Abstract
Background
Infertility is a medical condition affecting an estimated 186 million people worldwide. Medically assisted fertility treatments allow many of these individuals to have a baby. Insights about preferences of patients who have experienced fertility treatment should be used to inform funding policies and treatment configurations that best reflect the patients’ voice and the value of fertility treatment to patients.
Objective
To explore the preferences for fertility treatment attributes of infertile women who had previously undergone or were undergoing fertility treatments—ex post perspective.
Methods
We used data from a stated-preference discrete choice experiment (DCE) among 376 Australian women who had undergone or were undergoing fertility treatment. Respondents chose their preferred treatment choices in 12 hypothetical treatment choice scenarios described by seven attributes (success rates, side effects, counselling/peer support, treatment journey, continuity of care, availability of experimental treatment and out-of-pocket cost). We estimated random parameter logit (RPL) and latent class (LC) models that accounted for preference heterogeneity. The results were used to derive price elasticities of demand and marginal willingness-to-pay (WTP) values for the treatment attributes explored within the DCE survey.
Results
Income level did not have a significant effect on marginal WTP for fertility treatment attributes. The demand for fertility treatment from an ex post perspective was found to be highly inelastic (treatment cost changes had almost no impact on demand). Success rates and out-of-pocket costs were significant and important predictors of individuals’ treatment choices conditional on the attributes and levels included in the study. These were followed by counselling/peer support, side effects, treatment journey, continuity of care, and availability of experimental treatment, in that order. Respondents were willing to pay $383–$524 per one percentage point increase in the treatment success rate and over $2000 and over $3500 to avoid moderate and significant side effects, respectively (values are reported in AU$). Latent class models revealed that the majority of respondents (51%) were risk-averse success-rate seekers.
Conclusion
Infertile women who had previously undergone or were undergoing fertility treatment valued fertility treatment highly as reflected by highly price-inelastic demand. Success rate of treatment and out-of-pocket costs were the most important attributes and largely determined patients’ WTP for fertility treatment relative to the attributes and levels used in the study. While further research should investigate the price sensitivity of women who have not experienced fertility treatment, these results might explain why women continue fertility treatment once they have commenced despite their financial capacity to pay. Future research should also determine patients’ price elasticities for a fertility treatment program with multiple treatment cycles.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Infertile women who had been or were undergoing fertility treatment valued fertility treatment highly, with the treatment success rate and out-of-pocket cost attributes having the highest conditional relative importance among the attributes included in the study. |
Treatment demand was found to be highly inelastic to changes in cost, and marginal willingness-to-pay for treatment attributes did not change significantly with patients’ income level. |
While further research should investigate how price-sensitive women are to entering the fertility market, these results might explain why women continue fertility treatment once they have commenced despite their financial capacity to pay. |
1 Introduction
Infertility is recognized by the World Health Organization as a medical disease [1] causing significant suffering to an estimated 186 million people worldwide [2]. Infertility affects approximately 15% of couples during their lifetime and is equally prevalent across high- and low-income countries [3, 4]. The number of individuals affected by infertility continues to increase globally [4], largely due to the trend to delayed childbearing, which increases the risk of age-related infertility, increasing rates of obesity and sexually transmitted infections, and a global decrease in sperm counts [5,6,7].
However, fertility treatments, including assisted reproductive technologies (ARTs) such as in vitro fertilization (IVF), allow many women to conceive. An ART treatment cycle involves a series of steps performed in a fertility clinic over 4–6 weeks, involving hormonal stimulation to mature multiple eggs in the ovaries, retrieval of these eggs under general anaesthetic, fertilization in the laboratory with partner or donor sperm, and transfer of the resulting embryo(s) into the uterus in the hope of achieving a pregnancy. The success rate of each cycle depends largely on female age, with the chance of a live birth around 40% per cycle in women aged under 35 years to less than 10% in women aged ≥ 40 years [8]. Therefore, women often have to undergo multiple ART cycles to achieve a birth (if at all) and many will discontinue treatment due to psychological, financial or relationship stress [9]. The number of ART cycles undertaken globally has increased by around 5% per annum over the last decade, with an estimated 3.4 million cycles performed each year [10]. In Australia, approximately 80,000 ART cycles are undertaken annually, resulting in the birth of one in 20 babies born [11].
