Abstract
Background
The rate of an unintentional drug overdose involving prescription opioids continues to rise. An understanding of the threshold dose and dose(s) associated with unintentional prescription opioid overdose will help to mitigate this epidemic.
Objective
The objective of this systematic review is to systematically synthesise and meta-analyse studies on doses of prescription opioids and ascertain the doses of opioids that are associated with increased risk of severe opioid poisoning or mortality.
Data Sources
A search of PubMed, EMBASE, CINAHL and Web of Science from inception to 16 January 2017 was conducted using search strategies and the MeSH (Medical Subject Headings) terms for studies of adult patients using prescription opioids who experienced an accidental overdose.
Study Selection
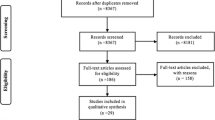
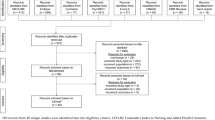
Of the 1332 studies identified, 117 were selected for full article review. Ten met the inclusion criteria for qualitative analysis, but only seven studies were meta-analysed. The included studies were in English, and participants met predetermined International Classification of Diseases (ICD) codes. Studies were excluded if they included only paediatric participants or the participants met the ICD code for intentional self-harm.
Data Extraction and Synthesis
Two researchers elaborated and validated a data extraction form. Data were then independently extracted by both reviewers as per this form. We assessed study quality using the Newcastle–Ottawa Scale (NOS) for non-randomised studies in meta-analyses. We performed a meta-regression using a random-effect model and summarised the results using relative risk (RR) and 95% confidence intervals (CIs). The threshold dose for an unintentional overdose is 20 morphine milligram equivalents (MME)/day. There were higher risks with larger doses: (1) ≤ 20 versus ≥ 21 MME/day: RR 2.81, 95% CI 1.09–7.22, p < 0.001; (2) ≤ 50 versus > 50 MME/day: RR 3.87, 95% CI 2.36–6.33, p < 0.001; (3) ≤ 100 versus > 100 MME/day: RR 4.28, 95% CI 2.61–7.1, p < 0.001; and (4) ≤ 50 versus > 50–100 MME/day: RR 3.09, 95% CI 1.84–5.18, p < 0.001). Heterogeneity was explained by the type of overdose event, inpatient or outpatient status, and length of observation. Type of pain (cancer or non-cancer pain) had no impact on heterogeneity.
Limitations
The definition of exposure in studies included in the meta-analysis was heterogeneous. Some studies defined exposure as the filling of a prescription while others defined exposure as the prescription of an opioid to the patient, and all studies assumed that patients took the prescribed opioid. Medications that may contribute to overdose, such as benzodiazepines and other drugs, were not considered.
Conclusions
A significantly increased risk of inadvertent prescription opioid overdose was found with 20–50 MME/day, with fatality more likely with opioid doses above 50 MME/day, although extensive heterogeneity was found with the dose comparisons. Clinicians should inform patients of this risk and monitor them closely.
Protocol Registration
This protocol was registered with PROSPERO 2017: CRD42017058426.


Similar content being viewed by others
References
Kissin I. Long-term opioid treatment of chronic nonmalignant pain: unproven efficacy and neglected safety? J Pain Res. 2013;6:513–29.
Manchikanti L, Abdi S, Atluri S, Balog CC, Benyamin RM, Boswell MV, et al.; American Society of Interventional Pain Physicians. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part I—evidence assessment. Pain Physician. 2012;15(3 Suppl):S1–65.
Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies—tackling the opioid-overdose epidemic. N Engl J Med. 2014;370(22):2063–6.
International Overdose Awareness Day. Overdose: worse than the road toll 2013. http://www.overdoseday.com/wp-content/uploads/Factsheet-Greater-than-the-Road-Toll-KE-FINAL-15-August-2013.pdf. Accessed 16 Feb 2017.
Warner M, Chen LH, Makuc DM, Anderson RN, Minino AM. Drug poisoning deaths in the United States, 1980–2008. NCHS Data Brief. 2011;81:1–8.
Centers for Disease Control and Prevention. (CDC). Unintentional poisoning deaths—United States, 1999–2004. MMWR. 2007;56(5):93–6.
Hasegawa K, Brown DFM, Tsugawa Y, Camargo CA. Epidemiology of emergency department visits for opioid overdose: a population-based study. Mayo Clin Proc. 2014;89(4):462–71.
Fernandes K, Martins D, Juurlink D, Mamdani M, Paterson JM, Spooner L, et al. High-dose opioid prescribing and opioid-related hospitalization: a population-based study. PLoS One. 2016;11(12):e0167479.
Inocencio TJ, Carroll NV, Read EJ, Holdford DA. The economic burden of opioid-related poisoning in the United States. Pain Med. 2013;14(10):1534–47.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American Psychiatric Association; 2013.
Dumas EO, Pollack GM. Opioid tolerance development: a pharmacokinetic/pharmacodynamic perspective. AAPS J. 2008;10(4):537–51.
Berecki-Gisolf J, Hassani-Mahmooei B, Clapperton A, McClure R. Prescription opioid dispensing and prescription opioid poisoning: population data from Victoria, Australia 2006 to 2013. Aust N Z J Public Health. 2017;41(1):85–91.
Dunn KM, Saunders KW, Rutter CM, Banta-Green CJ, Merrill JO, Sullivan MD, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92.
Zorzela L, Loke YK, Ioannidis JP, Golder S, Santaguida P, Altman DG, et al. PRISMA harms checklist: improving harms reporting in systematic reviews. BMJ. 2016;352:i157.
Herzig SJ, Rothberg MB, Cheung M, Ngo LH, Marcantonio ER. Opioid utilization and opioid-related adverse events in nonsurgical patients in US hospitals. J Hosp Med. 2014;9(2):73–81.
