Abstract
The article offers a comparative analysis of the influence of cost-effectiveness thresholds in the decision-making processes in financing policies, coverage, and price regulation of health technologies in nine countries. We investigated whether countries used cost-effectiveness thresholds for public health policy decision making and found that few countries have adopted the cost-effectiveness threshold as an official criterion for financing, reimbursement, or pricing. However, in countries where it is applied, such as Thailand, the results have been very favorable in terms of minimizing health technology prices and ensuring the financial sustainability of the health system. Although the cost-effectiveness threshold has opportunities for improvement, particularly in certain institutional contexts and with adequate participation of the different strategic actors in the formulation of public policy, its potential use and added value are significant in various aspects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Although several countries have estimated the cost-effectiveness threshold, Thailand is the only country that has made its use explicit, obtaining favorable results to date. |
Cost-effectiveness criteria help to strengthen the technical capabilities of the governing bodies of the health systems by providing criteria that guide national/regional health budget decisions. |
Implementing a cost-effectiveness threshold requires the participation of multiple stakeholders, including patients and civil society. |
1 Introduction
To determine the extent to which a health system is willing to incur additional costs to obtain the health benefits promised by a health technology, it is necessary to establish a decision rule aimed at maximizing health outcomes, given the country’s budgetary restrictions facing and the growing demand for more and better technologies available to citizens. One of the most recognized measures is known as the cost-effectiveness threshold (CET).
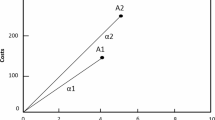
In general, it has been proposed that the decision rule should compare the incremental cost-effectiveness ratio with a CET [1, 2]. This threshold can be defined from two perspectives: (1) on the supply side, it is defined as the opportunity cost of allocating resources to a given technology, in terms of the health benefits displaced or not materialized because of the unavailability of resources to finance other alternatives competing for the same budget [1,2,3,4] and (2) on the demand side, it is established as the rate at which individuals would be willing to forego other forms of consumption to improve health, i.e., it represents their willingness to pay for health [4,5,6,7].
Lacking estimates with real-world evidence,Footnote 1 part of the literature began to use a CET between one and three times the gross domestic product per capita (GDPpc). However, as pointed out by the World Health Organization and other researchers [8,9,10,11,12,13], using this type of threshold as a criterion for decisions on coverage or financing of health technologies has important limitations: (1) it is not an appropriate interpretation of the values proposed by the World Health Organization, which in no case suggested them as guidance for funding and coverage decisions; (2) they are not a generic recommendation for any chosen health outcome; (3) using a threshold based on gross domestic product, which does not account for the budgetary restrictions of the health system, can lead to unsustainable increases in health spending in the medium and long term; and (4) these CETs are defined discretionarily by health authorities, often without a theoretical or empirical basis to support them.
As a result, a decision rule based on GDPpc could increase health inequalities and, ultimately, reduce population health [14]. This is because each country has a multifactorial context where the opportunity costs associated with health resources have a specific and exclusively local logic. Consequently, offering a new cost-effective technology, under this criterion, could risk improving the health outcomes of a few, resulting in a net loss in health when considering the population.
Given this, it is particularly important that when establishing a threshold for public funding decisions, a systematic process is developed to estimate a threshold that adequately reflects both the opportunity costs of financing new technologies and the improvement in informed health decision making. Additionally, a health technology assessment (HTA) has been considered an input for value-based pricing, which would define scenarios in which technology is or is not cost effective for the health system.
In this framework, we investigated the use of CETs in different countries with a tradition of using HTAs, to review the scope of this tool in public policy decision making. Recent works have tried to compile the methodological advances for estimating the CET [15, 16]; however, its implication and strength in health policy have not been reviewed. The article consists of three sections, in addition to this introduction. The second section presents the international review methodology. The third section presents the results. The final section provides the conclusions and discussion of the research work.
