Abstract
Background and Objective
Tirzepatide, a novel, once-weekly, dual glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1 receptor agonist, is approved in the US as a treatment for type 2 diabetes and is under development for long-term weight management, heart failure with preserved ejection fraction, and nonalcoholic steatohepatitis. This study evaluated the pharmacokinetics and tolerability of tirzepatide in participants with hepatic impairment (with or without type 2 diabetes) versus healthy participants with normal hepatic function.
Methods
Participants in this parallel, single-dose, open-label study were categorized by hepatic impairment defined by the baseline Child-Pugh (CP) score A (mild impairment; n = 6), B (moderate impairment; n = 6), or C (severe impairment; n = 7) or normal hepatic function (n = 13). All participants received a single subcutaneous 5-mg dose of tirzepatide. Blood samples were collected to determine tirzepatide plasma concentrations to estimate pharmacokinetic parameters. The primary pharmacokinetic parameters of area under the drug concentration–time curve from zero to infinity (AUC0–∞) and maximum observed drug concentration (Cmax) were evaluated using an analysis of covariance. The geometric least-squares means (LSM) and mean ratios for each group, between control and hepatic impairment levels, and the corresponding 90% confidence intervals (CIs) were estimated. The analysis of the time to maximum observed drug concentration was based on a nonparametric method. The relationships between the pharmacokinetic parameters and CP classification parameters (serum albumin level, total bilirubin level, and international normalized ratio) were also assessed. Adverse events were monitored to assess safety and tolerability.
Results
Tirzepatide exposure, based on AUC0–∞ and Cmax, was similar across the control and hepatic impairment groups. Statistical analysis showed no difference in the geometric LSM AUC0–∞ or Cmax between participants in the control group and the hepatic impairment groups, with the 90% CI for the ratios of geometric LSM spanning unity (AUC0–∞ ratio of geometric LSM vs control [90% CI 1.08 [0.879, 1.32], 0.960 [0.790, 1.17], and 0.852 [0.699, 1.04] and Cmax ratio of geometric LSM vs control [90% CI]: 0.916 [0.726, 1.16], 1.00 [0.802, 1.25], and 0.972 [0.784, 1.21] for mild, moderate and severe hepatic impairment groups, respectively). There was no change in median time to Cmax of tirzepatide across all groups (time to Cmax median difference vs control [90% CI]: 0 [− 4.00, 12.00], 0 [− 12.00, 12.00], and 0 [− 11.83, 4.17], respectively). There was no significant relationship between the exposure of tirzepatide and the CP score (p > 0.1 for AUC0–∞, Cmax, and apparent total body clearance). Similarly, there was no clinically relevant relationship between the exposure of tirzepatide and serum albumin level, total bilirubin level, or international normalized ratio. The geometric LSM half-life values were also similar across the control and hepatic impairment groups. No notable differences in safety profiles were observed between participants with hepatic impairment and healthy control participants.
Conclusions
Tirzepatide pharmacokinetics was similar in participants with varying degrees of hepatic impairment compared with healthy participants. Thus, people with hepatic impairment treated with tirzepatide may not require dose adjustments.
Clinical Trial Registration
ClinicalTrials.gov identifier number NCT03940742.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Tirzepatide is a novel, once-weekly, dual glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1 receptor agonist, approved in the US as a treatment for type 2 diabetes and under development for long-term weight management, heart failure with preserved ejection fraction, and nonalcoholic steatohepatitis. |
Tirzepatide pharmacokinetics was similar in participants with varying degrees of hepatic impairment (with or without type 2 diabetes) compared with healthy participants. |
People with hepatic impairment treated with tirzepatide may not require dose adjustments. |
1 Introduction
Type 2 diabetes (T2D) and its associated complications are a major burden worldwide with increasing cases being linked to comorbidities leading to increasing mortality [1]. Hepatic impairment has a complex bi-directional relationship with diabetes [2, 3]. The liver is the prominent site of metabolism of most small-molecule anti-hyperglycemia medications, and hence hepatic impairment imposes several limitations on the use of these agents or limits the dose in this population. Historically, the management of T2D in people with hepatic impairment was complicated by the propensity of small-molecule anti-hyperglycemia medications to rely on the liver organ system for metabolism and subsequent elimination.
