Abstract
Background and Objective
This paper describes two studies, which aimed to compare the safety and plasma antithrombin activity of recombinant human antithrombin gamma (rhAT-gamma) with plasma-derived antithrombin (pAT) 60 IU/kg, and to establish bioequivalence by adjusting the rhAT-gamma dose to that at which plasma antithrombin activity equaled that for pAT 60 IU/kg, based on results of the first study.
Methods
Healthy adult men aged 20–45 years received once-daily doses of rhAT-gamma or pAT intravenously for 3 days (first study: 60 IU/kg of each; second study: 72 IU/kg of rhAT-gamma and 60 IU/kg of pAT). Maximum plasma antithrombin activity after three doses (Cmax,day3) and area under the plasma antithrombin activity-time curve after the third dose (AUC48–t) were analyzed. Safety was also assessed.
Results
In the first study, we compared AUCs to 121 h (when the lower limit of quantification was first observed). Mean Cmax,day3 was 1.67 IU/mL in the rhAT-gamma group and 1.77 IU/mL in the pAT group; mean AUC48–121 was 58.44 and 71.94 IU·h/mL, respectively. Thus, we set the dose of rhAT-gamma in the second study to 72 IU/kg. As a result, ratios of Cmax,day3 and AUC48–t in the rhAT-gamma vs. the pAT group were 105.7% (90% confidence interval 100.3, 111.3) and 100.5% (90% confidence interval 91.5, 110.4), respectively. Adverse events were more frequent in the rhAT-gamma group.
Conclusions
As 90% confidence intervals for Cmax,day3 and AUC48–t ratios for rhAT-gamma:pAT were within the acceptability range for bioequivalence, rhAT-gamma (72 IU/kg) and pAT (60 IU/kg) are considered bioequivalent.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In healthy adult men aged 20–45 years, once-daily intravenous doses of recombinant human antithrombin gamma (rhAT-gamma) (72 IU/kg) or plasma-derived antithrombin (60 IU/kg) over 3 days demonstrated bioequivalence. |
Treatment with once-daily rhAT-gamma for 3 days did not pose any safety concerns. |
As a result, intravenous rhAT-gamma 600 IU and 1800 IU formulations have been approved in Japan for the treatment of thrombophilia caused by congenital antithrombin deficiency and disseminated intravascular coagulation. |
1 Introduction
The coagulation and fibrinolytic systems work in a careful balance to keep blood flowing smoothly without thrombus formation or bleeding. The coagulation system is activated in response to a break in a blood vessel. A cascade of reactions coagulates the blood to stem the flow through the break, and the fibrinolytic system quickly dissolves clots to re-establish smooth blood flow again. The two systems are carefully coordinated: if either system malfunctions, this can result in thrombosis or excessive bleeding.
Antithrombin (AT) is a major coagulation inhibitor mainly synthesized in the liver [1]. This 58-kDa glycoprotein is a serine protease inhibitor that binds and inactivates thrombin and other coagulation factors, including factors IX, X, XI, and XII [2,3,4]. Antithrombin activity is enhanced 1000-fold by heparin [5]. Antithrombin is located primarily in the blood and extravascular areas, including epithelial cells [6]. The AT concentration in blood from healthy adults is approximately 15–27 mg/dL, and the AT half-life is approximately 65 h [7].
Antithrombin deficiency can be inherited or acquired [8, 9]. Congenital AT deficiency, which affects 1 in 2000 to 1 in 5000 people, typically presents with recurrent thrombosis from a young age [9]. Inherited AT deficiency is often caused by point mutations, deletions, or insertions in the AT gene SERPINC1 [10]. Acquired AT deficiency can result from reduced production or increased degradation of AT and is often associated with liver cirrhosis, nephrotic syndrome, disseminated intravascular coagulation, or thrombotic diseases.
Plasma-derived AT (pAT) products have been approved for the treatment of thrombogenic tendency attributed to congenital AT deficiency or disseminated intravascular coagulation with decreased AT [11]. Although existing pAT products are manufactured with safety measures to prevent the transmission of infectious diseases, these products may still contain an unknown infectious agent. Therefore, a recombinant human AT product could provide the same clinical benefits as the plasma-derived products, but without the risk of infection derived from human blood [12]. Furthermore, a recombinant form can be stably synthesized without relying on a supply of human plasma.
