Abstract
Background
Aripiprazole lauroxil (AL) is a long-acting injectable antipsychotic approved for treatment of schizophrenia in adults. Approved AL doses and dosing regimens include 441 mg monthly, 662 mg monthly, and 882 mg monthly or every 6 weeks (q6wk), as well as the most recently approved dose, 1064 mg, administered every 2 months.
Objective
Pharmacokinetics, safety, and tolerability of an AL regimen with a dose interval of every 2 months (1064 mg) were compared with two other regimens available as monthly and q6wk options.
Methods
This study evaluated pharmacokinetics of AL given at a higher dosage strength (1064 mg) and at a longer dose interval (every 8 weeks [q8wk]) than previously studied. Patients with schizophrenia or schizoaffective disorder entering this 44-week, phase I, open-label, multicenter study had no recent exposure to aripiprazole and were maintained on other oral antipsychotics throughout the study. Patients were randomized to one of three AL dose regimens for 24 weeks (four 1064-mg injections [q8wk], five 882-mg injections [q6wk], or seven 441-mg injections [q4wk], with the last AL exposure at week 24). Oral aripiprazole was prohibited. Patients were followed for an additional 20 weeks to assess terminal aripiprazole plasma concentrations and ongoing safety. Plasma concentration samples were obtained at regular intervals to provide pharmacokinetic data for the duration of AL exposure and to measure persistence of plasma aripiprazole concentrations after AL discontinuation.
Results
Eligible patients received AL 1064 mg q8wk (n = 35), 882 mg q6wk (n = 34), or 441 mg q4wk (n = 35). Overall, 103/104 (99.0%) patients were taking concomitant non-aripiprazole oral antipsychotic medications during the study. All three AL dose regimens provided continuous exposure to aripiprazole. Mean aripiprazole concentrations from the 1064-mg q8wk regimen were comparable to the 882-mg q6wk regimen and higher than the 441-mg q4wk regimen. Overall incidence by group of any adverse events (AEs) throughout the study was 68.6% (1064 mg q8wk), 50.0% (882 mg q6wk), and 65.7% (441 mg q4wk). The most common AE across regimens was injection-site pain (range 8.6%–11.4%). Serious AEs were reported by eight patients (all but one [increased psychosis in one patient, 441-mg q4wk group] considered unrelated to study drug). Discontinuations due to AEs were reported for 2.9%, 11.8%, and 5.7% of patients receiving the 8-, 6-, and 4-week regimens, respectively. AEs of akathisia, dyskinesia, and dystonia occurred in 2.9%, 8.6%, and 5.7% of patients in the 1064-mg q8wk group, 8.8%, 0%, and 2.9% in the 882-mg q6wk group, and 8.6%, 0%, and 0% in the 441-mg q4wk group, respectively.
Conclusions
AL 1064 mg q8wk provided continuous exposure to aripiprazole throughout the 8-week dosing interval and had a safety profile consistent with the 4- and 6-week regimens. These findings were used to support FDA approval of the 1064-mg dose administered every 2 months.
Registration
Clinicaltrials.gov: NCT02320032
Similar content being viewed by others
Avoid common mistakes on your manuscript.
It is clinically important to have longer dose interval options for patients treated with long-acting injectable antipsychotics. |
This study evaluated the pharmacokinetics and safety of a higher dosage strength of aripiprazole lauroxil (AL; 1064 mg) for suitability to extend the longest available dose interval of AL to 2 months. |
The results of this study demonstrated that the 1064-mg dosage strength given every 2 months had plasma concentrations and a safety profile comparable to those of 441 mg monthly and 882 mg every 6 weeks. |
1 Introduction
Long-acting injectable (LAI) atypical antipsychotics are an alternative to daily oral antipsychotics for treating schizophrenia [1, 2]. While long-acting treatment does not guarantee adherence, the nature of the fixed treatment schedule for injections given in clinical settings allows real-time assessment of a patient’s ongoing adherence status and is often recommended for patients who struggle with taking daily oral antipsychotic medication. Nonetheless, long-acting regimens have their own set of challenges, including the need to provide staffing and logistical support to be able to administer the injection at a scheduled visit. Therefore, in some settings, the injection interval can be a factor that is relevant to the feasibility of administering LAIs. In addition, the injection interval may be a major determinant of LAI acceptability; for example, when the patient or family lives far away from the treatment facility. Taken together, staffing constraints, lengthy travel times, and patient preference can present ‘real world’ challenges that limit the use of LAIs for patients who otherwise might be excellent LAI candidates. Some of these constraints may be mitigated by having LAIs with longer dose intervals. Given the need to maintain therapeutic plasma levels for the entire interval between injections, the pharmacokinetics of some long-acting options may limit the maximal length of the dosing interval.
