Abstract
Background and Objective
HIV treatment options remain limited in children. Dolutegravir is a potent and well-tolerated, once-daily HIV-1 integrase inhibitor recommended for HIV-1 infection in both adults and children down to 4 weeks of age. To support pediatric dosing of dolutegravir in children, we used a population pharmacokinetic model with dolutegravir data from the P1093 and ODYSSEY clinical trials. The relationship between dolutegravir exposure and selected safety endpoints was also evaluated.
Methods
A population pharmacokinetic model was developed with data from P1093 and ODYSSEY to characterize the pharmacokinetics and associated variability and to evaluate the impact of pharmacokinetic covariates. The final population pharmacokinetic model simulated exposures across weight bands, doses, and formulations that were compared with established adult reference data. Exploratory exposure–safety analyses evaluated the relationship between dolutegravir pharmacokinetic parameters and selected clinical laboratory parameters and adverse events.
Results
A total of N = 239 participants were included, baseline age ranged from 0.1 to 17.5 years, weight ranged from 3.9 to 91 kg, 50% were male, and 80% were black. The final population pharmacokinetic model was a one-compartment model with first-order absorption and elimination, enabling predictions of dolutegravir concentrations in the pediatric population across weight bands and doses/formulations. The predicted geometric mean trough concentration was comparable to the adult value following a 50-mg daily dose of dolutegravir for all weight bands at recommended doses. Body weight, age, and formulation were significant predictors of dolutegravir pharmacokinetics in pediatrics. Additionally, during an exploratory exposure–safety analysis, no correlation was found between dolutegravir exposure and selected safety endpoints or adverse events.
Conclusions
The dolutegravir dosing in children ≥ 4 weeks of age on an age/weight-band basis provides comparable exposures to those historically observed in adults. Observed pharmacokinetic variability was higher in this pediatric population and no additional safety concerns were observed. These results support the weight-banded dosing of dolutegravir in pediatric participants currently recommended by the World Health Organization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Nearly half of all children living with HIV aged < 15 years do not have access to antiretroviral therapy owing in part to the limited number of optimal antiretroviral formulations available and the lack of pharmacokinetic data across age and weight groups. |
A population pharmacokinetic model using dolutegravir data from the P1093 and ODYSSEY clinical trials identified optimal doses of dolutegravir for children aged ≥ 4 weeks and weighing ≥ 3 kg using the World Health Organization weight bands. |
These results enable seamless dosing between infants and adults and reduce dissimilarities between the US Food and Drug Administration-approved and European Medicines Agency-approved weight-based dosing regimens. |
1 Introduction
Despite a decline in HIV incidence in recent years, approximately 1.7 million children less than 15 years of age were living with HIV worldwide in 2020, and only 54% were accessing antiretroviral therapy (ART) [1]. A barrier to effective treatment of children has been the limited number of antiretroviral agents available, with few optimal formulations and pharmacokinetic (PK) data across pediatric age and weight groups [2, 3].
Dolutegravir (DTG) is a once-daily (QD), integrase strand transfer inhibitor of HIV-1 integrase that has demonstrated good safety, tolerability, and efficacy in trials of treatment-naïve and experienced HIV-1-infected adults [4, 5]. In the European Union, the USA, and many other countries, DTG formulations (10-mg, 25-mg, and 50-mg film-coated tablets [FCT] and 5-mg dispersible tablets [DT]) are approved for adults and for pediatric patients weighing at least 3 kg and ≥ 4 weeks of age [6, 7]. Additionally, the World Health Organization (WHO) has recently updated their guidelines to include the use of DTG as a first-line and second-line ART in adolescents, children, and infants [3].
Two pediatric studies generated individual PK data in children with DTG FCT and DT formulations. The International Maternal Pediatric Adolescent AIDS Clinical Trials (IMPAACT) Network P1093 study, a phase I/II, multicenter, open-label, single-arm trial of HIV-1-infected children and adolescents aged 4 weeks to < 18 years who were either treatment naïve or treatment experienced [8, 9] and the ODYSSEY Study conducted by PENTA (Paediatric European Network for the Treatment of AIDS), a phase II/III, multicenter, open-label, randomized, non-inferiority, two-arm trial comparing the efficacy and safety of DTG plus two nucleoside reverse transcriptase inhibitors versus standard of care in HIV-infected children aged at least 28 days and < 18 years starting first-line ART or switching to second-line ART [10, 11]. The ODYSSEY study also included nested PK sub-studies to evaluate DTG dosing. Both the IMPAACT and PENTA networks bring together investigators, institutions, and representatives from around the globe to conduct trials focused on the treatment and prevention of HIV in children and pregnant women [12, 13].