Human recombinant antithrombin alfa (rhAT-alfa) [ATryn®; rEVO Biologics, Framingham, MA, USA] is a transgenic AT preparation purified from the milk of goats genetically engineered to produce human AT [13]. In 2008, the European Union approved rhAT-alfa for the prevention of venous thromboembolism during surgery for patients with congenital AT deficiency. In 2009, the USA approved rhAT-alfa for the prevention of thromboembolic events in patients with congenital AT deficiency during perioperative and perinatal periods [14]. The sugar chain structure of rhAT-alfa differs significantly from native AT [13]. Furthermore, rhAT-alfa is quickly cleared from the blood and must be administered continuously by intravenous injection for 24 h [14].
A new recombinant form of AT gamma (rhAT-gamma) has been produced in Chinese hamster ovary cells to overcome the limitations associated with rhAT-alfa and pAT. This product is the first AT preparation with a similar sugar chain structure to native human AT [15]. Using POTELLIGENT® technology (BioWa, Inc., Princeton, NJ, USA) [16], we focused on changing the oligosaccharide structure of human AT produced recombinantly in mammalian cells from the original mature complex-type lacking a core fucose to the immature high-mannose type. Chinese hamster ovary cell lines deficient in α-1, 6-fucosyltransferase, and N-acetylglucosaminyltransferase-1 [17] were employed to generate homogeneous recombinant human ATs fully lacking a core fucose with complex (rhAT-Com) and high-mannose-type (rhAT-Man) oligosaccharides, respectively. Therefore, this rhAT-gamma preparation has similar pharmacokinetics and biological activities to native AT.
We report two randomized, parallel-group, phase I studies in healthy adult men given the AT products for 3 days. The studies were designed to evaluate the safety and pharmacokinetics of rhAT-gamma 60–72 IU/kg, and to compare the bioavailability and establish bioequivalence between rhAT-gamma and a pAT product (60 IU/kg).
2 Methods
2.1 Ethical Considerations
Protocols were approved by the Institutional Review Board at Osaka Pharmacology Clinical Research Hospital (Osaka, Japan). All subjects provided voluntary written informed consent before any study-specific procedures. This study was conducted at Osaka Pharmacology Clinical Research Hospital, in accordance with the ethical principles of the Declaration of Helsinki.
2.2 Subjects
Healthy adult men aged 20–45 years with body mass index of 18.5–25.0 kg/m2 at screening were enrolled. Subjects were excluded if they had a disease that required treatment, an allergy to the investigational drugs, a history of thrombosis or abnormal bleeding, a history of gastrointestinal hemorrhage, drug or alcohol dependence, a positive test for infectious disease, or a history of drug use within 4 weeks of study start. Subjects were also excluded if they had been previously treated with rhAT-gamma or had received another investigational drug within 4 months of study start. In addition, subjects were not eligible if, in the previous 3 months, they had been hospitalized, undergone surgery, or donated more than 200 mL of blood.
2.3 Study Design and Treatments
The first study was conducted to evaluate the plasma AT activity of rhAT-gamma and pAT (60 IU/kg). Twenty subjects were randomized (1:1) according to a randomly assigned allocation list. Either 60 IU/kg of rhAT-gamma or 60 IU/kg of pAT (Neuart® I.V.; Japan Blood Products Organization, Tokyo, Japan) was administered by intravenous drip over 1 h. The individual dose was calculated using subject bodyweight the day before administration. The volume of drug solution given to each subject was set at 200 mL. Subjects received once-daily doses for 3 days.
The second study was designed to establish bioequivalence of plasma AT activity between rhAT-gamma and pAT; the rhAT-gamma dose was reset to 72 IU/kg because our analyses in the first study showed that rhAT-gamma (72 IU/kg) and pAT (60 IU/kg) had similar plasma AT activity. Forty-two subjects were randomized (1:1) according to a randomly assigned allocation list in the second study. Subjects in both studies were kept in the clinical unit for 10 days, and returned for follow-up examinations 3, 7, and 14 weeks after study treatment (unpublished data on file; Kyowa Kirin Co, Ltd, Tokyo, Japan).
Importantly, the elimination half-lives of rhAT-gamma and pAT are extremely long (~ 60 h and ~ 50 h, respectively), such that it would have been very difficult to conduct a crossover study [18]. A randomized parallel-group design, with specific reference to bioequivalence test guidelines for generic drugs, was therefore employed.
