Abstract
Introduction
There is a boom in imaging biomarker-driven companion and complementary diagnostics (CDx) for cancer, which brings opportunity for personalized medicine. Whether adoption of these technologies is likely to be cost-effective is a relevant question, and studies on this topic are emerging. Despite the growing number of economic evaluations, no review of the methods used, quality of reporting, and potential risk of bias has been done. We report a systematic review to identify, summarize, and critique the cost-effectiveness evidence for the use of biomarker-driven and imaging-based CDx to inform cancer treatments.
Methods
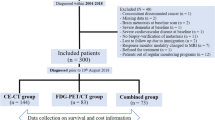
The Preferred Reporting Items of Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed. Systematic literature searches until 30 December 2022 were performed in PubMed, Web of Science, Medline, Embase, and Scopus for economic evaluations of imaging biomarker-based CDx for cancer. The inclusion and exclusion of studies were determined by pre-specified eligibility criteria informed by the ‘Patient, Intervention, Comparison, Outcome’ (PICO) framework. The Consolidated Health Economic Evaluation Reporting Standards (CHEERS) was used to assess the quality of reporting, and the Bias in Economic Evaluation (ECOBIAS) was used to examine the potential risk of bias of included studies.
Results
A total of 12 papers were included, with eight model-based and four trial-based studies. Implementing biomarker-driven, imaging-based CDx was reported to be cost-effective, cost saving, or dominant (cost saving and more effective) in ten papers. Inconsistent methods were found in the studies, and the quality of reporting was lacking against the CHEERS reporting guideline. Several potential sources of ‘risk of bias’ were identified. These should be acknowledged and carefully considered by researchers planning future health economic evaluations.
Conclusion
Despite favorable results towards the implementation of imaging biomarker-based CDx for cancer, there is room for improvement regarding the quantity and quality of economic evaluations, and that is expected as the awareness of current study limitations increases and more clinical data become available in the future.


Similar content being viewed by others
References
Ramón y Cajal S, Sesé M, Capdevila C, Aasen T, De Mattos-Arruda L, Diaz-Cano SJ, et al. Clinical implications of intratumor heterogeneity: challenges and opportunities. J Mol Med (Berl). 2020;98(2):161–77.
Janku F. Tumor heterogeneity in the clinic: is it a real problem? Ther Adv Med Oncol. 2014;6(2):43–51.
Dagogo-Jack I, Shaw AT. Tumour heterogeneity and resistance to cancer therapies. Nat Rev Clin Oncol. 2018;15(2):81–94.
Wang C, Yang J, Luo H, Wang K, Wang Y, Xiao Z-X, et al. CancerTracer: a curated database for intrapatient tumor heterogeneity. Nucleic Acids Res. 2020;48(D1):D797–806.
Verma M. Personalized medicine and cancer. J Pers Med. 2012;2(1):1–14.
Krzyszczyk P, Acevedo A, Davidoff EJ, Timmins LM, Marrero-Berrios I, Patel M, et al. The growing role of precision and personalized medicine for cancer treatment. Technology (Singap World Sci). 2018;6(03n04):79–100.
Jørgensen JT. Companion and complementary diagnostics: clinical and regulatory perspectives. Trends Cancer. 2016;2(12):706–12.
Jørgensen JT. The current landscape of the FDA approved companion diagnostics. Transl Oncol. 2021;14(6): 101063.
Marusyk A, Polyak K. Tumor heterogeneity: causes and consequences. Biochim Biophys Acta Rev Cancer. 2010;1805(1):105–17.
Marusyk A, Almendro V, Polyak K. Intra-tumour heterogeneity: a looking glass for cancer? Nat Rev Cancer. 2012;12(5):323–34.
Tully KM, Sobol NB, Pereira PMR, Lewis JS. Chapter 10-molecular imaging companion diagnostics. In: Jørgensen JT, editor. Companion and complementary diagnostics. Academic Press; 2019. p. 201–28.
Marusyk A, Janiszewska M, Polyak K. Intratumor heterogeneity: the Rosetta stone of therapy resistance. Cancer Cell. 2020;37(4):471–84.
Robertson E, Baxter G. Tumour seeding following percutaneous needle biopsy: the real story! Clin Radiol. 2011;66(11):1007–14.
Lone SN, Nisar S, Masoodi T, Singh M, Rizwan A, Hashem S, et al. Liquid biopsy: a step closer to transform diagnosis, prognosis and future of cancer treatments. Mol Cancer. 2022;21(1):1–22.
Bonanno L, Dal Maso A, Pavan A, Zulato E, Calvetti L, Pasello G, et al. Liquid biopsy and non-small cell lung cancer: are we looking at the tip of the iceberg? Br J Cancer. 2022;127(3):383–93.