The advent of the incretin era in T2D treatment has now provided therapeutic options that have shown little to no dependence on the liver for elimination. Incretin-based therapies such as selective glucagon-like peptide-1 (GLP-1) are largely composed of higher molecular weight drugs with a peptide backbone. Thus, they are less dependent on the liver as the single organ for their biotransformation. Most of these drugs are simply broken down into smaller amino acid fragments following proteolytic cleavage and subsequently eliminated. Hepatic impairment studies for larger molecule peptide agents such as GLP-1 receptor agonists, dulaglutide and semaglutide have previously shown that the severity of hepatic disease status does not impact the pharmacokinetics (PK) of these drugs [4, 5]. Some other incretins, namely, albiglutide and lixisenatide [6, 7], have not been included in hepatic impairment studies because, based on known metabolism pathways, it is expected that these peptide drugs would be broken down into smaller fragments by proteolytic enzymes, and thus there was no expectation for their PK to be influenced by hepatic impairment. Exenatide is understood to be renally eliminated and therefore not considered to be influenced by hepatic impairment [8].
Tirzepatide is a novel, dual glucose-dependent insulinotropic polypeptide and GLP-1 receptor agonist that is approved in the US as a treatment for type 2 diabetes and under development for long-term weight management, heart failure with preserved ejection fraction and related comorbidities, and nonalcoholic steatohepatitis. In the phase III SURPASS clinical trials in people with T2D, tirzepatide has shown superior reductions in glycosylated hemoglobin with 23–62% of tirzepatide-treated participants achieving normoglycemia (glycosylated hemoglobin < 5.7%), accompanied by reductions in body weight that ranged from 6.6 to 13.9% [9,10,11,12,13], which is greater than what is currently noted with approved selective GLP-1 receptor agonists.
Tirzepatide consists of a 39-amino acid peptide backbone attached to a C20 fatty diacid moiety. Tirzepatide is metabolized via proteolytic cleavages of the peptide backbone, b-oxidation of the C20 fatty diacid moiety, and amide hydrolysis. Tirzepatide is not metabolized via pathways involving cytochrome P450 enzymes, sulfation, or glucuronidation enzymes. Hence, the risk of drug–drug interactions mediated via liver metabolism or transporter pathways is intrinsically low. Additionally, tirzepatide is not a substrate for renal or hepatic transporters commonly involved in drug disposition (data on file, Eli Lilly and Company). Therefore, based on a known understanding of tirzepatide metabolism pathways, hepatic impairment is not expected to directly influence tirzepatide PK.
Tirzepatide is highly bound to albumin (i.e., 99.06% bound) in humans leading to a prolonged half-life of approximately 5 days. Albumin levels in people with hepatic impairment can be lower than that observed in control participants. As the patient population for tirzepatide may include people with hepatic impairment, it is important to ascertain whether tirzepatide can be prescribed to this population without a dose adjustment. The aim of this study was to examine the PK of tirzepatide in individuals with or without T2D and varying degrees of hepatic impairment compared to healthy participants.
2 Methods and Materials
2.1 Study Design and Participants
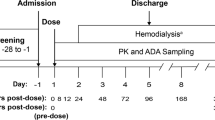
This phase I, parallel-design, open-label, multicenter, single-dose study assessed the PK and tolerability of tirzepatide in people with mild, moderate, or severe hepatic impairment and in people with normal hepatic function (control group) [Fig. 1 of the Electronic Supplementary Material (ESM)]. Study eligibility included adults aged 18–85 years, inclusive, with a body mass index ≥ 19.0 and ≤ 40.0 kg/m2 at screening. Participants were required to meet additional criteria associated with their degree of hepatic function, classified as a Child–Pugh (CP) score of A, B, or C (mild, moderate, or severe hepatic impairment, respectively). Criteria for participants with both T2D and hepatic impairment included T2D controlled with diet or exercise alone or taking stable doses of metformin for at least 8 weeks with a glycosylated hemoglobin ≥ 6.0 and ≤ 11.0% at screening. Additional criteria for the control group included healthy individuals as determined by medical history, physical examination, and other screening procedures, with clinically normal hepatic function at screening.