The rationale for a 3-day treatment phase with rhAT-gamma was based on the results of a phase I, single-dose (60 IU/kg) study in healthy adult male individuals, in which the mean peak plasma AT concentration (Cmax 1.08 IU/mL) occurred 1.13 h after starting administration, and data were calculated for up to 49 h after starting administration. However, considering the transition of plasma AT activity, and the lower limit of quantification after single doses of rhAT-gamma 60 and 120 IU/kg, the area under the plasma concentration–time curve (AUC) ratio of AUC0–t/AUC0–∞ for plasma AT activity after a single dose of rhAT-gamma 60 IU/kg was estimated to be about 65%. This was considered inadequate for accurate comparison of pharmacokinetics. Therefore, we simulated plasma AT activity after rhAT-gamma 60 IU/kg administered once a day for 3 days; the simulation was based on data for plasma AT activity obtained in an earlier phase I study (unpublished data on file; Kyowa Kirin Co, Ltd). The ratio of AUC48–t/AUC48–∞ for plasma AT activity (with t as time when the lower limit of quantification was evident after 3 doses) was estimated to be about 75%, which is close to the recommended value of 80% in Japanese bioequivalence guidelines [19]; thus, rhAT-gamma 60 IU/kg administered once a day for 3 days was compared with single-dose administration. Clinically, the study pAT preparation is administered for 2–5 days; thus, the administration period was set as 3 days, considering the burden on subjects.
The study was conducted according to CONSORT guidelines. However, as a preliminary trial, the study was not registered with a clinical trial registry.
2.4 Pharmacokinetic and Bioequivalence Analyses
Plasma AT activity, plasma AT antigen concentration, and anti-Xa activity were analyzed: plasma AT activity by a chromogenic synthetic method using a validated test kit (at a centralized laboratory: SRL Medisearch Inc., Tokyo, Japan), which provides a measure of precision; and plasma AT antigen and anti-Xa activity were assessed by general test methods at the centralized laboratory. In the first study, blood samples for these analyses were obtained on days 1 and 2, immediately before administration of the investigational drug, and at 1, 4, and 10 h after administration of the investigational drug. On day 3, blood samples were obtained immediately before administration of the investigational drug, and at 1, 4, 10, 25, 49, and 73 h after administration. In the second study, blood samples were obtained on days 1 and 2, immediately before administration of the investigational drug, and at 1, 4, and 10 h after administration. On day 3, blood samples were obtained immediately before administration of the investigational drug, and at 1, 4, 10, 25, 49, 73, 97, 121, 145, and 169 h after administration. From day 4 to day 10, samples were obtained daily. Blood samples were also obtained at the first follow-up visit (3 weeks after initial administration of the investigational drug). In both studies, the primary endpoints were peak plasma concentration after the third dose (Cmax,day3) and AUC48–t, calculated from plasma AT activity during the study period. Thus, AUC48–t was the area under the plasma AT activity time curve from 48 h after the first dose until the last time point at which plasma AT activity could be detected using the linear trapezoidal method. The pharmacokinetic parameters measured after three doses were used so that the AUC could be sufficiently evaluated. Importantly, the dose of rhAT-gamma showing bioequivalence with pAT (60 IU/kg) in the first study was then examined in the second study based on first-study ratios for Cmax,day3 and AUC48–t. As t for rhAT-gamma activity was 121 h, and that for pAT activity was 168 h, AUC from 48 to 121 h after initial administration (AUC48–121) was calculated using the linear trapezoidal method in all subjects.
Secondary endpoints included plasma AT activity; AT antigen concentration; anti-Xa activity; and additional pharmacokinetic parameters calculated from plasma AT activity, plasma antigen concentrations, and plasma anti-Xa. For these parameters, we used the value obtained by subtracting the pre-administration value from the value obtained after administration of the investigational drug, as the resulting value was considered to be derived from the effect of the administered investigational drug and endogenous AT.