Aripiprazole lauroxil (AL) is a prodrug developed to provide sustained release of aripiprazole into the plasma circulation [3]. The efficacy of AL was demonstrated in a phase III, 12-week, double-blind study comparing two dose regimens of AL (441 and 882 mg) given every 4 weeks (q4wk) with placebo for the treatment of acute symptoms of schizophrenia [4]. In that study, both dose regimens of AL were efficacious and well tolerated. In addition to the clinical data, pharmacokinetic modeling data for the 882-mg dose showed that steady-state plasma AL levels supported the feasibility of extending the dose interval of 882 mg to every 6 weeks (q6wk) [5]. Therefore, clinicians have the option of choosing the 882-mg dose for either a 4- or 6-week interval.
Based on an initial pharmacokinetic model [5], it was hypothesized that increasing the AL dosage strength to 1064 mg would achieve and sustain adequate aripiprazole plasma concentrations to extend the longest dose interval from 6 weeks to 2 months [3]. The phase I study described here was used to support the approval of the 1064-mg every 2 months AL regimen, which is the most recently approved AL dose regimen. Because the efficacy of the other AL regimens is established, the primary objective was to confirm that this higher dose strength would have a pharmacokinetic profile to support a 2-month interval with safety comparable to that of the other AL regimens. Therefore, this comprehensive study evaluated three AL dose regimens with different dosage strengths and dose intervals (1064 mg every 8 weeks [q8wk], 882 mg q6wk, and 441 mg q4wk). Another aspect of the safety and pharmacokinetic evaluation was to include a post-treatment evaluation period of 20 weeks, which is considerably longer than in most pharmacokinetics safety studies. Some pharmacokinetics results from this study were reported previously [6]; we provide additional analyses of pharmacokinetic data as well as full safety and tolerability results for each AL dose/dosing regimen.
This study also included a fourth treatment arm of a different formulation of AL 1064 mg known as 1064 mg (S). The particle size of the 1064 mg (S) formulation was larger and had a smaller surface-area-to-mass ratio compared with that of the commercially available AL formulations. The 1064 mg (S) formulation was included in the study in case the 1064-mg formulation did not meet the pharmacokinetic targets for a 2-month dose interval because, in theory, the larger particle size of 1064 mg (S) might decrease the rate of dissolution of the drug particles. Because the 1064-mg formulation met the criteria for a 2-month dose interval option, and the 1064 mg (S) did not offer any advantage over the 1064-mg formulation, its development was discontinued after study completion. Therefore, the 1064 mg (S) results are not included in this report.
2 Methods
This was a 44-week, phase I, open-label study to evaluate the pharmacokinetics, safety, and tolerability of different dose/dosing interval regimens of AL in patients with stable schizophrenia or schizoaffective disorder, and included a 24-week AL exposure period as well as a 20-week safety and pharmacokinetic post-treatment follow-up period. The study (Clinicaltrials.gov identifier: NCT02320032) was conducted from December 2014 to April 2016 in 15 centers in the United States in accordance with the ethical principles described in the Declaration of Helsinki and Good Clinical Practice Guidelines. Each eligible, consenting study participant provided written informed consent before study entry.
Because the primary outcomes of interest were the course of plasma aripiprazole concentrations and safety outcomes, patients continued on non-aripiprazole oral antipsychotics throughout the entire 44-week study period.
2.1 Study Design
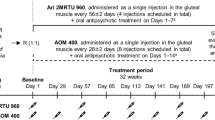
After an initial 30-day screening period, the 44-week open-label study comprised a 24-week treatment period and a 20-week post-treatment follow-up period (Fig. 1). Eligible patients were randomized to one of four dosing regimens (1:1:1:1) using a randomization schedule developed by an independent biostatistician and applied through an Interactive Web Response System: AL 1064 mg q8wk, AL 1064 mg (S) formulation (the alternative AL formulation) q8wk, AL 882 mg q6wk, or AL 441 mg q4wk. As discussed above, the 1064 mg (S) formulation was not developed further, and the rest of the article will focus on the remaining three dose regimens. Of an initial study sample of 140 patients, 35 were randomized to the (S) formulation, leaving 105 patients randomized to the remaining three regimens. Hereafter, the methods and results reported focus only on the three AL regimens of interest (n = 105).
