Abstract
Background and Objective
Evidence on the economic value of rotavirus vaccines in middle-income countries is limited. We aimed to model the implementation of three vaccines (human rotavirus, live, attenuated, oral vaccine [HRV, 2 doses]; rotavirus vaccine, live, oral, pentavalent [HBRV, 3 doses] and rotavirus vaccine, live attenuated oral, freeze-dried [BRV-PV, 3 doses] presented in 1-dose and 2-dose vials) into the South African National Immunisation Programme.
Methods
Cost and cost-effectiveness analyses were conducted to compare three rotavirus vaccines using a static, deterministic, population model in children aged <5 years in South Africa from country payer and societal perspectives. Deterministic and probabilistic sensitivity analyses were conducted to assess the impact of uncertainty in model inputs.
Results
The human rotavirus, live, attenuated, oral vaccine (HRV) was associated with cost savings versus HBRV from both perspectives, and versus BRV-PV 1-dose vial from the societal perspective. In the cost-effectiveness analysis, HRV was estimated to avoid 1,107 home care rotavirus gastroenteritis (RVGE) events, 247 medical visits, 35 hospitalisations, and 4 RVGE-related deaths versus HBRV and BRV-PV. This translated to 73 quality-adjusted life years gained. HRV was associated with lower costs versus HBRV from both payer (−$3.9M) and societal (−$11.5M) perspectives and versus BRV-PV 1-dose vial from the societal perspective (−$3.8M), dominating those options. HRV was associated with higher costs versus BRV-PV 1-dose vial from the payer perspective and versus BRV-PV 2‑dose vial from both payer and societal perspectives (ICERs: $51,834, $121,171, and $16,717, respectively), exceeding the assumed cost-effectiveness threshold of 0.5 GDP per capita.
Conclusion
Vaccination with a 2-dose schedule of HRV may lead to better health outcomes for children in South Africa compared with the 3-dose schedule rotavirus vaccines.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
An economic analysis was conducted to compare the total costs and cost-effectiveness of three different rotavirus vaccines (HRV, HBRV and BRV-PV 1- or 2-dose vial) when implemented into the National Immunisation Programme of South Africa. |
For the government, HRV may be a cost saving option compared with HBRV and may be a cost saving option for society compared with HBRV and BRV-PV 1-dose vial. |
Vaccination with HRV, which requires two doses, may lead to better health outcomes than HBRV and BRV-PV, which both require three doses. |
1 Introduction
Rotavirus has been identified as a significant cause of diarrheal disease; it is estimated to cause 30%–50% of diarrhoeal hospitalisations in children aged under 5 years worldwide and is responsible for approximately 258 million morbidity cases and 128,000 deaths each year in this population [1, 2]. Rotavirus is spread between people via the faecal-oral route, or from the consumption of contaminated food or water [1]. Therefore, the burden of rotavirus is particularly high in countries without access to safe water, effective medical treatment, or rotavirus vaccination as part of a national immunisation programme (NIP) [1, 3].
In South Africa, rotavirus has been estimated to cause approximately 11% of deaths in children aged <5 years [2]. The human rotavirus, live, attenuated, oral vaccine (HRV; Rotarix, GSK) was introduced into the South African NIP in 2009 and has led to a 50% reduction in rotavirus-related hospitalisations in young children [4]. A second vaccine (rotavirus vaccine, live, oral, pentavalent [HBRV; RotaTeq, Merck]) is available in South Africa accessible only through private health care [2, 5, 6]. Whilst not available in South Africa, two additional vaccines: rotavirus vaccine, live attenuated oral, freeze-dried (BRV-PV; Rotasiil, Serum Institute of India) and live, attenuated, oral rotavirus 116E (ORV 116E; Rotavac, Bharat Biotech) were prequalified by the World Health Organization (WHO) in 2018 [7]. The human rotavirus, live, attenuated, oral vaccine is the only 2-dose vaccine available in South Africa; the other available vaccine, HBRV, requires 3 doses for a complete vaccination schedule [6].
There are three genetic groups of rotaviruses known to infect humans (Groups A–C), with Group A responsible for the majority of disease in children [1, 3]. Group A rotaviruses are further stratified according to differences in outer capsid glycoproteins (G) and protease sensitive proteins (P) [1]. Prior to vaccine introduction in South Africa, the most common circulating strain of rotavirus was G1P [4, 8]. The human rotavirus, live, attenuated, oral vaccine is a G1P [8] vaccine; however, it has also demonstrated efficacy against various other circulating G and P rotavirus genotypes present in South Africa and Malawi [8]. Following the introduction of HRV into the South African NIP, temporal changes in circulating rotavirus genotypes have been reported in the region [1, 4].
Overall, there is limited evidence of the cost-effectiveness of different rotavirus vaccines in middle-income countries, such as South Africa [7]. Indeed, a recent modelling study, which used data from 63 middle-income countries, highlighted the lack of up-to-date evidence evaluating the cost-effectiveness of rotavirus vaccination in countries not eligible for Gavi, the Vaccine Alliance funding [7]. Therefore, the objective of the current study was to compare the total costs and cost-effectiveness of HRV with HBRV or BRV-PV for the vaccination of children aged <5 years in South Africa.
2 Methods
2.1 Population Included in the Analysis
The population considered in the analysis was children aged under 5 years in South Africa for the calendar year 2022. For the cost analysis, the population comprised the 2022 birth cohort only as no vaccine effects were considered [9]. Based on the simulated 2022 South African birth cohort and target vaccination coverage, the number of infants estimated to be vaccinated in this analysis was 1,021,750.