2.5 Safety
The safety of rhAT-gamma was assessed in both studies. Hematology, blood biochemistry, urinalysis, coagulation-fibrinolysis test values, bodyweight, blood pressure, pulse rate, and body temperature were assessed at screening, the day before investigational drug administration, during the 3-day administration period, and at the first follow-up visit. Blood pressure, pulse rate, and body temperature were also assessed daily from day 4 onwards. Subjects were also assessed by 12-lead electrocardiography and funduscopy at screening, day 10, and the first follow-up visit. All adverse events (AEs) were coded with Lowest Level Terms of the Japanese version of the International Conference on Harmonization Medical Dictionary for Regulatory Activities Version 12.1 in the first study, and Version 13.1 in the second study.
2.6 Statistical Methods
Assuming that there was no difference between rhAT-gamma and pAT, the 90% confidence interval (CI) for the difference in mean log-transformed Cmax and AUC0–t fell between log(0.80) and log(1.25), with a probability of ≥ 90% and a sample size of eight subjects per group. In the first study, Cmax,day3 and AUC48–t were used as indices. Thus, considering a possible increase in variance, the sample size was set at ten subjects per group.
Sample size for the second study was based on mean and variance of the log-transformed Cmax,day3 and AUC48–t of rhAT-gamma obtained from the first study and the estimated Cmax,day3 and AUC48–t of rhAT-gamma administered at a 1.2-fold dose of the pAT dose. It was estimated that a sample size of 42 subjects (21 subjects per group) would allow for a probability ≥ 80% and that the 90% CI for the difference in mean log-transformed Cmax,day3 and AUC48–t would fall within the bioequivalence criteria (80–125%) [19]. The regulatory criteria for bioequivalence states that blood sampling should be continued until AUC0–t is over 80% of AUC0–∞ (normally more than three times the elimination half-life after tmax) [19].
In the first study, the primary endpoints were Cmax,day3, and AUC48–t, which were calculated from plasma AT activity (with pre-dose adjustment) at the time of administration of rhAT-gamma or pAT. Secondary endpoints were Cmax,day1, Cmax,day2, tmax,day3, AUC0–t, AUC0–∞, elimination half-life (t1/2), mean residence time (MRT), and the elimination rate constant (kel), which were calculated from plasma AT activity (with pre-dose adjustment) at the time of administration of rhAT-gamma or pAT. Values for Cmax,day3 (antithrombin) and AUC48–t (antithrombin) were calculated from plasma AT-antigen concentrations (with pre-dose adjustment). Plasma AT activity, AT antigen concentration, and plasma anti-Xa activity (with pre-dose adjustment) were at the time of administration of rhAT-gamma or pAT.
In the second study, the primary endpoints were Cmax,day3 and AUC48–t, which were calculated from plasma AT activity at the time of administration of rhAT-gamma or pAT. Secondary endpoints were incremental recovery, Cmax,day1, Cmax,day2, tmax,day3, AUC0–t, AUC0–∞, t1/2, MRT, and kel, which were calculated from plasma AT activity at the time of administration of rhAT-gamma or pAT. Values for Cmax,day3 (antithrombin) and AUC48–t (antithrombin) were calculated from plasma AT antigen concentration. Values for Cmax,day3 (anti-Xa) and AUC48–t (anti-Xa) were calculated from plasma anti-Xa activity. Plasma AT activity, AT antigen concentration, and anti-Xa activity were at the time of administration of rhAT-gamma or pAT.
Categorical data were summarized with frequency and percentage, and continuous data were summarized with descriptive statistics, including the number of subjects, mean, standard deviation (SD), minimum, median, and maximum. Pharmacokinetic parameters were analyzed by an analysis of variance (ANOVA) with treatment group as a factor. Parameters, except for time to Cmax,day3 (tmax,day3), were analyzed after log transformation. Based on the guidelines for bioequivalence studies of generic drugs, we used 90% CIs for the evaluation of bioequivalence. The null hypothesis was that mean values in the two groups were equivalent. In addition, a 90% CI for the between-group difference in the mean log-transformed value for each parameter was calculated. If the 90% CIs for differences in mean log-transformed Cmax,day3 and AUC48–t values were between log(0.80) and log(1.25), the two treatments were considered bioequivalent [19].
Adverse events were tabulated for each treatment group. SAS® version 9.1.3 (SAS Inc.; Cary, NC, USA) was used for statistical analyses, and Phoenix® WinNonlin® versions 5.2.1 and 6.1 (Certara Inc., Princeton, NJ, USA) were used for calculation of pharmacokinetic parameters.