Study design. Arrows denote time of dosage. Breaks in the horizontal bars depict the three different dose intervals for the dose/dose interval groups. The double-line break on the right-hand side of the x-axis depicts the 20-week follow-up period after the last dose (not drawn to scale). In-clinic visits occurred approximately every 2 weeks for all patients (not shown). Patient screening period is not shown here. It is important to note that, unlike in clinical treatment, 21-day oral aripiprazole lead-in treatment was not administered in this study. *Injection volume for indicated doses: 1064 mg q8wk, 3.9 mL; 882 mg q6wk, 3.2 mL; 441 mg q4wk, 1.6 mL. AL aripiprazole lauroxil, q4wk every 4 weeks, q6wk every 6 weeks, q8wk every 8 weeks, wk week
AL was administered in all regimens via intramuscular (IM) gluteal injections by study center personnel. Patients received their assigned open-label dose at different scheduled intervals (Fig. 1), corresponding to a total of four, five, or seven injections of 1064-, 882-, or 441-mg doses of AL, respectively, over 24 weeks. Study visits included safety assessments and plasma pharmacokinetics sampling and were conducted every 2 weeks throughout the 24 weeks of active AL exposure. The last dose was given at the week 24 visit (day 169) for all three AL regimens. Patients continued to be followed with additional safety and plasma pharmacokinetics sampling visits for another 20 weeks until the end of the follow-up period (Fig. 1).
Oral aripiprazole was prohibited for the duration of this study (except for two 5-mg test doses given during screening to assess tolerability in patients without prior aripiprazole exposure). Patients who were stable on any other oral antipsychotic treatment at screening were permitted to continue their medication for the duration of the study.
2.2 Patients
Eligible patients were adults between 18 and 65 years of age with a primary diagnosis of schizophrenia or schizoaffective disorder as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [7], and were clinically stable at screening (defined as no psychiatric hospitalization for at least 3 months and a Clinical Global Improvement–Severity Subscale [CGI-S] score ≤ 3) [8]. Patients should also have been maintained on an antipsychotic medication regimen (apart from those mentioned in the exclusion criteria) for at least 2 months before screening.
Exclusion criteria included having a primary diagnosis other than schizophrenia or schizoaffective disorder, a history of intolerance to any form of aripiprazole, or any LAI exposure within 3 months before screening.
2.3 Concomitant Medications
Patients with ongoing or recent exposure to aripiprazole were excluded, as defined by exposure to any long-acting aripiprazole within 6 months of screening or oral aripiprazole within 28 days of randomization. Patients were also excluded if they had any known factor that would cause significant alterations in aripiprazole metabolism or plasma concentrations of aripiprazole (e.g., patients receiving potent oral inhibitors of the cytochrome P450 isoenzyme CYP2D6, such as fluoxetine, within 30 days before screening were excluded).
AL can be initiated with 21 days of oral aripiprazole. However, because of the nature of the phase I pharmacokinetics analysis, no initiation regimen was given. Almost all patients entering this study were maintained on a stable dose of a first-line (non-clozapine) oral antipsychotic that was continued throughout the 24 weeks of AL exposure and 20-week follow-up pharmacokinetics safety period.
2.4 Pharmacokinetics
Pharmacokinetic assessments were carried out as described previously [6]. Briefly, a total of up to 48 plasma samples were collected throughout the 44 weeks to measure plasma concentrations of aripiprazole over time using a validated analytical method.
2.5 Safety
Key safety assessments included adverse events (AEs), serious AEs (SAEs), discontinuations due to AEs, and injection-site reactions (ISRs) at each study visit. Extrapyramidal symptoms (EPS), here broadly defined to encompass akathisia, dyskinesia, dystonia, and Parkinson-like events, were assessed as AEs. In addition, EPS were evaluated using Extrapyramidal Symptom Rating Scale (ESRS) scores ≥ 2 for parkinsonism, akathisia, dystonia, or dyskinesia at any postbaseline visit [9].
Because the dose and volume associated with the AL 1064-mg regimen are higher than those associated with the other dosing regimens, ISRs were carefully monitored throughout the study. All patients, regardless of injection interval, were assessed for ISRs every 2 weeks. Patients who completed the study received 13 ISR assessments over the 24 weeks of AL treatment and an additional 10 ISR assessments in the 20-week follow-up period.