2 Methods
This international review aimed to identify how the CET is used in different countries or health contexts and to gather information on how policymakers utilize it for making decisions on financing, coverage, price regulation, and other public policy processes. This identification and the synthesis of relevant information in selected countries were conducted through a narrative review.
Three criteria were used to select the countries. First, we considered the information contained in four literature reviews on HTAs in the world [12, 13, 16, 17], which identified the health systems with significant experience in HTAs. Second, the information in these articles was validated with a preliminary review and the knowledge of the authors of this research. Finally, countries with different levels of development and income and from various continents were considered. This selection process resulted in the inclusion of Australia, Colombia, England, Malaysia, the Netherlands, Spain, South Africa, Thailand, and the USA. While we considered documents from other countries (Brazil, Canada, Chile, Egypt, Ireland, and Saudi Arabia), there was no information available from a country-specific CET based on a supply-side empirical exercise,Footnote 2 apart from estimates derived from cross-country studies [18,19,20]. For the selected nations, we discussed with thematic experts from these countries during international academic events to determine whether CETs were used for policy decisions, to complement our literature findings.
The review consulted multiple databases and sources, including Google Scholar, PubMed, Jstor, Science Direct, Research Papers in Economics (REPEC) databases, official pages of the ministries of HTA agencies of each selected country, information from the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) ROAD MAPS, the International Network of Agencies for Health Technology Assessment (INAHTA), the Red de Evaluación de Evaluación de Tecnologías en Salud de las Américas (REDETSA), the Inter-American Development Bank (IADB), the Pan American Health Organization (PAHO), and the European Observatory of Health Systems and Policies, accompanied by a general Google search. The key search terms employed (in addition to the names of countries of analysis) were: (1) cost-effectiveness threshold; (2) willingness-to-pay threshold; and (3) health opportunity cost. The search encompassed research articles, academic publications, and research reports, with no language restrictions. The publication range for determining a CET was primarily from 2010 to 2022. No exclusion criteria based on publication years were applied for contextual publications.
Paper screening was performed by five authors and a research assistant, followed by a review of the inclusion of papers by two other authors. With the identified information, a screening process was conducted employing a matrix, to identify the relevant data for the questions posed for each country. Two authors reviewed this data collection process. The Electronic Supplementary Material presents the 86 documents that were reviewed.
3 Results
Table 1 presents a summary of the results of the countries examined, indicating whether they have a CET, whether it was estimated from empirical research, whether it is used officially, and its value as a percentage of GDPpc.
Table 1 shows that the processes of defining, designing, formulating, implementing, and evaluating public health policies often do not explicitly involve the use of CETs. Moreover, in most settings, authorities have wide discretion in decision making, regardless of whether an estimated CET value exists. According to Paris and Belloni, countries that do not use an HTA and a CET are more likely to accept high prices under similar circumstances to countries that do incorporate HTAs in their policies such as those mentioned above [31].
As observed, there are no substantial differences between CET thresholds, concerning their relative magnitude as a function of GDPpc. Several thresholds are below one GDPpc, the minimum suggested by the World Health Organization, and many of them are estimated with real-world data evidence [13, 17, 18, 20, 22, 26, 28, 32,33,34,35,36,37]. However, when reviewing the implication of the CET as an element of official decision making by the government, the only countries that meet such criteria are England and Thailand.
England uses a CET conceived through a political process rather than a statistical approach using real-world evidence. With recent method updates by National Institute for Health and Care Excellence, some researchers have criticized that the range between £20,000 and £30,000 per QALY may be excessively high compared with several empirical investigations [38], which suggests a CET value less than or equal to £13,000 per QALY [36, 39].
Thailand has had several official CETs, the first was in 2008 with a monetary value of THB 100,000 per QALY, 2 years later, in 2010 it increased to THB 120,000 per QALY, and in 2013 it was defined at THB 160,000 per QALY. According to Isaranuwatchai et al. [40], only the latter value was partially supported by empirical evidence from Thavorncharoensap et al. [28]. However, since then, there has been constant pressure from different stakeholders, especially the industry, to increase its value [41].