3 Results
3.1 Subjects
Subject baseline demographics are summarized in Table 1. All baseline demographic and clinical characteristics were similar in both subject groups in each of the studies.
3.2 Pharmacokinetics and Bioequivalence
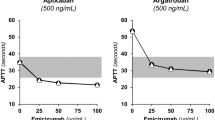
In the first study, plasma AT activity after the third dose (48 h after the first dose) remained lower in the rhAT-gamma than pAT group (Fig. 1; Table 2). Arithmetic mean Cmax,day3 of plasma AT activity, a primary endpoint, was 1.67 in the rhAT-gamma group and 1.77 IU/mL in the pAT group, with no statistically significant difference (p = 0.268). Arithmetic mean AUC48–t, another primary endpoint, was 58.44 IU·h/mL in the rhAT-gamma group and 91.44 IU·h/mL in the pAT group, a difference that was statistically significant (p < 0.001), supporting the increase in dose of rhAT-gamma in the second study. Ratios of plasma AT activity Cmax,day3 and AUC48–t in the rhAT-gamma vs. pAT groups, estimated from differences in log-transformed mean values between these groups were 92.6% (90% CI 82.5, 104.0) and 63.2% (90% CI 56.0, 71.3), respectively.
We adopted AUC48–121, not AUC48–t, to determine the dose to be used in the second study, because t was very different between rhAT-gamma and pAT, and the lower limit of quantification was first observed among subjects at 121 h. Mean AUC48–121 was 58.44 in the rhAT-gamma group and 71.94 IU·h/mL in the pAT group. AUC48–121 for pAT was 1.2-fold higher than that for rhAT-gamma, and was expected to result in comparable Cmax,day3 and AUC48–t. Therefore, the dose of rhAT-gamma for the second study was set to 72 IU/kg.
In the second study, the time course of plasma AT activity was similar for the two products (Fig. 2). Arithmetic mean Cmax,day3 of plasma AT activity was 2.08 in the rhAT-gamma group and 1.98 IU/mL in the pAT group (p = 0.081) (Table 2). Arithmetic mean AUC48–t was 98.71 in the rhAT-gamma group and 98.99 IU·h/mL in the pAT group. Ratios of plasma AT activity Cmax,day3 and AUC48–t in the rhAT-gamma vs. pAT group, calculated from differences in log-transformed mean values between these groups, were 105.7% (90% CI 100.3, 111.3) and 100.5% (90% CI 91.5, 110.4), respectively. Thus, bioequivalence of rhAT-gamma at 72 IU/kg and pAT at 60 IU/kg was confirmed.
The incremental recovery (ratio of Cmax to dose) was 1.69 ± 0.17%/IU/kg (mean ± SD) in the rhAT-gamma group and 1.84 ± 0.20%/IU/kg in the pAT group (Table 3). For other parameters, in the rhAT-gamma and pAT groups, Cmax,day1 (mean ± SD) was 1.21 ± 0.12 and 1.10 ± 0.12 IU/mL, respectively, and the ratio of plasma AT activity Cmax,day1 in the rhAT-gamma vs. pAT group was 110.0% (90% CI 104.2, 116.1); t1/2 after the third dose was 81.82 ± 50.07 and 58.02 ± 18.52 h, respectively; MRT was 128.10 ± 53.96 and 102.40 ± 21.00 h, respectively; and kel was 0.0101 ± 0.0032 and 0.0130 ± 0.0038 L/h, respectively (Table 3). An ANOVA with the treatment group as a factor revealed significant differences for Cmax,day1, t1/2, MRT, and kel (p < 0.05) (Table 3).
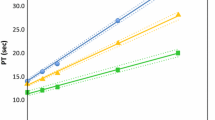
In the first study, mean ± SD Cmax,day3 for plasma AT antigen was 48.4 ± 6.7 mg/dL in the rhAT-gamma group and 47.5 ± 5.4 mg/dL in the pAT group. Mean ± SD AUC48–t for plasma AT antigen in these groups was 2216 ± 199 mg·h/dL and 2662 ± 149 mg·h/dL, respectively (Fig. 3).