2.6 Statistical Analysis
The pharmacokinetics population included all patients who received one or more dose of study drug and had at least one measurable concentration of aripiprazole. Pharmacokinetics parameters were calculated using noncompartmental techniques and summarized with descriptive statistics [6]. Calculated pharmacokinetics parameters reported here included area under the plasma drug concentration–time curve over the dosing interval (AUCτ), AUCτ normalized to dose (AUCτ/D), AUC from time zero until the last measurable plasma drug concentration time point (AUClast), average concentration (Cavg), maximum concentration (Cmax), time to Cmax (tmax), and half-life (t½). Additional pharmacokinetics results from this study have been reported previously [6]. The safety population included all randomized patients who received one or more dose of AL. Summary statistics were calculated for safety parameters, including mean, SD, median, minimum, and maximum values for continuous variables, and number and percentage of patients in each category for categorical variables.
Dose proportionality of aripiprazole was assessed using AUClast and Cmax over the studied dose range using the following power model: log (pharmacokinetics parameter) = μ + β × log (dose), where ‘μ’ was the intercept and ‘β’ was the slope. Estimates of slope and intercept with respective SEs and associated 90% CIs were calculated.
3 Results
3.1 Patient Disposition
The population in the analysis presented here included 104 patients who received at least one dose of the currently approved formulations of AL (1064 mg q8wk [n = 35], 882 mg q6wk [n = 34], and 441 mg q4wk [n = 35]); one patient randomized to 882 mg q6wk did not receive study drug (Fig. 2). For the 1064-mg q8wk group, 29 (82.9%) received their complete course of four injections, compared with 24 (70.6%) in the 882-mg q6wk group completing five injections and 29 (82.9%) in the 441-mg q4wk group completing seven injections. In total, 73.1% (76/104) of patients completed the study (i.e., received all of the injections associated with their dose/dosing interval assignment and completed the follow-up visit at study end).
Among the 28 (26.9%) patients in total who discontinued the study prematurely, the most common reasons by treatment arm were patient withdrawal of consent (11.4%) in the 1064-mg q8wk group and loss to follow-up in the 882-mg q6wk and 441-mg q4wk groups (17.6% and 8.6%, respectively).
3.2 Baseline Characteristics and Concomitant Medications
Patients entering this study were predominantly men (71.2%); mean age was 44.3 years (Table 1). Mean Clinical Global Impressions of Severity score was just under 3 (mildly ill) at study entry for all groups. Almost all patients (103/104 [99.0%]) were taking concomitant oral antipsychotic medications. As shown in Table 1, concomitant antipsychotics were prescribed at doses consistent with prescribing patterns in the United States, with risperidone being more frequent and at doses representative of outpatient maintenance treatment of schizophrenia.
3.3 Pharmacokinetics
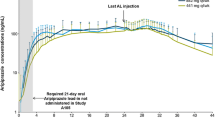
Analysis of plasma aripiprazole concentration over time showed that all treatment regimens provided continuous exposure to aripiprazole; mean aripiprazole concentrations with 1064 mg q8wk were comparable to those with 882 mg q6wk and were higher than those with 441 mg q4wk for the entire dosing interval (Fig. 3). During the 20-week follow-up period after the last injection of AL, plasma aripiprazole levels declined relatively slowly (Fig. 3).

Reproduced from Hard ML, Mills RJ, Sadler BM, Wehr AY, Weiden PJ, von Moltke L. Pharmacokinetic profile of a 2-month dose regimen of aripiprazole lauroxil: a phase I study and a population pharmacokinetic model. CNS Drugs. 2017;31(7):617–624; used with permission. AL aripiprazole lauroxil, q4wk every 4 weeks, q6wk every 6 weeks, q8wk every 8 weeks, wk week
Mean (SD) aripiprazole concentration over time.
A summary of key pharmacokinetics parameters for aripiprazole after the first dose and the last dose of AL is presented in Table 2. After the first injection, the exposure to aripiprazole, based on Cmax and AUC, increased with increasing dose. A similar dose-related increase was noted after the last dose in AUC but was less apparent in Cmax. On average, accumulation ratios for aripiprazole (AUCτ [last dose]/AUCτ [first dose]) were 2.0, 2.6, and 9.7 for the 1064-mg q8wk, 882-mg q6wk, and 441-mg q4wk groups, respectively. Mean Cavg after the final dose was higher with AL 1064 mg q8wk (140.7 ng/mL) than with 882 mg q6wk (131.1 ng/mL) and 441 mg q4wk (125.8 ng/mL; Table 2). In the power model, the 90% confidence intervals (CIs) for the estimates of slope included 1, and dose-adjusted normalized AUClast and Cmax values across the doses overlapped, suggesting dose linearity in the pharmacokinetics parameters (Table 3). Furthermore, dose-related increases were observed for AUCτ following the last dose (Fig. 4a), and values for dose-normalized AUCτ (including medians) were similar and showed overlap across the regimens (Fig. 4b), indicating dose proportionality of AL. Values for Cavg at steady state showed that average aripiprazole concentrations with the 1064-mg q8wk regimen were similar to those with 882 mg q6wk and higher than those with 441 mg q4wk (Fig. 5).