2.2 Vaccines Included in the Analysis
The analysis evaluated three different vaccines: human rotavirus, live, attenuated, oral vaccine; HRV, 2-dose schedule (Rotarix; GSK, Belgium), rotavirus vaccine, live, oral, pentavalent; HBRV, 3-dose schedule (RotaTeq; Merck, USA), and rotavirus vaccine, live attenuated oral, freeze-dried; BRV-PV, 3-dose schedule, available as either 1-dose or 2-dose vials (Rotasiil; Serum Institute of India, India). Details of these vaccines are summarised in Supplementary material Table S1.
2.3 Model Structure
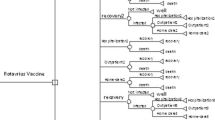
The model structure was based on a model previously developed by Bakir et al, (2013), who compared the clinical and economic impact of paediatric rotavirus vaccination in Turkey [10]. The model, developed in Microsoft Excel, was also used to assess the economic value of rotavirus vaccines in various countries [11, 12]. The construct was a static, deterministic, population model of the at-risk group (children aged <5 years). A decision tree on disease management was added comparing the costs and Quality Adjusted Life Years (QALYs) of vaccination, both in the absence of the vaccines (natural disease pathway) and in the presence of the vaccines (intervention). The total costs and clinical outcomes associated with each vaccine were estimated and assessed in a feedback loop structure, as depicted in Fig. S1 [13].
The health states of rotavirus infection have been described in previous modelling studies of rotavirus vaccines [7, 14]. Debellut et al defined the health states of rotavirus infection as: severe and non-severe rotavirus gastroenteritis (RVGE) cases, severe and non-severe RVGE clinic visits, severe RVGE hospital admissions, and RVGE deaths [7]. Similar to this approach, the current analysis defined four RVGE health states: (1) RVGE home care: RVGE cases that can be treated at home without the need for health care provider consultation, for example using oral rehydration fluids; (2) RVGE clinic visits: more severe RVGE cases that require outpatient visits; (3) RVGE hospitalisation: more severe RVGE cases that require hospital admissions; (4) RVGE death.
2.4 Cost Analysis
The cost analysis was performed from two perspectives: a country-payer perspective, which included vaccination costs and the costs associated with the vaccination supply chain, and a societal perspective, which incorporated all costs borne by the country payer as well as those incurred by attending caregivers. In South Africa, the Health Technology Assessment reference case for evaluating medicines for inclusion in The National Essential Medicines Program recommends that economic evaluations are conducted from a public health system perspective [15]. However, it is widely recognised that broader societal perspectives are also necessary to capture the full value of preventative measures such as vaccination [16, 17]. To accommodate both viewpoints, the results of this analysis were presented from both payer and societal perspectives.
The cost inputs of the cost analysis are summarised in Table S2. All costs are reported in USD ($1.00 USD=R16.356 ZAR [currency exchange rate accessed 29 May 2022]) [18].
2.4.1 Vaccination Costs
Total vaccination costs per fully immunised child (FIC) and for the 2022 birth cohort included vaccine acquisition costs (adjusted for wastage), vaccine administration costs and waste disposal costs. Rotavirus vaccine acquisition costs were obtained from the Pan American Health Organization (PAHO) Revolving Fund and are summarised in Table S1 and were adjusted for wastage using the WHO Wastage Rates Calculator (Table S3) [19]. Vaccine administration costs were calculated per minute of health care worker time, summarised in Table S4. The calculation of waste disposal costs is summarised in Fig. S2.
2.4.2 Supply Chain Costs
Supply chain costs included vaccine storage costs, the costs of international transport and handling and local storage and transport. All vaccines included in the analysis are stored in a refrigerator. International transportation and handling costs were estimated to represent a percentage of the acquisition cost per vaccine. This percentage was estimated to be 2.73% of the HRV acquisition cost based on data from the manufacturer and the same percentage was assumed for all vaccines within the analysis. Local storage and transport costs were assumed to include refrigerated storage and distribution costs, with an average transport distance of 50 km. Supply chain costs were estimated to be $13.35 per m3 per day of storage and $6.03 per m3 per km transported. Inputs used to calculate costs of refrigerated storage and transportation, and waste disposal are provided in Table S5.
2.4.3 Caregiver Costs
Caregiver costs included the costs associated with caregivers transporting children to vaccination centres and the productivity loss associated with this vaccination trip. As other vaccines may be given alongside the rotavirus vaccine, a conservative approach was taken whereby the estimated transport costs and average number of lost productivity hours were distributed over the number of vaccines given, assumed to be three vaccines. A return vaccination trip was assumed to cost $1.77 (based on local estimates; R20–R35; conversion accessed 9 June 2022) and the average number of hours of productivity loss were assumed to be 8 hours (a full working day). These two inputs were adjusted to reflect the number of concomitantly administered vaccines, resulting in a cost per return vaccination trip of $0.59 and 2.67 hours of productivity loss. The average hourly caregiver income was estimated to be $2.53, based on the adjusted net national income per capita [20].
2.5 Cost-Effectiveness Analysis
In line with the cost analysis, the cost-effectiveness analysis was conducted from the same country payer and societal perspectives. The cost-effectiveness threshold for South Africa was empirically estimated to equal 53% of the country’s gross domestic product (GDP) per capita [21]. Considering the 2020 GDP per capita for South Africa of $5,741.60 [22], the cost-effectiveness threshold was assumed to be $3,000 per QALY gained.
