Abstract
Background and Objective
Because of the narrow therapeutic window and huge inter-individual variation, the individual precision on anticoagulant therapy of warfarin is challenging. In our study, we aimed to construct a Back Propagation Neural Network (BPNN) model to predict the individual warfarin maintenance dose among Chinese patients who have undergone heart valve replacement, and validate its prediction accuracy.
Methods
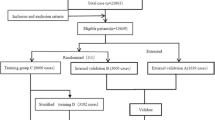
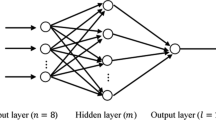
In this study, we analyzed 13,639 eligible patients extracted from the Chinese Low Intensity Anticoagulant Therapy after Heart Valve Replacement database, which collected data on patients using warfarin after heart valve replacement from 15 centers all over China. Ten percent of patients who were finally enrolled in the database were used as the external validation, while the remaining were randomly divided into the training and internal validation groups at a ratio of 3:1. Input variables were selected by univariate analysis of the general linear model; 2.0, the mean value of the international normalized ratio (INR) range 1.5–2.5, was used as the mandatory variable. The BPNN model and the multiple linear regression (MLR) model were constructed by the training group and validated through comparisons of the mean absolute error (MAE), mean squared error (MSE), root mean squared error (RMSE), and ideal predicted percentage.
Results
Finally, 10 input variables were selected and a three-layer BPNN model was constructed. In the BPNN model, the value of MAE (0.688 mg/day and 0.740 mg/day in internal and external validation, respectively), MSE (0.580 mg/day and 0.599 mg/day in internal and external validation, respectively), and RMSE (0.761 mg/day and 0.774 mg/day in internal and external validation, respectively) were achieved. Ideal predicted percentages were high in both internal (63.0%) and external validation (59.7%), respectively. Compared with the MLR model, the BPNN model showed a higher ideal prediction percentage in the external validation group (59.7% vs. 56.6%), and showed the best prediction accuracy in the intermediate-dose subgroup (internal validation group: 85.2%; external validation group: 84.7%) and a high predicted percentage in the high-dose subgroup (internal validation group: 36.2%; external validation group: 39.8%), but poor performance in the low-dose subgroup (internal validation group: 0%; external validation group: 0.3%). Meanwhile, the BPNN model showed better ideal prediction percentage in the high-dose group than the MLR model (internal validation: 36.2% vs. 31.6%; external validation: 42.8% vs. 37.8%).
Conclusion
The BPNN model shows promise for predicting the warfarin maintenance dose after heart valve replacement.
Plain Language Summary
Because of the narrow therapeutic window and huge inter-individual variation, the individual precision on anticoagulant therapy of warfarin is still a challenge. According to the rapid development of artificial intelligence, our study was based on a clinical big database and used the advanced algorithm—Back Propagation Neural Network—to construct a prediction model of warfarin maintenance dose. It showed a high prediction accuracy of over 59%, and manifested obvious improvement of the prediction ability in the high-dose group. Hence, the BPNN model shows promise for predicting the precise individual therapy of warfarin.



Similar content being viewed by others
References
Lim WY, Lloyd G, Bhattacharyya S. Mechanical and surgical bioprosthetic valve thrombosis. Heart. 2017;103(24):1934–41.
Egbe AC, Pislaru SV, Pellikka PA, et al. Bioprosthetic valve thrombosis versus structural failure: clinical and echocardiographic predictors. J Am Coll Cardiol. 2015;66(21):2285–94.
Puri R, Auffret V, Rodes-Cabau J. Bioprosthetic valve thrombosis. J Am Coll Cardiol. 2017;69(17):2193–211.
Osnabrugge RL, Mylotte D, Head SJ, et al. Aortic stenosis in the elderly: disease prevalence and number of candidates for transcatheter aortic valve replacement: a meta-analysis and modeling study. J Am Coll Cardiol. 2013;62(11):1002–12.