Box plots of a area under the plasma aripiprazole concentration–time curve over the dosing interval (AUCτ) and b AUCτ normalized to dose by treatment group following the last dose. Boxes represent the 75th and 25th percentiles; the line within each box represents the median, and the ‘ + ’ represents the mean. Whiskers indicate the minimum and maximum. AUCτ area under the plasma drug concentration–time curve over the dosing interval, AUCτ/D dose-normalized AUCτ; q4wk every 4 weeks, q6wk every 6 weeks, q8wk every 8 weeks
Box plot of average concentration for aripiprazole following the last dose by treatment group. Boxes represent the 75th and 25th percentiles; the line within each box represents the median, and the ‘plus’ represents the mean. Whiskers indicate the minimum and maximum. Cavg mean plasma drug concentration, q4wk every 4 weeks, q6wk every 6 weeks, q8wk every 8 weeks
3.4 Safety
The overall incidence of AEs over 44 weeks was 68.6%, 50.0%, and 65.7% in the 1064-mg q8wk, 882-mg q6wk, and 441-mg q4wk groups, respectively (Table 4); most AEs were of mild or moderate intensity. The most common AE across the three AL regimens was injection-site pain (8.6%–11.4%); weight increase, nasopharyngitis, and hypertension also occurred in > 5% of patients in each of the three dose/dosing interval groups.
Serious AEs were reported by 7.7% (n = 8) of the total study population: 8.6% (n = 3) of patients in the 1064-mg q8wk group (one patient each with knee injury, worsening of schizophrenia, and diabetic ketoacidosis), 8.6% (n = 3) in the 441-mg q4wk group (one patient each with increased psychosis, exacerbation of schizophrenia, and agitation), and 5.9% (n = 2) in the 882-mg q6wk group (one patient with worsening of osteoarthritis and one patient with cardiac arrest, acute respiratory failure, and acute myocardial infarction). With the exception of one event (increased psychosis in the 882-mg q6wk group, assessed as possibly related to study drug), SAEs were considered to be unrelated to AL.
AEs leading to study discontinuation occurred in 6.7% (n = 7) of the study population: 2.9% (n = 1) in the 1064-mg q8wk group (worsening schizophrenia), 11.8% (n = 4) in the 882-mg q6wk group (osteoarthritis, musculoskeletal stiffness, disturbance of attention, and cardiac arrest), and 5.7% (n = 2) in the 441-mg q4wk group (increased psychosis and epistaxis).
Overall, 11.5% (n = 12) of patients reported ISRs; the 1064-mg q8wk group had an ISR frequency of 14.3%, compared with 8.8% for the 882-mg q6wk group and 11.4% for the 441-mg q4wk group (Table 5). None of the ISRs were severe, and no patient discontinued the study because of an ISR. Pain was the most commonly reported ISR (83.3% [10/12 ISR events]; Table 5), with a similar incidence across all dose/dosing interval groups (75% [3/4 ISR events], 100% [3/3 ISR events], and 80% [4/5 ISR events] in the 1064-mg q8wk, 882-mg q6wk, and 441-mg q4wk groups, respectively; Table 5).
For the overall patient population, the first injection was associated with the highest occurrence of ISRs relative to subsequent injections (Table 5). The reduction in incidence of ISR as a function of number of injections already received was seen for all three dose/dosing interval groups. The incidence of any ISR in the 1064-mg q8wk group decreased from 5.7% with the first injection to 3.4% with the fourth injection.
Overall, 11.4% (n = 4), 17.6% (n = 6), and 14.3% (n = 5) of patients in the 1064-mg q8wk, 882-mg q6wk, and 441-mg q4wk groups, respectively, had AEs associated with EPS (Table 4). Akathisia was reported in 2.9% (n = 1), 8.8% (n = 3), and 8.6% (n = 3) of patients in the 1064-mg q8wk, 882-mg q6wk, and 441-mg q4wk groups, respectively. Dyskinesia was reported in three patients (8.6%) in the 1064-mg q8wk group but was not reported in any patients in the 882-mg q6wk or 441-mg q4wk groups.