Colombia is a unique case, given that the estimate was made officially by the Colombian Agency for HTAs (IETS for its acronym in Spanish) and financed by the Ministry of Finance and Public Credit, but to date, it has not yet been regulated by the Ministry of Health and Social Protection [42].Footnote 3 In the second version of the IETS health economic evaluation manual, the percentage of estimated GDPpc by Espinosa et al. is proposed as the CET for evaluating whether a technology is highly cost effective in Colombia’s healthcare system [22].
Spain, South Africa, and the USA, although they have CETs based on real-world evidence, they are not officially used by their respective ministries or secretaries of health for making decisions on health technology investments with public resources. In Spain, it is not officially used, but the reports of the network of HTA agencies of the Spanish Ministry of Health consider the Vallejo-Torres et al.’s threshold as a reference point [13, 43]. Authorities must balance therapeutic value, effectiveness, safety, price, impact on the budget and severity of the disease, and a set of social values in their decision-making processes and public policies [41, 44,45,46]. In the case of Malaysia, Australia, and the Netherlands, and after consulting with local experts in these countries, CETs are currently part of academic exercises, rather than official tools for determining the scope of their health benefit plans.
4 Discussion
Utilizing the CET, ideally estimated from empirical research, as one of the criteria for financing new health technologies offers several advantages: (1) it provides a clear decision rule for both the government and various actors in the health system; (2) it brings transparency to technical-scientific processes such as cost-effectiveness analyses applied to a specific country; (3) government decisions become predictable and stable for all strategic actors; and (4) it strengthens the design, updating, and expansion of publicly funded health benefit plans. Likewise, some authors such as Yanovskiy et al. have demonstrated through an ethical analysis the relevance of having CETs to improve the welfare of the entire population [47].
However, applying CETs also has particular challenges that can be problematic in health systems: (1) it can create an incentive for the industry to set prices of health technologies, at the threshold value, disregarding other factors and potential negative consequences, particularly in determining coverage, and future prices of technologies [9, 11, 48]; (2) research methods on the theoretical conceptualization of CETs and empirical methods for its estimation are still evolving; and (3) including other criteria in addition to CETs presents the risk of double-counting cost-effectiveness perspectives (and all that this implies) depending on the other criteria used.
Nonetheless, there are solutions to these disadvantages, and the international literature is progressing rapidly. First, to define in a systematic, rigorous, and participatory manner the criteria for analyzing the financing of health technologies with public resources. At this point, the inclusion of patients and academia can provide a broad perspective of the criteria, ensuring they address different dimensions without an overlap. Second, to incorporate equity considerations in cost-effectiveness analyses, such as, for example, distributive approaches. Several alternatives of extended cost-effectiveness analyses have been introduced in the academic literature [49,50,51].
Successful applications of CETs in public health policy include the experience of Thailand, where economic evaluations in health (cost-effectiveness analysis) reduced the HPV vaccine price by over 50%, benefiting households directly [52]. However, in the case of orphan or high-cost diseases, given their specific context, a higher CET could be determined (e.g., by applying an expansion factor to the estimated value) [53]. Following this positive public policy experience, recently some major economic powers have intensified their studies on CET estimation and HTA use, one of the most prominent cases being China, where the government has aimed to make their social health insurance system more equitable and sustainable [54,55,56]. Based on this, the HTA has played a pivotal role by gradually incorporating it as a formal procedure for evidence-based decisions on the drug list since 2017 [57].
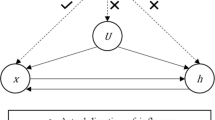
Several authors have highlighted the complexity of decision making in health systems owing to the processes, agents, and relationships involved, along with the social implications these factors determine. This complexity is heightened in health systems with diverse actors, each with different perspectives and interests that need reconciliation [58,59,60,61,62,63]. In this context, the methods and practices of HTAs have become crucial tools to support decision making, by basing it on relevant and robust scientific information, aligning with the principles and values that most States establish for health systems [64], as is the case of those considered in this article.
