Abstract
Background and Objectives
Several mechanisms have been proposed for the sudden unexpected death in epilepsy patients, such as cardiac arrhythmias, a decrease in heart rate variability and the use of anti-epileptic drugs (AEDs). Although carbamazepine is commonly used as an AED, the exact working mechanism of this drug as well as its effect on the heart are not completely understood. The aim of this study was to determine whether chronic carbamazepine therapy in patients with focal seizures and impaired awareness has an effect on the electrocardiogram (ECG).
Subjects and Methods
This cross-sectional study included 36 patients with focal seizures and impaired awareness treated for 12–32 months with carbamazepine monotherapy and 38 healthy volunteers. A 5-min modified three-electrode chest lead ECG with lead II configuration was recorded using LabChart 7 ECG software module at 1000-Hz sampling frequency. All data analysis was performed using custom-made Matlab 2015b scripts. ECGs of patients and controls were compared with respect to heart rate, time intervals and measures of short- and long-term variation.
Results
There were no significant differences in heart rate and ECG time intervals between the patient and control groups. Measures on short- and long-term variability also did not show any significant group differences.
Conclusion
Our study shows that chronic use of carbamazepine as monotherapy does not have any significant effects on ECG time intervals or measures of short- and long-term variability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Chronic use of carbamazepine as monotherapy does not influence ECG time intervals or measures of short- and long-term variability. | |
As such, we suggest that in the absence of pre-existing cardiac conditions, carbamazepine monotherapy might be safe from the cardiac point of view. |
1 Introduction
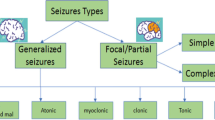
Sudden unexpected death in epilepsy patients (SUDEP) is presently recognized as the most important epilepsy-related mode of death [1, 2]. A sudden unexpected death occurs 24 times more often in patients suffering from epilepsy compared to the general population [3]. The potential pro-arrhythmogenic effect of seizures and/or antiepileptic drugs (AEDs) may be responsible for SUDEP [4,5,6,7,8]. AEDs might not only increase the QT interval in the electrocardiogram (ECG) [8], but might also reduce heart rate (HR) and blood pressure (BP) responses to physiological stressors [2], thereby predisposing to SUDEP.
Carbamazepine is commonly prescribed in patients with focal seizures. Use of carbamazepine has been related to sinus node dysfunction or atrio-ventricular (AV) conduction defects [9]. Carbamazepine also increases the risk of cardio-respiratory arrest [10]. Though the exact mechanism of action of carbamazepine is not completely understood, evidence suggests that carbamazepine might act as a voltage-gated sodium channel blocker [3, 11, 12], thereby blocking these sodium channels in the inactivated state. Consequently, the refractory period of an action potential might last longer [13]. Additionally, carbamazepine might have negative chronotropic and dromotropic effects [14, 15].
Because of the above-mentioned uncertainties in the mechanism of action of carbamazepine, we set out to determine whether chronic carbamazepine monotherapy in patients with focal onset seizures with impaired awareness leads to changes in the inter-ictal ECG. We evaluated resting lead II ECGs in patients on chronic carbamazepine monotherapy and in healthy controls, and compared cardiac parameters like heart rate, ECG time intervals and measures of short- and long-term variability.
2 Subjects and Methods
2.1 Subjects
This cross-sectional study included 36 patients with focal seizures and impaired awareness [16] on chronic carbamazepine monotherapy and 38 healthy volunteers. The study was approved by the Institute Review Board (IRB) of the National Institute of Mental Health and Neuro-Sciences (NIMHANS) in Bangalore, India, and written informed consent was obtained from all subjects.
The inclusion criteria for the patients were: presence of unprovoked focal seizures with impaired awareness; use of carbamazepine as monotherapy for at least 12 months; age between 10 and 50 years. The exclusion criteria were: use of medications other than carbamazepine; co-existing psychiatric illness; history of cardiac disease or any other major medical illnesses; recent surgery; alcohol abuse; or use of a pacemaker. The study and all measurements were performed at the Department of Neurophysiology, NIMHANS.
2.2 Measurements
From all subjects, a 5-min long, modified three-electrode chest lead ECG with lead II configuration was recorded with 1000-Hz sampling frequency using LabChart 7 ECG software module (AD Instruments, Australia). ECGs recordings were performed in the autonomic laboratory, Department of Neurophysiology, NIMHANS under standardized conditions. Subjects were instructed to take their morning dose of AED and have breakfast 2 h prior to the tests, which were performed between 9 and 11 am in a silent room maintained at a temperature of 22–26 °C. Subjects were asked to empty their bowel and bladder before the tests. ECGs from female subjects were recorded in the proliferative phase of the menstrual cycle. All data analysis was performed using a custom-made Matlab 2015b (The MathWorks, Natick, MA, USA) program.