In addition to the total vaccination costs estimated in the cost analysis described above, the cost-effectiveness analysis also considered cost elements related to the costs of managing RVGE, as well as other direct non-medical costs and productivity losses associated with RVGE management. Clinical outcomes were estimated in terms of QALYs accrued in four RVGE health states: RVGE home care, medical visits, hospitalisation and RVGE-related death.
All relevant costs were assumed to be incurred in the same year as vaccinating the birth cohort, thus discounting was not applied to costs. Quality of life improvement due to vaccination were calculated in the same year as vaccination of the birth cohort and were therefore also not discounted. Life expectancy was used to calculate the QALY loss of early death and a discount rate of 5% was applied to health-adjusted life expectancy. Health-adjusted life expectancy in South Africa was previously reported as 58.1 years at 5 years of age (2016) [23], and an additional year of life expectancy was added to each 1-year age group descending from 5 years. All-cause mortality data were obtained from WHO life tables for South Africa in 2019 [14].
2.5.1 Cost Inputs
From the country-payer perspective, all costs included in the cost analysis described above were included in the cost-effectiveness analysis (vaccination costs, supply chain costs, and caregiver costs). In addition to this, the cost-effectiveness model considered the costs associated with the management of RVGE based on different model health states: RVGE home care, medical visits, hospitalisation. The costs associated with each of the modelled health states were based on those previously published in a modelling study reporting the rate of RVGE events in 63 middle-income countries not eligible for Gavi funding by Debellut et al, and were assumed to be $0 for RVGE home care, $18 for RVGE medical visits and $394 for RVGE hospitalisation [7]. These costs were calculated by multiplying the probability and unit costs of each health state and applying the result on the simulated cohort. Probabilities of patients being in one of the four RVGE health states were informed by those published by Debellut et al (Table S6) [7]. Rotavirus gastroenteritis health state probabilities were applied to 1-year age groups from 0 to 5 years. Data on age group distribution were obtained from a surveillance programme conducted in South Africa [24].
From the societal perspective, all costs borne under the country-payer perspective were included, as well as additional direct non-medical costs such as transport to medical appointments to manage RVGE, and productivity losses due to caregiver management of RVGE. The number of days of caregiver productivity loss was informed by previously published data and was assumed to be four days of work time lost for an RVGE case that would require home care, five days for an RVGE case that would require medical visits, and seven days for an RVGE case that would require hospitalisation (Table S7) [25,26,27].
A summary of the cost inputs included in the cost analysis and cost-effectiveness analysis are presented in Table S2.
2.5.2 Vaccine Efficacy
It was assumed that all vaccines in the cost-effectiveness analysis, when given in their complete dosing schedules, had equal efficacies for all RVGE health states.
The estimate of vaccine efficacy was sourced from a previously published double-blind, randomised, placebo-controlled multicentre study in South Africa and Malawi. This study reported that vaccine efficacy against RVGE requiring hospitalisation in the pooled vaccine cohort for the two countries was 57.5% (95 % confidence interval [CI] 7.2–80.8) [28]. Although narrative and systematic literature reviews of rotavirus vaccination efficacy have indicated greater efficacy against severe outcomes, this information was not specifically available for South Africa [29,30,31]. Therefore, a single estimate of vaccine efficacy against RVGE hospitalisation was applied to all three vaccines for the four RVGE health states considered in the analysis, and for all 1-year age groups from 0 to 5 years.
The estimated proportion of infants completing the full vaccine schedule may vary and would depend on compliance with subsequent vaccine doses. First- and second-dose rotavirus vaccine coverage in South Africa was reported to be 88% and 70%, respectively for HRV [32, 33]. As 3-dose rotavirus vaccines are not utilised in the South African NIP, the coverage rate of the third dose of the Diphtheria, Tetanus and Pertussis (DTP3) vaccine was used as a proxy for the coverage of the third dose of HBRV and BRV-PV. Diphtheria, Tetanus and Pertussis vaccine coverage was reported to be 65%; as such, if a 3-dose vaccine was to be available in South Africa, it was assumed that 93% of those who would have received the second dose would also progress to receive the third dose [32, 33]. The rate of decrease in vaccine efficacy of partial schedules was obtained from previously published economic evaluations (Table S8) [16, 17]. The analysis was conducted assuming vaccine steady state level, i.e., the vaccine uptake period was not considered and, consequently, any potential herd effect of the vaccines was not accounted for.
2.5.3 Health State Utility Values
Health state utility values, summarised in Table S7, were applied to each of the RVGE model health states based on previously published utility values in RVGE [25, 27].
2.5.4 Sensitivity Analysis
One-way deterministic sensitivity analyses (DSA) were conducted for the cost analysis and cost-effectiveness analysis to identify the model parameters with the greatest influence on the results for both the country payer and societal perspectives. All model inputs were varied by ±50% with the exception of vaccine acquisition costs and utility values (±20%, the latter capped at 1) and the cost of international transport and handling (fixed at 100% as South Africa is not eligible for Gavi support). Multivariate probabilistic sensitivity analyses (PSA) with 1,000 iterations were also conducted for the cost-effectiveness analysis to test the robustness of the base-case results.
2.5.5 Scenario Analysis
A scenario analysis was conducted to test the assumption that caregiver attendance costs would not be affected by the number of vaccines concomitantly administered with the rotavirus vaccine.