An initial population PK (PopPK) analysis of DTG after oral administration in pediatric participants of 6 to < 18 years from P1093 led to the approval of DTG for use in pediatric patients weighing ≥ 30 kg in the USA and ≥ 14 kg in the European Union [14]. For the analysis presented here, all available data from P1093 and ODYSSEY as of the cut-off dates of 30 April, 2019 and 28 February, 2019, respectively, were combined to update this previously existing model. A population approach was used to characterize DTG pharmacokinetics and safety in pediatric patients weighing ≥ 3 kg and aged at least 4 weeks to < 18 years who were assigned to various DTG doses/formulations in treatment cohorts based on age and weight. This PopPK analysis was conducted to support pediatric dosing regimens for DTG for both FCT and DT formulations using the WHO-defined weight bands to achieve DTG exposures similar to adults. Exploratory exposure–safety analyses evaluating the relationship between DTG exposure and clinical laboratory parameters and adverse events (AEs) were also performed. These results were intended to support the regulatory approval of DTG down to 3 kg, and also to inform further on DTG fixed-dose combination approvals for pediatric populations in the future.
2 Methods
2.1 Ethics
The P1093 and ODYSSEY trials were designed in accordance with the International Council for Harmonization, Good Clinical Practice guidelines, and applicable country-specific requirements, and abided by the ethical principles of the Declaration of Helsinki. Informed consent was obtained from all participants prior to screening. The trial protocol, amendments, and informed consent forms were reviewed and approved by institutional review boards and national authorities.
2.2 Trial Design and Population
All participants in P1093 received DTG in combination with optimized background therapy that consisted of at least one fully active drug and one additional drug in addition to DTG. Trial enrollment initially occurred sequentially in age-specific cohorts starting with 12 to < 18 years of age (Cohort I, FCT), followed by 6 to < 12 years of age (Cohort IIA, FCT; Cohort IIB, granules), 2 to < 6 years of age (Cohort III, granules and DT), 6 months to < 2 years of age (Cohort IV, granules and DT), and 4 weeks to < 6 months of age (Cohort V, DT). Because of increasing international recommendations for pediatric dosing independent of age, enrollment of participants to analyze data by WHO weight bands was ultimately incorporated for the youngest participants, from 3 to < 20 kg [8, 9, 15].
The ODYSSEY study included both treatment-naïve and treatment-experienced participants, with slightly less than half starting first-line ART and slightly more than half starting second-line ART. Of those randomized to standard of care, the majority receiving first-line ART were on an efavirenz-based regimen while those randomized to standard of care receiving second-line ART were on a protease inhibitor-based regimen. A WHO-weight band approach was used from the beginning and the PK sub-studies evaluating DTG dosing for children ranged from 3 to < 40 kg [10, 11, 16, 17].
In P1093, intensive PK samples were collected (pre-dose, 1, 2, 3, 4, 6, 8, and 24 h post-dose) over a single day on study days 5–10 from a subset of at least eight participants within each WHO weight band (Fig. S1 of the Electronic Supplementary Material [ESM]). Weight-based fixed doses of QD DTG FCT, granule, or DT formulations were administered under fasting conditions. Sparse PK samples were collected from all participants at week 4 (pre-dose and 2–4 h post-dose), week 12 (any time post-dose), and week 24 (2 samples 2 h apart between 12 and 26 h post-dose); and sparse PK samples were collected from participants receiving any of the three formulations and irrespective of food intake. A subset of children from the ODYSSEY trial were enrolled in two PK sub-studies to evaluate the dosing of DTG FCT and DT across WHO weight bands. Several dose concentrations were tested, with the overall aim to reduce the number of doses and dosage form strengths (i.e., to support the use of 5-mg DT and 50-mg FCT strengths only) and to achieve exposures similar to adults. In P1093, dose adjustments were implemented for new enrollees and those under study in cases where initial PK results showed suboptimal exposure. Dolutegravir was administered QD under fasting conditions, and DTG PK samples were collected at baseline (pre-dose) and 1, 2, 3, 4, 6, and 24 h post-dose. Dolutegravir plasma concentrations were quantified using liquid chromatography with tandem mass spectrometry [18, 19]. The lower limit of quantification of DTG in plasma was 5 ng/mL for P1093 and 9.7 ng/mL for ODYSSEY. For this PopPK analysis, the PK population (239 participants) comprised all participants from whom a PK sample was obtained and analyzed for DTG and for which the time of dosing and the time of the PK sample draw relative to dosing were recorded.