In the second study, mean ± SD Cmax,day3 for plasma AT antigen was 63.3 ± 4.6 mg/dL in the rhAT-gamma group and 55.0 ± 5.4 mg/dL in the pAT group, while mean ± SD AUC48–t for plasma AT antigen was 3234 ± 341 mg·h/dL and 3161 ± 438 mg·h/dL, respectively (Fig. 4). Thus, in the first study, levels of plasma AT antigen were lower in the rhAT-gamma than pAT group, whereas in the second study there was no obvious difference between groups.
In the first study, mean ± SD Cmax,day3 for anti-Xa activity was 178 ± 14% in the rhAT-gamma group and 178 ± 14% in the pAT group, while mean ± SD AUC48–121 for anti-Xa activity was 6736 ± 770%·h and 10,280 ± 1060%·h, respectively (Fig. 5). In the second study, mean ± SD Cmax,day3 for anti-Xa activity was 215 ± 20% in the rhAT-gamma group and 203 ± 20% in the pAT group, while mean ± SD AUC48–t for anti-Xa activity was 11,940 ± 1000%·h and 11,600 ± 1280%·h, respectively (Fig. 6). Thus, in the first study, anti-Xa activity was lower in the rhAT-gamma than pAT group, whereas in the second study there was no obvious difference in anti-Xa activity between groups.
3.3 Safety
In the first study, AEs occurred in two (20%) of the ten subjects in the rhAT-gamma group [Electronic Supplementary Material (ESM)]. These events were alanine aminotransferase increased, aspartate aminotransferase (AST) increased, and eosinophil percentage increased in one subject (10%); and erythema in the other subject (10%). All AEs were mild. Adverse drug reactions (ADRs) occurred in one (10%) of the ten subjects in the rhAT-gamma group. These ADRs were alanine aminotransferase increased and AST increased. Both events were mild in severity and resolved without intervention.
In the second study, AEs occurred in 13 (61.9%) of the 21 subjects in the 72 IU/kg rhAT-gamma group, and in four (19.0%) of the 21 subjects in the pAT group (ESM). Adverse events that occurred in more than one subject in the 72 IU/kg rhAT-gamma group were C-reactive protein (CRP) increased in three subjects (14.3%), and pericoronitis, activated partial thromboplastin time prolonged, AST increased, and headache in two subjects (9.5%) each. The CRP elevation was linked to pericoronitis in one case; however, no instance of CRP elevation was linked with elevated hepatic enzyme levels. No AEs were observed in more than one subject in the pAT group. Pericoronitis was rated as moderate in severity, and all other AEs were rated as mild. Adverse drug reactions occurred in five subjects (23.8%) in the rhAT-gamma group and no subjects in the pAT group. The ADRs were activated partial thromboplastin time prolonged in two subjects (9.5%), and alanine aminotransferase increased, CRP increased, and rash in one subject (4.8%) each. Prolonged activated partial thromboplastin time appeared to be associated with the blood collection technique, specimen storage method, reagents, and measuring equipment in the two affected subjects. However, because the changes occurred after study product administration, a causal relationship to the investigational drug could not be ruled out completely. All ADRs were mild in severity.
4 Discussion
The biological activity of rhAT-alfa produced from the milk of transgenic goats is quite different from that of pAT owing to its unusual oligosaccharide structures. Plasma-derived antithrombin does not contain fucose, whereas rhAT-alfa contains fucose. The predominant oligosaccharide structure in rhAT-alfa is of the monosialylated and core-fucosylated biantennary complex type. Additionally, rhAT-alfa contains oligomannose- and hybrid-type oligosaccharides at Asn155. Recombinant human antithrombin alfa has four times the heparin-binding ability of pAT, but its half-life is one ninth that for pAT [15]. Given its short half-life, a continuous 24-h intravenous infusion is required [20, 21].
Recombinant human antithrombin gamma is a new form of recombinant AT that has a similar sugar chain structure to native human AT. Recombinant human antithrombin gamma was developed using POTELLIGENT® technology [16, 17], which relies on a host Chinese hamster ovary cell line that produces fucose-free recombinant proteins. Because of its structural similarity to human AT, rhAT-gamma has pharmacokinetic and biological activities similar to those of native AT.
In the first study, comparing rhAT-gamma (60 IU/kg) and pAT (60 IU/kg), we found that the plasma AT activity of rhAT-gamma was lower than that of pAT and that plasma AT activity was quantifiable for ~ 50% longer in the pAT group. This small reduction in rhAT-gamma activity may be attributable to slight differences in sugar chain structure, such as slightly smaller sialic acid content per AT gamma protein than per pAT protein [22]. These results demonstrated that an rhAT-gamma dose 1.2-fold higher than a pAT dose is expected to be equivalent to pAT. Therefore, 72 IU/kg was considered appropriate as the rhAT-gamma dose in the second study.