Integrating evidence-informed deliberative processes into the HTA (e.g., using a CET) to create more legitimate spaces and to somehow gather diverse stakeholders’ values and criteria is seen as a necessity [65]. In general terms, considering diverse stakeholders and interests in deliberative scenarios within HTA frameworks allows for managing discussions and tensions meaningfully, transcending methodological aspects to position stakeholder involvement as necessary for democracy, and exercising rights and justice. This approach aligns with frameworks of “accountability for reasonableness” [65], proposing that decision-making processes on limited resources be public deliberative exercises involving various social actors, with diverse needs, so that the establishment of priorities for the investment of these resources is not only transparent, but also within the framework of a social agreement [65, 66].
The notions of opportunity costs and limited budgets may not be familiar to many citizens when considering health choices and decisions, especially in contexts where individualistic vision dominates over collective decisions linked to social contracts in health. In this sense, improving the connection and communication between decision makers and the public is crucial, particularly to gain support for negative decisions or limitations to the scope of health benefits available to the population.
For countries to apply their CET (the result of empirical research), we believe that it is necessary to strengthen, in a systematic, deliberative, and participatory manner, the institutional processes of effective and assertive communication with society about using resources in health systems. This communication should highlight the benefits of using a CET as one of the decision criteria for the general welfare of the population, health spending efficiency, financial sustainability of the publicly funded health system, and protection of out-of-pocket spending, which prevents catastrophic impacts on households. Likewise, the technical agencies or departments that carry out HTAs should be technically and financially strengthened, as the success and agility of incorporating new health technologies (or, in a subsequent process, the review of those already incorporated in the health benefit plans, thus studying their technological obsolescence) depends on this.
We consider that the existence of a CET estimated with real-world evidence can highlight the health opportunity costs of including or excluding an intervention from the health benefit plan. This can provide greater political support for decisions not to invest or to disinvest, making these decisions more socially and politically acceptable by framing them as a trade-off between actual or potential health outcomes rather than between health and money. Hence, the importance of assertive and timely communication with society by health and economic authorities is essential to ensure the multiple benefits of having clear decision criteria (such as a CET) are understood. Decision criteria should be based on empirical considerations related to the specific context of each country, to ensure financial sustainability and protect against out-of-pocket spending for families, especially the most socioeconomically vulnerable. This research work had the limitation that we only analyzed a group of countries, even though our selection was based on the cases most referred to in international literature.
5 Conclusions
This work reviewed multiple countries on the use and importance of a CET in public health policy decision making. Although most countries in the analysis have estimated a CET with real-world evidence, a high proportion do not make it explicit as one of their criteria.
The main recommendations of our paper are summarized below: (1) it is necessary to strengthen governance within the institutional framework of the governing bodies of the health systems, based on well-defined and clear criteria that guide the decisions of national/regional health budgets, a CET can be one of these criteria; (2) the CET must be estimated using real-world evidence, separating it from the rule of one to three times the GDPpc; (3) it is essential to socially legitimize the processes of the HTA and the use of a CET through the participation of multiple actors, including patients and civil society; (4) the HTA agencies or departments must be technically and financially strengthened, resulting in agile and well-informed decision making; and (5) when using different criteria in the prioritization, coverage, reimbursement, and financing of health technologies, it is crucial to ensure that the dimensions do not overlap [64]. Finally, although there is still much to be done, there have already been concrete successful experiences (e.g., in Thailand) using a CET in public policy to make health spending efficient and thereby maximize social well-being, as we described in the document.
Notes
We follow the US Food and Drug Administration’s definition of real-world evidence (2023).
Although the CET used in England was not estimated with real-world evidence, we considered studying it because England was the first country in the world to use this prioritization tool.
In mid-2022, an attempt was made to legally legitimize the CET by incorporating it as a technical criterion for the pricing of new drugs, but in the end no such regulation was issued [40].
References
Weinstein M, Zeckhauser R. Critical ratios and efficient allocation. J Public Econ. 1973;2(2):147–57.
