Abstract
There is currently deep uncertainty about the clinical benefits and cost effectiveness of highly specialised technologies (HSTs), like gene and cell therapies. These treatments are novel, typically have high upfront costs, the patient populations are small and heterogenous, there is minimal information on their long-term safety and effectiveness, and data are limited and often of poor quality. With the increasing number of these technologies and their high cost burden on governments and health care providers, policy makers are currently walking a decision tightrope. On the one hand, an unfavourable funding decision could potentially limit patient access to life-saving treatments, while on the other, a favourable decision could result in unsustainable budget impacts and perhaps poorer patient health outcomes. Health technology assessment (HTA) is meant to determine the value of a health technology in order to promote an equitable, efficient, and high-quality health system. However, standard HTA processes have failed to mitigate the deep uncertainties associated with these technologies. In this paper, we propose a Living HTA framework to address these challenges. This framework includes a one-off process for making explicit the societal values associated with HSTs. These would inform the decision-making approach, data collection and the development of disease-specific reference models to be used by industry sponsors as the basis for their submissions for public funding. Coverage with an evidence development mechanism is also proposed by which data can be collected in real time to update the reference model on a rolling basis, thereby allowing re-assessment of the clinical and cost effectiveness of individual HSTs. The HTA would be ‘live’ until the results indicate there is sufficient certainty for the funding decision to be confirmed, the price changed or the funding removed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Highly specialised technologies (HSTs), like gene and cell therapies, treat small, heterogeneous patient groups with often limited alternative treatment options and so there is high unmet clinical need. |
The clinical effectiveness and cost effectiveness of HSTs are often uncertain due to evidence being scarce or of poor quality and so subsequent public funding decisions are high risk. |
A framework is proposed for identifying societal preferences to guide HST funding decisions and the development of disease-specific reference models and protocols for the collection and analysis of real-world data. The integration of this post-launch data into the reference models would allow a rolling consideration of the clinical and cost effectiveness of HSTs as the evidence base develops. |
1 The Promise of Gene and Cell Therapies
Cell and gene therapies (GTx) have the potential to fundamentally shift medical treatment for many previously intractable diseases, providing long-term benefits from a single treatment with substantial savings in direct medical and indirect societal costs [1]. Due to their novelty and high cost, the current development of these highly specialised technologies (HSTs) is focused on rare diseases with a defect in a single gene or advanced untreatable blood cancers. These diseases share many characteristics including high unmet need, high disease severity and small patient populations. They are often associated with a high health care burden and substantial social consequences.
One GTx approach is a single injection of viral vectors carrying a gene with incorporation of DNA either directly into the genome or as episomes in the nucleus. In clinical trials, a single treatment with an adeno-associated viral vector GTx delivered an effective and durable treatment for 96% of Haemophilia B trial participants [2]. Alternatively, genes can be edited directly using CRISPR-Cas9 techniques or cells collected from the patient/donor can be genetically modified ex vivo and transfused into the patient as seen in chimeric antigen receptor T (CAR-T) cell therapy [3]. Promising GTx are under development or currently funded for a range of rare diseases, including haemophilia, sickle cell disease, inherited retinal dystrophy, beta thalassaemia and spinal muscular atrophy [4, 5].
The durability of some HSTs shows promise, but evidence of long-term effectiveness, safety and cost effectiveness is uncertain [4]. Side effects can be severe, for example, severe immune-related adverse events have been observed in at least a quarter of CAR-T cell therapy recipients treated for acute lymphocytic leukaemia [6]. Tools for detecting off-target effects (mutations outside the targeted site) are not well developed. At the same time, HSTs demand high prices reflecting the financial risks for industry in developing these technologies. Small target populations have meant that some effective treatments, such as Alipogene tiparvovec (Glybera) for lipoprotein lipase deficiency, have been abandoned because they are not economically viable [5]. Countries with small populations and demanding regulatory and reimbursement approval processes, such as Australia, offer less incentive for drug companies to pursue the marketing of HSTs. Australia has lagged well behind other countries in approving public funding for HSTs [7].