Leighl NB, Page RD, Raymond VM, Daniel DB, Divers SG, Reckamp KL, et al. Clinical utility of comprehensive cell-free DNA analysis to identify genomic biomarkers in patients with newly diagnosed metastatic non–small cell lung cancer. Clin Cancer Res. 2019;25(15):4691–700.
Schrock AB, Welsh A, Chung JH, Pavlick D, Bernicker EH, Creelan BC, et al. Hybrid capture–based genomic profiling of circulating tumor DNA from patients with advanced non–small cell lung cancer. J Thorac Oncol. 2019;14(2):255–64.
Govaerts L, Simoens S, Van Dyck W, Huys I. Shedding light on reimbursement policies of companion diagnostics in European countries. Value Health. 2020;23(5):606–15.
Goodacre S, McCabe C. An introduction to economic evaluation. Emerg Med J. 2002;19(3):198.
Gazelle GS, Mcmahon PM, Siebert U, Beinfeld MT. Cost-effectiveness analysis in the assessment of diagnostic imaging technologies. Radiology. 2005;235(2):361–70.
Oosterhoff M, van der Maas ME, Steuten LM. A systematic review of health economic evaluations of diagnostic biomarkers. Appl Health Econ Health Policy. 2016;14(1):51–65.
Seo MK, Cairns J. How are we evaluating the cost-effectiveness of companion biomarkers for targeted cancer therapies? A systematic review. BMC Cancer. 2021;21(1):1–21.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34.
Schardt C, Adams MB, Owens T, Keitz S, Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak. 2007;7(1):16.
Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, et al. Consolidated health economic evaluation reporting standards (CHEERS) 2022 explanation and elaboration: a report of the ISPOR CHEERS II Good Practices Task Force. Value Health. 2022;25(1):10–31.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated health economic evaluation reporting standards (CHEERS) statement. Int J Technol Assess Health Care. 2013;29(2):117–22.
Adarkwah CC, van Gils PF, Hiligsmann M, Evers SM. Risk of bias in model-based economic evaluations: the ECOBIAS checklist. Expert Rev Pharmacoecon Outcomes Res. 2016;16(4):513–23.
Evers SM, Hiligsmann M, Adarkwah CC. Risk of bias in trial-based economic evaluations: Identification of sources and bias-reducing strategies. Psychol Health. 2015;30(1):52–71.
Schwenck J, Olthof SC, Pfannenberg C, Reischl G, Wegener D, Marzec J, et al. Intention-to-treat analysis of Ga-68-PSMA and C-11-choline PET/CT versus CT for prostate cancer recurrence after surgery. J Nucl Med. 2019;60(10):1359–65.
Gordon LG, Elliott TM, Joshi A, Williams ED, Vela I. Exploratory cost-effectiveness analysis of 68Gallium-PSMA PET/MRI-based imaging in patients with biochemical recurrence of prostate cancer. Clin Exp Metastasis. 2020;37(2):305–12.
Scholte M, Barentsz JO, Sedelaar JPM, Gotthardt M, Grutters JPC, Rovers MM. Modelling study with an interactive model assessing the cost-effectiveness of Ga-68 prostate-specific membrane antigen positron emission tomography/computed tomography and nano magnetic resonance imaging for the detection of pelvic lymph node metastases in patients with primary prostate cancer. Eur Urol Focus. 2020;6(5):967–74.
Alberts I, Mingels C, Zacho HD, Lanz S, Schoder H, Rominger A, et al. Comparing the clinical performance and cost efficacy of [68Ga]Ga-PSMA-11 and [18F]PSMA-1007 in the diagnosis of recurrent prostate cancer: a Markov chain decision analysis. Eur J Nucl Med Mol Imaging. 2022;49(12):4252–61.
Cardet RED, Hofman MS, Segard T, Yim J, Williams S, Francis RJ, et al. Is prostate-specific membrane antigen positron emission tomography/computed tomography imaging cost-effective in prostate cancer: an analysis informed by the proPSMA Trial. Eur Urol. 2021;79(3):413–8.
Song R, Jeet V, Sharma R, Hoyle M, Parkinson B. Cost-effectiveness analysis of prostate-specific membrane antigen (PSMA) positron emission tomography/computed tomography (PET/CT) for the primary staging of prostate cancer in Australia. Pharmacoeconomics. 2022;40(8):807–21.
van der Sar ECA, Keusters WR, van Kalmthout LWM, Braat AJAT, de Keizer B, Frederix GWJ, et al. Cost-effectiveness of the implementation of [68Ga]Ga-PSMA-11 PET/CT at initial prostate cancer staging. Insights Imaging. 2022;13(1):132.