Plasma concentration profile of tirzepatide following a single 5-mg subcutaneous dose. A Arithmetic mean (standard deviation) and B–E individual participant profiles. h hours. AUC0–∞ area under the concentration versus time curve from time zero to infinity, CI confidence interval, CL/F apparent total body clearance of drug calculated after extra-vascular administration. Cmax maximum observed drug concentration, PK pharmacokinetics
Key exclusion criteria for all participants included organ transplantation; personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2; a significant history of or presence of cardiovascular (e.g., myocardial infarction, cerebrovascular accident, within the past 6 months), respiratory, hepatic (applies to control participants only), gastrointestinal, endocrine (except T2D), hematological, or neurological disorders capable of significantly altering the absorption, metabolism, or elimination of drugs; of constituting a risk when taking the study medication; or of interfering with the interpretation of data; and have estimated creatinine clearance < 50 mL/min (using the four-factor Modification of Diet in Renal Disease) at screening. A full list of inclusion and exclusion criteria is provided in the Appendix in the ESM.
Participants were assigned to groups of varying hepatic impairment based on the CP score on day − 1, using the criteria outlined in Table 1 of the ESM. People with T2D were not included in the control group; however, people with T2D were permitted to enroll in the hepatic impairment groups.
All study participants provided written informed consent prior to the start of any study-related activities. The study was conducted in accordance with the ethical standards of the appropriate research committee and the Declaration of Helsinki.
2.2 Tirzepatide Administration, Sample Collection, and Other Assessments
A single subcutaneous injection of tirzepatide 5 mg (Lot number: D065329) was administered. Blood samples were collected and plasma was analyzed for tirzepatide using a validated liquid chromatography/mass spectroscopy method at Q2 Solutions (Ithaca, New York, NY, USA). Tirzepatide was extracted from human plasma by immunoprecipitation and measured by high-resolution mass spectrometry with a Thermo Q-Exactive Orbitrap utilizing Heated Electrospray Ionization™ (HESI) operated in the positive ion mode; LCquan, version 2.9 was used for all data integrations. The range of quantification was from 2.00 to 500.00 ng/mL. The inter-assay accuracy (% relative error) during validation ranged from − 0.5 to 10.9%. The inter-assay precision (% relative standard deviation) during validation was ≤ 12.2%.
Plasma concentrations of tirzepatide measured pre-dose, and at 8, 12, 24, 48, 72, 96, 168, and 336 hours post-dose were used to determine the following PK parameters using standard noncompartmental methods in a validated software program (Phoenix WinNonlin Version 8.1): area under the concentration–time curve from time zero to infinity (AUC0–∞), AUC time zero to time t (AUC0–tlast), where t is the last timepoint with a measurable concentration, %AUC0–∞ that is due to extrapolation from the last measurable concentration to infinity, the maximum observed drug concentration (Cmax), the time to Cmax (tmax), the half-life associated with the terminal rate constant (λz) in noncompartmental analysis (t1/2), apparent total body clearance of drug calculated after extra-vascular administration (CL/F), apparent volume of distribution at steady state following extra-vascular administration (Vss/F), and apparent volume of distribution during the terminal phase after extra-vascular administration (Vz/F). Actual sampling times were used in the calculation of all PK parameters. Concentration versus time profiles were plotted using nominal times.
2.3 Safety Parameters
Safety parameters assessed included adverse events, hypoglycemic events, clinical laboratory parameters, including serum amylase and lipase measurements, vital signs, and injection-site reactions including edema, erythema, induration, itching, and pain. Hyperglycemia and hypoglycemia events are defined in the Appendix in the ESM.
2.4 Statistical Analyses
PK parameter estimates for tirzepatide were calculated by standard noncompartmental methods of analysis. The primary parameters analyzed were Cmax and AUC0–∞. The primary PK analysis was the evaluation of log-transformed AUC0–∞ and Cmax using an analysis of covariance model with hepatic function group as a fixed factor and body weight as a covariate. The geometric least-squares means for each group, geometric least-squares mean ratios between each hepatic impairment level versus the control group, and the corresponding 90% confidence intervals was estimated from the analysis of covariance model. The analysis of the time of maximum observed drug concentration was based on a nonparametric method. Medians and differences in medians for hepatic function groups were calculated. The relationship between the PK parameters and CP classification parameters (serum albumin level, total bilirubin level, and prothrombin time) were assessed graphically. The PK parameters AUC0–∞, Cmax, and apparent clearance were plotted against each CP classification parameter separately. Safety data were summarized using descriptive methodology.