2 Key Challenges in the Use of Health Technology Assessment (HTA) for Highly Specialised Technologies (HSTs) in Australia
In Australia, health technology assessment (HTA) appraisal committees, including the Pharmaceutical Benefits Advisory Committee (PBAC) and Medical Services Advisory Committee (MSAC), advise the Minister for Health and Aged Care on the value of new technologies, thereby informing decisions to fund these technologies through the Pharmaceutical Benefits Scheme (PBS) and Medical Benefits Schedule (MBS), and through the National Health Reform Agreement (where States and Territories jointly fund, with the Commonwealth, selected HSTs). In 2020–2021, spending on the MBS and PBS accounted for 45.1% (A$41.2 billion) of Australian Government health expenditure [8].
Like elsewhere in the world, national HTA agencies are increasingly asked to evaluate high upfront cost HSTs. These technologies are characterised by deep uncertainty due to a poor clinical evidence base (parameter uncertainty), methodological uncertainty (relating to the choice of analytic methods such as discounting approaches and choice of perspective) and structural uncertainty (relating to the choice of model structure and structural assumptions) [9] in the decision analytic models submitted for a funding decision.
Developing an adequate evidence base to inform public funding decisions for HSTs is difficult. Challenges include small sample sizes in clinical trials, the use of single-arm studies and indirect comparisons, limited data about natural history and long-term benefits, heterogenous patient populations, a lack of established clinical endpoints and the use of surrogate outcomes [10,11,12]. In addition, due to the high upfront costs of HSTs, before most clinical benefits are realised, the discount rate applied in an economic model and the methods used to extrapolate to long-term outcomes can have a large impact on HST cost effectiveness [11]. Deep uncertainty creates a significant risk of making suboptimal funding decisions. Without an effective and consistent approach to reduce this uncertainty and its consequences, there is a high risk that the potentially transformative nature of HSTs will be underestimated. Equally, there is also a risk that clinical and economic benefits may be overestimated, with an adverse effect on health budgets and foregone health benefits from not funding alternative therapies, with consequential impacts on population health. Finally, the capacity to assess the true societal value of HSTs is hamstrung by not systematically incorporating patient and public perspectives in the cost-effectiveness analyses that strongly influence decision making.
The circumstances under which an informed Australian public would be willing to pay for the high upfront cost of potentially life-changing drugs (with the loss of opportunity to fund health care elsewhere) is currently unknown, as is the willingness of affected people to adopt HSTs. Therefore, essential factors that decision makers should consider are currently poorly delineated. We identified two Australian surveys, one asking patients their perspectives on ocular GTx [13] and one asking the general public about the acceptability of GTx more generally [14]. In the former, 62% of participants would consider a payment plan to access GTx. In the latter, 95% believed that the use of GTx for severe chronic illnesses was acceptable but only 77% for moderate chronic illness. To date, there has been limited opportunity to engage with the public or with communities most affected by the potential of HSTs. In particular, it is rare to see informed, supported, extended conversations about factors that impact public support for GTx, and the broader class of HSTs that are high cost and characterised by deep uncertainty.
3 Building on Existing Knowledge to Address the Key Challenges
The issues associated with evaluating HSTs have been variably addressed internationally through specific pathways for ‘ultra-orphan’ or ‘life-saving’ drugs, managed access programs (including coverage with evidence development [CED]) [15], risk share arrangements between government and industry [16], and sometimes ad hoc acceptance of surrogate endpoints and lower levels of statistical significance in clinical outcomes [10]. Each of these approaches has strengths and weaknesses. Most address deep uncertainty by proposing different decision criteria to those used for other technologies, such as higher willingness-to-pay thresholds due to the small patient populations involved, sharing the costs with industry, or more generous (and risky) funding criteria that are not empirically derived and may be costly [12]. However, while these approaches address the unmet clinical need for HSTs in these small populations, they usually do not address the clinical uncertainty associated with these technologies (due to the limited evidence base) and they do not address the methodological issues peculiar to the economic evaluation of HSTs which are characterised by high upfront costs, thereby affecting the timing and distribution of costs relative to when the benefits might be gained. This can impact the incremental cost-effectiveness ratio of HSTs when compared with other technologies and disadvantage them in funding decisions.
Our proposed ‘Living HTA’ methodology is an integrated framework that would use the knowledge and perspectives collected from a range of stakeholders as a scaffold both for decision making and for model development. ‘Living HTA’ was first coined by Merlin (2021) in a plenary conference presentation to Health Technology Assessment international (HTAi) [17] and builds on the Australian experience with living systematic reviews and living clinical practice guidelines which have been produced for over a decade or more. The Living HTA framework adapts the ‘living’ concept to the work undertaken by Afzali, Karnon and Merlin (2013) [18] on reference models and incorporates the lifecycle HTA approach suggested by Kirwin et al. (2022) [19]. A commentary on the promise of living HTA has also recently been published by Sarri et al. (2023), although a specific methodology was not presented [20].