Bove T, Van Belleghem Y, Francois K, et al. Low target-INR anticoagulation is safe in selected aortic valve patients with the Medtronic Open Pivot mechanical prosthesis: long-term results of a propensity-matched comparison with standard anticoagulation. Interact Cardiovasc Thorac Surg. 2017;24(6):862–8.
Di Minno G, Russolillo A, Gambacorta C, Di Minno A, Prisco D. Improving the use of direct oral anticoagulants in atrial fibrillation. Eur J Intern Med. 2013;24(4):288–94.
Eikelboom JW, Connolly SJ, Brueckmann M, et al. Dabigatran versus warfarin in patients with mechanical heart valves. N Engl J Med. 2013;369(13):1206–14.
Marcy TR, Truong T, Rai A. Comparing direct oral anticoagulants and warfarin for atrial fibrillation, venous thromboembolism, and mechanical heart valves. Consult Pharm. 2015;30(11):644–56.
Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017;70(2):252–89.
Anderson J, Horne B, Stevens S, et al. Randomized trial of genotype-guided versus standard warfarin dosing in patients initiating oral anticoagulation. Circulation. 2007;116(22):2563–70.
Klein TE, Altman RB, Eriksson N, et al. Estimation of the warfarin dose with clinical and pharmacogenetic data. N Engl J Med. 2009;360(8):753–64.
Liu R, Li X, Zhang W, Zhou H-H. Comparison of nine statistical model based warfarin pharmacogenetic dosing algorithms using the racially diverse international warfarin pharmacogenetic consortium cohort database. PLoS One. 2015;10(8):e0135784.
Ugrinowitsch C, Fellingham GW, Ricard MD. Limitations of ordinary least squares models in analyzing repeated measures data. Med Sci Sports Exerc. 2004;36(12):2144–8.
Tao Y, Chen YJ, Fu X, Jiang B, Zhang Y. Evolutionary ensemble learning algorithm to modeling of warfarin dose prediction for Chinese. IEEE J Biomed Health Inform. 2019;23(1):395–406.
Dong J, Shi GH, Lu M, et al. Evaluation of the predictive performance of Bayesian dosing for warfarin in Chinese patients. Pharmacogenomics. 2019;20(3):167–77.
Tao Y, Chen YJ, Xue L, Xie C, Jiang B, Zhang Y. An ensemble model with cluster assumption for warfarin dose prediction in Chinese patients. IEEE J Biomed Health Inform. 2019. https://doi.org/10.1109/jbhi.2019.2891164(Epub 7 Jan 2019).
Hamberg AK, Hellman J, Dahlberg J, Jonsson EN, Wadelius M. A Bayesian decision support tool for efficient dose individualization of warfarin in adults and children. BMC Med Inform Decis Mak. 2015;15:7.
Tao H, Li Q, Zhou Q, et al. A prediction study of warfarin individual stable dose after mechanical heart valve replacement: adaptive neural-fuzzy inference system prediction. BMC Surg. 2018;18(1):10.
Grossi E, Podda GM, Pugliano M, et al. Prediction of optimal warfarin maintenance dose using advanced artificial neural networks. Pharmacogenomics. 2014;15(1):29–37.
Solomon I, Maharshak N, Chechik G, et al. Applying an artificial neural network to warfarin maintenance dose prediction. Isr Med Assoc J. 2004;6(12):732–5.
Dong L, Shi YK, Xu JP, et al. The multicenter study on the registration and follow-up of low anticoagulation therapy for the heart valve operation in China [in Chinese]. Zhonghua yi xue za zhi. 2016;96(19):1489–94.
Lenzini P, Wadelius M, Kimmel S, et al. Integration of genetic, clinical, and INR data to refine warfarin dosing. Clin Pharmacol Ther. 2010;87(5):572–8.
Steyerberg EW, Harrell FE Jr. Prediction models need appropriate internal, internal-external, and external validation. J Clin Epidemiol. 2016;69:245–7.
Zahedi F. An introduction to neural networks and a comparison with artificial intelligence and expert systems. Interfaces. 1991;21(2):25–38.