3 Results
3.1 Number of Required Doses
The number of required vaccine doses, based on the number of doses in the vaccine schedule and the wastage rate, was estimated to be lower for HRV (2,128,647 doses) compared with HBRV (3,192,970 doses) and BRV-PV (3,192,970 doses for the 1-dose vial and 4,943,954 doses for the 2-dose vial).
3.2 Cost Analysis
3.2.1 Base-case Results
From the country payer perspective, the total costs associated with the implementation of rotavirus vaccination in children aged under 5 in South Africa was $15,112,143 for HRV, $18,986,117 for HBRV, $11,314,117 for BRV-PV 1-dose vial and $6,258,203 for BRV-PV 2-dose vial. From the societal perspective, the total costs associated with rotavirus vaccination increased to $30,104,627 for HRV, $41,474,843 for HBRV, $33,802,844 for BRV-PV 1-dose and $28,746,930 for BRV-PV 2-dose. HRV was associated with substantial cost savings versus HBRV from both perspectives, and versus BRV-PV 1-dose vial from the societal perspective. The total vaccination costs associated with BRV-PV 2-dose vial were lower than those for HRV from both perspectives (Table 1).
3.2.2 Sensitivity Analysis of the Cost Comparison Results
The DSA for the comparison of HRV and HBRV from the country-payer perspective showed the biggest driver of costs to be HBRV vaccine acquisition cost per dose, followed by HRV vaccine acquisition cost per dose (Fig. S3A). In the comparison of HRV and BRV-PV 1-dose vial, the biggest driver of costs was shown to be HRV vaccine acquisition cost per dose, followed by BRV-PV 1-dose vial vaccine acquisition cost per dose (Fig. S3B). In the comparison of HRV and BRV-PV 2-dose vial, the biggest driver was HRV vaccine acquisition cost per dose followed by the assumed wastage percentage for BRV-PV 2-dose vial (Fig. S3C). From the societal perspective, the average hours of productivity loss per vaccine dose administered, followed by the average income per hour worked, were shown to be the biggest drivers in the DSA for all comparisons (Fig. S4A, S4B and S4C).
3.3 Cost-Effectiveness Analysis
3.3.1 Health Outcomes
The estimated number of RVGE events across the four RVGE health states and associated QALY gains for the simulated 2022 South African birth cohort are summarised in Table S9. Overall, vaccination with HRV led to better health outcomes compared with HBRV and BRV-PV (1- and 2-dose vials). HRV was projected to avoid 1,107 home care RVGE events, 247 medical visits, 35 hospitalisations, and 4 RVGE-related deaths when compared with HBRV and BRV-PV (1- and 2-dose vials) (all 3-dose vaccines). These reductions in RVGE events translated to an overall difference of 73 discounted QALYs gained (219 undiscounted) with HRV compared with the 3-dose vaccines (HBRV and BRV-PV 1-dose vial and 2-dose vial) for the total simulated cohort over the model duration.
3.3.2 Costs
Vaccination with HRV was associated with lower direct medical treatment costs compared with the 3-dose vaccines (HBRV and BRV-PV 1- and 2-dose vials) (Table S10). This difference was driven by lower costs needed to manage RVGE cases that required either home care, medical visits, or hospitalisation. Similarly, HRV was associated with lower caregiver attendance costs, caregiver productivity losses to manage RVGE cases, and direct non-medical costs across all comparisons. HRV was estimated to result in lower total costs compared with HBRV from both the country-payer (−$3,892,391) and societal (−$11,508,975) perspectives. The reduced cost with HRV compared with HBRV was mainly driven by lower total vaccination costs, supply chain costs, and caregiver attendance costs. Similarly, from the societal perspective, HRV was associated with lower total costs compared with BRV-PV 1-dose vial from the societal perspective (−$3,836,975), mainly driven by the lower caregiver attendance costs and caregiver productivity losses to manage RVGE. Conversely, HRV resulted in higher costs compared with BRV-PV 1-dose vial from the country-payer perspective and from both perspectives when compared with BRV-PV 2-dose vial, driven by higher total vaccination costs and supply chain costs with HRV (Table S10).
3.3.3 Incremental Cost-Effectiveness Ratio (ICER)
3.3.3.1 Base-Case Results
From the country-payer perspective, HRV dominated HBRV, i.e., vaccination with HRV was associated with higher QALY gains at a lower cost versus HBRV. Although HRV vaccination led to fewer projected RVGE events, the total costs associated with BRV-PV 1- and 2-dose vials were lower than HRV. This resulted in ICERs for HRV versus BRV-PV 1- and 2-dose of $51,834 and $121,171 per QALY gained, respectively, lying above the assumed $3,000 per QALY gained cost-effectiveness threshold (Table 2).
From the societal perspective, HRV dominated both HBRV and BRV-PV 1-dose vial. However, BRV-PV 2-dose vial was associated with lower total costs compared with HRV, resulting in an ICER for HRV versus BRV-PV 2-dose vial of $16,717 per QALY gained.
3.3.3.2 Sensitivity Analysis Results
In the DSA, HRV remained dominant versus HBRV from both the country-payer and societal perspectives, even when the low input value of HBRV price per dose was used (Fig. S5A, S6A). In the comparisons of HRV versus BRV-PV 1- and 2-dose vials, the biggest driver of the cost-effectiveness results was HRV vaccine acquisition cost from the country-payer perspective (Fig. S5B, S5C) and average income per worker hour from the societal perspective (Fig. S6B, S6C). The ICERs for HRV remained above the $3,000 per QALY gained cost-effectiveness threshold from the country-payer perspective (Fig. S5B, S5C).