3 Results
3.1 Baseline Characteristics and Demographics and Patient Disposition
A total of 32 participants, 24 were male and eight were female, aged 27–72 years, inclusive, participated in this study (Table 1). Of the 32 participants, three had T2D (mild hepatic impairment group). Participants were enrolled from three sites all based in the USA and were assigned to the control (normal hepatic function) or hepatic impairment group based on individual CP classification scores. All but one participant (severe hepatic impairment) completed the study. This participant was lost to follow-up and subsequently replaced. There were no discontinuations because of adverse events.
3.2 PK of Tirzepatide
Tirzepatide concentration–time profiles are shown in Fig. 1. The mean profiles did not differ over time between participants with mild-to-severe hepatic impairment and participants with normal hepatic function following a single 5-mg dose of tirzepatide (Fig. 1A). Individual participant profiles for each group are shown in Fig. 1B–E.
The overall exposure to tirzepatide, based on AUC0–tlast, AUC0–∞, and Cmax, was similar across the control and hepatic impairment groups (Table 2). The geometric least-squares mean half-life values were also similar across the control and hepatic impairment groups.
Statistical analysis showed no difference in the geometric least-squares mean Cmax or AUC0–∞ between participants in the control group and the hepatic impairment groups, with the 90% CIs for the ratios of geometric least-squares means spanning unity (Table 3). There was no change in the median tmax of tirzepatide across all groups.
3.3 Relationship Between PK Parameters of Tirzepatide and Hepatic Function at Baseline
There was no significant relationship between the exposure of tirzepatide and CP scores, with the p values of the regression line slopes being > 0.1 for each of the PK parameters (Cmax, AUC0–∞, and apparent total body clearance) (Fig. 2A–C). Similarly, there was no significant relationship between the exposure of tirzepatide and serum albumin level (Fig. 2D–F), total bilirubin level (Fig. 2G–I), or international normalized ratio (Fig. 2J–L).
Relationship between PK parameters of tirzepatide and hepatic function. AUC0–∞ area under the concentration–time curve from time zero to infinity, CI confidence interval, CL/F apparent total body clearance of drug calculated after extra-vascular administration, Cmax maximum observed drug concentration, PK pharmacokinetics
3.4 Safety Parameters
Safety parameters are presented in Table 4. No deaths occurred during this study. One serious adverse event of worsening of hepatic encephalopathy occurred in one participant in the severe hepatic impairment group. Approximately 15 hours after dosing, the participant developed nausea and vomiting that lasted for 2 days. Because of continued vomiting, the participant was sent to the hospital and subsequently admitted on day 3. On day 5, the participant recovered and was discharged on the same day. The participant returned to the study site and completed the study. Tirzepatide was considered to have resulted in the participant experiencing nausea and vomiting, which subsequently caused the participant to be unable to take her lactulose. This ultimately resulted in worsening of hepatic encephalopathy.
The incidence of all treatment-emergent adverse events reported during the study was similar across all groups and consistent with what was expected for this population and study intervention. Of the 32 participants who received tirzepatide, ten participants reported a total of 25 treatment-emergent adverse events. A majority of the reported treatment-emergent adverse events were gastrointestinal related, including nausea and vomiting.
Overall, there were no clinically meaningful findings in the clinical laboratory data, vital signs, physical examination assessments, electrocardiograms, or other observations related to safety in this study (data not shown). The assessments and observations were comparable across groups. Although data from some measurements were outside the appropriate reference ranges, these findings were generally transient and occurred at isolated timepoints. One hypoglycemic event (blood glucose level of 62 mg/dL) was reported in one participant from the control group. This participant was asymptomatic, and promptly recovered without the need for rescue therapy. There were no hypersensitivity or injection-site reactions during this study.
4 Discussion
This parallel-design open-label study evaluated the PK parameters of tirzepatide in participants with mild, moderate, or severe hepatic impairment as classified by CP status, compared to control participants with normal hepatic function, after a single subcutaneous dose of tirzepatide 5 mg. The tolerability and safety of tirzepatide in participants with varying degrees of hepatic impairment were also assessed.