4 Proposed Methodology
Generally, HTA is undertaken in two complementary phases—evidence assessment and appraisal [19]. Evidence assessment for new medicines usually involves the independent evaluation of an evidence dossier submitted by the industry sponsor who is seeking public funding for the technology. The dossier includes both clinical and economic evidence, some of which may not be in the public domain. For medical services and other technologies, a similar approach can be undertaken or, alternatively, an HTA agency may be commissioned to conduct a systematic review of the clinical evidence and a cost-effectiveness analysis, with or without inclusion of materials supplied by the sponsor. In Australia, HSTs have been progressed both through the medicine HTA pathway (to PBAC) and through the medical services pathway (to MSAC).
In the appraisal phase, the results of the evidence assessment are reviewed by the committee tasked with making recommendations for payer adoption decisions. The funding recommendations typically take the form of (1) recommend, (2) recommend with conditions, (3) defer until further information is received, or (4) reject. Conditional recommendations may restrict access to specific patient subgroups or specify price reductions to achieve an acceptable level of value or budget impact. Often a rejection decision invites a further resubmission that addresses the concerns raised. When there is deep uncertainty this can result in ‘resubmission churn’.
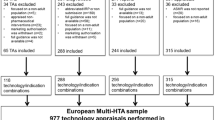
Any new process for addressing the challenges of high-cost HSTs needs to consider both evidence assessment and appraisal. We propose a new assessment framework for these technologies that can be feasibly used within current Australian HTA processes (Fig. 1) and adapted to the international context. It has application to all HSTs affected by deep uncertainty about their clinical and cost effectiveness.
This framework incorporates values and preferences from a range of societal perspectives in both the assessment and appraisal phases of HTA. A Decision Guide would be created that thematically integrates key issues identified by engaging a number of stakeholders. This Decision Guide would likely only need to be developed once and would enable structured, transparent, and consistent consideration by HTA decision makers. The Decision Guide could be used by decision makers independent of the development of the Reference Model but can also be used to inform the construction of such a model, for example, by informing the use of surrogate and patient-relevant outcomes, perspective, discount rate, and incorporation of carer burden in the model.
For each disease area where an HST would be used, a Reference Model would be created to calculate the value of the technology at a specific point in time (using the best available evidence and data sources). The model would also assess the probable value of additional research being undertaken using value-of-information (VOI) methods. This would inform whether to pursue a coverage with evidence development (CED) approach to managed access, that is, provisional funding is provided for the HST, contingent on the development of additional evidence to resolve the decision uncertainty and confirm (or remove) funding.
4.1 Developing the Decision Guide
Five steps are proposed for the development of the Decision Guide, although some of these might be forgone or modified depending on whether a holistic or streamlined approach is preferred.
The first step would be to determine what current international approaches are being used to assess HSTs for a public funding decision, with the aim of identifying a range of factors that could be considered in decision making. This could be done through a scoping review of the methodological literature, as is proposed as part of the Australian HTA Policy and Methods Review [21,22,23]. Since many HTA agencies are situated in, or funded by, Government, information on their methods and approaches will often be unpublished. It would therefore be prudent to conduct a grey literature search or survey of agencies, for example, through the International Network of Agencies for HTA (INAHTA) and request unpublished documentation.
The second step would be to undertake an analysis of ethical and legal issues relating to the funding of HSTs. This would examine respect for persons, consent, equity of access, personal identity, and other issues raised in the HTA ethics literature [24], with a focus on implications for autonomy, how society views people with particular diseases, the technology’s symbolic value, and ethical issues relating to the choice of end points in the assessment. The legal analysis would consider a broad spectrum of regulatory models including (but not limited to), case law, legislation, codes of practise and industry standards. Lessons from comparable high-cost technologies could then be considered.
The third step would be to determine the factors that currently influence decision making about HSTs undertaken by local policy makers. This could be done through interviews and a reflexive thematic analysis of the interview data [25].
The fourth step would be to identify the factors that patients think are important for making public funding decisions on high upfront cost therapies affected by deep uncertainty. This could be achieved through deliberative World Cafés [26, 27]. World Café methodology has increasingly been adopted as an exploratory step in a mixed methods approach [28]. Recruitment strategies could include advertising through dedicated rare disease clinics and specific support groups and organisations. Recorded audio from the Cafés would be analysed for identification of themes important to patients on this topic.