From the societal perspective, HRV dominated BRV-PV 1-dose vial across all scenarios (Fig. S6B). Compared with BRV-PV 2-dose vial, HRV was demonstrated to be a cost saving option when using the higher input value of the following parameters: health care worker average hourly income, average hours of caregiver productivity loss per vaccine dose administration and BRV-PV 2-dose vial waste percentage, and when using the lower input value of HRV purchase price per dose (Fig. S6C).
In the PSA with 1,000 iterations (Figs. 1 and 2), HRV had a very high probability, close to 100 %, of being a cost-effective option compared to HBRV from both perspectives at the $3,000 threshold, with the majority of iterations in the lower right quadrant of the cost-effectiveness plane. From a societal perspective, HRV demonstrated probabilities of around 90 % (Fig. 2C) and 40 % (Fig. 2D) of being a cost-effective option compared to BRV-PV 1- and 2-dose vials, respectively, at the $3,000 threshold.
Cost-effectiveness analysis probabilistic sensitivity analysis (country payer perspective). A Cost-effectiveness plane: HBRV and BRV-PV 1-dose vial as reference compared with HRV; B Cost-effectiveness plane: HBRV and BRV-PV 2-dose vial as reference compared with HRV; C Cost-effectiveness acceptability curve at $3,000 per QALY threshold: HRV vs HBRV and BRV-PV 1-dose vial; D Cost-effectiveness acceptability curve at $3,000 per QALY threshold: HRV vs HBRV and BRV-PV 2-dose vial. BRV-PV rotavirus vaccine, live attenuated oral, freeze-dried, HBRV rotavirus vaccine, live, oral, pentavalent, HRV human rotavirus, live, attenuated, oral vaccine, QALY quality-adjusted life year
Cost-effectiveness analysis probabilistic sensitivity analysis (societal perspective). A Cost-effectiveness plane: HBRV and BRV-PV 1-dose vial as reference compared with HRV; B Cost-effectiveness plane: HBRV and BRV-PV 2-dose vial as reference compared with HRV; C Cost-effectiveness acceptability curve at $3,000 per QALY threshold: HRV versus HBRV and BRV-PV 1-dose vial; D Cost-effectiveness acceptability curve at $3,000 per QALY threshold: HRV versus HBRV and BRV-PV 2-dose vial. BRV-PV rotavirus vaccine, live attenuated oral, freeze-dried, HBRV rotavirus vaccine, live, oral, pentavalent, HRV human rotavirus, live, attenuated, oral vaccine, QALY quality-adjusted life year
3.3.3.3 Scenario Analysis Results
Results of the scenario analysis, whereby it was assumed that caregiver attendance costs would not be affected by the number of vaccines concomitantly administered with the rotavirus vaccine, showed that HRV remained cost saving versus HBRV from the country-payer perspective. HRV was also cost saving versus all 3-dose vaccine options from the societal perspective (Tables S11 and S12).
4 Discussion
The introduction of rotavirus vaccination in 2009 has had a positive impact on public health in South Africa and is estimated to have prevented 13,000 to 20,000 RVGE hospitalisations in the two years following implementation into the NIP [2]. A recent modelling study reported that rotavirus vaccination was a cost-effective choice versus no vaccination in middle-income countries, such as South Africa [7]. The study reported a 100% probability for the costs per disability-adjusted life year (DALY) averted to be below 0.5 GDP per capita for HRV and BRV-PV from a government perspective in South Africa [7]. Additionally, the study estimated that age-restricted rotavirus vaccination schedules would avert 68,535 rotavirus hospitalisations in South Africa between 2020 and 2029 [7]. Furthermore, in a published systematic review and meta-analysis of rotavirus cost-effectiveness studies, rotavirus vaccines were shown to be a cost-effective strategy compared with no vaccination, when implemented in low- and middle-income countries [34].
Given the lower acquisition costs of vaccines recently prequalified by the WHO, it is important to assess their impact and value in comparison to earlier available vaccines in South Africa. The current cost analysis and cost-effectiveness analysis demonstrated that the expected costs of vaccinating the eligible infant population in South Africa were lower with HRV compared with HBRV from both the country-payer and societal perspectives. This was driven by lower vaccination costs, supply chain costs, and caregiver attendance costs compared with HBRV. However, BRV-PV was associated with lower total vaccination costs than HRV, driven by lower vaccination acquisition costs and supply chain costs. When caregiver costs of vaccination were considered, the lower costs associated with BRV-PV were fully offset for BRV-PV 1-dose vial and partly offset for BRV-PV 2-dose vial. This resulted in an overall lower cost with HRV from the societal perspective when compared with BRV-PV 1-dose vial. In the cost-effectiveness analysis, HRV dominated HBRV from the country-payer perspective. From the societal perspective, HRV dominated both HBRV and BRV-PV 1-dose vial. While HRV was not cost saving when compared with BRV-PV 2-dose vial from both perspectives in the base-case results, there were scenarios of the sensitivity analysis where HRV was demonstrated to be a cost saving option from the societal perspective, as shown in Figure S6C.