The safety population included 151 participants from P1093 and 88 participants from ODYSSEY. For both studies, safety assessments included monitoring and recording of AEs, serious AEs, and laboratory parameters including hematology, fasting lipid profile, and blood chemistry. In P1093, AEs, hematology, and blood chemistry were collected at screening, day 0, days 5–10 in the intensive PK subset, or day 10 for all other participants, and at weeks 4, 8, 12, 16, 24, 32, 40, and 48. Fasting lipids were collected at screening and at weeks 24 and 48 in all participants. In ODYSSEY, AEs were collected at weeks 2, 4, 12, 24, 36, 48, 60, 72, 84, and 96. Biochemistry and hematology assessments were collected at screening, day 0, and weeks 2 (for all participants 3 to < 14 kg and optional for ≥ 14 kg), 4, 24, 48, 72, and 96 weeks. Additional assessments at weeks 12, 36, 60, and 84 were optional. Fasting lipids and glucose assessments were mandated on day 0 and at weeks 48 and 96 and optional at week 24. For both studies, AEs (clinical and laboratory) were graded using the Division of AIDS toxicity grading scale with modification for neutropenia based on differences observed for normal neutrophil counts by race [20, 21].
2.3 PK Modeling Methods
A PopPK analysis was performed using a nonlinear mixed-effect modeling approach with NONMEM software version 7.3.0 (ICON, Gaithersburg, MD, USA) and the Monte Carlo Importance Sampling Expectation Maximization method as the estimation method. R version 3.2.0 was used as a supporting application for data handling, summary statistics, exploratory diagnostics, and simulations. An interim PopPK model for DTG was initially developed using partial data from P1093 for children 6 to < 18 years of age [14]. The interim model, a one-compartment linear model with first-order absorption and elimination, was used as a starting point for development of the final model. Data from children who received granules were included in the models because studies in healthy adult volunteers have shown that the relative bioavailability of DT was comparable to granules at the same dose [22]. Covariates explored for the model included: age, body weight, serum albumin, serum alanine aminotransferase, serum creatinine, creatinine clearance, race, ethnicity, sex, emesis, hepatitis C or hepatitis B virus co-infection, Centers for Disease Control and Prevention (CDC) HIV classification for P1093 and WHO Clinical Staging of HIV for ODYSSEY, background ART, prior integrase inhibitor exposure, DTG formulation, fasted status versus without regard to food, and concomitant use of metal cation-containing products, ginkgo biloba use, and non-ART medications such as cytochrome P450 3A inhibitors and inducers, UGT1A1/1A3 inhibitors and inducers, P-glycoprotein inhibitor, and inducers as data permitted. Covariates likely to change over time, such as body weight, age, liver function tests, kidney function, or concomitant medications, were evaluated as time-varying covariates. Model performance was evaluated by goodness-of-fit plots and residual standard error of parameter estimates. The decrease in objective function value to establish statistical significance was ≥ 6.64 for a single parameter in the forward addition step and < 10.83 for a single parameter in the backward elimination step. To minimize variability due to dose differences, a prediction-corrected visual predictive check (pcVPC) was performed for the final PopPK model.
The final PopPK model was used to compute individual estimates of steady-state exposure (area under the concentration–time curve from 0 to 24 h [AUC0–24]), maximum concentration (Cmax), and trough concentration (C24) following repeat dosing of DTG included in the current PopPK analysis. The individual estimates of all model parameters were obtained from the final model by an empirical Bayes estimation. Individual estimates of PK parameters were calculated by non-compartmental methods. These estimates were obtained by simulating steady-state intensive PK concentration–time profiles (concentrations simulated at 0, 1, 2, 3, 4, 6, 8, and 24 h) following steady-state dosing using individual PK parameter values. Exposure targets for the pediatric population were predefined values comparable to respective adult exposures at 50 mg QD [15, 23,24,25]. The target for geometric mean C24 was 0.995 µg/mL with a target range of 0.697–2.260 µg/mL. The lower limit for individual C24 was 0.500 µg/mL. The target geometric mean AUC0–24 was 46 µg‧h/mL with a target range of 37–134 µg‧h/mL. The primary PK target for matching with the adult-dose exposure was C24, and AUC0–24 was secondary [15].
2.4 PK Simulation Methods
Simulations were performed to evaluate the appropriateness of DTG dosing regimens based on WHO weight bands and formulations. The concentration–time profiles were simulated by including intensive PK sampling timepoints. A total of 11 weight band/formulation/dose combinations were evaluated for DTG QD dosing: 5-mg DT (3 to < 6 kg; ≥ 1 month), 10-mg DT (6 to < 10 kg; ≥ 1 to < 6 months), 15-mg DT (6 to < 10 kg; ≥ 6 months), 20-mg DT (10 to < 14 kg), 25-mg DT (14 to < 20 kg), 40-mg FCT (14 to < 20 kg), 30-mg DT (20 to < 25 kg), 50-mg FCT (20 to < 25 kg, 25 to < 30 kg, 30 to < 35 kg, ≥ 35 kg). Two hundred participants (100 male and 100 female) were generated for each of the weight band/dose combinations for a total of 2200 participants in the QD dosing simulation. The infantile CDC chart (up to 36 months of age) was used to sample for the first three dose/weight band categories and the pediatric CDC chart (from 24 to 240 months of age) was used to sample the uniform distribution of age. The body weight of each subject was then derived according to the CDC Growth Chart. In addition to QD dosing, other simulation scenarios were explored (e.g., twice-daily [BID] dosing and alternate posology) to evaluate their impact on DTG exposure. The PK parameters AUC0–24, Cmax, and C24 were determined by using non-compartmental methods and compared against pre-defined target exposures.
