Abstract
Background
Indacaterol acetate (IND), a long-acting β2-agonist in combination with mometasone furoate (MF), an inhaled corticosteroid (ICS), is being explored as a once-daily (od) treatment for asthma in children. This study examined the efficacy, safety, and systemic exposure of IND 75 µg and IND 150 µg in children with persistent asthma.
Methods
In this Phase IIb, multicenter, randomized, double-blind, parallel-group study, pediatric patients (aged ≥ 6 to < 12 years) with persistent asthma were randomized (1:1) to receive either IND 75 µg od or IND 150 µg od via Breezhaler® in combination with ICS background therapy. The primary endpoint was change from baseline in pre-dose trough forced expiratory volume in one second (FEV1) after two weeks of treatment.
Results
In total, 80 patients received IND 75 µg (n = 39) or IND 150 µg (n = 41). The study met its primary endpoint; both doses demonstrated improvements in pre-dose trough FEV1 from baseline to Day 14 (mean change [Δ]: 212 mL, IND 75 µg; 171 mL, IND 150 µg). The secondary spirometry parameters (post-dose FEV1 after 1-h, post-dose forced vital capacity; morning and evening peak expiratory flow) also improved. Overall, 36.1% in IND 75 μg group and 25% patients in IND 150 μg group achieved a decrease from baseline in Pediatric Interviewer-administered Asthma Control Questionnaire score of ≥ 0.5 units. A dose-dependent increase in plasma IND concentration was noted between the two groups. Both IND doses demonstrated an acceptable safety profile.
Conclusions
Once-daily IND 75 μg and IND 150 μg via Breezhaler® in combination with background ICS therapy provided substantial bronchodilation in children with asthma and were well tolerated. Taken together, these clinical and systemic exposure findings support IND 75 μg as the most appropriate dose for evaluation in Phase III trials in combination with MF in pediatric asthma.
Trial Registration
ClinicalTrials.gov (NCT02892019; 08-Sep-2016).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Asthma is a chronic inflammatory disorder of the airways affecting more than 262 million people of all ages, worldwide [1, 2]. It is one of the most common chronic diseases reported in children [2]. As per the International study of Asthma and Allergies in Childhood (ISAAC), the global prevalence of asthma among children aged 6–7 years is 10.8% [3, 4]. Childhood asthma is known for male predominance prior to puberty, common remission, and rare mortality, while adult-onset disease is more prevalent in women with low remission rates and increased mortality [5]. Recurrent episodes of wheezing, coughing, chest tightness, and dyspnea might affect the quality of life in children [5].
Although most pediatric asthma cases are controlled with low- to medium-dose inhaled corticosteroids (ICS), a substantial proportion of children require maintenance treatment of high-dose ICS with an additional controller for their symptom control [6]. The Global Initiative for Asthma (GINA) guidelines recommend the use of long-acting β2-agonists (LABAs) in combination with ICS as maintenance therapy for children aged 6–11 years who remain symptomatic despite low doses of ICS (GINA Step 3) [7]. The addition of LABA to ICS has been shown to improve lung function and asthma control and reduce exacerbations and rescue medication use, with a similar safety profile to either ICS alone or placebo in pediatric patients with asthma [8,9,10]. Non-adherence to medication is a major cause of poor control of asthma and may be related to several factors including complicated regimen [11]. Although both once-daily (od) and twice-daily (bid) regimen were reported to be equally effective, od regimen improved adherence and had a lower risk of treatment discontinuation in pediatric and young patients [11,12,13]. However, the currently available ICS/LABA combination therapies for children require a bid regimen [14, 15]. Consequently, there is a need for new treatment options for pediatric patients with asthma.
Indacaterol acetate (IND) is an ultra-LABA with rapid onset of action and sustained bronchodilator effect, making it an ideal od combination with an ICS [16]. The od mometasone furoate (MF) and IND combination delivered via Breezhaler® is already approved as a maintenance treatment of asthma in adults and adolescents [17]. However, od, single-inhaler, MF/IND combination is currently being developed for treating pediatric patients (aged 6–11 years) with asthma [18]. The efficacy, safety, and dosing of IND in the pediatric population needed to be established to support pediatric development of od MF/IND.