The fifth step would explore what principles should underpin public funding of HSTs affected by deep uncertainty. The mechanism proposed is citizens’ juries with a sample of participants that reflects the national population, in terms of a range of sociodemographic characteristics [29, 30]. The citizens’ juries would produce a list of factors which citizens believe should underpin public funding of HSTs.
Using all of the information obtained, data would inform the basis of a Decision Guide for policy makers to use when making funding decisions about HSTs.
Decision aids have been used in HTA previously, ranging from simple decision criteria (as per the PBAC Guidelines [31]) to multi-criteria decision analysis (MCDA) [32]. However, both of these approaches have their limitations. The criteria outlined in the 2016 PBAC Guidelines reflect quantifiable factors like clinical benefit, cost effectiveness and financial impact, together with less readily quantifiable factors like confidence in the presented evidence or assumptions, equity, the presence of effective therapeutic alternatives, and the severity of the medical condition treated. The criteria are primarily clinical or economic and do not systematically incorporate patient, ethical, legal and social perspectives into the value of a therapy.
MCDA has been adopted or piloted by HTA agencies in several countries. The approach is appealing because it arrives at a final ‘score’ through a simple weighted sum of pre-specified decision criteria scores. This final score indicates a favourable or unfavourable funding decision. However, many applications of MCDA violate theoretical requirements that the criteria should be preferentially independent and not overlap (to ensure there is no double-counting of some dimensions of value) [32]. MCDA also fails to accommodate deliberative enrichment within the decision-making process itself, in that the preference weights are pre-set (static) and so do not reflect how multiple views expressed on a topic can inform and persuade a decision maker to change their initial position.
Our proposed Decision Guide includes elements from MCDA but is not quantitative and so allows more flexibility for decision makers. Critical decision criteria would be derived from a range of perspectives in a systematised, transparent manner. The Guide is primarily aimed at decision makers and may or may not be used to inform the development of the Reference Model.
4.2 Constructing a Living HTA Reference Model
Variations in modelled depictions of the costs and effects of alternative treatments (e.g., choice of model structure) significantly increase the level of decision-maker uncertainty. To reduce this uncertainty, a disease-specific Living HTA Reference Model can be constructed to address multiple problems, as opposed to the construction of single-use models [18]. The key distinguishing features of such a Reference Model are its (i) flexibility to evaluate a range of alternative health technologies that target disease progression for the disease it is modelling (including all relevant comparators); (ii) capacity to characterise key sources of uncertainty; and (iii) ability to incorporate VOI analysis [33].
The Reference Model can be provided, by government or the health care payer, to any industry sponsor intending to submit an HST to an HTA appraisal committee, to provide a standardised approach to modelling the use of the technology in the disease area. The data gathered to feed the model once submitted (see further below) would regularly update parameter estimation, that is, as evidence is generated, the economic value of the technology is re-assessed and decision uncertainty re-evaluated. It is here that the HTA is living, in the sense that re-assessment is live and ongoing. Pre-determined research-oriented managed access (ROMA) protocols would specify the frequency and criteria that need to be met for re-appraisal by the HTA committees. The outcome of this phase would inform confirmation of funding for the technology, disinvestment of the technology if it is found to have low value, or price changes. Depending on the model data sources, the model updates and reassessment alerts may be able to be automated.
Following the choice of analytical methods (e.g., discounting approaches) informed by our Decision Guide, the Reference Model would be developed in line with good modelling practice (as per the ISPOR Modelling Task Force) and according to a published methodological framework [18, 34].
Briefly, this process involves five stages:
-
Model conceptualisation—based on a systematic review of clinical and economic literature on the natural history or progress of the condition that the HST is targeting, after which its final structure will be validated by an expert panel. This process will also inform the choice of patient population and appropriate comparators that can serve as the control group.
-
Choice of modelling technique—for example, an individual-based technique is more appropriate when a number of events and several patient attributes (influencing disease progression) are included in the model.
-
Model construction—relevant data sources would be systematically identified to obtain data (e.g., baseline risks, utility values and costs of health states/events) and to estimate risk equations following good modelling practice. These data might be real-world data (RWD) such as clinical registry data, claims data, and other administrative data sets providing information on diagnosis, laboratory and clinical outcomes, and complications of disease and treatment from patients. These data would be supplemented by a synthesis of evidence from the published literature. If the data sources identified do not inform the estimation of all model inputs, an expert elicitation process would be undertaken.