2.3 Data Processing
2.3.1 Preprocessing
The raw ECG signals were filtered with a 50-Hz notch filter, a 0.5–150-Hz second-order bandpass Butterworth filter and a median filter with a window of 500 samples. Additionally, the signal was smoothed using a second-order Savitsky–Golay filter with a window of 50 ms.
2.3.2 ECG Fiducial Points and Intervals
The smoothed signals were used to determine the fiducial points as follows. The isoelectric baseline was defined as the mean voltage between the end of the P-wave and the onset of the QRS complex. Onset of the P-wave, Pstart, was indicated by a peak in the second derivative within a window of 100 ms prior to the corresponding P-peak. The P-peak was defined as the maximum peak within a window of 200 ms prior to Q-onset till Q-onset. The end of the P-wave, Pend, was detected by a peak in the second (or third) derivative within a window starting 10 ms after P-peak and ending 10 ms before the Q-onset. The largest peak in the second derivative of the ECG signal within a window of 100–200 ms before the corresponding R-peak was used to localize the onset of the QRS complex [17]. The R-peak was detected using the Pan–Tompkins algorithm [18]. The S-point was defined as the largest negative peak within a window of 5–50 ms after the R-peak. The J-point was defined as the peak in the second derivative of the ECG signal in a window of 5–90 ms after the corresponding S-peak [19]. If there was no peak in the second derivative, the J-point was defined as the first point of intersection from the baseline with the ECG signal in the same window. T-peak was defined as the largest peak within a window that started at the preceding J-peak and ended at 70% of the RR-interval. A tangent through the point with the maximal slope in the final limb of the T-wave was estimated using a simple numerical differentiation within a 10-ms window. The intersection of this tangent and the baseline was used to detect Tend.
From these fiducial points the RR, PQ, QRS and QT intervals were calculated. The heart-rate-corrected QT interval (QTc) was estimated by means of Bazett’s method [20].
2.3.3 Poincaré Plots and Short- and Long-term Variability
To visualize short-(STV) and long-term variability (LTV) of the ECG intervals, we created Poincaré plots in which interval (n) on the x-axis was plotted versus interval (n + 1) - i.e. the succeeding interval - on the y-axis. Measures of STV and LTV of the various time intervals (I) were calculated according to Eqs. 1 and 2 [21,22,23]:
2.3.4 Statistical Analysis
Independent samples t tests were performed in SPSS 22 to compare the patient group with the control group regarding clinical characteristics, ECG intervals, ECG morphology measures and measures of STV and LTV.
3 Results
The clinical characteristics of patients with focal seizures with impaired awareness and the healthy controls are shown in Table 1. All patients were on carbamazepine controlled-release (CR) formulation monotherapy. The median duration of carbamazepine therapy was 21 months (range 12–32 months) with a median dosage of 650 mg/day (range 300–1000 mg/day). The average seizure frequency of patients at the time of recruitment was 4.3 ± 2.3/month. Of the 36 patients, 29 (81%) were cases of complex partial seizures with secondary generalization. There were no cases of mesial temporal lobe epilepsy in our study. If necessary, patient drug prescription was changed immediately after the ECG recordings.
3.1 ECG Intervals
The results regarding the various ECG time intervals are shown in Table 2. There were no significant differences in any interval between the patient and control groups.
3.2 Poincaré Plots and Short- and Long-term Variability
The left panels of Fig. 1 show 5-min time courses of the PQ-, QT-, QTc- and RR-interval of a healthy control. Poincaré plots based on these time courses are presented in the right panels. The deviation from the line of identity is indicative of the STV, whereas the range along the identity line is indicative of the LTV.
Values for STV, LTV and the ratio thereof of the PQ-, QT-, QTc- and RR-interval were not significantly different between the patient and the control groups (Table 3).