Previously, a dose-ranging study has demonstrated the efficacy and safety of IND 75 μg and IND 150 μg in adult patients with asthma [19]. Limited information was available about the pharmacokinetics of IND in the pediatric asthma population prior to the conduct of the present study. However, systemic exposure (100–400 μg doses, od dosing for 7 days) assessments showed dose-dependent increases which were comparable to adults (similar doses) in cross-study comparisons (data on file, CQAB149C2101). Based on the available data in adults [19,20,21] and pharmacokinetic information in children, IND 75 μg and IND 150 μg were considered suitable for evaluation to establish appropriate dose in combination therapy (ICS/LABA) for further studies in a pediatric population with persistent asthma [22].
The objective of this study was to assess the efficacy, safety, and systemic exposure of two IND doses (75 μg od and 150 μg od) administered via Breezhaler® in children (aged ≥ 6 to < 12 years) with persistent asthma who were on background fluticasone propionate (FLU) to enable the selection of appropriate dose to be further progressed to long-term clinical trials.
2 Methods
2.1 Study Design
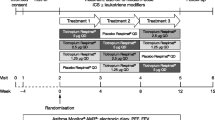
This was a Phase IIb, multicenter, randomized, double-blind, 2-week treatment, parallel-group study in pediatric patients with persistent asthma conducted between April 2017 and July 2019 [22]. The study consisted of a 30-day screening period, followed by a 2-week run-in period, a 2-week treatment period, and a 30-day safety follow-up. The details of the study design are presented in Fig. 1. The study design did not include a placebo arm as including placebo is against scientific and ethical conduct when the background standard-of-care is not optimized for pediatric populations with asthma [23]. The study was approved by the independent ethics committee or institutional review boards of each participating center (Online Resource, Table S1) and was conducted in accordance with the International Conference on Harmonization Guidelines for Good Clinical Practice and the Declaration of Helsinki.
Written informed consent from the parent/legal guardian of pediatric participants and assent by the pediatric patient (depending on local requirements) were obtained. A single parent/legal guardian was designated to complete all electronic patient diary (e-Diary) entries and attend all clinic visits with the patient. The parent/legal guardian was required to be willing and able to assist the child with the procedures including compliance with study medication, completion of the e-Diary, etc.
2.2 Participants
Participants were recruited from 29 centers across 11 countries. Eligible patients included in the study were male and female children aged ≥ 6 years to < 12 years with asthma for ≥ 1 year prior to enrollment in the study and receiving a stable low-dose ICS (with or without additional controller), or stable medium-dose ICS (monotherapy or together with leukotriene receptor antagonist [LTRA]) for ≥ 4 weeks before screening. Patients who could tolerate FLU 100 μg bid and had a pre-bronchodilator forced expiratory volume in one second (FEV1) ≥ 50 and ≤ 90% of the predicted normal value at screening and demonstrated an increase in FEV1 of ≥ 12% within 30 min of administration of salbutamol 400 μg or albuterol 360 μg were included in the study. Patients were excluded if they were treated with high-dose ICS or medium-dose ICS in combination with a LABA, had evidence of an unstable disease within 4 weeks prior to screening, had experienced asthma attack/exacerbation requiring systemic corticosteroids or hospitalization or an emergency room visit within 3 months prior to screening or ≥ 3 separate exacerbations in the 12 months prior to screening. Patients with a history of long QT syndrome or a corrected QT interval measured at the start and end of the run-in period were also excluded. Patients who experienced moderate or severe asthma exacerbation were discontinued from the study during screening prior to randomization (list of key inclusion and exclusion criteria is provided in the supplementary material).
2.3 Randomization and Procedures
Interactive response technology was used to randomize all the eligible patients to one of the treatment arms. This could ensure that the treatment assignment was unbiased, and all staff remained masked to allocation. Randomization was stratified by region. Eligible patients were randomly assigned (1:1) to receive IND 75 µg od or IND 150 µg od, both via Breezhaler®. The dose/regimen, route of administration, and duration of treatment were based upon known pharmacokinetic/pharmacodynamic effects of IND as well the clinical data from Phase II studies in asthma in adults and available data from children (data on file, CQAB149C2101). Indacaterol acetate od doses were administered in the morning via Breezhaler®. Fluticasone propionate 100 μg bid (morning and evening) was delivered via Diskus® throughout the study period. Patients were provided with a short-acting β2-agonist (100 μg salbutamol/90 μg albuterol per inhalation) as rescue medication throughout the study period. All patients were required to attend clinic visits on Day 1 and Day 14 for their morning FLU dose, pre-dose trough measurements of lung function prior to taking the study medication, and post-dose measurements. More information on randomization and procedure has been provided in supplementary material.