-
Verification and validation—using the Assessment of the Validation Status of Health-Economic decision models (AdViSHE) tool [35], the model would be verified (checked for errors) and validated to allow more confidence in model predictions.
-
Uncertainty analysis—one of the key strengths of a Reference Model is that it fully identifies alternative plausible health states and treatment choices during the model development process and thereby systematically characterises both structural uncertainty and parameter uncertainty. Scenario analysis and parameterisation can be used to address structural uncertainty, along with deterministic sensitivity analysis and probabilistic sensitivity analysis to characterise parameter uncertainty [9].
The model would be provided to the industry sponsor to adapt to the economic evaluation of the HST that they are submitting.
The model can be constructed to inform a VOI analysis, using a willingness-to-pay threshold based on previous funding decisions for the disease being treated. The VOI analysis would assess the value of additional certainty for parameter inputs in the model. In this case, the value relates to the reduction in the probability of making an incorrect funding decision. If this value exceeds the cost of research, then additional research may be undertaken. If the value of additional certainty is low, or the cost of research is too high, then decision makers can be informed that the current presented evidence is the best they are going to get. This information, in itself, is valuable for decision makers.
If, however, there is additional value from further research then there needs to be guidance on the type and shape of that research. Research-oriented Managed Access (ROMA) protocols can be co-designed between industry and government (payers) that specify the different elements of RWD that are to be collected and used to update inputs in the Reference Model [19]. The ROMA protocols would be informed by two ‘bolt on’ components to the reference model: (i) a Technology Diffusion Model (TDM) that estimates the uptake (e.g., of the HST) locally, and (ii) a ‘real-world evidence’ (RWE) generation model that analyses clinical registry and administrative data to estimate clinical effectiveness while the technology is being conditionally and provisionally funded in the health system. Data architecture (including storage and linkage) is a key enabler for the implementation of this Living HTA framework. For the framework to be feasible, data need to be identifiable, of good quality, validated, secure and with patient privacy and consenting principles observed. The outputs from the TDM and RWE models would be used to regularly update parameter estimation in the Reference Model (i.e., as evidence is generated, the economic value of the technology is re-assessed and decision uncertainty re-evaluated). As mentioned earlier, depending on the RWE model data sources available, the model updates and reassessment alerts may be able to be automated.
Given the resource intensiveness of the proposed framework, it is not intended for broader use in HTA. Its use is proposed for coverage with evidence development of HSTs because of the high unmet clinical need of patients with the diseases and conditions targeted by HSTs and the concomitant evidentiary challenges that cannot be resolved in a timely way (due to the small number of patients). In addition, unlike other therapies, the economic evaluation of HSTs is associated with deep methodological issues such as the choice of perspective (i.e., social vs health system) and discounting (high upfront costs), that is, timing and distribution of costs in relation to when benefits might be gained, and which can impact the incremental cost-effectiveness ratio when compared with other technologies. Also, commonly for these technologies there is limited evidence of long-term data which can lead to temporal uncertainty and affect structural assumptions in the modelling.
Our proposed methodological framework is a practical approach developed by HTA methodologists to reduce deep uncertainty associated with decisions to fund HSTs. In addition, it could feasibly (i) better support outcomes-based contractual agreements with industry sponsors to subsidise and expedite early patient access to HSTs and other promising technologies, (ii) increase the efficiency and reduce the cost of HTA processes by reducing ‘re-submission churn’, (iii) provide a financial incentive for industry to innovate in neglected disease areas, (iv) facilitate health system sustainability and (v) feature triggers for price adjustment or disinvestment if therapies prove to be clinically or cost ineffective.
References
Rodriguez-Santana I, DasMahapatra P, Burke T, Hakimi Z, Bartelt-Hofer J, Nazir J, O’Hara J. Health-related quality of life, direct medical and societal costs among children with moderate or severe haemophilia in Europe: multivariable models of the CHESS-PAEDs study. Orphanet J Rare Dis. 2022;17(1):150. https://doi.org/10.1186/s13023-022-02301-0.
European Medicines Agency. First gene therapy to treat haemophilia B. 2022. https://www.ema.europa.eu/en/news/first-gene-therapy-treat-haemophilia-b. (Accessed 23 Apr 2023).