Carlucci D, Renna P, Schiuma G. Evaluating service quality dimensions as antecedents to outpatient satisfaction using back propagation neural network. Health Care Manag Sci. 2013;16(1):37–44.
Sridevi K, Sivaraman E, Mullai P. Back propagation neural network modelling of biodegradation and fermentative biohydrogen production using distillery wastewater in a hybrid upflow anaerobic sludge blanket reactor. Bioresour Technol. 2014;165:233–40.
Rumelhart DE, Hinton GE, Williams RJ. Learning internal representations by error propagation. Amsterdam: Elsevier Inc.; 1988.
Xiang LC, Xiao LH, Li M, et al. Diagnosis values of back propagation neural network integrating age, transrectal ultrasound characteristics and serum PSA for prostate cancer [in Chinese]. Sichuan da xue xue bao Yi xue ban. 2016;47(1):77–80 (84).
Sheiner LB, Beal SL. Some suggestions for measuring predictive performance. J Pharmacokinet Biopharm. 1981;9(4):503–12.
Justice AC, Covinsky KE, Berlin JA. Assessing the generalizability of prognostic information. Ann Intern Med. 1999;130(6):515–24.
Zhao W, Berger V. Imbalance control in clinical trial subject randomization-from philosophy to strategy. J Clin Epidemiol. 2018;101:116–8.
Moons KG, Kengne AP, Grobbee DE, et al. Risk prediction models: II. External validation, model updating, and impact assessment. Heart. 2012;98(9):691–8.
Dong L, Shi Y, Xu J, et al. The multicenter study on the registration and follow-up of low anticoagulation therapy for the heart valve operation in China. Natl Med J China. 2016;96(19):1489–94.
Gu Q, Kong Y, Schneede J, et al. VKORC1-1639G > A, CYP2C9, EPHX1691A > G genotype, body weight, and age are important predictors for warfarin maintenance doses in patients with mechanical heart valve prostheses in southwest China. Eur J Clin Pharmacol. 2010;66(12):1217–27.
Lee VW, You JH, Lee KK, Chau TS, Waye MM, Cheng G. Factors affecting the maintenance stable warfarin dosage in Hong Kong Chinese patients. J Thromb Thrombolysis. 2005;20(1):33–8.
Jie-qiong S, Shao-wen LIU, Song-wen C, et al. The relationships between anticoagulation therapy during operation and thromboembolic events in patients with persistent/permanent atrial fibrillation who underwent radiofrequency catheter ablation [in Chinese]. Chin J Cardiac Arrhythm. 2009;13(3):209–12.
Wang JT, Dong MF, Song GM, Ma ZS, Ma SJ. Combined low-dose aspirin and warfarin anticoagulant therapy of postoperative atrial fibrillation following mechanical heart valve replacement. J Huazhong Univ Sci Technol Med Sci. 2014;34(6):902–6.
Chen L, Xiao Y, Ma R, et al. Bipolar radiofrequency ablation is useful for treating atrial fibrillation combined with heart valve diseases. BMC Surg. 2014;14:32.
Dong L, Shi Y, Tian Z. The follow-up of 12 pregnant women with anticoagulation therapy after mechanical heart valve replacement. Chin J Obstet Gynecol. 2001;36(8):465–7.
Li D, Xin-hui L, Ying-kang S, Er-yong Z, Teng D, Li XR. Low-intensity anticoagulation therapy in the pregnant women with mechanical heart valves:a report with 56 cases [in Chinese]. Chin J Thorac Cardiovasc Surg. 2011;27(1):8–10.
Lip GYH, Al-Saady N, Jin J, et al. Anticoagulation control in warfarin-treated patients undergoing cardioversion of atrial fibrillation (from the Edoxaban Versus Enoxaparin-Warfarin in Patients Undergoing Cardioversion of Atrial Fibrillation Trial). Am J Cardiol. 2017;120(5):792–6.