2.4 Outcome and Assessments
The primary end point was change in pre-dose trough FEV1 from baseline to Week 2 (Day 14) with IND 75 μg and IND 150 μg. The pre-dose trough FEV1 was defined as the mean of two FEV1 values measured at − 45 min and − 15 min pre-dose.
Secondary efficacy endpoints included change in Pediatric Interviewer-Administered Asthma Control Questionnaire (ACQ-IA) score from baseline to Day 14, change in FEV1 and forced vital capacity (FVC) at Day 14 post-dose at 30 min and 1 h, change in pre-dose peak expiratory flow (PEF, assessed once in the morning and once in the evening) over 2 weeks of treatment, change in asthma symptoms and the use of rescue medication over 2 weeks. The proportion of patients who achieved a decrease in ACQ-IA score of ≥ 0.5 units from baseline over 2 weeks was also assessed. Additional secondary endpoints included the evaluation of the systemic exposure to IND in plasma using a sparse pharmacokinetic sampling approach. Blood samples for pharmacokinetic analysis were collected at pre-dose (≤ 2 h) and at 15-min and 1-h post-dose on Day 1 and Day 14 of treatment period. At specified time points, a 3-L blood sample was collected in lithium heparin tubes. In total, for the pharmacokinetic analysis, 18 mL blood was drawn. Within 30 min, the sample was centrifuged at 3–5 °C for 15 min at approximately 2000 g. Immediately after centrifugation, the supernatant was transferred into 1.8 mL NUNC tubes that were frozen within 60 min of blood sampling over solid carbon dioxide (dry ice) and then, kept frozen at or below − 20 °C for pending analysis. All time points listed were relative to the time of dose administration and were recorded in eCRF (electronic Case Report Form). The concentrations of IND in plasma were determined by a validated liquid chromatography–mass spectrometry/mass spectrometry (LC–MS/MS) method [24] at a single bioanalytical laboratory; the lower limit of quantification (LLOQ) was 5.00 pg/mL.
Safety and tolerability were evaluated for both doses of IND throughout the study. Adverse events (AEs) were monitored for all patients evaluating the severity and relationship to treatment. MedDRA Version 22.0 has been used for the reporting of AEs. Electrocardiogram (ECG) and laboratory tests were also measured as part of the safety assessment.
2.5 Statistical Analyses
The primary and secondary efficacy analyses were based on the full analyses set (FAS), consisting of all randomized patients who received at least one dose of study medication. Supportive analyses for primary efficacy were performed in the per protocol set (PPS), which included all patients in the FAS who had no major protocol deviations. Patients in the PPS were analyzed according to the treatment they received. Continuous variables were summarized using descriptive statistics (n, mean, 25th percentile, median, 75th percentile, standard deviation [SD], minimum and maximum) and categorical variables were summarized in terms of the number and percentage of patients in each category. Inferential testing statistics were not performed since the sample was small and power was limited. The safety set was used in the analysis of pharmacokinetics and safety variables, comprising all patients who received at least one dose of study medication. The patients were analyzed according to the treatment received. Listings and descriptive statistics were provided for pharmacokinetic concentration data. Plasma concentrations were expressed in pg/mL units. Concentrations below the LLOQ were treated as zero in summary statistics of concentration data. All analyses were performed using SAS Version 9.4. Detailed information regarding statistical analysis is provided in supplementary material.
3 Results
In total, 80 patients were randomized (1:1) to receive IND 75 µg or IND 150 µg. Most patients (95.0%) completed two weeks of treatment. Patient demographic and baseline asthma characteristics were well balanced across the treatment groups (Table 1).
