Abstract
Background and Objective
Doravirine is a novel, next-generation, non-nucleoside reverse transcriptase inhibitor in development for the treatment of human immunodeficiency virus-1 infection in combination with other antiretrovirals. Doravirine is a substrate for cytochrome P450 (CYP) 3A and P-glycoprotein. Rifampin (rifampicin) is used for treating tuberculosis in patients who are co-infected with human immunodeficiency virus. Rifampin demonstrates organic anion-transporting polypeptide 1B1 and P-glycoprotein inhibition after single-dose administration and CYP3A and P-glycoprotein induction after multiple-dose administration. The objective of this study was to evaluate the effects of co-administration of single and multiple doses of rifampin on doravirine pharmacokinetics.
Methods
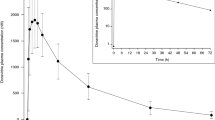
In period 1 of this open-label, two-period, fixed-sequence study in healthy adults, subjects received single-dose doravirine 100 mg; blood samples for measuring plasma concentration were collected pre-dose and up to 72 h post-dose. In period 2, following a 7-day washout, subjects received doravirine 100 mg and rifampin 600 mg on day 1, rifampin 600 mg daily on days 4–18, with doravirine 100 mg co-administered on day 17; blood samples were collected pre-dose and up to 72 h post-dose on day 1 and up to 48 h post-dose on day 17. Safety assessments included adverse events, physical examinations, vital signs, and clinical laboratory measurements.
Results
Ten subjects completed the study. Doravirine area under the concentration-time curve from time zero extrapolated to infinity and plasma concentration at 24 h post-dose were comparable in the presence and absence of single-dose rifampin [geometric mean ratios (90% confidence intervals)] of 0.91 (0.78–1.06) and 0.90 (0.80–1.01), respectively. Doravirine maximum plasma concentration increased when co-administered with single-dose rifampin vs. doravirine alone, geometric mean ratio (90% confidence interval): 1.40 (1.21–1.63). Reductions in doravirine geometric mean ratios (90% confidence interval), area under the concentration-time curve from time zero extrapolated to infinity: 0.12 (0.10–0.15), plasma concentration at 24 h post-dose: 0.03 (0.02–0.04), maximum plasma concentration: 0.43 (0.35–0.52), and apparent terminal half-life were observed when co-administered with multiple-dose rifampin vs. doravirine administered alone. Doravirine was well tolerated. Adverse events were mild and resolved by study completion.
Conclusions
Doravirine co-administration with single-dose rifampin indicated that inhibition of organic anion-transporting polypeptide uptake transporters and P-glycoprotein has little impact on doravirine pharmacokinetics. Long-term co-administration of rifampin or other strong CYP3A inducers with doravirine will likely reduce its efficacy.


Similar content being viewed by others
References
World Health Organization. Fact sheet no. 360: HIV/AIDS. 2016. Available from: http://www.who.int/mediacentre/factsheets/fs360/en/. Accessed 28 July 2016.
National Institutes of Health. HIV/AIDS treatment. 2015. Available from: https://www.niaid.nih.gov/diseases-conditions/hiv-treatment. Accessed 10 Oct 2016.
National Institutes of Health. HIV/AIDS. 2015. Available from: https://www.niaid.nih.gov/diseases-conditions/hivaids. Accessed 10 Oct 2016.
Liu E, Makubi A, Drain P, et al. Tuberculosis incidence rate and risk factors among HIV-infected adults with access to antiretroviral therapy. AIDS. 2015;29:1391–9.
Wasserman S, Meintjes G. The diagnosis, management and prevention of HIV-associated tuberculosis. S Afr Med J. 2014;104:886–93.
World Health Organization. Fact sheet no. 104: tuberculosis. 2015. Available from: http://www.who.int/mediacentre/factsheets/fs104/en/. Accessed 7 Oct 2016.
Kaplan JE, Benson C, Holmes KK, et al. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep. 2009;58:1–207.
Department of Health and Human Services. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents. 2015. Available from: https://aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf. Accessed 8 Mar 2016.