The second study showed that rhAT-gamma 72 IU/kg is bioequivalent to pAT 60 IU/kg. Values for Cmax,day3 and AUC48–t were very similar in the 72 IU/kg rhAT-gamma and 60 IU/kg pAT groups. Although the ANOVA revealed significant differences (p < 0.05) in MRT and t1/2, these differences may be attributed to two subjects in the rhAT-gamma group having much longer t1/2 and MRT than other subjects in that group, and this may have skewed mean values upwards. The ANOVA also showed a significant difference between groups (p < 0.05) in Cmax,day1; however, the ratio between groups for Cmax,day1 (rhAT-gamma:pAT; 110%) was very similar to that for Cmax,day3 (105.7%). Thus, the statistically significant differences in these reference parameters are not considered clinically significant.
Levels of plasma AT antigen were lower in the rhAT-gamma group than the pAT group in the first study, but there was no obvious difference between groups in the second study. The reason for this is unknown, although it does seem that pAT contains more plasma AT antigen than rhAT-gamma.
Anti-Xa activity was also lower in the rhAT-gamma group than the pAT group in the first study, but again there was no obvious difference between groups in the second study. Anti-Xa activity is thought to be correlated with plasma AT activity.
Safety analyses indicated that once-daily rhAT-gamma for 3 days did not pose any safety concerns. At a dose of rhAT-gamma 60 IU/kg, AEs were all mild, and the rate of AEs was the same as in the control group (pAT 60 IU/kg). The incidences of AEs and ADRs were both higher in the 72 IU/kg rhAT-gamma group. Eight of the 13 AEs in this group occurred after hospital discharge, and several were likely caused by unrelated events such as dental procedures and alcohol intake. All ADRs were mild in severity.
The findings of these studies should be considered in light of several limitations. The main limitations were the small sample size and lack of generalizability to other populations because the sample comprised healthy adult Japanese men aged 20–45 years. Another limitation is that the investigational drug dose was repeated for only 3 days to measure AUC. However, this differs from treatment duration for patients in actual clinical practice.
5 Conclusions
Overall, the present data support rhAT-gamma as a safe alternative to pAT products. Based on these data, the rhAT-gamma intravenous formulation of 600 IU (ACOALAN® injection 600) was approved in 2015, and the rhAT-gamma intravenous formulation of 1800 IU (ACOALAN® injection 1800) was approved in 2017, by the Ministry of Health, Labour and Welfare in Japan. These formulations are currently being used for the treatment of thrombophilia caused by congenital AT deficiency and disseminated intravascular coagulation.
Data Sharing
Data sets from this study will be made available upon appropriate request.
References
Zhu Y, Cong QW, Liu Y, et al. Antithrombin, an important inhibitor in blood clots. Curr Top Med Chem. 2016;16:666–74.
Damus PS, Hicks M, Rosenberg RD. Anticoagulant action of heparin. Nature. 1973;246:355–7.
Olson ST, Bjork I. Regulation of thrombin activity by antithrombin and heparin. Semin Thromb Hemost. 1994;20:373–409.
Rosenberg RD. Biochemistry of heparin antithrombin interactions, and the physiologic role of this natural anticoagulant mechanism. Am J Med. 1989;87:2s–9s.
Jin L, Abrahams JP, Skinner R, Petitou M, Pike RN, Carrell RW. The anticoagulant activation of antithrombin by heparin. Proc Natl Acad Sci U S A. 1997;94:14683–8.
Carlson TH, Simon TL, Atencio AC. In vivo behavior of human radioiodinated antithrombin III: distribution among three physiologic pools. Blood. 1985;66:13–9.
Rosenberg RD, Damus PS. The purification and mechanism of action of human antithrombin-heparin cofactor. J Biol Chem. 1973;248:6490–505.
Patnaik MM, Moll S. Inherited antithrombin deficiency: a review. Haemophilia. 2008;14:1229–39.
Maclean PS, Tait RC. Hereditary and acquired antithrombin deficiency: epidemiology, pathogenesis and treatment options. Drugs. 2007;67:1429–40.