Shah NN, Lee DW, Yates B, Yuan CM, Shalabi H, Martin S, Wolters PL, Steinberg SM, Baker EH, Delbrook CP, Stetler-Stevenson M, Fry TJ, Stroncek DF, Mackall CL. Long-term follow-up of CD19-CAR T-Cell therapy in children and young adults with B-ALL. J Clin Oncol. 2021;39(15):1650–9. https://doi.org/10.1200/JCO.20.02262.
O’Sullivan G, Philips JG, Rasko JE. Clinical gene technology in Australia: building on solid foundations. Med J Aust. 2022;217(2):65–70. https://doi.org/10.5694/mja2.51629.
Ponchopień M, Paterak E, Clay E, Janik J, Aballea S, Biernikiewicz M, Toumi M. An overview of health technology assessments of gene therapies with the focus on cost-effectiveness models. J Mark Access Hlth Pol. 2021;9(1):2002–6. https://doi.org/10.1080/20016689.2021.2002006.
Anagnostou T, Riaz IB, Hashmi SK, Murad MH, Kenderian SS. Anti-CD19 chimeric antigen receptor T-cell therapy in acute lymphocytic leukaemia: a systematic review and meta-analysis. Lancet Haematol. 2020;7(11):e816–26. https://doi.org/10.1016/S2352-3026(20)30277-5.
Vu B-K, Forsythe A, Nguyen K, Tomaras D. PBI135 Health technology assessment (HTA) review of cell and gene therapies: the road to reimbursement. Value Health. 2020;2(Suppl 1):S20. https://doi.org/10.1016/j.jval.2020.04.099.
Australian Institute of Health and Welfare (AIHW). Health expenditure Australia 2020-21. 2022. https://www.aihw.gov.au/reports/health-welfare-expenditure/health-expenditure-australia. (Accessed 23 Apr 2023).
Afzali HH, Bojke L, Karnon J. Model structuring for economic evaluations of new health technologies. Pharmacoeconomics. 2018;36:1309–19.
Stafinski T, Glennie J, Young A, Menon D. HTA decision-making for drugs for rare diseases: comparison of processes across countries. Orphanet J Rare Dis. 2022;17:258. https://doi.org/10.1186/s13023-022-02397-4.
Huygens S, Versteegh MM, Vegter S, Schouten LJ, Kanters TA. Methodological challenges in the economic evaluation of a gene therapy for RPE65-mediated inherited retinal disease: the value of vision. Pharmacoeconomics. 2021;39(4):383–97. https://doi.org/10.1007/s40273-021-01003-y.
Drummond M, Ciani O, Fornaro G, et al. How are health technology assessment bodies responding to the assessment challenges posed by cell and gene therapy? BMC Health Serv Res. 2023;23:484. https://doi.org/10.1186/s12913-023-09494-5.
Mack HG, Britten-Jones AC, McGuinness MB, Chen FK, Grigg JR, Jamieson RV, Edwards TL, De Roach J, O’Hare F, Martin KR, Ayton LN. Survey of perspectives of people with inherited retinal diseases on ocular gene therapy in Australia. Gene Ther. 2023;30(3–4):336–46. https://doi.org/10.1038/s41434-022-00364-z.
Watson M. Defining public attitudes and understanding of human gene therapy in Australia. A thesis submitted for degree of Doctor of Philosophy. Canberra: ANU; 2020. https://doi.org/10.25911/HPSW-SJ81.
Carter D, Merlin T, Hunter D. An ethical analysis of coverage with evidence development. Value Health. 2019;22(8):878–83. https://doi.org/10.1016/j.jval.2019.02.011.
Robinson MF, Mihalopoulos C, Merlin T, Roughead E. Characteristics of managed entry agreements in Australia. Int J Technol Assess Health Care. 2018;34(1):46–55. https://doi.org/10.1017/S0266462317001106.
Merlin T. Evidence for HTA: innovative methods for challenging times. Plenary presentation. Health Technology Assessment international (HTAi) Annual Meeting, June 21, 2021.
Afzali H, Karnon J, Merlin T. Improving the accuracy and comparability of model-based economic evaluations of health technologies for reimbursement decisions: a methodological framework for the development of reference models. Med Decis Making. 2013;33(3):325–32. https://doi.org/10.1177/0272989X12458160.