Mofenson LM, Brady MT, Danner SP, et al. Guidelines for the prevention and treatment of opportunistic infections among HIV-exposed and HIV-infected children: recommendations from CDC, the National Institutes of Health, the HIV Medicine Association of the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the American Academy of Pediatrics. MMWR Recomm Rep. 2009;58:1–166.
Xu Y, Zhou Y, Hayashi M, et al. Simulation of clinical drug-drug interactions from hepatocyte CYP3A4 induction data and its potential utility in trial designs. Drug Metab Dispos. 2011;39:1139–48.
Anderson MS, Gilmartin J, Cilissen C, et al. Safety, tolerability and pharmacokinetics of doravirine, a novel HIV non-nucleoside reverse transcriptase inhibitor, after single and multiple doses in healthy subjects. Antivir Ther. 2015;20:397–405.
Feng M, Wang D, Grobler JA, et al. In vitro resistance selection with doravirine (MK-1439), a novel nonnucleoside reverse transcriptase inhibitor with distinct mutation development pathways. Antimicrob Agents Chemother. 2015;59:590–8.
Gatell JM, Morales-Ramirez JO, Hagins DP, et al. Forty-eight-week efficacy and safety and early CNS tolerability of doravirine (MK-1439), a novel NNRTI, with TDF/FTC in ART-naive HIV-positive patients. J Int AIDS Soc. 2014;17:19532.
Sanchez RI, Fillgrove K, Hafey M, et al. In vitro evaluation of doravirine potential for pharmacokinetic drug interactions. Drug Metab Rev. 2016;48:73.
Khalilieh S, Yee KL, Sanchez RI, et al. Results of a doravirine-atorvastatin drug-drug interaction study. Antimicrob Agents Chemother. 2017;61(2):pii: e01364–16.
Anderson MS, Kaufman D, Castronuovo P, et al. Effect of doravirine (MK-1439) on the pharmacokinetics of an oral contraceptive (ethinyl estradiol [EE] and levonorgestrel [LNG]). In: Abstract presented at the International Workshop on HIV and Women, Boston (MA); 20–21 Feb 2016.
Sanchez RI, Khalilieh S, Yee KL, et al. Co-administration of doravirine with metformin does not have a clinically meaningful effect on metformin pharmacokinetics. In: Abstract presented at the American Association of Pharmaceutical Scientists, Denver (CO); 13–17 Nov 2016.
Anderson MS, Khalilieh S, Yee KL, et al. A two-way steady-state pharmacokinetic interaction study of doravirine (MK-1439) and dolutegravir. Clin Pharmacokinet. 2016. doi:10.1007/s40262-016-0458-4 .
Reitman ML, Chu X, Cai X, et al. Rifampin’s acute inhibitory and chronic inductive drug interactions: experimental and model-based approaches to drug-drug interaction trial design. Clin Pharmacol Ther. 2011;89:234–42.
Vavricka SR, Van Montfoort J, Ha HR, et al. Interactions of rifamycin SV and rifampicin with organic anion uptake systems of human liver. Hepatology. 2002;36:164–72.
Niemi M, Backman JT, Fromm MF, et al. Pharmacokinetic interactions with rifampicin: clinical relevance. Clin Pharmacokinet. 2003;42:819–50.
Schürmann D, Sobotha C, Gilmartin J, et al. A randomized, double-blind, placebo-controlled, short-term monotherapy study of doravirine in treatment-naive HIV-infected individuals. AIDS. 2016;30:57–63.
Frymoyer A, Shugarts S, Browne M, et al. Effect of single-dose rifampin on the pharmacokinetics of warfarin in healthy volunteers. Clin Pharmacol Ther. 2010;88:540–7.
Ndanusa BU, Mustapha A, Abdu-Aguye I. The effect of single doses of rifampicin on the pharmacokinetics of oral nifedipine. J Pharm Biomed Anal. 1997;15:1571–5.
Anderson MS, Gilmartin J, Mitselos A, et al. Effect of ritonavir (RTV) and tenofovir (TDF) on the pharmacokinetics (PK) of MK-1439, a novel HIV-1 non-nucleoside reverse transcriptase inhibitor (NNRTI). In: Abstract no. H-1462 presented at the Interscience Conference on Antimicrobial Agents and Chemotherapy: Denver (CO); 10–13 Sept 2013.