The study met its primary end point with both doses of IND showing improvement in the pre-dose trough FEV1 compared to baseline after 2 weeks of treatment. The median change from baseline in pre-dose trough FEV1 was comparable between IND 75 μg (167 mL) and 150 μg (154 mL) treatment arms, although increase from baseline with IND 75 μg dose was numerically higher than that with IND 150 μg dose (Fig. 2). However, the mean change from baseline in pre-dose trough FEV1 for IND 75 μg (212 mL) was higher than that for IND 150 μg (171 mL). An extreme value (change from baseline of 1180 mL) observed in the IND 75 μg group and mean change from baseline might have been inflated in higher direction. Similarly, a supportive analysis to assess the treatment effects in PPS performed for pre-dose trough FEV1 showed improvements with both doses of IND after 2 weeks of treatment. The mean change from baseline FEV1 observed for the IND 75 μg dose (226 mL) was higher than that for the IND 150 μg dose group (195 mL).
Change in pre-dose trough FEV1 for IND doses after two weeks of treatment. Pre-dose trough FEV1 is defined as the mean of the two FEV1 values measured 45- and 15-min pre-dose. Baseline FEV1 is defined as average of the −45 min and −15 min FEV1 values taken on Day 1 prior to the first dose. Only patients with a value at both baseline and Day 14 were included. Spirometry measurements taken within 6 h of rescue medication use, or within 7 days of systemic corticosteroids use, or actually measured outside the 22- to 30-h time window from the last dose of the previous day (Day 13) were set to missing. There is an outlier in the IND 75 µg dose group (one patient with lower lung volume at the start of examination). FEV1 forced expiratory volume in one second, IND indacaterol acetate
At Day 14, both IND 75 µg and IND 150 μg showed improvement in post-dose FEV1 compared with baseline after 30 min (mean change: 224 mL and 234 mL), and 1 h (mean change: 258 mL and 224 mL) of drug administration, respectively. The mean change of post-dose FVC from baseline was 141 mL and 81 mL with IND 75 µg and IND 150 μg, respectively, after 2 weeks of treatment. Both treatments showed improvements in the ACQ-IA score over 2 weeks with a 0.270 unit decrease from baseline in the IND 75 μg group and a 0.375 unit decrease from baseline in the IND 150 μg group, respectively. Overall, 36.1% and 25% patients achieved a decrease from baseline in the ACQ-IA score of ≥ 0.5 units in IND 75 μg and 150 μg dose groups, respectively. The improvement in post-dose FEV1 was comparable across doses while improvement in post-dose FVC, and ACQ-IA score were higher for the IND 75 μg than that for the IND 150 μg dose group. Improvement in morning (mean change, 14.7 L/min and 29.6 L/min) and evening (mean change, 15.2 L/min and 29.7 L/min) PEF from baseline was observed with IND 75 and 150 μg doses over 2 weeks of treatment, respectively. The percentage of days without rescue medication and asthma symptom-free days were reduced in both IND 75 μg and IND 150 μg doses over two weeks of treatment. Improvement in morning and evening PEF values, percentage of days without rescue medication and percentage of asthma symptom-free days was higher with IND 150 μg than IND 75 μg dose groups (Table 2).
A dose-dependent increase in plasma IND concentration was observed between the two IND dose groups from Day 1 to Day 14 (Table 3).
Safety data for both treatments are shown in Table 4. Overall, 13 patients (34.2%) in the IND 75 μg group and 3 patients (7.3%) in the IND 150 μg group experienced at least one AE. The most frequently reported AEs were upper respiratory tract infections and asthma exacerbations. No serious AEs or deaths were reported during the study period. One patient in the IND 75 μg dose group experienced treatment-emergent severe AE of asthma (exacerbation) not related to treatment. Three patients were observed with suspected drug-related AEs (nausea, vomiting, increase in blood glucose and dysphonia) in the IND 75 μg dose and one patient (nausea) in the IND 150 μg dose group. One patient in each of the dose groups discontinued permanently due to AEs (nausea and vomiting) suspected to be drug related. No new or unexpected safety signals were observed in the study. The overall incidence or proportion of patients with newly occurring or worsening clinically notable laboratory or ECG values was low.