2.5 Exposure–Safety Analysis
The relationship between DTG and selected safety endpoints was explored by plotting DTG observed concentrations and model-derived exposure (Cmax and AUC0–24) against selected, time-matched clinical laboratory parameters. The following safety endpoints were explored: aspartate aminotransferase, alanine aminotransferase, total bilirubin, triglycerides, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, serum creatinine, urine albumin/creatinine ratio, bicarbonate blood level, creatine kinase, neutrophils, leukocytes, and hemoglobin. To explore the relationship between DTG and AEs, a logistic regression model was fit to the data, and a maximum effect function was used on the logit scale to assess the probability of the absence or presence of selected AEs given a particular exposure to dolutegravir. The following AEs were included in the analysis: insomnia, abnormal dreams, depression, suicidality, dizziness, headache, nausea, diarrhea, abdominal pain, abdominal discomfort, flatulence, upper abdominal pain, vomiting, rash, vertigo, cough, decreased appetite, immune reconstitution inflammatory syndrome, and jaundice/icterus.
3 Results
3.1 Summary of Samples and Demographics
A total of 240 participants provided 2714 PK plasma concentrations. Of the 2714 plasma concentrations, 64 were excluded because of values below the limit of quantification (21), outlier or very low concentrations (7), sample mix-up (4), sample hemolysis (13), non-adherence to trial medication (6), or the sample being from a participant with multiple co-morbidities (13). As a result, the current population analysis included 2650 samples (1909 intensive and 741 sparse pharmacokinetics) from 239 participants (Table 1). The median (range) age was 6.00 (0.170–17.5) years with equal portions of the population being female and male, with the majority of the population being black (80%).
3.2 Dolutegravir Model Development
Initially, a PopPK model was developed using data from an analysis of DTG after oral administration in pediatric participants (n = 41) from Cohort I (12 to < 18 years), IIA (6 to < 12 years, FCT), and IIB (6 to < 12 years, granules) of P1093 participants. This interim model was a one-compartment model with first-order absorption, absorption lag time, and first-order elimination. A pcVPC of the interim model, once updated with additional data from P1093 and available data from ODYSSEY, demonstrated reasonable prediction of the observed data. The addition of absorption lag time was not supported for inclusion in the base model because of a lack of sufficient data in the absorption phase to estimate absorption lag time with good precision. For the updated model, a maturation function (Hill model) was applied to apparent clearance (CL/F) to account for the CL/F in infants. The fixed values of the maturation function were based on paracetamol because of its clearance pathways involving similar metabolic enzymes as dolutegravir [26]. Random effects included inter-individual variability (IIV) on all parameters as well as inter-occasion variability on both CL/F and the absorption rate constant (Ka). Separate residual errors were estimated for the two studies as different bioanalysis methods were used to determine concentrations of dolutegravir.
The final DTG model was a one-compartment model with first-order absorption and elimination. Significant effects were observed for age and body weight on CL/F and for body weight on apparent distribution volume (V/F). Additionally, Ka was formulation specific, and relative bioavailability was both formulation and diet specific (e.g., fasting vs without regard to food) (Table 2 and Table S1 of the ESM). The IIV and inter-occasion variability were moderate for CL/F (coefficient of variation = 29% and 34%, respectively) and large for Ka (coefficient of variation = 107% and 92%, respectively). However, the precision was reasonable for the Ka estimates. Goodness-of-fit plots (Fig. S2A of the ESM) and pcVPC (Fig. S2B of the ESM) suggested an adequate model fit with no obvious systemic bias in predictions and good prediction of observed concentrations. The effect of weight on CL/F and V/F was estimated as 0.455 (95% CI 0.418–0.492) and 0.566 (95% CI 0.514–0.598), respectively. For the range of weights in the analysis dataset (4–96 kg), CL/F ranged from 0.280 to 1.19 L/h. Apparent distribution volume also scaled linearly with weight, with a range from 2.77 to 16.2 L across the weight range. In addition to allometry, age (maturation function) was applied as a covariate on CL/F. No other covariates were identified.
3.3 Steady-State Post-hoc Parameters
Individual post-hoc estimates of PK parameters were derived from the final model by an empirical Bayes estimation method and summarized by weight band, formulation, and dose (Table S2 of the ESM). On average, DTG exposures appeared to be similar across the weight bands for the current analysis population.