4 Discussion
The results of this study show that chronic carbamazepine monotherapy in patients with focal seizures does neither significantly impact ECG time-intervals nor measures of short-term and long-term variability. Our finding that neither AV-conduction nor depolarization and repolarization are significantly influenced by long-term use of carbamazepine is in accordance with findings both in healthy subjects on carbamazepine for 2–3 weeks [13, 15] as well as in patients with epilepsy who just started with carbamazepine therapy [24]. Since continuous intake of carbamazepine had no noticeable electrophysiological cardiac effect in patients with focal seizures without a past history of cardiovascular disorders, we suggest that in the absence of pre-existing cardiac conditions, carbamazepine monotherapy might be safe from the cardiac point of view.
4.1 Carbamazepine as an Antiepileptic Drug (AED)
Carbamazepine is one of the more frequently prescribed medications in patients with focal seizures. Yet, as carbamazepine is additionally a cardio-active medication, it infrequently initiates sinus dysfunction or atrio-ventricular (AV) conduction defects. It has been suggested that carbamazepine amplifies the risk of cardiorespiratory arrest, especially when associated with ventricular tachycardia and arrhythmia [2, 10]. Several attempts to assess the cardio-toxic effect of carbamazepine have been made, with contradictory findings. A few researchers have shown that there is no relationship between carbamazepine and sudden death unless there is drug toxicity or previous history of coronary disease [25, 26]. Another report assessed QT interval and QTc values in carbamazepine monotherapy seizure cases and reported a non-noteworthy ‘statistical’ relationship between carbamazepine and QTc interval [13]. In addition, studies by Apfelbaum et al. [26] and Kennebäck et al. [27] did not detect any relationship between serum carbamazepine concentration and ECG variables. On the other hand, there have been reports of AV block even with typical or low serum carbamazepine level [28, 29].
4.2 QTc Interval Changes in Epilepsy
Beside heart rate, the QT interval is the most studied ECG parameter in epilepsy. Previous studies of the ECG of patients with epilepsy have focused on the heart rate-corrected QT (QTc) interval [30, 31], commonly calculated using either Bazett’s or Framingham’s formula. The danger of sudden cardiac death increases when QTc changes [30,31,32,33,34,35], though the direction of QTc change is unclear. While some of studies demonstrate that epilepsy itself is related to a prolonged QTc interval [31,32,33], one study contradicted this and instead suggested a relationship between carbamazepine and a short QTc interval [34].
4.3 PR Interval Changes in Epilepsy
Krishnan and Krishnamurthy observed that longer PR intervals were associated with epilepsy [36]. This effect was significant in a subgroup of women and in those with localization-related epilepsy. PR interval prolongation has been associated with an elevated risk of future atrial fibrillation, demand for pacemaker implantation or death [37]. However, in the same study, there was no relationship between poly-therapy and PR interval, which might imply that the PR interval alteration is due to epilepsy itself rather than a medication effect [36]. A longer PR interval in epilepsy might reflect extrinsic or intrinsic cardiac changes, highlighting the need for more definitive cardiac structural imaging studies.
4.4 Sudden Unexpected Death in Epilepsy Patients (SUDEP) and ECG Changes
Untimely mortality is by all accounts increasingly recognized in epilepsy [38]. It has been proposed that ECG changes during ictus can be utilized as biomarkers for SUDEP. The AED- and/or seizure-induced arrhythmias have been linked to SUDEP [39]. In addition, early repolarization patterns (ERP) and severe QTc prolongation are reported to be more prevalent in individuals with refractory epilepsy, but their role in sudden death in these patients has not been established [4].
Mesial temporal lobe epilepsy is specifically associated with sudden death as it is postulated to cause brainstem network disruption leading to breakdown of central autonomic control and hence predisposing to fatal arrhythmias [40]. However, there were no cases of temporal lobe epilepsy in our study.
4.5 Effect of Poly- and Monotherapy AEDs on ECG
Anti-epileptic drug therapy likewise appears to impact ECG variability. Reviews demonstrate a higher risk for SUDEP in patients subjected to poly-AED treatment, with carbamazepine being one of the drugs, when contrasted with mono-AED treatment [8, 41, 42]. Previous case–control studies have proposed that use of carbamazepine and lamotrigine imposes risk of SUDEP [43, 44]. Hesdorffer and partners combined information from three case–control studies and demonstrated that SUDEP risk was not related to monotherapy or polytherapy [45]. In another study, patients on the poly-therapy had the shortest QTc interval with unaffected PR interval [36].