Additional assessments also demonstrated minimal effects on movement disorders; mean changes from baseline in ESRS scores were generally small and not clinically meaningful. The proportions of patients with akathisia, dyskinesia, parkinsonism, and dystonia assessed using the ESRS (CGI-S item score ≥ 2 in ESRS at any postbaseline visit) in the 1064-mg q8wk group (5.7%, 5.7%, 8.6%, and 8.6%, respectively) were similar to those in the 441-mg q4wk (2.9%, 5.7%, 5.7%, 0%) and 882-mg q6wk groups (5.9%, 8.8%, 8.8%, 2.9%).
4 Discussion
In this study, the pharmacokinetics, safety, and tolerability of the 1064-mg q8wk regimen were compared with those of two other approved AL regimens. Pharmacokinetics data from the study presented in this article as well as another publication [6] show that plasma aripiprazole concentrations achieved with the AL 1064-mg q8wk regimen were found to be within the upper and lower limits of the range associated with clinically effective and well tolerated doses of AL, as determined in a phase III efficacy study of two AL doses, 441 mg q4wk and 882 mg q4wk [4], and aripiprazole exposure increased with increasing AL dose. In addition, administration of AL 1064 mg q8wk resulted in plasma aripiprazole concentrations comparable to that observed with administration of 882 mg q6wk for the entire dosing interval. Although some patients were receiving concomitant antipsychotics metabolized by CYP2D6 (i.e., risperidone or haloperidol), given the in vivo CYP2D6 inhibitory profile of these antipsychotics [10,11,12], it is not anticipated that these or any of the other non-aripiprazole concomitant oral antipsychotics would affect the pharmacokinetics of aripiprazole. The overall safety profile of the AL 1064-mg q8wk regimen was similar to that of the other two AL regimens in this population of patients with stable schizophrenia. The safety profile of the 1064-mg q8wk regimen was also consistent with that of oral aripiprazole as well as the known safety profile of AL [4, 13,14,15,16,17].
The incidence of ISRs was comparable for each dosage group. Given that the frequency of ISRs for the 882-mg q6wk group (8.8%) was lower than that for both the 441-mg q4wk (11.4%) and 1064-mg q8wk (14.3%) groups, the frequency of ISRs reported did not demonstrate an association with the dose or volume of AL. The incidence of injection-site pain in this phase I study was higher than the incidence previously reported for AL 441-mg q4wk and 882-mg q4wk regimens [4, 18]. We hypothesize that these differences may be related to the study design of the current phase I study, which focused primarily on safety. Higher ISR (pain) rates associated with phase I studies for another long-acting formulation of aripiprazole (compared with later-phase/open-label studies) have also been noted [19, 20].
The overall incidence of EPS-related AEs was consistent with earlier results. There were no obvious differences in akathisia incidence between the 1064-mg q8wk group and the 882-mg q6wk or 441-mg q4wk groups. The incidence of akathisia events (2.9%–8.8%) in this study was consistent with that reported in the 52-week long-term study in patients who had not previously received AL (0.9%–4.6%) [18]. Higher frequencies of dystonia and dyskinesia as AEs were observed in the 1064-mg q8wk group in the current study compared with the 441-mg q4wk and 882-mg q4wk groups evaluated in the 52-week study (dystonia: 5.7% vs 1.4%–2.7%; dyskinesia: 8.6% vs 0%–0.5%) [18].
Results from this study demonstrate that the 1064-mg q8wk dosage regimen offers similar safety and tolerability to that of the 4- or 6-week dosage regimens of AL and comparable or higher aripiprazole plasma concentrations with the option of dosing only six times per year. Having a range of dosing interval options allows for greater flexibility in treatment planning. A 2-month dosing interval option may expand the range of ways to individualize the LAI regimen into the patient’s treatment plan, taking into account factors such as patient preferences, logistical barriers, or aligning injection regimen with other psychosocial interventions.