Karlsson G, Johannesson M. The decision rules of cost-effectiveness analysis. Pharmacoeconomics. 1996;9(2):113–20.
McCabe C, Claxton K, Culyer AJ. The NICE cost-effectiveness threshold: what it is and what that means. Pharmacoeconomics. 2008;26(9):733–44.
Santos A, Guerra-Junior A, Godman B, Morton A, Ruas C. Cost-effectiveness thresholds: methods for setting and examples from around the world. Expert Rev Pharmacoecon Outcomes Res. 2018;18(3):277–88.
Bobinac A, Van Exel N, Rutten F, Brouwer W. Willingness to pay for a quality-adjusted life-year: the individual perspective. Value Health. 2010;13(8):1046–55.
Nimdet K, Chaiyakunapruk N, Vichansavakul K, Ngorsuraches S. A systematic review of studies eliciting willingness-to-pay per quality-adjusted life year: does it justify CE threshold? PLoS One. 2015;10(4): e0122760.
Ryen L, Svensson M. The willingness to pay for a quality adjusted life year: a review of the empirical literature. Health Econ. 2015;24(10):1289–301.
WHO Commission on Macroeconomics and Health. Macroeconomics and health: investing in health for economic development. Geneva: World Health Organization; 2001.
Shillcutt S, Walker D, Goodman C, Mills A. Cost effectiveness in low- and middle-income countries: a review of the debates surrounding decision rules. Pharmacoeconomics. 2009;27(11):903–17.
Cleemput I, Neyt M, Thiry N, De Laet C, Leys M. Using threshold values for cost per quality-adjusted life-year gained in healthcare decisions. Int J Technol Assess Health Care. 2011;27(1):71–6.
Marseille E, Larson B, Kazi D, Kahn J, Rosen S. Thresholds for the cost-effectiveness of interventions: alternative approaches. Bull World Health Organ. 2015;93(2):118–24.
Griffiths UK, Legood R, Pitt C. Comparison of economic evaluation methods across low-income, middle-income and high-income countries: what are the differences and why? Economic evaluation methods: differences across country income groups. Health Econ. 2016;25(Suppl.1):29–41.
Vallejo-Torres L, García-Lorenzo B, Edney L, Stadhouders N, Edoka I, Castilla-Rodríguez I, et al. Are estimates of the health opportunity cost being used to draw conclusions in published cost-effectiveness analyses? A scoping review in four countries. Appl Health Econ Health Policy. 2022;20(3):337–49.
Revill P, Sculpher M. Cost effectiveness of interventions to tackle non-communicable diseases. BMJ. 2012;344:d7883.
Gloria M, Thavorncharoensap M, Chaikledkaew U, Youngkong S, Thakkinstian A, Chaiyakunapruk N, et al. Systematic review of the impact of health care expenditure on health outcome measures: implications for cost-effectiveness thresholds. Expert Rev Pharmacoecon Outcomes Res. 2024;24(2):203–15.
Thokala P, Ochalek J, Leech A, Tong T. Cost-effectiveness thresholds: the past, the present and the future. Pharmacoeconomics. 2018;36(5):509–22.
Schwarzer R, Rochau U, Saverno K, Jahn B, Bornschein B, Muehlberger N, et al. Systematic overview of cost-effectiveness thresholds in ten countries across four continents. J Comp Eff Res. 2015;4(5):485–504.
Woods B, Revill P, Sculpher M, Claxton K. Country-level cost-effectiveness thresholds: initial estimates and the need for further research. Value Health. 2016;19(8):929–35.
Pichón-Riviere A, Drummond M, García-Martí S, Augustovski F. Aplicación de la evidencia económica en la evaluación de tecnologías sanitarias y la toma de decisiones sobre asignación de recursos sanitarios en América Latina: siete temas clave y una propuesta preliminar de implementación. In: Nota Técnica IDB-TN-2286. Washington, DC: Banco Interamericano de Desarrollo; 2021.