3.4 Simulations
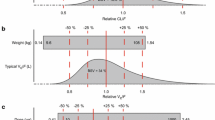
The box-and-whisker plot depicts the simulation with QD dosing of steady-state C24 for each cohort (11 weight band/dose combinations) overlaid by the observed C24 (Fig. 1). The predicted median geometric C24 ranges were fairly consistent across the different weight bands for the FCT (0.814–1.08 µg/mL) and DT (0.719–1.24 µg/mL) formulations and were comparable to the target concentration of 0.995 µg/mL. Similarly, median geometric mean AUC ranges for FCT were 54.0–78.6 µg.h/mL and for DT were 49.4–72.0 µg.h/mL across the weight bands for the recommended doses. Steady-state exposure parameters (Cmax, C24, and AUC0–24) for QD dosing are summarized by weight band and formulation in Table 3. Simulations were also performed with BID dosing and alternative posology (Table S3 of the ESM), and the results did not show a significant advantage over QD administration.
Comparison between the simulated concentration at the end of a dosing interval (C24) at the evaluated weight bands for once-daily dosing and the observed C24 on semi-log scales. Boxes represent the median (black horizontal line in the middle), first quartile, and third quartile of the data; the vertical black line through the middle of the boxes (whiskers) represents the minimum and maximum; red circles represent observed concentrations; the red solid line represents the target geometric mean C24 of 0.995 µg/mL; and the blue solid line represents the minimum target geometric mean C24 of 0.697 µg/mL. DT dispersible tablets, FCT film-coated tablets, mths months
3.5 Exploratory Exposure–Safety Analysis
Model derived AUC0–24 and Cmax values were plotted against selected safety endpoints for all data (Fig. 2 and Fig. S3 of the ESM) and the probability of the absence or presence of selected AEs for P1093 (Fig. 3). These plots suggest a lack of correlation between DTG exposure and evaluated safety endpoints and AEs.
Exploratory plots of observed dolutegravir concentrations and model-derived (A) area under the concentration–time curve from 0 to 24 h (AUC0–24) and (B) maximum concentration (Cmax) versus safety endpoints for all data (linear regression model). The blue line represents the model regression line and the gray area represents the 95% confidence interval around the model line. ALT alanine aminotransferase, AST aspartate aminotransferase, HDL high-density lipoprotein, LDL low-density lipoprotein
Exploratory plots of observed dolutegravir concentrations and model-derived (A) area under the concentration–time curve from 0 to 24 h (AUC0–24) and (B) maximum concentration (Cmax) versus select adverse events for Study P1093 (maximum effect [Emax] function on the logit scale). The red line represents the model line and the gray area represents the 95% confidence interval around the model line. GI gastrointestinal, IRIS immune reconstitution inflammatory syndrome, Prob probability
4 Discussion and Conclusions
Dolutegravir is currently recommended by the WHO for first-line and second-line treatment of children with HIV, with dosing that bridges from infants and children receiving the DT formulation up to 20 kg, and children 20 kg and above and adults primarily receiving the 50-mg FCT formulation. The data presented here contributed to these WHO guidelines and to approvals of DTG dosing by the European Medicines Agency and the US Food and Drug Administration [6, 7, 27].
The final PopPK model for DTG in pediatric participants was a one-compartment model with first-order absorption and elimination. Significant predictors of DTG pharmacokinetics in the pediatric population were body weight, age, formulation, and food intake. The final model incorporated the effect of age on CL/F and of body weight on CL/F and V/F along with formulation-specific Ka and formulation-specific and diet-specific (fasted vs without regard to food) relative bioavailability. The model was similar in structure to the adult model [28].
The PK parameter estimates for DTG in the pediatric population were comparable to estimates from the adult model, suggesting similar PK behavior of DTG between children of various ages and adults when accounting for differences in body weight. The relative bioavailability estimated by the final model was 53% higher for the DT formulation than the FCT formulation under fasted conditions (Table 2). Additionally, the bioavailability estimate for the FCT formulation was 10% higher when food status was not considered compared with fasted conditions and was lower than the bioavailability seen in adults. The difference in adult and pediatric bioavailability is likely owing to the well-defined meals used in the adult population compared with the pediatric population. Allometric exponents for CL/F and V/F were estimated to be lower than the standard 0.75 and 1.0 estimates, respectively. However, the relative ratio of the exponents was generally maintained, which may reflect the exponents addressing weight influences outside of direct hepatic capacity. As allometry alone was insufficient to predict clearance in infants compared to adults, a maturation function (Hill model) was applied to CL/F.