4.6 Heart Rate Variability (HRV) and Epilepsy
We have previously examined heart rate variability (HRV) to understand how epilepsy might lead to sudden death. Studies were performed in patients with different types of epilepsy, namely hot water epilepsy (HWE) patients on carbamazepine treatment [46] and chronic refractory epilepsy on poly-therapy [47]. These studies demonstrated an altered sympatho-vagal balance or dysregulated HRV, characterized by increased sympathetic activity and reduced parasympathetic activity. HRV is a sensitive indicator of autonomic dysregulation and most of the parameters in the time and frequency domain will be diminished in epilepsy patients. It is, however, known that impaired cardiac autonomic function predicts mortality and more specifically sudden death. It is also reported in HRV research that SUDEP occurs mostly in patients with poorly controlled seizures, on polytherapy for more than 3 years, or having frequent generalized tonic–clonic seizures [3, 48]. It is unclear if the observed impaired autonomic regulation and ECG changes in inter-ictal patients (with controlled epilepsy) were caused due to inter-ictal discharges, AEDs, underlying brain pathology or other factors. Further research is necessary especially on the longer-term effects of carbamazepine on ECG changes.
Overall, the above research suggests that resting ECG changes have little value in predicting sudden death in patients with epilepsy without any cardiac co-morbidities. Nevertheless, these issues may influence SUDEP and may comparatively increase the resting heart rate. Relatively altered QT and PR interval with seizures might also indicate neurally-mediated cardiac excitability that might contribute to SUDEP. However, little is known about ECG changes that occur at therapeutic AED doses. The present study shows that epileptiform activity and carbamazepine are not associated with ECG-wave alterations.
4.7 Limitations
Some of the limitations of this study must be taken in consideration when interpreting the results. In this study, only ECG lead II was recorded. Although lead II is accurate for detecting arrhythmias, the 12-lead ECG remains the most reliable and information-rich measure [49]. Also, though lead II is appropriate for QT analysis, it remains unclear whether lead II gives reliable outcomes for other ECG parameters. For further research, it is recommended to use more than one ECG lead to obtain information about the cardiac axis. Based on the cardiac axis, more reliable algorithms to determine fiducial points should be developed. Analysis of prolonged 12-lead ECG might unravel the true relationship between carbamazepine monotherapy and cardiac rhythm alterations, if any.
5 Conclusion
Our study shows that the use of carbamazepine for 12–32 months as monotherapy in patients with focal seizures does not have any detectable effect on cardiac AV-conduction, depolarization and repolarization nor on measures of short-term and long-term variation of time-intervals of the ECG. As such, carbamazepine may be safely used in the absence of pre-existing cardiac disease, but other non-cardiac events like cutaneous drug reactions and hepatitis, for instance, could still occur. Further research on whether carbamazepine acts as a contributor in SUDEP is required.
References
Jehi L, Najm IM. Sudden unexpected death in epilepsy: impact, mechanisms, and prevention. Cleve Clin J Med. 2008;75(Suppl 2):S66–70.
Tomson T, Nashef L, Ryvlin P. Sudden unexpected death in epilepsy: current knowledge and future directions. Lancet Neurol. 2008;7:1021–31.
Walczak TS, Leppik IE, D’Amelio M, Rarick J, So E, Ahman P, et al. Incidence and risk factors in sudden unexpected death in epilepsy: a prospective cohort study. Neurology. 2001;56:519–25.
Lamberts RJ, Blom MT, Novy J, Belluzzo M, Seldenrijk A, Penninx BW, et al. Increased prevalence of ECG markers for sudden cardiac arrest in refractory epilepsy. J Neurol Neurosurg Psychiatry. 2015;86:309–13.
Rugg-Gunn FJ, Simister RJ, Squirrell M, Holdright DR, Duncan PJS. Cardiac arrhythmias in focal epilepsy: a prospective long-term study. Lancet. 2004;364:2212–9.
Leung H, Kwan P, Elger CE. Finding the missing link between ictal bradyarrhythmia, ictal asystole, and sudden unexpected death in epilepsy. Epilepsy Behav. 2006;9:19–30.
Velagapudi P, Turagam M, Laurence T, Kocheril A. Cardiac arrhythmias and sudden unexpected death in epilepsy (SUDEP). Pacing Clin Electrophysiol. 2011;35:1–8.
Hesdorffer DC, Tomson T. Sudden unexpected death in epilepsy. CNS Drugs. 2013;27:113–9.
Takayanagi K, Hisauchi I, Watanabe J, Maekawa Y, Fujito T, Sakai Y, et al. Carbamazepine-induced sinus node dysfunction and atrioventricular block in elderly women. Jpn Heart J. 1998;39(4):469–79.