4 Discussion
In the present study, IND in combination with background ICS therapy proved beneficial in terms of lung function and asthma control with lower systemic exposure of the drug in pediatric patients with persistent asthma. The study showed that the IND 75 μg od or IND 150 µg od in combination with background ICS resulted in meaningful improvements in pre-dose trough FEV1 in both doses with greater benefits observed with the IND 75 μg group. Supportive analysis results were consistent with primary analysis showing higher improvement in the IND 75 μg dose group.
Studies indicating clinically relevant improvement in baseline pre-dose FEV1 have been reported for other LABAs in patients aged ≥ 5 to < 12 years. In the CHASE 3 study, budesonide/formoterol (160/9 µg) versus budesonide (160 µg) alone in children (aged 6 to < 12 years) showed a statistically significant greater change from baseline in pre-dose FEV1 to 1-h post-dose FEV1 with treatment difference of 120 mL (95% CI 30–200; p = 0.006) at Week 12 while a numerical difference of 80 mL (95% CI 00–160; p = 0.063) was observed with budesonide/formoterol (160/4.5 µg) versus budesonide (160 µg) alone [25]. In another study, fluticasone/formoterol (100/10 µg) was superior to fluticasone (100 µg) alone with a treatment difference of 70 mL (95% CI 30–110) in change from pre-dose FEV1 at baseline to 2-h post-dose FEV1 over 12 weeks in patients aged 5 to < 12 years with persistent asthma [26].
In the secondary efficacy analyses, the post-dose FVC change was greater in the IND 75 μg group than in the IND 150 μg group, while the change in post-dose FEV1 was comparable between both doses after 2 weeks of treatment. Further, improvements in morning and evening PEF changes were observed with numerically greater values seen in IND 150 μg than in IND 75 μg. Earlier studies report no significant change in baseline pre-dose FVC to the post-dose FVC with any of the ICS/LABA combinations studied (budesonide/formoterol, fluticasone/formoterol, fluticasone/salmeterol vs ICS monotherapy) in children with asthma [25, 26]. A Cochrane review reported significantly greater improvement in morning PEF (7.55 L/min) and evening PEF (5.5 L/min) with ICS/LABA combination versus ICS alone in children with asthma [27]. In general, lung function benefits observed in this study were consistent with previous studies that compared ICS/LABA combinations over ICS monotherapy in pediatric patients [8, 28].
Improvement in asthma control in terms of ACQ-IA score, rescue medication-free periods and asthma symptom-free days from baseline were observed in both IND dose groups over 2 weeks of treatment. The results are in line with those of other studies reporting asthma control in children when treated with ICS/LABA therapy [13, 29,30,31].
The present study established lower plasma concentrations of the IND 75 μg compared with IND 150 μg in children with asthma at the corresponding time points. Plasma concentrations of IND 75 µg od on Day 14 in patients with asthma aged ≥ 6 years and <12 years in this study were lower than the corresponding concentrations in adult patients with asthma at IND 150 µg od in a prior study (Table 3) [32]. The results agree with conclusions from an earlier study by Chawes et al [33], which compared the systemic exposure of beclomethasone dipropionate/formoterol combination in children, adolescents, and adults with asthma. The study observed that dosage regimen of medications should be adjusted for age and body weight to avoid high systemic drug levels in children when compared with adults. No new safety findings were reported with od IND doses indicating no incremental risks with LABA added on top of background ICS. This finding is in tandem with results of other trials in pediatric patients with asthma, in which use of a LABA as add-on to ICS did not contribute to additional safety concerns [25, 26].
The convenience of once-daily ICS/LABA dosing is likely to improve compliance in patients with asthma, leading to better patient outcomes [34]. A retrospective study has established improved adherence and asthma control with once-daily ICS/LABA administration compared to twice-daily administration in adolescents with asthma [13].
5 Conclusions
Once-daily IND 75 μg and IND 150 μg delivered via Breezhaler® with background ICS therapy, selected based on clinical evidence in adults and pharmacokinetic outcomes in children, showed meaningful improvement in lung function and asthma control in children aged ≥ 6 years and <12 years with asthma. Both treatments were well tolerated with no new or unexpected safety concerns. Lower systemic exposure compared to adults was observed with IND 75 μg than IND 150 μg, while providing comparable lung function benefits. Based on these findings, IND 75 μg dose was considered appropriate for evaluating once-daily (MF/IND) combination therapies in further confirmatory Phase III studies in this 6- to 11-year-old population.