The pediatric dosing strategy was based on body weight to achieve exposures similar to adults receiving DTG 50 mg QD. The predicted C24 for QD dosing in pediatric participants was comparable to the target concentration of 0.995 µg/mL (Fig. 1 and Table 3). The percentage of pediatric participants below the minimum C24 DTG target concentration (0.5 µg/mL) ranged from 15 to 32% and the percentage of participants with predicted C24 lower than the tenth percentile of the adult estimate (0.323 µg/mL) ranged from 8 to 20. However, all of the participants were above the IC90 (0.064 µg/mL) and there was no evidence of a decreasing virologic response in participants with lower plasma DTG exposure. Predicted C24 values were similar to observed C24 values. The increased PK variability and shorter half-life in younger participants with decreased weights required a higher mg/kg dose resulting in higher Cmax to achieve target C24 values. Up to approximately 92% of predicted Cmax values in pediatric participants were above the 90th percentile for Cmax in adults (4.42 µg/mL). Simulations were performed for BID dosing/alternative posology (Table S3 of the ESM) to assess if a different dosing strategy would produce lower Cmax values. The modification in the dosing regimen from QD to BID resulted in decreased Cmax. However, based on adult data and the pediatric exposure–safety analysis confirming no relationship between exposure and clinical or laboratory events, together with the advantages of a QD dosing regimen, Cmax following QD dosing was deemed acceptable [6]. Maintaining a QD dosing schedule would be expected to positively affect sustained adherence and efficacy as opposed to BID dosing.
While the exposure–safety analysis found no correlation between DTG exposure and select safety endpoints (Fig. 2) or AEs (Fig. 3), the analysis was limited by the small number of participants per weight band and high variability in PK exposures and clinical laboratory data. This lack of a exposure–safety relationship observed in the pediatric participants was similar to that observed across the clinical studies in adults.
The dosing in the ≥ 6 to < 10 kg weight band is dependent on age. In P1093, participants < 6 months of age demonstrated adequate exposures (geometric mean C24 = 1.82 µg/mL) with DTG DT 10 mg QD whereas participants ≥ 6 months of age receiving DTG DT 10 mg QD showed relatively lower C24 (geometric mean C24 = 0.735 µg/mL) concentrations compared with those < 6 months of age owing to the effect of UGT1A1 enzyme maturation. However, a dose of DTG DT 15 mg QD achieved sufficient exposure (geometric mean C24 = 0.908 µg/mL) for those ≥ 6 months of age. The Cmax predicted with the 15-mg DT dose in < 6 months (8.56 µg/mL), and ≥ 6 months (6.69 µg/mL), was comparable to the Cmax observed in the pediatric participants in other weight bands as well as that historically observed in adults. Thus, based on observed data and supported by the maturation effect in the PopPK model, the Food and Drug Administration recommends a single 15-mg dose in the ≥ 6 to < 10 kg weight band without regard to age while the European Medicines Agency recommends two different doses (10 mg in < 6 months of age and 15 mg in ≥ 6 months of age).
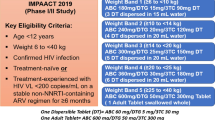
The final PopPK DTG model developed using data from P1093 and ODYSSEY reflected observed data in pediatric participants (Fig. 1 and Fig. S4 of the ESM). Using exposure matching to the efficacious adult DTG concentrations, this modeling analysis strongly supports the following daily doses for DTG DT and FCT formulations in pediatric patients aged ≥ 4 weeks and weighing ≥ 3 kg using the WHO weight bands: 5 mg DT (3 to < 6 kg; ≥ 4 weeks), 10 mg DT (6 to < 10 kg, < 6 months), 15 mg DT (6 to < 10 kg, ≥ 6months), 20 mg DT (10 to < 14 kg), 25 mg DT (14 to < 20 kg), 40 mg FCT (14 to < 20 kg), 30 mg DT (20 kg and greater), 50 mg FCT (20 kg and greater) [Table S4 of the ESM]. These results enable seamless dosing between infants and adults and reduce dissimilarities between the Food and Drug Administration-approved and European Medicines Agency-approved weight-based dosing regimens. The remains a knowledge gap for children (neonates) < 4 weeks of age but study is ongoing (IMPAACT 2023) to address this gap.
References
United Nations Programme on HIV/AIDS (UNAIDS). Global HIV & AIDS statistics: fact sheet. 2021. https://www.unaids.org/en/resources/fact-sheet. Accessed 6 Aug 2021.
World Health Organization (WHO). Paediatric Antiretroviral Drug Optimization (PADO) Meeting 4. 2018. https://www.who.int/groups/antiretroviral-drug-optimization. Accessed 6 Aug 2021.
World Health Organization (WHO). Update of recommendations on first- and second-line antiretroviral regimens. 2019. https://apps.who.int/iris/bitstream/handle/10665/325892/WHO-CDS-HIV-19.15-eng.pdf?ua=1. Accessed 6 Aug 2021.
Raffi F, Jaeger H, Quiros-Roldan E, Albrecht H, Belonosova E, Gatell JM, et al. Once-daily dolutegravir versus twice-daily raltegravir in antiretroviral-naive adults with HIV-1 infection (SPRING-2 study): 96 week results from a randomised, double-blind, non-inferiority trial. Lancet Infect Dis. 2013;13(11):927–35.