Anderson MS, Chung C, Tetteh E, et al. Effect of ketoconazole on the pharmacokinetics of doravirine (MK-1439), a novel non-nucleoside reverse transcriptase inhibitor for the treatment of HIV-1 infection. In: Abstract presented at the International Workshop on Clinical Pharmacology of HIV and Hepatitis Therapy, Washington (DC); 19–21 April 2015.
Gatell JM, Raffi F, Plettenberg A, et al. Efficacy and safety of doravirine 100 mg QD vs efavirenz 600 mg QD with TDF/FTC in ART-naive HIV-infected patients: week 24 results. In: 8th International AIDS Society Conference on HIV Pathogenesis, Treatment, and Prevention. TUAB0104, Vancouver; 19–22 July 2015.
Yee KL, Chatterjee M, Dockendorf MF, et al. Pharmacokinetics (PK) of doravirine and exposure-response analysis: efficacy and safety implications. In: Poster abstract no. H-647b presented at the Interscience Conference on Antimicrobial Agents and Chemotherapy: Washington, DC; 5–9 Sept 2014.
US Food and Drug Administration. Sustiva® (efavirenz): full prescribing information. 2009. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020972s033,021360s021lbl.pdf. Accessed 15 Mar 2016.
US Food and Drug Administration. Viramune® (nevirapine): full prescribing information. 2010. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/020933s022,020636s032lbl.pdf. Accessed 15 Mar 2016.
US Food and Drug Administration. Edurant® (rilpivirine): full prescribing information. 2011. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/202022s000lbl.pdf. Accessed 15 Mar 2016.
US Food and Drug Administration. Rescriptor® (delaviridine mesylate): full prescribing information. 2012. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/020705s018lbl.pdf. Accessed 15 Mar 2016.
Gorski JC, Jones DR, Haehner-Daniels BD, et al. The contribution of intestinal and hepatic CYP3A to the interaction between midazolam and clarithromycin. Clin Pharmacol Ther. 1998;64:133–43.
Krecic-Shepard ME, Barnas CR, Slimko J, et al. Gender-specific effects on verapamil pharmacokinetics and pharmacodynamics in humans. J Clin Pharmacol. 2000;40:219–30.
Conte JE, Golden JA, Kipps JE, et al. Effect of sex and AIDS status on the plasma and intrapulmonary pharmacokinetics of rifampicin. Clin Pharmacokinet. 2004;43:395–404.
Behm M, Yee KL, Fan L, Fackler P. Effect of gender and age on the relative bioavailability of doravirine: results of a phase 1 trial in healthy subjects. Antivir Ther. 2017. doi:10.3851/IMP3142
Sanchez RI, Fillgrove K, Hafey M, et al. In vitro evaluation of doravirine potential for pharmacokinetic drug interactions. In: Abstract presented at the 20th North American Meeting of the International Society for the Study of Xenobiotics: Orlando (FL); 18–22 Oct 2015.
Acknowledgements
Medical writing assistance was provided by Carole Evans, PhD, of Complete Medical Communications, Hackensack, NJ, USA. This assistance was funded by Merck & Co., Inc., Kenilworth, NJ, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research was funded by Merck & Co., Inc., Kenilworth, NJ, USA.
Conflict of interest
Ka L. Yee, Sauzanne G. Khalilieh, Rosa I. Sanchez, Rachael Liu, Matt S. Anderson, and Joan R. Butterton are current or former employees of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, and may own stock and/or stock options. Helen Manthos, Timothy Judge, and John Brejda have no conflicts of interest to disclose.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
All subjects gave written informed consent to participate in the trials.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yee, K.L., Khalilieh, S.G., Sanchez, R.I. et al. The Effect of Single and Multiple Doses of Rifampin on the Pharmacokinetics of Doravirine in Healthy Subjects. Clin Drug Investig 37, 659–667 (2017). https://doi.org/10.1007/s40261-017-0513-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-017-0513-4