The overall exposure following a single 5-mg dose of tirzepatide based on the assessment of area under the concentration–time curve and Cmax showed that exposure was similar across the control and hepatic impaired groups. Statistical analysis showed no difference in the geometric least-squares mean Cmax or AUC0–∞ between participants in the control group and the hepatic impairment groups, with the 90% CIs for the ratios of geometric least-squares means spanning unity. In concordance, there was no significant relationship between the exposure of tirzepatide and the CP score when assessed as a continuous variable. A single subcutaneous dose of tirzepatide 5 mg was well tolerated by healthy participants and participants with varying degrees of hepatic impairment (with or without T2D) in this study. Given there were no relevant effects of hepatic impairment on the PK of tirzepatide, dose adjustment may not be required in people with hepatic impairment. These outcomes are similar to the results for other incretin-based therapies, namely, dulaglutide and semaglutide, which also showed a lack of relationship between the PK of GLP-1 receptor agonists and hepatic function [14,15,16].
Tirzepatide is highly bound to albumin, thereby resulting in a half-life of ~ 5 days enabling once-weekly administration. Albumin levels in people with hepatic impairment, especially those with cirrhosis, can be lower than in healthy people with normal hepatic function. This leads to the question of whether the lower albumin level, if any, among people with hepatic impairment can impact the half-life of tirzepatide and consequently its efficacy. While it is important to acknowledge that effective albumin levels could be lower and more variable in a hepatic impaired population, it is also important to understand the relative abundance of physiological albumin concentration versus tirzepatide exposure. In our study, we did not note any relationship between serum albumin levels and tirzepatide exposure. The normal range of albumin levels in humans is approximately 3.5–5 g/dL (35–50 g/L) [17, 18]. The average steady-state tirzepatide exposures following attainment of 15-mg tirzepatide dose is expected to be approximately 1500 ng/mL (0.0015 g/L) [19]. Hence, under physiological conditions, the level of albumin is expected to be in several folds excess of maximum possible tirzepatide concentrations. Even in conditions where albumin levels can be low (e.g., hepatic impairment, nephrotic syndrome), albumin is still not expected to decrease to levels that could directly impact tirzepatide PK.
The study was conducted under the auspices of regulatory guidance for hepatic impairment studies [20, 21]. The study included a relevant number of participants in the mild, moderate, and severe impairment groups, while comparing to an appropriately baseline matched and sized control reference group.
Limitations of this study include the single-dose study design conducted in impaired participants with or without T2D. Only three participants with T2D were enrolled. Furthermore, the tirzepatide dose used in this study was 5 mg, which is the maximum tolerated dose of tirzepatide when administered as a single dose (i.e., without dose escalation). The development program of tirzepatide involved the examination of three maintenance dose levels; 5, 10, and 15 mg, which are achieved following a starting dose of 2.5 mg given for 4 weeks, followed by stepwise increments of 2.5 mg every 4 weeks to attain the final dose of 5, 10, or 15 mg. The nature of the stepwise escalation required to attain higher dose levels of 10 and 15 mg does not permit us to evaluate these doses in a single-dose hepatic impairment study.
While a single 5-mg dose pharmacokinetic study cannot provide long-term data, results from phase III studies consistently showed decreases in mean alanine transaminase and aspartate transaminase values in people with T2D treated with tirzepatide (mean percent changes from baseline ranged from − 12 to − 33% for alanine transaminase and − 1 to − 16% for aspartate transaminase) [9,10,11,12,13]. A post-hoc analysis of the phase II study showed an improvement in several non-alcoholic steatohepatitis-related biomarkers after 26 weeks of treatment with tirzepatide [22]. In a sub-study of the phase III SURPASS-3 study, participants treated with tirzepatide had a significantly greater decrease in liver fat content at 52 weeks compared with insulin degludec [23]. Among the tirzepatide-treated participants, 67‒81% achieved a ≥ 30% relative reduction in liver fat content at 52 weeks, a degree of response that has been associated with improvements in liver histology [23,24,25]. All this evidence suggests that tirzepatide may lead to improvements in liver-related clinical markers, thus providing patients with therapeutic benefit.
5 Conclusions
The absence of any effects of hepatic impairment on the PK of tirzepatide would suggest that a dose adjustment of tirzepatide, based on PK parameters, may not be required in people with hepatic impairment.
References
International Diabetes Federation. IDF diabetes atlas. 10th ed. Brussels, Belgium: 2021. Available from: https://www.diabetesatlas.org. Accessed 24 May 2022.
de Marco R, Locatelli F, Zoppini G, Verlato G, Bonora E, Muggeo M. Cause-specific mortality in type 2 diabetes. The Verona diabetes study. Diabetes Care. 1999;22(5):756v61.