Pedley TA, Hauser WA. Sudden death in epilepsy: a wake-up call for management. Lancet. 2002;359:1790–1.
Neu HC. Diagnosis and treatment: drugs five years later. Amoxicillin. Ann Intern Med. 1979;90:356–60.
Kito M, Maehara M, Watanabe K. Antiepileptic drugs-calcium current interaction in cultured human neuroblastoma cells. Seizure. 1994;3:141–9.
Amin OSM, Shwanni SS, Noori SF, Hasan AM. Carbamazepine and the QTc interval: any association? Neurology Asia. 2010;15:119–23.
Kennebäck G, Bergfeldt L, Vallin H, Tomson T, Edhag O. Electrophysiologic effects and clinical hazards of carbamazepine treatment for neurologic disorders in patients with abnormalities of the cardiac conduction system. Am Heart J. 1991;121:1421–9.
Kennebäck G, Bergfeldt L, Tomson T. Electrophysiological evaluation of the sodium-channel blocker carbamazepine in healthy human subjects. Cardiovasc Drugs Ther. 1995;9:709–14.
Fisher RS, Cross JH, French JA, Higurashi N, Hirsch E, Jansen FE, et al. Operational classification of seizure types by the International League Against Epilepsy: position Paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58(4):522–30.
Shin HS, Lee C, Lee M. Principal point discrimination of electrocardiogram for automatic diagnosis. In: Kim SI, Suh TS, editors. IFMBE proceedings world congress on medical physics and biomedical engineering. Berlin: Springer; 2006. p. 1087–90.
Pan J, Tompkins WJ. A real-time QRS detection Algorithm. IEEE Trans Biomed Eng. 1985;32:230–6.
Clifford G. ECG statistics, noise, artifacts, and missing data. Adv Methods Tools ECG Data Anal. 2006;2006:55–99.
Bazett HC. An analysis of the time-relations of electrocardiograms. Heart. 1920;7:353–70.
Brennan M, Palaniswami M, Kamen P. Do existing measures of Poincare plot geometry reflect nonlinear features of heart rate variability? IEEE Trans Biomed Eng. 2001;48:1342–7.
Golińska AK. Poincaré plots in analysis of selected biomedical signals. Stud Logic Gramm Rhetor. 2013;35(1):117–27.
Piskorski J, Guzik P. Geometry of the Poincaré plot of RR intervals and its asymmetry in healthy adults. Physiol Meas. 2007;28:287–300.
Saetre E, Abdelnoor M, Amlie JP, Tossebro M, Perucca E, Taubøll E, et al. Cardiac function and antiepileptic drug treatment in the elderly: a comparison between lamotrigine and sustained-release carbamazepine. Epilepsia. 2009;50:1841–9.
Matteoli S, Trappolini M, Curione M, Fanari F, Borgia MC, Puletti M. Effects of carbamazepine on heart conduction in young patients: a serial study using ambulatory ECG. G Ital Cardiol. 1994;24:391–7.
Apfelbaum JD, Caravati EM, Kerns WP, Bossart PJ, Larsen G. Cardiovascular effects of carbamazepine toxicity. Ann Emerg Med. 1995;25:631–5.
Kennebäck G, Bergfeldt L, Tomson T, Spina E, Edhag O. Carbamazepine induced bradycardia—a problem in general or only in susceptible patients? A 24-h long-term electrocardiogram study. Epilepsy Res. 1992;13:141–5.
Celik IE, Akyel A, Colgecen M, Ozeke O. A rare cause of 2:1 atrioventricular block: carbamazepine. Am J Emerg Med. 2015;33:10.
Ide A, Kamijo Y. Intermittent complete atrioventricular block after long term low-dose carbamazepine therapy with a serum concentration less than the therapeutic level. Intern Med. 2007;46:627–9.
Feldman AE, Gidal BE. QTc prolongation by antiepileptic drugs and the risk of torsade de pointes in patients with epilepsy. Epilepsy Behav. 2013;26:421–6.
Zhang Y, Post WS, Blasco-Colmenares E, Dalal D, Tomaselli GF, Guallar E. Electrocardiographic QT interval and mortality. Epidemiology. 2011;22:660–70.
Dogan EAA, Dogan U, Yildiz GU, Akilli H, Genc E, Genc BO, et al. Evaluation of cardiac repolarization indices in well-controlled partial epilepsy: 12-lead ECG findings. Epilepsy Res. 2010;90:157–63.