References
Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22. https://doi.org/10.1016/S0140-6736(20)30925-9.
Asthma. World Health Organization. 2021. https://www.who.int/news-room/fact-sheets/detail/asthma. Accessed 28 Sep 2021.
Uphoff EP, Bird PK, Antó JM, Basterrechea M, von Berg A, Bergström A, Bousquet J, Chatzi L, Fantini MP, Ferrero A, Gehring U, Gori D, Heinrich J, Keil T, Kull I, Lau S, Maier D, Momas I, Narduzzi S, Porta D, Ranciere F, Roumeliotaki T, Schikowski T, Smit HA, Standl M, Sunyer J, Wright J. Variations in the prevalence of childhood asthma and wheeze in MeDALL cohorts in Europe. ERJ Open Res. 2017;3(3):00150–2016. https://doi.org/10.1183/23120541.00150-2016.
Pearce N, Ait-Khaled N, Beasley R, Mallol J, Keil U, Mitchell E, Robertson C, Group IPTS. Worldwide trends in the prevalence of asthma symptoms: phase III of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax. 2007;62(9):758–66. https://doi.org/10.1136/thx.2006.070169.
Trivedi M, Denton E. Asthma in children and adults-what are the differences and what can they tell us about asthma? Front Pediatr. 2019;7:256. https://doi.org/10.3389/fped.2019.00256.
Haktanir Abul M, Phipatanakul W. Severe asthma in children: evaluation and management. Allergol Int. 2019;68(2):150–7. https://doi.org/10.1016/j.alit.2018.11.007.
GINA. Global strategy for asthma management and prevention. 2021. http://ginasthma.org/. Accessed 26 Sep 2021.
Chauhan BF, Chartrand C, Ni Chroinin M, Milan SJ, Ducharme FM. Addition of long-acting beta2-agonists to inhaled corticosteroids for chronic asthma in children. Cochrane Database Syst Rev. 2015;2015(11):Cd007949. https://doi.org/10.1002/14651858.CD007949.pub2.
Zhao Y, Han S, Shang J, Zhao X, Pu R, Shi L. Effectiveness of drug treatment strategies to prevent asthma exacerbations and increase symptom-free days in asthmatic children: a network meta-analysis. J Asthma. 2015;52(8):846–57. https://doi.org/10.3109/02770903.2015.1014101.
Akpinarli A, Tuncer A, Saraçlar Y, Sekerel BE, Kalayci O. Effect of formoterol on clinical parameters and lung functions in patients with bronchial asthma: a randomised controlled trial. Arch Dis Child. 1999;81(1):45–8. https://doi.org/10.1136/adc.81.1.45.
Price D, Robertson A, Bullen K, Rand C, Horne R, Staudinger H. Improved adherence with once-daily versus twice-daily dosing of mometasone furoate administered via a dry powder inhaler: a randomized open-label study. BMC Pulm Med. 2010;10:1. https://doi.org/10.1186/1471-2466-10-1.
Kerwin EM, Oppenheimer JJ, LaForce C, Parasuraman B, Miller CJ, O’Dowd L, Goldman M. Efficacy and tolerability of once-daily budesonide/formoterol pressurized metered–dose inhaler in adults and adolescents with asthma previously stable with twice-daily budesonide/ formoterol dosing. Ann Allergy Asthma Immunol. 2009;103(1):62–72. https://doi.org/10.1016/S1081-1206(10)60145-7.
Langley RJ, Dryden C, Westwood J, Anderson E, Thompson A, Urquhart D. Once daily combined inhaled steroid and ultra long-acting bronchodilator prescribing in pediatric asthma: a dual Center retrospective cohort study. J Asthma. 2021;58(4):512–3. https://doi.org/10.1080/02770903.2019.1702674.
Editor DDT. FDA approves AstraZeneca’s Symbicort to treat pediatric asthma. 2017. https://www.drugdiscoverytrends.com/fda-approves-astrazenecas-symbicort-to-treat-pediatric-asthma/ Accessed 26 Sep 2021.
Drugs DFF-A. 2008. https://www.accessdata.fda.gov/drugsatfda_docs/label/2008/021077s029lbl.pdf. Accessed 26 Sep 2021.