In the PSA, HRV had a very high probability (close to 100%), of being a cost-effective option compared to HBRV from both the country-payer and societal perspectives. However, due to the ICERs being significantly higher than the $3,000 threshold, HRV had a very low probability (close to 0%) of being cost-effective compared with BRV-PV 1-dose vial and BRV-PV 2-dose vial from the country-payer perspective (Fig. 1C, D). Conversely, from the societal perspective, HRV demonstrated probabilities of approximately 90% and 40% of being a cost-effective option compared to BRV-PV 1- and 2-dose vials, respectively, at the $3,000 threshold (Fig. 2C, D).
Conventional health economic analyses evaluate the clinical value and benefit of interventions at the individual patient level, using outcomes such as QALYs [35]. However, vaccination has a broad societal impact beyond the individual level that cannot be adequately captured by these evaluations [35, 36]. Therefore, the societal benefits of vaccination may be undervalued in these analyses. There is growing support for increasing the emphasis of the societal perspective in health economic evaluations of vaccines, as this perspective more truly reflects the population-level benefits that vaccines can provide [35, 36]. For example, vaccination can prevent disease events that may directly cause absenteeism or cause productivity losses of non-professional caregivers, such as the family of children with a disease [35]. Additionally, vaccinations with high coverage can improve overall disease control leading to large scale societal shifts, such as the reallocation of resources to other disease areas to improve the quality care for other social priorities [35, 36].
While evidence on the efficacy of BRV-PV and ORV 116E in low and medium mortality settings is lacking, a Cochrane systematic literature review and meta-analysis using data from high mortality settings, such as that of South Africa, estimated the efficacy of HRV against severe RVGE at two years follow-up to be 54% (95% CI 9%–77%), compared with 44% (95% CI 23%–59%) for HBRV and 44% (95% CI 26%–58%) for BRV-PV [37, 38]. The vaccine efficacy estimate used in the current analysis (57.5% [95% CI 7.2%–80.8%]) was the efficacy of HRV pooled 2- and 3-dose vaccines against RVGE hospitalisation [28]. Notably, the pooled 2-dose and 3-dose vaccine efficacy against severe RVGE was reported to be higher than the efficacy against hospitalisation, at 76.9% [28]. However, the lower vaccine efficacy estimate of 57.5% used in this analysis was consistent with a Cochrane systematic literature review and meta-analysis of the safety and effectiveness of rotavirus childhood vaccination schedules, reporting results of vaccine efficacy in high mortality countries [37]. On top of this, in a separate case-control study conducted in the setting of Africa, the effectiveness of the 2-dose rotavirus vaccine under conditions of routine use in South Africa was estimated to be 57% [39]. Therefore, the conservative efficacy estimate of 57.5%, which was consistent with other empirical and non-empirical literature in the field, was chosen as the input for the current model.
Although vaccine efficacy was assumed to be equal between completed vaccine schedules in this analysis, it can be expected that incomplete vaccination schedules will result in lower vaccine efficacy. Hence, efficacy decrements were applied to account for missed subsequent doses resulting in incomplete vaccination dosing schedules. A 2-dose vaccine is likely to provide earlier protection than a 3-dose vaccine and have higher vaccine coverage due to the shorter vaccine schedule. In the current analysis, the impact of early protection against rotavirus was demonstrated by the better health outcomes of HRV (fewer RVGE events and higher QALY gains) compared with the 3-dose vaccines (HBRV and BRV-PV 1- and 2-dose vials).
There are currently a limited number of economic evaluations investigating the economic impact of the rotavirus vaccines recently prequalified by the WHO, compared with previously available vaccines [7]. The model used in this analysis was designed to be adaptable to different settings and to therefore allow for the development of tailored economic analyses of rotavirus vaccination for specific countries [10]. This model can also include costs that may not be typically considered in other analyses. For example, this particular analysis was tailored to the setting of South Africa and was adapted to include specific costs of waste disposal, international and local transportation and caregiver attendance costs. While some inputs could not be sourced for this particular adaptation, such as overhead costs, non-medical costs (including the cost of diapers and meals during hospitalisation) and costs of vaccine adverse events, the model allows for these costs to be considered in future evaluations in the same or different settings. Furthermore, either QALYs or DALYs can be used as a measure of health in this model. In a previous case study, which investigated the influence of different health metrics on the conclusions drawn in health economic evaluations of rotavirus vaccination in Burundi, the use of DALYs led to more favourable cost-effective results than the use of QALYs. However, such effects were small and less likely to affect the analysis conclusion [40].
The cost estimates used in this analysis are considered to be comprehensive as both total vaccination costs and other cost outcomes that would have an impact on the government payer and the caregiver alike were considered. Uncertainty around the estimated caregiver attendance costs associated with different rotavirus vaccines may have impacted the results of this analysis, particularly from the societal perspective. This model input drives a significant difference between the costs associated with vaccines included in the analysis due to the fewer trips to vaccination centres required for HRV compared with 3-dose vaccines. This was partially addressed by using a conservative estimate in the base-case analysis, in which caregiver attendance costs were distributed between a number of concomitantly administered vaccines. However, there may be cases where one or more of the vaccines that should be given together in the same setting are not available for logistical or supply reasons, hence the caregivers will have to return to attend appointments for the missing vaccine(s). To address this uncertainty, a scenario analysis was conducted to test the impact of not distributing the caregiver attendance cost between the concomitantly administered vaccine. In this scenario analysis, HRV was dominant compared with all other vaccines from the societal perspective. While this less conservative scenario cannot be generalised to be the default, it would significantly impact the caregiver attendance costs and was deemed appropriate to explore. A final potential limitation of this analysis was the uncertainty of some model inputs, such as waste disposal costs; however, the DSA showed that these costs were not a large driver of the base-case results in any of the comparisons.