Limdi NA, Beasley TM, Baird MF, et al. Kidney function influences warfarin responsiveness and hemorrhagic complications. J Am Soc Nephrol. 2009;20(4):912–21.
Hijazi Z, Hohnloser SH, Oldgren J, et al. Efficacy and safety of dabigatran compared with warfarin in relation to baseline renal function in patients with atrial fibrillation: a RE-LY (Randomized Evaluation of Long-term Anticoagulation Therapy) trial analysis. Circulation. 2014;129(9):961–70.
Kucuk M, Ozdemir R, Karacelik M, et al. Risk factors for thrombosis, overshunting and death in infants after modified blalock-taussig shunt. Acta Cardiol Sin. 2016;32(3):337–42.
Shao-hui W, Liang Z, Wei-feng J, et al. Risk factors of atrial fibrillation recurrence in patients who obtained ablation endpoints with longstanding persistent atrial fibrillation [in Chinese]. Int J Cardiovasc Dis. 2014;41(04):268–70.
Sharabiani A, Bress A, Douzali E, Darabi H. Revisiting warfarin dosing using machine learning techniques. Comput Math Methods Med. 2015;2015:560108.
Ma Z, Wang P, Gao Z, Wang R, Khalighi K. Ensemble of machine learning algorithms using the stacked generalization approach to estimate the warfarin dose. PLoS One. 2018;13(10):e0205872.
Li Q, Tao H, Wang J, et al. Warfarin maintenance dose prediction for patients undergoing heart valve replacement—a hybrid model with genetic algorithm and back-propagation neural network. Sci Rep. 2018;8(1):9712.
Saffian SM, Duffull SB, Wright DFB. Warfarin dosing algorithms underpredict dose requirements in patients requiring ≥ 7 mg daily: a systematic review and meta-analysis. Clin Pharmacol Ther. 2017;102(2):297–304.
Peng Q, Huang S, Chen X, et al. Validation of warfarin pharmacogenetic algorithms in 586 Han Chinese patients. Pharmacogenomics. 2015;16(13):1465–74.
Centers for Medicare & Medicaid Services. Medicare coverage database—potential NCD topics. http://www.cms.hhs.gov/mcd/ncpc_view_document.asp?id=1.
Acknowledgements
The authors appreciated the other members who provided their generous contributions during the study.
Author information
Authors and Affiliations
Contributions
QL and JW were co-first authors and were responsible for interpretation and analysis of the data, and drafting of the manuscript. HT and QZ were responsible for analysis of the data. JC and WQ were responsible for interpretation of the research. BF, JH and LD performed the conception work, and data acquisition. WHZ was responsible for revising the language for the content and verifying the design of the research. JC, as the corresponding author, was responsible for the conception and design of the research, and revising critically for important intellectual content. All authors approved the final version submitted for publication.
Corresponding author
Ethics declarations
Funding
This project was supported by the National Natural Science Foundation (Project Numbers 71974137 and 81641021) and the National Science and Technology Pillar Program during the Twelfth Five-Year Plan Period (Project Number 2011BAI11B18). The funding sources have no role in the design, implementation, data analysis, and article writing, or in the decision to submit the article for publication.
Conflict of interest
Qian Li, Jing Wang, Huan Tao, Qin Zhou, Jie Chen, Bo Fu, WenZhe Qin, Dong Li, JiangLong Hou, Jin Chen, and Wei-hong Zhang declare that they have no conflicts of interests.
Ethics approval
All methods and study protocols have been approved by the Ethics Committee of West China Hospital of Sichuan University (ChiECRCT-201792). As this was a retrospective study, as per the ethical approval documents.
Informed consent
Informed consent has been exempted.
Rights and permissions
About this article
Cite this article
Li, Q., Wang, J., Tao, H. et al. The Prediction Model of Warfarin Individual Maintenance Dose for Patients Undergoing Heart Valve Replacement, Based on the Back Propagation Neural Network. Clin Drug Investig 40, 41–53 (2020). https://doi.org/10.1007/s40261-019-00850-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-019-00850-0