Trombetta M, Spiazzi G, Zoppini G, Muggeo M. Review article: type 2 diabetes and chronic liver disease in the Verona diabetes study. Aliment Pharmacol Ther. 2005;22(Suppl. 2):24–7.
Geiser JS, Heathman MA, Xuewei C, Martin J, Loghin C, Chien JY, et al. Clinical pharmacokinetics of dulaglutide in patients with type 2 diabetes: analyses of data from clinical trials. Clin Pharmacokinet. 2016;55(5):625–34.
Jensen L, Kupcova V, Arold G, Pettersson J, Hjerpsted JB. Pharmacokinetics and tolerability of semaglutide in people with hepatic impairment. Diabetes Obes Metab. 2018;20(4):998–1005.
Tanzeum [prescribing information]. London: GlaxoSmithKline; revised August 2017. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/125431s019lbl.pdf. Accessed 8 Apr 2022.
Adlyxin [prescribing information]. Paris: Sanofi-Aventis US LLC; revised July 2016. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/208471orig1s000lbl.pdf. Accessed 8 Apr 2022.
Byetta [prescribing information]. Cambridge: AstraZeneca Pharmaceuticals, LP; revised November 2021. Available from: https://www.azpicentral.com/byetta/pi_byetta.pdf#page=1. Accessed 8 Apr 2022.
Dahl D, Onishi Y, Norwood P, Huh R, Patel H, Rodríguez A. Effect of subcutaneous tirzepatide vs placebo added to titrated insulin glargine on glycemic control in patients with type 2 diabetes: the SURPASS-5 randomized clinical trial. JAMA. 2022;327(6):534–45.
Del Prato S, Kahn SE, Pavo I, Weerakkody GJ, Yang Z, Doupis J, et al. Tirzepatide versus insulin glargine in type 2 diabetes and increased cardiovascular risk (SURPASS-4): a randomised, open-label, parallel-group, multicentre, phase 3 trial. Lancet. 2021;S0140–6736(21):02188–97.
Ludvik B, Giorgino F, Jodar E, Frias JP, Fernandez Lando L, Brown K, et al. Once-weekly tirzepatide versus once-daily insulin degludec as add-on to metformin with or without SGLT2 inhibitors in patients with type 2 diabetes (SURPASS-3): a randomised, open-label, parallel-group, phase 3 trial. Lancet. 2021;398(10300):583–98.
Rosenstock J, Wysham C, Frias JP, Kaneko S, Lee CJ, Fernández Landó L, et al. Efficacy and safety of a novel dual GIP and GLP-1 receptor agonist tirzepatide in patients with type 2 diabetes (SURPASS-1): a double-blind, randomised, phase 3 trial. Lancet. 2021;398(10295):143–55.
Frias JP, Davies MJ, Rosenstock J, Perez Manghi FC, Fernandez Lando L, Bergman BK, et al. Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. N Engl J Med. 2021;385(6):503–15.
Loghin C, De la Pena A, Cui X, Zhang X, Geiser JS, Chien JY. Pharmacokinetics of once weekly dulaglutide in special populations. Diabetologia. 2014;57(1):S358.
Marbury TC, Flint A, Jacobsen JB, Derving Karsbol J, Lasseter K. Pharmacokinetics and tolerability of a single dose of semaglutide, a human glucagon-like peptide-1 analog, in subjects with and without renal impairment. Clin Pharmacokinet. 2017;56(11):1381–90.
Granhall C, Sondergaard FL, Thomsen M, Anderson TW. Pharmacokinetics, safety and tolerability of oral semaglutide in subjects with renal impairment. Clin Pharmacokinet. 2018;57(12):1571–80.
Doweiko JP, Nompleggi DJ. The role of albumin in human physiology and pathophysiology, part III: albumin and disease states. JPEN J Parenter Enteral Nutr. 1991;15(4):476–83.
Spinella R, Sawhney R, Jalan R. Albumin in chronic liver disease: structure, functions and therapeutic implications. Hepatol Int. 2016;10(1):124–32.