Kirwin E, Round J, Bond K, McCabe C. A conceptual framework for life-cycle health technology assessment. Value Health. 2022;25(7):1116–23. https://doi.org/10.1016/j.jval.2021.11.1373.
Sarri G, Forsythe A, Elvidge J, et al. Living health technology assessments: how close to living reality? BMJ Evidence-Based Med. 2023. https://doi.org/10.1136/bmjebm-2022-112152.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. https://doi.org/10.1080/1364557032000119616.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. https://doi.org/10.1186/1748-5908-5-69.
Australian Government Department of Health and Aged Care. Research and analysis plan – Evidence to support the HTA Review. https://www.health.gov.au/resources/publications/research-and-analysis-plan-evidence-to-support-the-hta-review
Hofmann B. Toward a procedure for integrating moral issues in health technology assessment. Int J Technol Assess Health Care. 2005;21(3):312–8. https://doi.org/10.1017/s0266462305050415.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. https://doi.org/10.1191/1478088706qp063oa.
Street J, Barrie H, Eliott J, Carolan L, McCorry F, Cebulla A, Phillipson L, Prokopovich K, Hanson-Easey S, Burgess T, On Behalf Of The Smart Ageing Research Group. Older adults’ perspectives of smart technologies to support aging at home: insights from five World Cafe forums. IJERPH. 2022;19(13):7817. https://doi.org/10.3390/ijerph19137817.
Prokopovich K, Phillipson L, West Pitts L, Stanoevska B, Street J, Braunack-Mayer A. Using World Cafés to engage an Australian culturally and linguistically diverse community around human papillomavirus vaccination. Health Expect. 2023. https://doi.org/10.1111/hex.13703.
Löhr K, Weinhardt M, Sieber S. The, “World Café” as a participatory method for collecting qualitative data. Int J Qual Method. 2020. https://doi.org/10.1177/1609406920916976.
Stafinski T, Street J, Young A, Menon D. Moving beyond the court of public opinion: A citizens’ jury exploring the public’s values around funding decisions for ultra-orphan drugs. Int J Environ Res Public Health. 2023;20(1):633. https://doi.org/10.3390/ijerph20010633.
Street J, Duszynski K, Krawczyk S, Braunack-Mayer A. The use of citizens’ juries in health policy decision-making: a systematic review. Soc Sci Med. 2014;109:1–9. https://doi.org/10.1016/j.socscimed.2014.03.005.
Australian Government Department of Health. Guidelines for preparing a submission to the Pharmaceutical Benefits Advisory Committee (Version 5.0). 2016. https://pbac.pbs.gov.au/. (Accessed 23 Apr 2023).
Marsh KD, et al. The use of MCDA in HTA: great potential, but more effort needed. Value Health. 2018;21(4):394–7. https://doi.org/10.1016/j.jval.2017.10.001.
Afzali HH, Karnon J. Expediting patient access to new health technologies: role of disease-specific reference models. Value Health. 2021;24:755–8. https://doi.org/10.1016/j.jval.2020.12.013.
Afzali HH, Karnon J, Theou O, Beilby J, Cesari M, Visvanathan R. Structuring a conceptual model for cost-effectiveness analysis of frailty interventions. PLoS One. 2019;14: e0222049. https://doi.org/10.1371/journal.pone.0222049.
Vemer P, Corro Ramos I, van Voorn GA, Al MJ, Feenstra TL. AdViSHE: a validation-assessment tool of health-economic models for decision makers and model users. Pharmacoeconomics. 2016;34(4):349–61. https://doi.org/10.1007/s40273-015-0327-2.
Acknowledgement
This manuscript was the result of a grant application. Our thanks go to the team of chief and associate investigators on the Living HTA project.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors have no financial conflicts of interest. Professor Merlin’s research team, Adelaide Health Technology Assessment (AHTA), evaluates medicines and medical services submitted for Australian Government funding decisions in Australia. The Australian Government had no role in the conception or development of this article.
Funding
Not applicable.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication (from Patients/Participants)
Not applicable.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Contributions
All authors contributed to the conception and design of this paper. The first draft of the manuscript was written by Tracy Merlin and all authors commented on other versions of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Merlin, T., Street, J., Carter, D. et al. Challenges in the Evaluation of Emerging Highly Specialised Technologies: Is There a Role for Living HTA?. Appl Health Econ Health Policy 21, 823–830 (2023). https://doi.org/10.1007/s40258-023-00835-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-023-00835-3