Koleva-Kolarova RG, Greuter MJW, Van Kruchten M, Vermeulen KM, Feenstra T, Buskens E, et al. The value of PET/CT with FES or FDG tracers in metastatic breast cancer: a computer simulation study in ER-positive patients. Br J Cancer. 2015;112(10):1617–25.
Koleva-Kolarova RG, Greuter MJW, Feenstra TL, Vermeulen KM, de Vries EFJ, Parkin D, et al. Molecular imaging with positron emission tomography and computed tomography (PET/CT) for selecting first-line targeted treatment in metastatic breast cancer: a cost-effectiveness study. Oncotarget. 2018;9(28):19836–46.
Kosuda S, Kusano S, Ishihara S, Nawashiro H, Shima K, Kamata N, et al. Combined Tl-201 and Ga-67 brain SPECT in patients with suspected central nervous system lymphoma or germinoma: clinical and economic value. Ann Nucl Med. 2003;17(5):359–67.
Dimitroulopoulos D, Xynopoulos D, Tsamakidis K, Paraskevas E, Zisimopoulos A, Andriotis E, et al. Scintigraphic detection of carcinoid tumors with a cost effectiveness analysis. World J Gastroenterol. 2004;10(24):3628–33.
Froelich MF, Schnitzer ML, Holzgreve A, Gassert FG, Gresser E, Overhoff D, et al. Cost-effectiveness analysis of Ga-68 DOTA-TATE PET/CT, in-111-pentetreotide SPECT/CT and CT for diagnostic workup of neuroendocrine tumors. Diagnostics (Basel). 2021;11(2):334.
Öberg K. Gallium-68 somatostatin receptor PET/CT: is it time to replace 111Indium DTPA octreotide for patients with neuroendocrine tumors? Endocrine. 2012;42(1):3–4.
Schreiter NF, Brenner W, Nogami M, Buchert R, Huppertz A, Pape U-F, et al. Cost comparison of 111In-DTPA-octreotide scintigraphy and 68Ga-DOTATOC PET/CT for staging enteropancreatic neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2012;39(1):72–82.
Eberlein U, Lassmann M. Dosimetry of [68Ga]-labeled compounds. Appl Radiat Isot. 2013;76:70–4.
Hofman MS, Kong G, Neels OC, Eu P, Hong E, Hicks RJ. High management impact of Ga-68 DOTATATE (GaTate) PET/CT for imaging neuroendocrine and other somatostatin expressing tumours. J Med Imag Radiat Oncol. 2012;56(1):40–7.
Jacobsson H, Larsson P, Jonsson C, Jussing E, Grybäck P. Normal uptake of 68Ga-DOTA-TOC by the pancreas uncinate process mimicking malignancy at somatostatin receptor PET. Clin Nucl Med. 2012;37(4):362–5.
Velikyan I. Prospective of 68Ga-radiopharmaceutical development. Theranostics. 2014;4(1):47.
Bateman TM. Advantages and disadvantages of PET and SPECT in a busy clinical practice. J Nucl Cardiol. 2012;19(1):3–11.
Ten JB. arguments for a societal perspective in the economic evaluation of medical innovations. Eur J Health Econ. 2009;10(4):357–9.
Hendriks MR, Al MJ, Bleijlevens MH, van Haastregt JC, Crebolder HF, van Eijk JTM, et al. Continuous versus intermittent data collection of health care utilization. Med Decis Making. 2013;33(8):998–1008.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This research was supported by Singapore’s Health and Biomedical Sciences (HBMS) Industry Alignment Fund Pre-Positioning (IAF-PP) grant H18/01/a0/018 (A-MC) administered by the Agency for Science, Technology and Research (A*STAR), and Duke-NUS Phase 2 Research Block Grant (NG).
Conflict of Interest
SL, DT, NG, and A-MC declare that they have no conflict of interest.
Data Availability
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
Code Availability
Not applicable.
Authors’ Contributions
SL: study rationale and design, literature search, literature selection, data extraction, quality assessment, interpretation and refection, and writing and reviewing the manuscript. DT: reviewing the manuscript. NG: study rationale and design, interpretation and refection, reviewing the manuscript, and guarantor of the study. A-MC: study rationale and design, interpretation and refection, and reviewing the manuscript.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication (from patients/participants)
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, S., Tan, D.S., Graves, N. et al. Economic Evaluations of Imaging Biomarker-Driven Companion Diagnostics for Cancer: A Systematic Review. Appl Health Econ Health Policy 21, 841–855 (2023). https://doi.org/10.1007/s40258-023-00833-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-023-00833-5