5 Conclusions
Overall, HRV (a 2-dose vaccine) led to better health outcomes, reflected by fewer RVGE events and more QALY gains, than HBRV and BRV-PV 1- and 2-dose vials, and the 3-dose vaccines. This was, in part, driven by the earlier protection provided by the 2-dose vaccination schedule compared with other 3-dose vaccines. This analysis demonstrated that HRV is estimated to be a cost saving option compared with HBRV from the country-payer perspective and compared with HBRV and BRV-PV 1-dose from a social perspective. This analysis provides important and up-to-date information to health care decision makers regarding the implementation of rotavirus vaccination programmes in South Africa.
References
Omatola CA, Ogunsakin RE, Olaniran AO. Prevalence, pattern and genetic diversity of rotaviruses among children under 5 years of age with acute gastroenteritis in South Africa: a systematic review and meta-analysis. Viruses. 2021;13(10):1905.
Msimang VMY, Page N, Groome MJ, et al. Impact of rotavirus vaccine on childhood diarrheal hospitalization after introduction into the South African public immunization program. Pediatric Infect Dis J. 2013;32(12):1359–64.
Crawford SE, Ramani S, Tate JE, et al. Rotavirus infection. Nat Rev Dis Primers. 2017;3:17083.
Page NA, Seheri LM, Groome MJ, et al. Temporal association of rotavirus vaccination and genotype circulation in South Africa: observations from 2002 to 2014. Vaccine. 2018;36(47):7231–7.
Amayeza. Vaccine information, schedules and records 2022 [Available from: https://www.amayeza-info.co.za/vaccine-info/; Accessed: 05 May 2023
Paediatrician Management Group NPC. Vaccinaiton Schedule 2021 [Available from: https://paeds.co.za/position-statements; Accessed: 05 May 2023
Debellut F, Clark A, Pecenka C, et al. Evaluating the potential economic and health impact of rotavirus vaccination in 63 middle-income countries not eligible for Gavi funding: a modelling study. Lancet Glob Health. 2021;9(7):e942–56.
Steele AD, Neuzil KM, Cunliffe NA, et al. Human rotavirus vaccine Rotarix™ provides protection against diverse circulating rotavirus strains in African infants: a randomized controlled trial. BMC Infect Dis. 2012;12:213.
United Nations. File INT/3-1: Total population (both sexes combined) by single age, region, subregion and country, annually for 1950–2100. Medium fertility variant, 2020–2100. POP/DB/WPP/Rev.2019/INT/F03-1.: United Nations, Department of Economics and Social Affairs, Population Division (2022). 2022. Available from: https://population.un.org/wpp/Download/Standard/Population/. Accessed: 19 June 2022
Bakir M, Standaert B, Turel O, Bilge ZE, Postma M. Estimating and comparing the clinical and economic impact of paediatric rotavirus vaccination in Turkey using a simple versus an advanced model. Vaccine. 2013;31(6):979–86.
Alkoshi S, Maimaiti N, Dahlui M. Cost-effectiveness analysis of rotavirus vaccination among Libyan children using a simple economic model. Libyan J Med. 2014;9(1):26236.
Saokaew S, Prasitsuebsai W, Bibera GL, et al. Economic evaluation of human rotavirus vaccine in Thailand. Infect Dis Ther. 2019;8(3):397–415.
Gomez J, Castillo FRV, Guzman-Holst A, et al. Cost-effectiveness analysis measuring the total costs against the health benefits of three different rotavirus vaccines for Mexico. Human Vaccines Immunotherapeutics. 2023. https://doi.org/10.1080/21645515.2023.2219189.
World Health Organisation. Life tables: Life tables by country South Africa [Available from: https://apps.who.int/gho/data/view.searo.61540?lang=en; Accessed: 05 May 2023
National Department of Health. Health technology assessment methods guide to inform the selection of medicines to the South African national essential medicines list 2021 [Available from: https://health.gov.za/wp-content/uploads/2021/07/DRAFT_HTA-Methods-Guide_v1.2_14Jun21-1.pdf; Accessed: 24 August 2023
Tilson L, Jit M, Schmitz S, et al. Cost-effectiveness of universal rotavirus vaccination in reducing rotavirus gastroenteritis in Ireland. Vaccine. 2011;29(43):7463–73.
Jit M, Mangen MJ, Melliez H, et al. An update to “The cost-effectiveness of rotavirus vaccination: comparative analyses for five European countries and transferability in Europe.” Vaccine. 2010;28(47):7457–9.
Organisation for Economic Co-operation and Development. Exchange rates. Available from: https://data.oecd.org/conversion/exchange-rates.htm#indicator-chart; Accessed: 29 May 2022
World Health Organization. Vaccine Wastage Rates Calculator. Available from: https://www.who.int/publications/m/item/vaccine-wastage-rates-calculator; Accessed: 05 May 2023
The World Bank. Adjusted net national income per capita (current US$) [29 May 2022]. Available from: https://data.worldbank.org/indicator/NY.ADJ.NNTY.PC.CD; Accessed: 05 May 2023
Edoka IP, Stacey NK. Estimating a cost-effectiveness threshold for health care decision-making in South Africa. Health Policy Plan. 2020;35(5):546–55.
The World Bank. GDP per capita (current US$) - South Africa 2022. Available from: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=ZA. Accessed: 16 June 2022
Bredenkamp C, Burger R, Jourdan A, Van Doorslaer E. Changing inequalities in health-adjusted life expectancy by income and race in South Africa. Health Syst Reform. 2021;7(2): e1909303.