Rossi A, Polese G. Indacaterol: a comprehensive review. Int J Chron Obstruct Pulmon Dis. 2013;8:353–63. https://doi.org/10.2147/COPD.S21625.
Indacaterol/mometasone EMAsop, characteristics. 2020. https://www.ema.europa.eu/en/medicines/human/EPAR/atectura-breezhaler. Accessed 26 Sep 2021.
Study to compare the pharmacokinetics of mometasone furoate alone and in combination with indacaterol in patients ≥ 6 to < 12 years old with asthma. https://clinicaltrials.gov/ct2/show/NCT04589663. Accessed 31 Dec 2021.
Efficacy and safety of different doses of indacaterol. https://clinicaltrials.gov/ct2/show/NCT01079130. Accessed 07 Dec 2021.
Efficacy, safety, tolerability, and pharmacokinetics of indacaterol salts in patients with asthma. https://clinicaltrials.gov/ct2/show/NCT00927901. Accessed 07 Dec 2021.
Efficacy, safety and pharmacokinetics of indacaterol acetate in patients with persistent asthma. https://clinicaltrials.gov/ct2/show/NCT01609478. Accessed 07 Dec 2021.
Efficacy and safety of indacaterol acetate delivered via the concept1 inhalation device in children greater or equal to 6 and less than 12 years of age with asthma. https://clinicaltrials.gov/ct2/show/NCT02892019. Accessed 07 Dec 2021.
Di Pietro ML, Cutrera R, Teleman AA, Barbaccia ML. Placebo-controlled trials in pediatrics and the child’s best interest. Ital J Pediatr. 2015;41:11. https://doi.org/10.1186/s13052-015-0118-6.
Shimada S, Vaidya S, Khindri S, Tashiro N, Cheng Y, Hara H, Majumdar T, Woessner R, Furihata K, Kobayashi K. Pharmacokinetics of QMF149 in Japanese versus Caucasian subjects: an open-label, randomized phase I study. Int J Clin Pharmacol Ther. 2015;53(5):398–407. https://doi.org/10.5414/CP202239.
Pearlman DS, Eckerwall G, McLaren J, Lamarca R, Puu M, Gilbert I, Jorup C, Sandin K, Lanz MJ. Efficacy and safety of budesonide/formoterol pMDI vs budesonide pMDI in asthmatic children (6-<12 years). Ann Allergy Asthma Immunol. 2017;118(4):489-99.e1. https://doi.org/10.1016/j.anai.2017.01.020.
Płoszczuk A, Bosheva M, Spooner K, McIver T, Dissanayake S. Efficacy and safety of fluticasone propionate/formoterol fumarate in pediatric asthma patients: a randomized controlled trial. Ther Adv Respir Dis. 2018;12:1753466618777924. https://doi.org/10.1177/1753466618777924.
Ni Chroinin M, Lasserson TJ, Greenstone I, Ducharme FM. Addition of long-acting beta-agonists to inhaled corticosteroids for chronic asthma in children. Cochrane Database Syst Rev. 2009;3:Cd007949. https://doi.org/10.1002/14651858.CD007949.
Vogelberg C, Goldstein S, Graham L, Kaplan A, de la Hoz A, Hamelmann E. A comparison of tiotropium, long-acting β(2)-agonists and leukotriene receptor antagonists on lung function and exacerbations in paediatric patients with asthma. Respir Res. 2020;21(1):19. https://doi.org/10.1186/s12931-020-1282-9.
Oliver AJ, Covar RA, Goldfrad CH, Klein RM, Pedersen SE, Sorkness CA, Tomkins SA, Villarán C, Grigg J. Randomised trial of once-daily vilanterol in children with asthma on inhaled corticosteroid therapy. Respir Res. 2016;17:37. https://doi.org/10.1186/s12931-016-0353-4.
Lemanske RF Jr, Mauger DT, Sorkness CA, Jackson DJ, Boehmer SJ, Martinez FD, Strunk RC, Szefler SJ, Zeiger RS, Bacharier LB, Covar RA, Guilbert TW, Larsen G, Morgan WJ, Moss MH, Spahn JD, Taussig LM. Step-up therapy for children with uncontrolled asthma receiving inhaled corticosteroids. N Engl J Med. 2010;362(11):975–85. https://doi.org/10.1056/NEJMoa1001278.