Ochalek J, Lomas J, Claxton K. Estimating health opportunity costs in low-income and middle-income countries: a novel approach and evidence from cross-country data. BMJ Glob Health. 2018;3(6):e000964.
Edney L. Estimating the reference incremental cost-effectiveness ratio for the Australian health system. Pharmacoeconomics. 2018;36(2):239–52.
Espinosa O, Rodríguez-Lesmes P, Orozco L, Ávila D, Enríquez H, Romano G. Estimating cost-effectiveness thresholds under a managed healthcare system: experiences from Colombia. Health Policy Plan. 2022;37(3):359–68.
Appleby J, Devlin N, Parkin D. NICE’s cost effectiveness threshold. BMJ. 2007;335(7616):358–9.
National Institute for Health and Care Excellence. NICE health technology evaluations: the manual. London; 2022. https://www.nice.org.uk/process/pmg36/resources/nice-health-technology-evaluations-the-manual-pdf-72286779244741. Accessed 28 Jun 2024.
Lim Y. Determination of cost-effectiveness threshold for health care interventions in Malaysia. Value Health. 2017;20(8):1131–8.
Stadhouders N, Koolman X, van Dijk C, Jeurissen P, Adang E. The marginal benefits of healthcare spending in the Netherlands: estimating cost-effectiveness thresholds using a translog production function. Health Econ. 2019;28(11):1331–44.
Edoka I, Stacey N. Estimating a cost-effectiveness threshold for health care decision-making in South Africa. Health Policy Plan. 2020;35(5):546–55.
Thavorncharoensap M, Teerawattananon Y, Natanant S, Kulpeng W, Yothasamut J, Werayingyoung P. Estimating the willingness to pay for a quality-adjusted life year in Thailand: does the context of health gain matter? Clinicoecon Outcomes Res. 2013;5:29–36.
Teerawattananon Y, Tantivess S, Yothasamut J, Kingkaew P, Chaisiri K. Historical development of health technology assessment in Thailand. Int J Technol Assess Health Care. 2009;25(Suppl.1):241–52.
Vanness D, Lomas J, Ahn H. A health opportunity cost threshold for cost-effectiveness analysis in the United States. Ann Intern Med. 2021;174(1):25–32.
Paris V, Belloni A. Value in pharmaceutical pricing. OECD Health Working Papers, No. 63, OECD Publishing, Paris.
Edney L, Haji Ali Afzali H, Cheng T, Karnon J. Estimating the reference incremental cost-effectiveness ratio for the Australian health system. Pharmacoeconomics. 2018;36(2):239–52.
Lim Y, Shafie A, Chua G, Ahmad Hassali M. Determination of cost-effectiveness threshold for health care interventions in Malaysia. Value Health. 2017;20(8):1131–8.
Weinstein M. How much are Americans willing to pay for a quality-adjusted life year? Med Care. 2008;46(4):343–5.
Teerawattananon Y. The use of economic evaluation for guiding the pharmaceutical reimbursement list in Thailand. Z Evid Fortbild Qual Gesundhwes. 2014;108(7):397–404.
Claxton K, Martin S, Soares M, Rice N, Spackman E, Hinde S, et al. Methods for the estimation of the National Institute for Health and Care Excellence cost-effectiveness threshold. Health Technol Assess. 2015;19(14):1–503.
van Baal P, Perry-Duxbury M, Bakx P, Versteegh M, van Doorslaer E, Brouwer W. A cost-effectiveness threshold based on the marginal returns of cardiovascular hospital spending. Health Econ. 2019;28(1):87–100.
Angelis A, Harker M, Cairns J, Seo M, Legood R, Miners A, et al. The evolving nature of health technology assessment: a critical appraisal of NICE’s new methods manual. Value Health. 2023;26(10):1503–9.
Martin S, Lomas J, Claxton K, Longo F. How effective is marginal healthcare expenditure? New evidence from England for 2003/04 to 2012/13. Appl Health Econ Health Policy. 2021;19(6):885–903.