Cahn P, Madero JS, Arribas JR, Antinori A, Ortiz R, Clarke AE, et al. Durable efficacy of dolutegravir plus lamivudine in antiretroviral treatment-naive adults with HIV-1 infection: 96-week results from the GEMINI-1 and GEMINI-2 randomized clinical trials. J Acquir Immune Defic Syndr. 2020;83(3):310–8.
TIVICAY (dolutegravir) [package insert]. Research Triangle Park (NC): ViiV Healthcare; 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/204790s028,213983s002lbl.pdf. Accessed 6 Aug 2021.
TIVICAY (dolutegravir) [package leaflet]. Amersfoort, Netherlands. 2021. https://www.medicines.org.uk/emc/files/pil.12066.pdf. Accessed 6 Aug 2021.
Viani RM, Alvero C, Fenton T, Acosta EP, Hazra R, Townley E, et al. Safety, pharmacokinetics and efficacy of dolutegravir in treatment-experienced HIV-1 infected adolescents: forty-eight-week results from IMPAACT P1093. Pediatr Infect Dis J. 2015;34(11):1207–13.
Viani RM, Ruel T, Alvero C, Fenton T, Acosta EP, Hazra R, et al. Long-term safety and efficacy of dolutegravir in treatment-experienced adolescents with human immunodeficiency virus infection: results of the IMPAACT P1093 Study. J Pediatric Infect Dis Soc. 2020;9(2):159–65.
Bollen PDJ, Moore CL, Mujuru HA, Makumbi S, Kekitiinwa AR, Kaudha E, et al. Simplified dolutegravir dosing for children with HIV weighing 20 kg or more: pharmacokinetic and safety substudies of the multicentre, randomised ODYSSEY trial. Lancet HIV. 2020;7(8):e533–44.
Moore CL, Turkova A, Mujuru H, Kekitiinwa A, Lugemwa A, Kityo CM, et al. ODYSSEY clinical trial design: a randomised global study to evaluate the efficacy and safety of dolutegravir-based antiretroviral therapy in HIV-positive children, with nested pharmacokinetic sub-studies to evaluate pragmatic WHO-weight-band based dolutegravir dosing. BMC Infect Dis. 2021;21(1):5.
International Maternal Pediatric Adolescent AIDS Clinical Trials (IMPAACT). 2020. https://www.impaactnetwork.org/about. Accessed 6 Aug 2021.
Paediatric Euoropean Network for Treatment of AIDS (PENTA). Our activities: HIV. 2019. https://penta-id.org/hiv/. Accessed 6 Aug 2021.
Singh R, Edwards A, Ruel T, Wiznia A, Acosta E, Hazra R, et al. Abstract W-64 of abstracts accepted for American Conference on Pharmacometrics 2016 (ACoP7). J Pharmacokinet Pharmacodyn. 2016;43(Suppl 1):11–122.
Ruel TD, Acosta EP, Liu JP, Gray KP, George K, Montanez N, et al. Pharmacokinetics, safety, tolerability, and antiviral activity of dolutegravir dispersible tablets in infants and children with HIV-1 (IMPAACT P1093): results of an open-label, phase 1–2 trial. Lancet HIV. 2022;9(5):e332–40.
Turkova A, White E, Mujuru HA, Kekitiinwa AR, Kityo CM, Violari A, et al. Dolutegravir as first- or second-line treatment for HIV-1 infection in Children. N Engl J Med. 2021;385(27):2531–43.
Waalewijn H, Chan MK, Bollen PDJ, Mujuru HA, Makumbi S, Kekitiinwa AR, et al. Dolutegravir dosing for children with HIV weighing less than 20 kg: pharmacokinetic and safety substudies nested in the open-label, multicentre, randomised, non-inferiority ODYSSEY trial. Lancet HIV. 2022;9(5):e341–52.
Bollen PDJ, de Graaff-Teulen MJA, Schalkwijk S, van Erp NP, Burger DM. Development and validation of an UPLC-MS/MS bioanalytical method for simultaneous quantification of the antiretroviral drugs dolutegravir, elvitegravir, raltegravir, nevirapine and etravirine in human plasma. J Chromatogr B Analyt Technol Biomed Life Sci. 2019;15(1105):76–84.
Bennetto-Hood C, Tabolt G, Savina P, Acosta EP. A sensitive HPLC-MS/MS method for the determination of dolutegravir in human plasma. J Chromatogr B Analyt Technol Biomed Life Sci. 2014;15(945–6):225–32.
Bain BJ. Ethnic and sex differences in the total and differential white cell count and platelet count. J Clin Pathol. 1996;49(8):664–6.