Kumar R, Chan AK, Dawson JE, Forman-Kay JD, Kahr WH, Williams S. Clinical presentation and molecular basis of congenital antithrombin deficiency in children: a cohort study. Br J Haematol. 2014;166:130–9.
Wada H, Asakura H, Okamoto K, et al. Expert consensus for the treatment of disseminated intravascular coagulation in Japan. Thromb Res. 2010;125:6–11.
MacLennan S, Barbara JA. Risks and side effects of therapy with plasma and plasma fractions. Best Pract Res Clin Haematol. 2006;19:169–89.
Edmunds T, Van Patten SM, Pollock J, et al. Transgenically produced human antithrombin: structural and functional comparison to human plasma-derived antithrombin. Blood. 1998;91:4561–71.
Paidas MJ, Forsyth C, Quere I, Rodger M, Frieling JT, Tait RC. Perioperative and peripartum prevention of venous thromboembolism in patients with hereditary antithrombin deficiency using recombinant antithrombin therapy. Blood Coagul Fibrinolysis. 2014;25:444–50.
Yamada T, Kanda Y, Takayama M, et al. Comparison of biological activities of human antithrombins with high-mannose or complex-type nonfucosylated N-linked oligosaccharides. Glycobiology. 2016;26:482–92.
Matsushita T. Engineered therapeutic antibodies with enhanced effector functions: clinical application of the POTELLIGENT® Technology. Korean J Hematol. 2011;46:148–50.
Yamane-Ohnuki N, Kinoshita S, Inoue-Urakubo M, et al. Establishment of FUT8 knockout Chinese hamster ovary cells: an ideal host cell line for producing completely defucosylated antibodies with enhanced antibody-dependent cellular cytotoxicity. Biotechnol Bioeng. 2004;87:614–22.
Marzo A, Ceppi-Monti N, Giusti A, Abbiati G, Parenti M. Pharmacokinetic behaviour of antithrombin III following intravenous infusion in healthy volunteers. Arzneimittelforschung. 2002;52:187–93.
Partial Revision of the Guidelines for Bioequivalence Studies of Generic Products (PFSB/ELD Notification No. 0229-10 dated February 29, 2012 issued by the Director of Evaluation of Licensing Division, Pharmaceutical and Food Safety Bureau, Ministry of Health, Labour and Welfare). Available from: http://www.nihs.go.jp/drug/be-guide(e)/Generic/GL-E_120229_BE.pdf. Accessed 26 June 2019.
Dickneite G. A comparison of the pharmacokinetics of antithrombin derived from human plasma and from transgenic goats and the prevention of sepsis in an animal model. Biopharm Drug Dispos. 2008;29:356–65.
Dennis JC, Terri LL, Danial EB. Formulary drug reviews: antithrombin (recombinant). Hosp Pharm. 2009;44:758–93.
Endo S, Shimazaki R, Antithrombin Gamma Study Group. An open-label, randomized, phase 3 study of the efficacy and safety of antithrombin gamma in patients with sepsis-induced disseminated intravascular coagulation syndrome. J Intensive Care. 2018;6:75.
Acknowledgements
Recombinant human AT gamma is being developed by Kyowa Kirin Co., Ltd. Susan Cottrell, Ph.D., and Keyra Martinez Dunn, MD, of Edanz Medical Writing provided medical writing support.
Author information
Authors and Affiliations
Contributions
All authors participated in the conception and design of the study. All authors were involved in analysis and interpretation of the data. HF drafted the manuscript. HF and HK provided intellectual content of critical importance. All authors revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Funding
This study was funded by Kyowa Kirin Co., Ltd.
Conflict of interest
Hidetoshi Furuie has received consulting/lecture fees and research funding from Kyowa Kirin Co., Ltd. Hironori Kanda is an employee of Kyowa Kirin Co., Ltd.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board at Osaka Pharmacology Clinical Research Hospital, Osaka, Japan (approval no. 787PC and no. 814PC) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Furuie, H., Kanda, H. Randomized Comparison Study of Novel Recombinant Human Antithrombin Gamma and Plasma-Derived Antithrombin in Healthy Volunteers. Clin Drug Investig 39, 1185–1194 (2019). https://doi.org/10.1007/s40261-019-00847-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-019-00847-9