Isaranuwatchai W, Nakamura R, Wee HL, Sarajan MH, Wang Y, Soboon B, et al. What are the impacts of increasing cost-effectiveness threshold? A protocol on an empirical study based on economic evaluations conducted in Thailand. PLoS One. 2022;17(10):e0274944.
Angelis A, Lange A, Kanavos P. Using health technology assessment to assess the value of new medicines: results of a systematic review and expert consultation across eight European countries. Eur J Health Econ. 2018;19(1):123–52.
Comisión Nacional de Precios de Medicamentos y Dispositivos Médicos. Proyecto de Decreto. 2022. Por la cual se establece la metodología para la fijación del precio de los medicamentos nuevos a partir de la evaluación de valor terapéutico y económica realizada por el IETS. https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/MET/proyecto-circular-precios-basados-valor-terapeutico.pdf. Accessed 19 May 2024].
Giménez E, García-Pérez L, Márquez S, Asun Gutiérrez M, Bayón JC, Espallargues M, et al. Once años de evaluaciones económicas de productos sanitarios en la Red de Agencias de Evaluación: calidad metodológica e impacto del coste-utilidad. Gac Sanit. 2020;34(4):326–33.
Golan O, Hansen P, Kaplan G, Tal O. Health technology prioritization: which criteria for prioritizing new technologies and what are their relative weights? Health Policy (New York). 2011;102(2–3):126–35.
Charlton V. Justice, transparency and the guiding principles of the UK’s National Institute for Health and Care Excellence. Health Care Anal. 2022;30(2):115–45.
Charlton V. NICE and fair? Health technology assessment policy under the UK’s National Institute for Health and Care Excellence, 1999–2018. Health Care Anal. 2020;28(3):193–227.
Yanovskiy M, Levy O, Shaki Y, Zigdon A, Socol Y. Cost-effectiveness threshold for healthcare: justification and quantification. Inquiry. 2022;59:469580221081438.
Bertram M, Lauer J, De Joncheere K, Edejer T, Hutubessy R, Kieny M, et al. Cost-effectiveness thresholds: pros and cons. Bull World Health Organ. 2016;94(12):925–30.
Fraser H, Feldhaus I, Edoka I, Wade A, Kohli-Lynch C, Hofman K, et al. Extended cost-effectiveness analysis of interventions to improve uptake of diabetes services in South Africa. Health Policy Plan. 2024;39(3):253–67.
Dixit J, Prinja S, Jyani G, Bahuguna P, Gupta A, Vijayvergiya R, et al. Evaluating efficiency and equity of prevention and control strategies for rheumatic fever and rheumatic heart disease in India: an extended cost-effectiveness analysis. Lancet Glob Health. 2023;11(3):e445–55.
Verguet S, Kim J, Jamison D. Extended cost-effectiveness analysis for health policy assessment: a tutorial. Pharmacoeconomics. 2016;34(9):913–23.
Teerawattananon Y, Tritasavit N. A learning experience from price negotiations for vaccines. Vaccine. 2015;33(Suppl.1):A11–2.
Butani D, Faradiba D, Dabak S, Isaranuwatchai W, Huang-Ku E, Pachanee K, et al. Expanding access to high-cost medicines under the universal health coverage scheme in Thailand: review of current practices and recommendations. J Pharm Policy Pract. 2023;16(1):138.
Ochalek J, Wang H, Gu Y, Lomas J, Cutler H, Jin C. Informing a cost-effectiveness threshold for health technology assessment in China: a marginal productivity approach. Pharmacoeconomics. 2020;38(12):1319–31.
Butt T, Liu G, Kim D, Neumann P. Taking stock of cost-effectiveness analysis of healthcare in China. BMJ Glob Health. 2019;4(3):e001418.
Cai D, Shi S, Jiang S, Si L, Wu J, Jiang Y. Estimation of the cost-effective threshold of a quality-adjusted life year in China based on the value of statistical life. Eur J Health Econ. 2022;23(4):607–15.