Limitations of the study included the lack of a placebo group or active control and the relatively small patient populations in each treatment group; therefore, no conclusions on dose-related effects could be drawn. The use of concomitant antipsychotic drugs makes it harder to attribute any new-onset AE to the prior oral antipsychotic, the AL exposure, or the combination of these. Presumably, the baseline AE assessment would capture any pre-existing AE associated with the ongoing oral antipsychotic; in addition, as part of ongoing AE monitoring, investigators were asked their assessment of the likelihood of any given AE as being attributable to study medication exposure. However, the primary goal of this analysis was to determine the relative safety of the 1064-mg dosage strength. Because all patients across the AL dose regimens were on other oral antipsychotics, presumably any impact of ongoing oral antipsychotic use would be equivalent across the randomized groups. The lack of serious AEs associated with dopamine antagonism (e.g., severe antipsychotic-induced parkinsonism) provides some additional information on the safety of AL with some other antipsychotics. We strongly caution the reader to use other sources of safety data from short-term and long-term phase III and phase IIIb studies as being a more accurate source of safety information for AL as a treatment for schizophrenia [4, 18, 21]. Nonetheless, the overall results of this safety analysis demonstrated a low incidence of EPS with AL even at higher doses and during prolonged treatment (together with concomitant oral antipsychotic medication).
5 Conclusions
The results of this study provide an overview of the pharmacokinetics and long-term safety profile associated with the administration of different dose/dosing interval regimens of AL in a variety of patient populations that might be encountered in the real-world clinical setting. Overall, the results from the current study show that AL 1064-mg q8wk, 882-mg q6wk, and 441-mg q4wk regimens provide continuous exposure to aripiprazole within the previously established clinically relevant range. Taking into consideration the limitations of the data derived from this study, including the fact that most patients were taking concomitant oral antipsychotic medications, AL across dosing groups appeared to be well tolerated and had a safety profile similar to the established safety profile of oral aripiprazole.
References
Kane JM. Treatment strategies to prevent relapse and encourage remission. J Clin Psychiatry. 2007;68(Suppl 14):27–30.
Kaplan G, Casoy J, Zummo J. Impact of long-acting injectable antipsychotics on medication adherence and clinical, functional, and economic outcomes of schizophrenia. Patient Prefer Adherence. 2013;7:1171–80.
Aristada [package insert]. Waltham, MA: Alkermes, Inc.; 2018.
Meltzer HY, Risinger R, Nasrallah HA, Du Y, Zummo J, Corey L, et al. A randomized, double-blind, placebo-controlled trial of aripiprazole lauroxil in acute exacerbation of schizophrenia. J Clin Psychiatry. 2015;76(8):1085–90.
Hard ML, Mills RJ, Sadler BM, Turncliff RZ, Citrome L. Aripiprazole lauroxil: pharmacokinetic profile of this long-acting injectable antipsychotic in persons with schizophrenia. J Clin Psychopharmacol. 2017;37(3):289–95.
Hard ML, Mills RJ, Sadler BM, Wehr AY, Weiden PJ, von Moltke L. Pharmacokinetic profile of a 2-month dose regimen of aripiprazole lauroxil: a phase I study and a population pharmacokinetic model. CNS Drugs. 2017;31(7):617–24.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, DSM-5. 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
Guy W. ECDEU Assessment Manual for Psychopharmacology. Rockville, MD: US Dept of Health, Education, and Welfare, Alcohol, Drug Abuse and Mental Health Administration, NIMH Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976.
Chouinard G, Margolese HC. Manual for the Extrapyramidal Symptom Rating Scale (ESRS). Schizophr Res. 2005;76(2–3):247–65.
Reyes JF, Preskorn SH, Khan A, Kumar D, Cullen EI, Perdomo CA, et al. Concurrent administration of donepezil HCl and risperidone in patients with schizophrenia: assessment of pharmacokinetic changes and safety following multiple oral doses. Br J Clin Pharmacol. 2004;58(Suppl 1):50–7.
Huang F, Lasseter KC, Janssens L, Verhaeghe T, Lau H, Zhao Q. Pharmacokinetic and safety assessments of galantamine and risperidone after the two drugs are administered alone and together. J Clin Pharmacol. 2002;42(12):1341–51.
Gram LF, Overo KF. Drug interaction: inhibitory effect of neuroleptics on metabolism of tricyclic antidepressants in man. Br Med J. 1972;1(5798):463–5.
Kane JM, Carson WH, Saha AR, McQuade RD, Ingenito GG, Zimbroff DL, et al. Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry. 2002;63(9):763–71.
Kane JM, Peters-Strickland T, Baker RA, Hertel P, Eramo A, Jin N, et al. Aripiprazole once-monthly in the acute treatment of schizophrenia: findings from a 12-week, randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2014;75(11):1254–60.
