Abstract
Background
Bimagrumab is a human monoclonal antibody binding to the activin type II receptor with therapeutic potential in conditions of muscle wasting and obesity. This phase I study evaluated the pharmacokinetics (PK), pharmacodynamics (PD), and safety of various dose regimens of bimagrumab and routes of administration in healthy older adults.
Methods
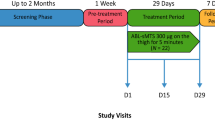
This was a randomized, double-blind, placebo-controlled, parallel-arm, multiple-dose study in older adult men and women (aged ≥ 70 years, body mass index [BMI] 18–34 kg/m2) with stable health and diet. The study comprised seven treatment groups (Cohorts 1–7). Participants received bimagrumab or placebo treatment every 4 weeks for three doses (Cohorts 1 [700 mg] and 2 [210 mg] intravenous infusion; Cohorts 3 [1500 mg] and 4 [525 mg] subcutaneous infusion), or every week for 12 doses (Cohorts 5 [300 mg], 6 [150 mg], and 7 [52.5 mg] subcutaneous bolus injection) and were followed up until week 20. Blood samples were collected for bimagrumab PK analysis. PD were assessed by dual energy X-ray absorptiometry to quantify the change from baseline in lean body mass (LBM) and fat body mass (FBM) compared with placebo. Safety was assessed throughout the study.
Results
Eighty-four of 91 (92.3%) randomized participants (mean age 74.5 years; BMI 28.0 kg/m2) completed the study. Demographic characteristics were generally balanced across the groups. A target-mediated drug disposition profile was observed following both intravenous and subcutaneous administration. The absolute subcutaneous bioavailability was estimated at approximately 40%. LBM increased by 4–6% (1.5–2 kg) from baseline throughout the treatment period for intravenous and subcutaneous regimens, except for the 52.5 mg subcutaneous dose, which did not differ from placebo. Concurrently, there was a decrease in FBM (approximately 2–3 kg) for all intravenous and subcutaneous regimens. Bimagrumab was generally safe and well tolerated; adverse events were mostly mild to moderate in severity.
Conclusions
Dose levels of bimagrumab administered weekly subcutaneously resulted in PK profiles and PD effects comparable with monthly intravenous dosing, which supports the feasibility of the subcutaneous route of administration for bimagrumab for future clinical development.




Similar content being viewed by others
References
Lee SJ, Reed LA, Davies MV, Girgenrath S, Goad ME, Tomkinson KN, et al. Regulation of muscle growth by multiple ligands signaling through activin type II receptors. Proc Natl Acad Sci USA. 2005;102(50):18117–22.
Trendelenburg AU, Meyer A, Rohner D, Boyle J, Hatakeyama S, Glass DJ. Myostatin reduces Akt/TORC1/p70S6K signaling, inhibiting myoblast differentiation and myotube size. Am J Physiol Cell Physiol. 2009;296(6):C1258–70.
Lach-Trifilieff E, Minetti GC, Sheppard K, Ibebunjo C, Feige JN, Hartmann S, et al. An antibody blocking activin type II receptors induces strong skeletal muscle hypertrophy and protects from atrophy. Mol Cell Biol. 2014;34(4):606–18.
Morvan F, Rondeau JM, Zou C, Minetti G, Scheufler C, Scharenberg M, et al. Blockade of activin type II receptors with a dual anti-ActRIIA/IIB antibody is critical to promote maximal skeletal muscle hypertrophy. Proc Natl Acad Sci USA. 2017;114(47):12448–53.
Rooks D, Praestgaard J, Hariry S, Laurent D, Petricoul O, Perry RG, et al. Treatment of sarcopenia with bimagrumab: results from a phase II, randomized, controlled, proof-of-concept study. J Am Geriatr Soc. 2017;65(9):1988–95.
Rooks D, Swan T, Goswami B, Filosa LA, Bunte O, Panchaud N, et al. Bimagrumab vs optimized standard of care for treatment of sarcopenia in community-dwelling older adults: a randomized clinical trial. JAMA Netw Open. 2020;3(10): e2020836.
Polkey MI, Praestgaard J, Berwick A, Franssen FME, Singh D, Steiner MC, et al. Activin type II receptor blockade for treatment of muscle depletion in chronic obstructive pulmonary disease. A randomized trial. Am J Respir Crit Care Med. 2019;199(3):313–20.
Amato AA, Sivakumar K, Goyal N, David WS, Salajegheh M, Praestgaard J, et al. Treatment of sporadic inclusion body myositis with bimagrumab. Neurology. 2014;83(24):2239–46.
Hanna MG, Badrising UA, Benveniste O, Lloyd TE, Needham M, Chinoy H, et al. Safety and efficacy of intravenous bimagrumab in inclusion body myositis (RESILIENT): a randomised, double-blind, placebo-controlled phase 2b trial. Lancet Neurol. 2019;18(9):834–44.