Paulozzi LJ, Kilbourne EM, Shah NG, Nolte KB, Desai HA, Landen MG, et al. A history of being prescribed controlled substances and risk of drug overdose death. Pain Med. 2012;13(1):87–95.
Ottawa Hospital Research Institute. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses 2014. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 14 Mar 2017.
Bae J-M. A suggestion for quality assessment in systematic reviews of observational studies in nutritional epidemiology. Epidemiol Health. 2016;38:e2016014.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Higgins JPT, Thompson SG. Controlling the risk of spurious findings from meta-regression. Stat Med. 2004;23(11):1663–82.
Gagnier JJ, Moher D, Boon H, Bombardier C, Beyene J. An empirical study using permutation-based resampling in meta-regression. Syst Rev. 2012;1(1):18.
Harbord RM, Higgins JPT. Meta-regression in Stata. Stata J. 2008;8(4):493–519.
Harbord RM, Harris RJ, Sterne JAC. Updated tests for small-study effects in meta-analyses. Stata J. 2009;9(2):197–210.
Dilokthornsakul P, Moore G, Campbell JD, Lodge R, Traugott C, Zerzan J, et al. Risk factors of prescription opioid overdose among Colorado Medicaid beneficiaries. J Pain. 2016;17(4):436–43.
Cochran G, Gordon AJ, Lo-Ciganic WH, Gellad WF, Frazier W, Lobo C, et al. An examination of claims-based predictors of overdose from a large Medicaid program. Med Care. 2017;55(3):291–8.
Dasgupta N, Funk MJ, Proescholdbell S, Hirsch A, Ribisl KM, Marshall S. Cohort study of the impact of high-dose opioid analgesics on overdose mortality. Pain Med. 2016;17(1):85–98.
Bohnert ASB, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–21.
Fulton-Kehoe D, Garg RK, Turner JA, Bauer AM, Sullivan MD, Wickizer TM, et al. Opioid poisonings and opioid adverse effects in workers in Washington State. Am J Ind Med. 2013;56(12):1452–62.
Fulton-Kehoe D, Sullivan MD, Turner JA, Garg RK, Bauer AM, Wickizer TM, et al. Opioid poisonings in Washington State Medicaid: trends, dosing, and guidelines. Med Care. 2015;53(8):679–85.
Larochelle MR, Liebschutz JM, Fang Z, Ross-Degnan D, Wharam JF, Zhang F. Opioid prescribing after nonfatal overdose and association with repeated overdose: a cohort study. Ann Intern Med. 2016;164(1):1–9.
Zedler B, Xie L, Wang L, Joyce A, Vick C, Kariburyo F, et al. Risk factors for serious prescription opioid-related toxicity or overdose among Veterans Health Administration patients. Pain Med. 2014;15(11):1911–29.
NCIS fact sheet. Opioids related deaths in Australia (2007–2011). Australia: National Coronial Information System; 2014. p. 1–20.
Australian Medicines Handbook. Morphine. In: Australian medicines handbook. Adelaide: Australian Medicines Handbook Pty Ltd; 2017. https://amhonline.amh.net.au/.
MS Contin modified release tablets. In: MIMS Australia. St Leonards: MIMS Australia Pty Ltd; 2017. Available from: http://www.mims.com.au.
Pattinson K. Opioids and the control of respiration. Br J Anaesth. 2008;100(6):747–58.
Iwabe T, Ozaki I, Hashizume A. The respiratory cycle modulates brain potentials, sympathetic activity, and subjective pain sensation induced by noxious stimulation. Neurosci Res. 2014;84:47–59.
Borgbjerg FM, Nielsen K, Franks J. Experimental pain stimulates respiration and attenuates morphine-induced respiratory depression: a controlled study in human volunteers. Pain. 1996;64(1):123.
Bourke DL. Respiratory effects of regional anesthesia during acute pain. Reg Anesth. 1993;18(6):361.
Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315(15):1624–45.
Cruccu G, Truini A. Tools for assessing neuropathic pain. PLoS Med. 2009;6(4):e1000045.
Sorg MH, Long DL, Abate MA, Kaplan JA, Kraner J, Greenwald MS, et al. Additive effects of cointoxicants in single-opioid induced deaths. Acad Forensic Pathol. 2016;6(3):532–42.
Garg KR, Fulton-Kehoe MD, Franklin MG. Patterns of opioid use and risk of opioid overdose death among medicaid patients. Med Care. 2017;55(7):661–8.
International classification of diseases. 10th rev. Geneva: WHO; 1992.
International classification of diseases. 9th rev. Geneva: WHO; 1977.
Acknowledgements
Special thanks to (a) Mr Glen Tapley, the Director of Pharmacy at the Maryborough Hospital for approving the time needed to complete this project and (b) Mr Olumuyiwa Omonaiye of Deakin University for assisting with part of the study selection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Adeleke D. Adewumi was supported by the Australian Government’s Research Training Program (RTP) scholarship. The funder had no role in the design or conduct of this study, including the acquisition, analysis and interpretation of data, as well as in the preparation, review or approval of manuscript or in the decision to submit for publication. No other conflict of interest is declared by authors Samantha A. Hollingworth, Joemer C. Maravilla, Jason P. Connor and Rosa Alati.
Funding
There are no other sources of funding to report.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Adewumi, A.D., Hollingworth, S.A., Maravilla, J.C. et al. Prescribed Dose of Opioids and Overdose: A Systematic Review and Meta-Analysis of Unintentional Prescription Opioid Overdose. CNS Drugs 32, 101–116 (2018). https://doi.org/10.1007/s40263-018-0499-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-018-0499-3