Potkin SG, Raoufinia A, Mallikaarjun S, Bricmont P, Peters-Strickland T, Kasper W, et al. Safety and tolerability of once monthly aripiprazole treatment initiation in adults with schizophrenia stabilized on selected atypical oral antipsychotics other than aripiprazole. Curr Med Res Opin. 2013;29(10):1241–51.
Nasrallah HA, Newcomer JW, Risinger R, Du Y, Zummo J, Bose A, et al. Effect of aripiprazole lauroxil on metabolic and endocrine profiles and related safety considerations among patients with acute schizophrenia. J Clin Psychiatry. 2016;77(11):1519–25.
Stip E, Tourjman V. Aripiprazole in schizophrenia and schizoaffective disorder: a review. Clin Ther. 2010;32(Suppl 1):S3–20.
Nasrallah HA, Aquila R, Du Y, Stanford AD, Claxton A, Weiden PJ. Long-term safety and tolerability of aripiprazole lauroxil in patients with schizophrenia. CNS Spectr. 2019;24(4):395–403.
Mallikaarjun S, Kane JM, Bricmont P, McQuade R, Carson W, Sanchez R, et al. Pharmacokinetics, tolerability and safety of aripiprazole once-monthly in adult schizophrenia: an open-label, parallel-arm, multiple-dose study. Schizophr Res. 2013;150(1):281–8.
Peters-Strickland T, Baker RA, McQuade RD, Jin N, Eramo A, Perry P, et al. Aripiprazole once-monthly 400 mg for long-term maintenance treatment of schizophrenia: a 52-week open-label study. NPJ Schizophr. 2015;1:15039.
Weiden PJ, Claxton A, Kunovac J, Walling DP, Du Y, Yao B, et al. Efficacy and safety of a 2-month formulation of aripiprazole lauroxil with 1-day initiation in patients hospitalized for acute schizophrenia transitioned to outpatient care: phase 3, randomized, double-blind, active control ALPINE study. J Clin Psychiatry. 2020;81(3):19m13207.
Acknowledgements
The authors thank all the patients and investigators who participated and contributed to this study. The authors also thank Dr. Chih-Chin Liu (formerly of Alkermes, Inc.) for her contribution to the biostatistical analyses of the study. Editorial support for the preparation of this manuscript (under the guidance of the authors) was provided by Karen Yee, Ph.D. (ApotheCom, London, UK), and Jane A. Phillips, Ph.D. (Peloton Advantage, LLC, Parsippany, NJ, USA, an OPEN Health company).
Author information
Authors and Affiliations
Contributions
Study conceptualization and design: LvM, MH (emphasis on pharmacokinetics). Data interpretation: PJW (safety), AW (pharmacokinetics), MM, DPW. Clinical trial investigator: MM, DPW. Statistical analysis: YD. Writing of first draft: PJW, AW (pharmacokinetics). Review and substantive edits: All authors. Approval of the final manuscript and decision to submit: All authors.
Corresponding author
Ethics declarations
Funding
This study was sponsored by Alkermes, Inc., Waltham, MA, USA. Funding for editorial support was provided by Alkermes, Inc., Waltham, MA, USA.
Conflict of Interest
P.J. Weiden, L. von Moltke, A. Wehr, and M. Hard are former employees of Alkermes, Inc., and may own stock/options in the company; Y. Du is currently an employee of Alkermes, Inc., and may own stock/options in the company; M. Hard is currently an employee of Moderna, Inc.; M. Marandi has received advisory and speaking fees from Alkermes, Inc.; D.P. Walling has received grants from Alkermes, Inc., Janssen, Otsuka, Forum, Lundbeck, Sunvion, Acadia, Allergan, IntraCellular, Noven, Merck, AbbVie, and Roche.
Research Involving Human Participants
The study was conducted in accordance with the ethical principles described in the Declaration of Helsinki and Good Clinical Practice Guidelines.
Informed Consent
Each eligible, consenting study participant provided written informed consent before study entry.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Weiden, P.J., Du, Y., von Moltke, L. et al. Pharmacokinetics, Safety, and Tolerability of a 2-Month Dose Interval Regimen of the Long-Acting Injectable Antipsychotic Aripiprazole Lauroxil: Results From a 44-Week Phase I Study. CNS Drugs 34, 961–972 (2020). https://doi.org/10.1007/s40263-020-00745-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-020-00745-1