National Institute for Communicable Diseases. National Institute for Communicable Diseases Annual Overview 2019/2020 2020. Available from: https://www.nicd.ac.za/archives/; Accessed: 05 May 2023
Standaert B, Parez N, Tehard B, Colin X, Detournay B. Cost-effectiveness analysis of vaccination against rotavirus with RIX4414 in France. Appl Health Econ Health Policy. 2008;6(4):199–216.
Szende A, Janssen BMF, Cabasés JM. Self-Reported Population Health: an international perspective based on EQ-5D. Value Health. 2013;16:A464.
Martin A, Cottrell S, Standaert B. Estimating utility scores in young children with acute rotavirus gastroenteritis in the UK. J Med Econ. 2008;11(3):471–84.
Madhi SA, Cunliffe NA, Steele D, et al. Effect of human rotavirus vaccine on severe diarrhea in African infants. N Engl J Med. 2010;362(4):289–98.
Burnett E, Parashar U, Tate J. Rotavirus vaccines: effectiveness, safety, and future directions. Paediatr Drugs. 2018;20(3):223–33.
Vesikari T. Rotavirus vaccination: a concise review. Clin Microbiol Infect. 2012;18:57–63.
Soares‐Weiser K, MacLehose H, Bergman H, et al. Vaccines for preventing rotavirus diarrhoea: vaccines in use. Cochrane Database Syst Rev. 2012;(2).
Makamba-Mutevedzi P, S. M, R. B. Republic of South Africa Expanded Programme On Immunisation (EPI) National Coveraeg Survery Report 2020. In: Health Do, editor. National Expanded Program on Immunization Pretoria South Africa 2020
Department of Health. South Africa Demographic and Health Survey 2016. In: Health Do, editor. 2016
Haider S, Chaikledkaew U, Thavorncharoensap M, Youngkong S, Islam MA, Thakkinstian A. Systematic review and meta-analysis of cost-effectiveness of rotavirus vaccine in low-income and lower-middle-income countries. Open Forum Infect Dis. 2019;6(4): ofz117.
Standaert B, Rappuoli R. Towards a more comprehensive approach for a total economic assessment of vaccines? J Market Access Health Policy. 2017;5(1):1335162.
Standaert B, Rappuoli R. 2. How is the economic assessment of vaccines performed today? J Mark Access Health Policy. 2017;5(1):1335163.
World Health Organization. Update of a systematic review and meta-analysis of the safety, effectiveness and efficacy of childhood schedules using Rotavirus vaccines 2017 [Available from: https://www.who.int/publications/m/item/review-meta-analysis-rotavirus-vaccines; Accessed: 05 May 2023
World Health Organization. Summary of Key Characteristics of WHO Prequalified Rotavirus Vaccines 2021 [Available from: https://www.who.int/publications/i/item/WHO-IVB-2021.03; Accessed: 05 May 2023
Groome MJ, Page N, Cortese MM, et al. Effectiveness of monovalent human rotavirus vaccine against admission to hospital for acute rotavirus diarrhoea in South African children: a case-control study. Lancet Infect Dis. 2014;14(11):1096–104.
Niyibitegeka F, Thavorncharoensap M, Riewpaiboon A, Youngkong S. Does the choice of health metric, DALY or QALY, influence conclusions of health economic evaluation? A case study of rotavirus vaccine in Burundi. Appl Health Econ Health Policy. 2022;20(5):707–16.
Acknowledgements
The authors acknowledge Ben Namale, Warehousing and Logistics Lead at GSK, for providing insights on the costs of vaccine transportation and storage in South Africa, Baudouin Standaert for providing scientific expertise and advice as well as creating the model used in this study with Laure-Anne Van Bellinghen and Ilse Van Vlaaenderen at CHESS in Health, and Bella Dragova for publication management. The authors also thank Costello Medical for editorial assistance and publication coordination, on behalf of GSK, and acknowledge Megan Thomas, Costello Medical, UK for medical writing and editorial assistance based on authors’ input and direction.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was sponsored by GlaxoSmithKline Biologicals SA (Study identifier VEO-000364). Support for third-party writing assistance for this article, provided by Megan Thomas, Costello Medical, UK was funded by GSK in accordance with Good Publication Practice (GPP 2022) guidelines (https://www.ismpp.org/gpp-2022).
Authors’ Contributions
Substantial contributions to study conception and design: AM, NP, WB, JAG; substantial contributions to analysis and interpretation of the data: AM, NP, WB, JAG; drafting the article or revising it critically for important intellectual content: AM, NP, WB, JAG; final approval of the version of the article to be published: AM, NP, WB, JAG.
Conflict of Interest
AM and JAG are employed by and hold shares in the GSK group of companies; NP has received contractual fees by GSK, has received grants or contracts from the German Federal Ministry of Education and Research (BMBF) and the PATH Center for Vaccine Innovation and Access, has received support from the Defence Threat Reduction Agency for attending meetings for the Annual Biological Safety Conference, Milwaukee and has participated on the GSK Rotavirus Advisory Board; WB is employed by and owns shares in the GSK group of companies.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Data Sharing Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Mohy, A., Page, N., Boyce, W. et al. Economic Evaluation of Rotavirus Vaccination in Children Aged Under Five Years in South Africa. Clin Drug Investig 43, 851–863 (2023). https://doi.org/10.1007/s40261-023-01312-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-023-01312-4