Coskun T, Sloop KW, Loghin C, Alsina-Fernandez J, Urva S, Bokvist KB, et al. LY3298176, a novel dual GIP and GLP-1 receptor agonist for the treatment of type 2 diabetes mellitus: from discovery to clinical proof of concept. Mol Metab. 2018;18:3–14.
US Food and Drug Administration. Guidance for industry: pharmacokinetics in patients with impaired renal function: study design, data analysis, and impact on dosing and labeling. Draft Guidance September 2020. Available from: https://www.fda.gov/media/78573/download. Accessed 24 May 2022.
European Medicines Agency. Guideline on the evaluation of the pharmacokinetics of medicinal products in patients with decreased renal function. December 2015. Available from: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-evaluation-pharmacokinetics-medicinal-products-patients-decreased-renal-function_en.pdf. Accessed 24 May 2022.
Hartman ML, Sanyal AJ, Loomba R, Wilson JM, Nikooienejad A, Bray R, et al. Effects of novel dual gip and glp-1 receptor agonist tirzepatide on biomarkers of nonalcoholic steatohepatitis in patients with type 2 diabetes. Diabetes Care. 2020;43(6):1352–5.
Gastaldelli A, Cusi K, Fernández Landó L, Bray R, Brouwers B, Rodríguez A. Effect of tirzepatide versus insulin degludec on liver fat content and abdominal adipose tissue in patients with type 2 diabetes (SURPASS-3 MRI): a substudy of the randomised, open-label, parallel-group, phase 3 SURPASS-3 trial. Lancet Diabetes Endocrinol 2022;10(6):393–406.
Patel J, Bettencourt R, Cui J, Salotti J, Hooker J, Bhatt A, et al. Association of noninvasive quantitative decline in liver fat content on MRI with histologic response in nonalcoholic steatohepatitis. Ther Adv Gastroenterol. 2016;9(5):692–701.
Harrison SA, Bashir MR, Guy CD, Zhou R, Moylan CA, Frias JP, et al. Resmetirom (MGL-3196) for the treatment of non-alcoholic steatohepatitis: a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. 2019;394(10213):2012–24.
Acknowledgements
The authors thank Chrisanthi A. Karanikas (Eli Lilly and Company) for her writing and editorial contributions, and Laura Fernández Landó, Ángel Rodríguez, Govinda Weerakkody, Brandi Doyle, and Parag Garhyan (Eli Lilly and Company) for their insights and review contributions. The participants and the US centers where the study was performed are gratefully acknowledged: Orange County Research Center, Tustin, CA, USA, Alliance for Multispecialty Research, LLC, Knoxville, TN, USA, and Orlando Clinical Research Center, Orlando, FL, USA. Partial data were presented at the 57th Annual Meeting of the European Association Study of Diabetes, held virtually on 27 September–1 October, 2021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding for this study was provided by Eli Lilly and Company.
Conflict of interest
Shweta Urva, Tonya Quinlan, John Landry, Xiaosu Ma, Jennifer A. Martin, and Charles T. Benson are employees and shareholders of Eli Lilly and Company.
Ethics approval
The protocol was approved by local institutional review boards, and the trial was conducted in accordance with the principles of the Declaration of Helsinki and in accordance with the Good Clinical Practice guidelines of the International Council for Harmonisation.
Consent to participate
All participants gave their written informed consent to participate in this trial.
Consent for publication
Not applicable.
Availability of data and material
Eli Lilly and Company provides access to all individual participant data collected during the trial, after anonymization, with the exception of pharmacokinetic or genetic data. Data are available to request 6 months after the indication studied has been approved in the USA and European Union and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once data are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, and blank or annotated case report forms, will be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at http://www.vivli.org.
Code availability
Not applicable.
Author contributions
SU, JL, JM, and CTB contributed to the study design. CTB provided medical oversight during the trial. JL was responsible for the statistical analyses. SU and CTB are the guarantors of this work and, as such, take responsibility for the integrity of the data and the accuracy of the data analysis. All authors participated in interpretation of the data and critical review of the manuscript, had full access to all the data in the study, and approved of this manuscript to be submitted for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Urva, S., Quinlan, T., Landry, J. et al. Effects of Hepatic Impairment on the Pharmacokinetics of the Dual GIP and GLP-1 Receptor Agonist Tirzepatide. Clin Pharmacokinet 61, 1057–1067 (2022). https://doi.org/10.1007/s40262-022-01140-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-022-01140-3