci. 2014;11:26–30.
Citrome L, Ketter TA. When does a difference make a difference? Interpretation of number needed to treat, number needed to harm, and likelihood to be helped or harmed. Int J Clin Pract. 2013;67:407–11.
Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14:540–5.
Johns M, Hocking B. Excessive daytime sleepiness: daytime sleepiness and sleep habits of Australian workers. Sleep. 1997;20:844–9.
Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Mahwah: Lawrence Erlbaum Associates; 1988.
Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4:863.
Black J, Swick T, Bogan R, et al. Impact of sodium oxybate, modafinil, and combination treatment on excessive daytime sleepiness in patients who have narcolepsy with or without cataplexy. Sleep Med. 2016;24:57–62.
Bussière M, Wiebe S. Progress in clinical neurosciences: measuring the benefit of therapies for neurological disorders. Can J Neurol Sci. 2005;32:419–24.
Rosenberg R, Baladi M, Bron M. Clinically relevant effects of solriamfetol on excessive daytime sleepiness: a posthoc analysis of the magnitude of change in clinical trials in adults with narcolepsy or obstructive sleep apnea. J Clin Sleep Med. 2021;17:711–7.
Harsh JR, Hayduk R, Rosenberg R, et al. The efficacy and safety of armodafinil as treatment for adults with excessive sleepiness associated with narcolepsy. Curr Med Res Opin. 2006;22:761–74.
Steffen AD, Lai C, Weaver TE. Criteria for gauging response to sodium oxybate for narcolepsy. J Sleep Res. 2018;27: e12628.
Scrima L, Emsellem HA, Becker PM, et al. Identifying clinically important difference on the Epworth Sleepiness Scale: results from a narcolepsy clinical trial of JZP-110. Sleep Med. 2017;38:108–12.
Bussière M, Wiebe S. The numbers needed to treat for neurological disorders. Can J Neurol Sci. 2005;32:440–9.
Bodalia PN, Grosso AM, Sofat R, et al. Comparative efficacy and tolerability of anti-epileptic drugs for refractory focal epilepsy: systematic review and network meta-analysis reveals the need for long term comparator trials. Br J Clin Pharmacol. 2013;76:649–67.
Brigo F, Lattanzi S, Igwe SC, et al. Zonisamide add-on therapy for focal epilepsy. Cochrane Database Syst Rev. 2020;7: CD001416.
Adelman JU. Meta-analysis of oral triptan therapy for migraine: number needed to treat and relative cost to achieve relief within 2 hours. J Manage Care Pharm. 2003;9:45–52.
Watson NF, Davis CW, Zarycranski D, et al. Time to onset of response to pitolisant for the treatment of excessive daytime sleepiness and cataplexy in patients with narcolepsy: an analysis of randomized placebo-controlled trials. CNS Drugs. 2021;35(12):1303–15.
Davis CW, Kallweit U, Schwartz J-C, et al. Efficacy of pitolisant in patients with high burden of narcolepsy symptoms: pooled analysis of short-term, placebo-controlled studies. Sleep Med. 2021;81:210–7.
Setnik B, McDonnell M, Mills C, et al. Evaluation of the abuse potential of pitolisant, a selective H3-receptor antagonist/inverse agonist, for the treatment of adult patients with narcolepsy with or without cataplexy. Sleep. 2020;43:1–12.
Acknowledgements
Statistical analyses were conducted by Ben Vaughn, MS, Rho, Durham, NC, USA, and funded by Harmony Biosciences, LLC, Plymouth Meeting, PA, USA. Technical editorial and medical writing assistance was provided under the direction of the authors by Nancy Holland, PhD, Synchrony Medical Communications, LLC, West Chester, PA, USA, and funded by Harmony Biosciences, LLC, Plymouth Meeting, PA, USA. WAKIX is a registered trademark of Bioprojet Europe, Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
These studies (NCT01067222, NCT01800045) were funded by Bioprojet Pharma, Paris, France. Funding for this analysis was provided by Harmony Biosciences, LLC, Plymouth Meeting, PA, USA. Harmony Biosciences, LLC also funded open access publication of this article.
Conflicts of interest/competing interests
GJM reports serving on advisory boards and on the speakers’ bureau for Harmony Biosciences and Jazz Pharmaceuticals. CWD, DZ, MD, and JMD are employees of Harmony Biosciences. JCS is a co-founder of Bioprojet Pharma.
Availability of data and material
The datasets generated and/or analyzed for the current study are not publicly available.
Code availability
Not applicable.
Authors’ contributions
GJM: data analysis and interpretation, and review and editing of the article; CWD: conceptualization, data analysis and interpretation, and review and editing of the article; DZ: conceptualization, data analysis and interpretation, and review and editing of the article; MD: data analysis and interpretation, and review and editing of the article; JCS: data analysis and interpretation, and review and editing of the article; and JMD: data analysis and interpretation, and review and editing of the article. All authors provided input into the drafting of the manuscript, reviewed and approved the final version, and agree to be accountable for the work presented in the article.
Ethics approval
Both studies (NCT01067222, NCT01800045) were conducted in accordance with the Good Clinical Practice guidelines of the International Council for Harmonisation and the ethical principles of the Declaration of Helsinki. Each study protocol was approved by an institutional review board or independent ethics committee at each study site.
Consent to participate
All patients provided written informed consent before study enrollment.
Consent for publication
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Meskill, G.J., Davis, C.W., Zarycranski, D. et al. Clinical Impact of Pitolisant on Excessive Daytime Sleepiness and Cataplexy in Adults With Narcolepsy: An Analysis of Randomized Placebo-Controlled Trials. CNS Drugs 36, 61–69 (2022). https://doi.org/10.1007/s40263-021-00886-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-021-00886-x