Wells J, Shetty AK, Stranix L, Falkovitz-Halpern MS, Chipato T, Nyoni N, et al. Range of normal neutrophil counts in healthy zimbabwean infants: implications for monitoring antiretroviral drug toxicity. J Acquir Immune Defic Syndr. 2006;42(4):460–3.
Buchanan AM, Holton M, Conn I, Davies M, Choukour M, Wynne BR. Relative bioavailability of a dolutegravir dispersible tablet and the effects of low- and high-mineral-content water on the tablet in healthy adults. Clin Pharmacol Drug Dev. 2017;6(6):577–83.
Cahn P, Pozniak AL, Mingrone H, Shuldyakov A, Brites C, Andrade-Villanueva JF, et al. Dolutegravir versus raltegravir in antiretroviral-experienced, integrase-inhibitor-naive adults with HIV: week 48 results from the randomised, double-blind, non-inferiority SAILING study. Lancet. 2013;382(9893):700–8.
Raffi F, Rachlis A, Stellbrink HJ, Hardy WD, Torti C, Orkin C, et al. Once-daily dolutegravir versus raltegravir in antiretroviral-naive adults with HIV-1 infection: 48 week results from the randomised, double-blind, non-inferiority SPRING-2 study. Lancet. 2013;381(9868):735–43.
van Lunzen J, Maggiolo F, Arribas JR, Rakhmanova A, Yeni P, Young B, et al. Once daily dolutegravir (S/GSK1349572) in combination therapy in antiretroviral-naive adults with HIV: planned interim 48 week results from SPRING-1, a dose-ranging, randomised, phase 2b trial. Lancet Infect Dis. 2012;12(2):111–8.
Anderson BJ, Holford NH. Mechanistic basis of using body size and maturation to predict clearance in humans. Drug Metab Pharmacokinet. 2009;24(1):25–36.
World Health Organization (WHO) Panel on Antiretroviral Therapy and Medical Management of Children Living with HIV. Guidelines for the use of antiretroviral agents in pediatric HIV infection. 2021. https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/PediatricGuidelines.pdf. Accessed 6 Aug 2021.
Zhang J, Hayes S, Sadler BM, Minto I, Brandt J, Piscitelli S, et al. Population pharmacokinetics of dolutegravir in HIV-infected treatment-naive patients. Br J Clin Pharmacol. 2015;80(3):502–14.
Acknowledgments
The authors thank all the patients (and their caregivers) who provided data for the PopPK model and the staff at the pharmacokinetic sites and the coordinating (IMPAACT and PENTA) networks.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
The IMPAACT P1093 and ODYSSEY (PENTA 20) studies were funded by ViiV Healthcare. Diana M. Gibb, Anna Turkova, and Deborah Ford receive support from the Medical Research Council Program MC_UU_00004/03.
Conflicts of Interest/Competing Interests
Anna Turkova is an employer of MRC CTU at UCL and a paid consultant for the VH Global Paediatrics Advisory Board (Long-Acting Agents/New Delivery Methods/New Technologies) with fees paid to MRC CTU at UCL. Ann Buchanan and Mark Baker are employees of ViiV HC; Hardik Chandasana is an employee of GSK and Rajendra Singh was an employee of GSK at the time of this research; all authors are eligible for stock/stock options in GSK.
Ethics Approval
The P1093 and ODYSSEY studies were designed in accordance with the International Council for Harmonization, Good Clinical Practice guidelines, and applicable country-specific requirements and abided by the ethical principles of the Declaration of Helsinki. The trial protocol, amendments, and informed consent forms were reviewed and approved by institutional review boards and national authorities.
Consent to Participate
Informed consent was obtained from all participants prior to screening.
Consent for Publication
Not applicable.
Availability of Data and Material
Anonymized individual participant data and study documents can be requested for further research from http://www.clinicalstudydatarequest.com.
Code Availability
The final PK model code is available in ESM.
Authors’ Contributions
HC, MB, DMG, AT, DF, TR, AW, CA, RH, ET, AB, EPA, and RS contributed to the conception of the study. HC, MB, TR, AW, EPA, and RS contributed to the design of the study. DF, LF, MB-D, HM, CA, and MF contributed to the acquisition of the data. HC, MT, SH, and RS contributed to the analysis of the data. HC, MT, SH, MB, DMG, AT, DF, TR, AW, CA, MF, AB, PB, HW, AC, DB, EPA, and RS contributed to the interpretation of the data. HC, AB, and RS contributed to drafting the manuscript. All authors contributed to critically revising the manuscript for important intellectual content and approve the manuscript for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/
About this article
Cite this article
Chandasana, H., Thapar, M., Hayes, S. et al. Population Pharmacokinetic Modeling of Dolutegravir to Optimize Pediatric Dosing in HIV-1-Infected Infants, Children, and Adolescents. Clin Pharmacokinet 62, 1445–1459 (2023). https://doi.org/10.1007/s40262-023-01289-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-023-01289-5