Chen W, Zhang L, Hu M, Hu S. Use of health technology assessment in drug reimbursement decisions in China. BMJ. 2023;381:e068915.
Ciani O, Tarricone R, Torbica A. Diffusion and use of health technology assessment in policy making: what lessons for decentralised healthcare systems? Health Policy. 2012;108(2–3):194–202.
Molina-Marín G, Andrés R, Adriana. Tensiones en las decisiones en salud pública en el sistema de salud colombiano: el bien común en confrontación con los intereses y prácticas particulares. 1era ed. Así vamos en salud. Medellín: Pulso & Letra Editores; 2014.
Rosén M, Werkö S. Does health technology assessment affect policy-making and clinical practice in Sweden? Int J Technol Assess Health Care. 2014;30(3):265–72.
García-Lorenzo B, Vallejo-Torres L, Del Mar T, Perestelo-Pérez L, Valcárcel-Nazco C, Aguilar P. Economic evaluation seeks threshold to support decision-making. Rev Esp Salud Publica. 2015;89(6):537–44.
Liu W, Shi L, Pong R, Dong H, Mao Y, Tang M, et al. Determinants of knowledge translation from health technology assessment to policy-making in China: from the perspective of researchers. PLoS One. 2018;13(1):e0190732.
World Health Organization, European Observatory on Health Systems and Policies, Velasco M, Kristensen F, Nielsen C, Busse R. (editors). Health technology assessment and health policy-making in Europe: current status, challenges and potential. Copenhagen: World Health Organization; 2008.
Allen L. The philosophical foundations of “health for all” and universal health coverage’. Int J Equity Health. 2022;21(1):155.
Daniels N, van der Wilt G. Health technology assessment, deliberative process, and ethically contested issues. Int J Technol Assess Health Care. 2016;32(1–2):10–5.
Daniels N. Accountability for reasonableness. BMJ. 2000;321(7272):1300–1.
Acknowledgements
We are grateful for discussions with the members of health technology assessment agencies from Colombia (IETS), England (National Institute for Health and Care Excellence), and Thailand (HITAP) for their valuable input. Oscar Espinosa is grateful for all the teachings of the Centre for Health Economics at the University of York, especially the conversations with Michael Drummond, Jessica Ochalek, and Paul Revill.We also thank the participants of the HTAsiaLink webinars and the VIII CIMED Research Meeting and acknowledge Catalina Durán’s work as a research assistant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding provided by Colombia Consortium. The study was funded by the Instituto de Evaluación Económica en Salud (IETS) and the Ministry of Finance and Public Credit. Paul Rodríguez-Lesmes also acknowledges financial support from Fulbright-Colciencias and Colombia Científica—Alianza EFI No. 60185, Contract no, FP44842-220-2018, funded by The World Bank through the Scientific Ecosystems, managed by the Colombian Ministry of Science, Technology and Innovation.
Conflict of interest
Oscar Espinosa, Paul Rodríguez-Lesmes, Giancarlo Romano, Esteban Orozco, Sergio Basto, Diego Ávila, Lorena Mesa, and Hernán Enríquez have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Ethics approval for this type of study is not required by our institute or Colombian Law.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The table with the entire list of revised manuscripts is available in the supplementary material.
Code availability
Not applicable.
Authors’ contributions
Conception or design of the work: OE, PR, GR, EO; data collection: PR, OE, GR, EO, SB, DÁ, HE; data analysis and interpretation: OE, PR, GR, EO, SB, DÁ, HE; drafting the article: OE, PR, GR, EO; critical revision of the article: OE, PR, GR, EO, SB, DÁ, LM, HE; final approval of the version to be submitted: OE, PR, GR, EO, SB, DÁ, LM, HE.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Espinosa, O., Rodríguez-Lesmes, P., Romano, G. et al. Use of Cost-Effectiveness Thresholds in Healthcare Public Policy: Progress and Challenges. Appl Health Econ Health Policy (2024). https://doi.org/10.1007/s40258-024-00900-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s40258-024-00900-5