Garito T, Roubenoff R, Hompesch M, Morrow L, Gomez K, Rooks D, et al. Bimagrumab improves body composition and insulin sensitivity in insulin-resistant individuals. Diabetes Obes Metab. 2018;20(1):94–102.
Heymsfield SB, Coleman LA, Miller R, Rooks DS, Laurent D, Petricoul O, et al. Effect of bimagrumab vs placebo on body fat mass among adults with type 2 diabetes and obesity: a phase 2 randomized clinical trial. JAMA Netw Open. 2021;4(1): e2033457.
Garito T, Zakaria M, Papanicolaou DA, Li Y, Pinot P, Petricoul O, et al. Effects of bimagrumab, an activin receptor type II inhibitor, on pituitary neurohormonal axes. Clin Endocrinol (Oxf). 2018;88(6):908–19.
Rooks D, Petricoul O, Praestgaard J, Bartlett M, Laurent D, Roubenoff R. Safety and pharmacokinetics of bimagrumab in healthy older and obese adults with body composition changes in the older cohort. J Cachexia Sarcopenia Muscle. 2020;11(6):1525–34.
Rooks DS, Laurent D, Praestgaard J, Rasmussen S, Bartlett M, Tanko LB. Effect of bimagrumab on thigh muscle volume and composition in men with casting-induced atrophy. J Cachexia Sarcopenia Muscle. 2017;8(5):727–34.
Ellis J, Marks DJB, Srinivasan N, Barrett C, Hopkins TG, Richards A, et al. Depletion of LAG-3(+) T cells translated to pharmacology and improvement in psoriasis disease activity: a phase I randomized study of mAb GSK2831781. Clin Pharmacol Ther. 2021;109(5):1293–303.
Gabrielsson J, Weiner D. Non-compartmental analysis. Methods Mol Biol. 2012;929:377–89.
Gabrielsson J, Weiner D. Pharmacokinetics and pharmacodynamic data analysis: concepts and applications. Stockholm: Apotekarsocieteten; 2006.
Dubois A, Gsteiger S, Balser S, Pigeolet E, Steimer JL, Pillai G, et al. Pharmacokinetic similarity of biologics: analysis using nonlinear mixed-effects modeling. Clin Pharmacol Ther. 2012;91(2):234–42.
Mager DE, Jusko WJ. General pharmacokinetic model for drugs exhibiting target-mediated drug disposition. J Pharmacokinet Pharmacodyn. 2001;28(6):507–32.
Wang W, Wang EQ, Balthasar JP. Monoclonal antibody pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther. 2008;84(5):548–58.
Dubois A, Gsteiger S, Pigeolet E, Mentre F. Bioequivalence tests based on individual estimates using non-compartmental or model-based analyses: evaluation of estimates of sample means and type I error for different designs. Pharm Res. 2010;27(1):92–104.
Albanese CV, Diessel E, Genant HK. Clinical applications of body composition measurements using DXA. J Clin Densitom. 2003;6(2):75–85.
Gibiansky L, Gibiansky E, Kakkar T, Ma P. Approximations of the target-mediated drug disposition model and identifiability of model parameters. J Pharmacokinet Pharmacodyn. 2008;35(5):573–91.
Acknowledgements
The authors thank Hans-Joachim Wallny (Project Technical Leader) and Nicole Getzmann (Clinical Trial Leader; assisted in design and execution of the study). The authors acknowledge BioTel Research, Rochester, NY, USA, for medical imaging support. The authors also thank Hardik Ashar and Rohita Sri Gattoju for providing medical writing support, and Jitendriya Mishra for internal review support for the manuscript, employees of Novartis Healthcare in Hyderabad, India, in accordance with Good Publication Practice guidelines.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author contributions
All authors participated in the study design and implementation and/or conduct of the study. All authors read and approved the final manuscript.
Funding
This study was funded by Novartis Institutes for BioMedical Research, Basel, Switzerland
Conflict of interest
Olivier Petricoul, Arman Nazarian, Uwe Schuehly, Ursula Schramm, Olivier J. David, Didier Laurent, Jens Praestgaard, Ronenn Roubenoff, Dimitris A. Papanicolaou, and Daniel Rooks are employees of Novartis and, as such, may be eligible for Novartis stock and stock options.
Data availability
Data that support the findings of this study may be available upon reasonable request. Inquiries should be sent to info@versanisbio.com
Role of the sponsor
The study was designed by the Novartis Institutes of BioMedical Research (NIBR) and executed in collaboration with external principal investigators and their study sites. The data were analyzed by an independent contractor, and the NIBR study team was responsible for data interpretation.
Ethics approval
The study was conducted according to the ethical principles of the Declaration of Helsinki. The study protocol was reviewed by the Institutional Review Board for each center.
Consent to participate
Written informed consent was obtained from each participant before conducting any study-specific procedures.
Consent for publication
Not applicable.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Petricoul, O., Nazarian, A., Schuehly, U. et al. Pharmacokinetics and Pharmacodynamics of Bimagrumab (BYM338). Clin Pharmacokinet 62, 141–155 (2023). https://doi.org/10.1007/s40262-022-01189-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-022-01189-0