Ducharme FM, Ni Chroinin M, Greenstone I, Lasserson TJ. Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma. Cochrane Database Syst Rev. 2010;4:Cd005533. https://doi.org/10.1002/14651858.CD005533.pub2.
Miller D, Vaidya S, Jauernig J, Ethell B, Wagner K, Radhakrishnan R, Tillmann HC. Lung function, pharmacokinetics, and tolerability of inhaled indacaterol maleate and acetate in asthma patients. Respir Res. 2020;21(1):248. https://doi.org/10.1186/s12931-020-01501-1.
Chawes BL, Govoni M, Kreiner-Møller E, Vissing NH, Poorisrisak P, Mortensen L, Nilsson E, Bisgaard A, Dossing A, Deleuran M, Skytt NL, Samandari N, Piccinno A, Sergio F, Ciurlia G, Poli G, Acerbi D, Singh D, Bisgaard H. Systemic exposure to inhaled beclometasone/formoterol DPI is age and body size dependent. Respir Med. 2014;108(8):1108–16. https://doi.org/10.1016/j.rmed.2014.05.007.
Averell CM, Stanford RH, Laliberté F, Wu JW, Germain G, Duh MS. Medication adherence in patients with asthma using once-daily versus twice-daily ICS/LABAs. J Asthma. 2021;58(1):102–11. https://doi.org/10.1080/02770903.2019.1663429.
Acknowledgements
We thank the investigators and patients at the investigative sites for their support during the conduct of the study. Under the direction of authors, Rabi Panigrahy, Roopashree Subbaiaih, Anupama Boddupalli and Sagar Prakash Wagh, (professional medical writers; Novartis) assisted in the preparation of this article in accordance with the third edition of Good Publication Practice guidelines (https://www.ismpp.org/gpp3).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the independent ethics committee or institutional review boards of each participating center and was conducted in accordance with the International Conference on Harmonization Guidelines for Good Clinical Practice and the Declaration of Helsinki. Written informed consent from the parent/legal guardian of pediatric participants and assent by the pediatric patient (depending on local requirements) were obtained.
Consent for publication
Not applicable.
Data availability
Novartis is committed to sharing access to patient-level data and supporting documents from eligible studies with qualified external researchers. These requests are reviewed and approved by an independent review panel based on scientific merit. All data provided are anonymised to respect the privacy of patients who have participated in the trial in line with applicable laws and regulations.
Code availability
Not applicable.
Funding
The study was funded by Novartis Pharmaceuticals Corporation, East Hanover.
Conflict of interest
BES reports speaker fees from Abbott, Abdi Ibrahim, and Sandoz, outside the submitted work. HN, IL, TP, and EC have nothing to disclose. PD and MV are employees of Novartis Pharmaceutical Corporation, East Hanover. MJ is an employee of Novartis Institutes for BioMedical Research, Cambridge. BS was an employee of Novartis Healthcare Pvt. Ltd, Hyderabad; AK was an employee of Novartis Pharma AG, Basel; VM was an employee of Novartis Pharmaceutical Corporation, East Hanover and SV was an employee of Novartis Institutes for BioMedical Research, Cambridge at the time of study completion.
Author contributions
The study was designed by SV, PD, VM, and BS. MV, and SV contributed to conduct of these studies. Data were acquired by MV and analyzed by SV, MJ, PD and BS. All authors contributed equally to the interpretation of data. BES is the principal investigator for this study. Data were reviewed by BES, HN, IL, TP, EC, and AK. All authors contributed to intellectual content of the manuscript and approved for publication.
Additional information
Adam Kolarz, Volkan Manga, Soniya Vaidya and Biswajit Sen: Employee of Novartis at the time of study completion.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sekerel, B.E., Nell, H., Laki, I. et al. Efficacy, Safety, and Systemic Exposure of Once-Daily Indacaterol Acetate in Pediatric Asthma: A Randomized, Double-Blind, Controlled Dose-Finding Study. Clin Drug Investig 43, 719–728 (2023). https://doi.org/10.1007/s40261-023-01300-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-023-01300-8