Drake ME, Reider CR, Kay A. Electrocardiography in epilepsy patients without cardiac symptoms. Seizure. 1993;2:63–5.
Teh HS, Tan HJ, Loo CY, Raymond AA. Short QTc in epilepsy patients without cardiac symptoms. Med J Malaysia. 2007;62:104–8.
Surges R, Scott CA, Walker MC. Enhanced QT shortening and persistent tachycardia after generalized seizures. Neurology. 2010;74:421–6.
Krishnan V, Krishnamurthy KB. Interictal 12-lead electrocardiography in patients with epilepsy. Epilepsy Behav. 2013;29:240–6.
Cheng S, Keyes MJ, Larson MG, McCabe EL, Newton-Cheh C, Levy D, et al. Long-term outcomes in individuals with prolonged PR interval or first-degree atrioventricular block. JAMA. 2009;301:2571–7.
Pinto KGFD, Scorza FA, Arida RM, Cavalheiro EA, Martins LD, Machado HR, et al. Sudden unexpected death in an adolescent with epilepsy: all roads lead to the heart? Cardiol J. 2011;18:194–6.
Rheims S, Cucherat M, Arzimanoglou A, Ryvlin P. Greater response to placebo in children than in adults: a systematic review and meta-analysis in drug-resistant partial epilepsy. PLoS Med. 2008;5(8):e166.
Mueller G, Bateman M, Laxer KD. Evidence for brainstem network disruption in temporal lobe epilepsy and sudden unexplained death in epilepsy. Neuroimage Clin. 2014;5:208–16.
Pack AM. SUDEP: what are the risk factors? Do seizures or antiepileptic drugs contribute to an increased risk? Epilepsy Curr. 2012;12:131–2.
Ryvlin P, Montavont A, Kahane P. Sudden unexpected death in epilepsy: from mechanisms to prevention. Curr Opin Neurol. 2006;19:194–9.
Hesdorffer DC, Tomson T, Benn E, Sander JW, Nilsson L, Langan Y, et al. Combined analysis of risk factors for SUDEP. Epilepsia. 2011;52:1150–9.
Ryu HU, Hong JP, Han SH, Choi EJ, Song JH, Lee SA, et al. Seizure frequencies and number of anti-epileptic drugs as risk factors for sudden unexpected death in epilepsy. J Korean Med Sci. 2015;30(6):788–92.
Hesdorffer DC, Tomson T, Benn E, Sander JW, Nilsson L, Langan Y, et al. Do antiepileptic drugs or generalized tonic-clonic seizure frequency increase SUDEP risk? A combined analysis. Epilepsia. 2012;53:249–52.
Meghana A, Sathyaprabha TN, Sinha S, Satishchandra P. Cardiac autonomic dysfunction in drug naïve hot water epilepsy. Seizure. 2012;21:706–10.
Sathyaprabha TN, Satishchandra P, Netravathi K, Sinha S, Thennarasu K, Raju TR. Cardiac autonomic dysfunctions in chronic refractory epilepsy. Epilepsy Res. 2006;72:49–56.
Evrengül H, Tanriverdi H, Dursunoglu D, Kaftan A, Kuru O, Unlu U, Kilic M. Time and frequency domain analyses of heart rate variability in patients with epilepsy. Epilepsy Res. 2005;63(2–3):131–9.
Davey PP. Which lead for Q–T interval measurements? Cardiology. 2000;94:159–64.
Acknowledgements
We are grateful to the study volunteers for their participation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding.
Conflicts of interest
Talakad N Sathyaprabha: No conflicts of interest. Laura A.M. Koot: No conflicts of interest. Ben H.M. Hermans: No conflicts of interest. Meghana Adoor: No conflicts of interest. Sanjib Sinha: No conflicts of interest. Boris W. Kramer: No conflicts of interest. Trichur R Raju: No conflicts of interest. Parthasarathy Satishchandra: No conflicts of interest. Tammo Delhaas: No conflicts of interest.
Ethics approval
The study was conducted in the Department of Neurophysiology, NIMHANS, Bangalore, India with approval from NIMHANS Ethics Committee.
Informed consent
Written informed consent obtained from all patients.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sathyaprabha, T.N., Koot, L.A.M., Hermans, B.H.M. et al. Effects of Chronic Carbamazepine Treatment on the ECG in Patients with Focal Seizures. Clin Drug Investig 38, 845–851 (2018). https://doi.org/10.1007/s40261-018-0677-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-018-0677-6