1.1 Funding for Fertility Treatment
Funding for fertility treatments varies substantially around the world [12,13,14,15]. Australia has a supportive funding environment with its universal health insurance scheme reimbursing around two-thirds of the costs of each ART cycle, without restrictions based on age or number of previous attempts [16]. Arguably the reason for the wide variation in funding arrangements for fertility treatments globally is that current evaluation frameworks used by health-technology-assessment bodies are not fit-for-purpose for assessing the relative value/benefits associated with fertility treatments. This is fundamentally because most healthcare interventions aim to improve, extend or save the life of an existing individual, while fertility treatments are judged by their ability to create a new life.
Traditional health economic outcome measures, including quality-adjusted life-years (QALYs), are designed to value existing life and, therefore, do not adequately quantify health gains of a life that has not yet been created, and QALYs arguably cannot be improved by creating them [17, 18]. Furthermore, preference-based utility weights are designed to value health-related quality of life and much of the (dis)utility (harms and benefit) associated with having children are not health-related (e.g., carer burden, purpose/meaning in life). The variation in funding is also partly due to fertility treatment being considered as a somewhat discretionary good, despite infertility being a medical disease and reproduction being the most fundamental of human functions.
1.2 Discrete Choice Experiments (DCEs) in the Context of Fertility Treatment
Several stated-preference DCEs that assessed preferences for fertility treatments have been published [19,20,21,22,23,24,25,26,27,28,29,30], of which some elicited marginal willingness-to-pay (WTP) values for different attributes of fertility treatment [21, 23, 27,28,29,30] and, notably, one study comparing preferences across countries [29]. We are aware of only one application of DCEs to a fertility treatment context in Australia [28], which elicited taxpayer/societal preferences for fertility treatment and derived marginal WTP values for treatment attributes explored. A similar DCE survey has been administered to an ex post sample (i.e., women who have undergone or were undergoing fertility treatment), which is the focus of this study, providing the unique opportunity to compare preferences from a societal and ex post patient perspective. Understanding preferences of patients for fertility treatment and the impact of changes in treatment costs on their demand is important because most women undergo multiple ART treatment cycles, particularly if previous cycles have been unsuccessful. Therefore, insights about preferences of patients who have experienced fertility treatment can help inform funding policies and the treatment configuration that best captures and reflects the patients’ voice and the ex post value of fertility treatment to patients (rather than to those who have never experienced treatment or the general public). The importance of incorporating patient experiences and preferences (co-design) in health policy and reimbursement decisions are key principles of contemporary health technology assessment [31].
1.3 Price Elasticities of Demand
Price elasticities indicate the percentage change in the quantity demanded for every 1% change in price. Goods and services with an elasticity of demand less than − 1 are classified as having elastic demand, whereas elasticities of demand between − 1 and 0 indicate inelastic demand [32]. For policymakers, insurance companies and fertility treatment providers it is important to understand how strongly patients react to changes in treatment cost, with price elasticities being critical for understanding the change in consumer demand. Price elasticities are used by health insurers and providers for resource planning, informing the quantity of displaced treatment under constrained budgets, and regulating demand through pricing.
There is limited literature on price elasticities for fertility treatments which are based on either survey data from WTP studies [33] or empirical market data including changes in the quantity demanded due to the introduction of a policy intervention [34,35,36,37,38].
1.4 Objectives
This study aimed to derive price elasticities of demand for fertility treatment and marginal WTP values for its key characteristics, by applying the results of a DCE conducted with women who had undergone or were undergoing fertility treatment (i.e., ex post perspective).
2 Methods
2.1 Design of the DCE
A DCE conducted in Australia in 2018 asked women to choose their preferred treatment in 12 hypothetical choice scenarios describing two fertility treatments. The unlabelled treatments related to a single fertility treatment cycle and were defined by seven attributes: success rates, side effects, counselling/peer support, treatment journey, continuity of care, availability of experimental treatment, and out-of-pocket cost (Online Supplemental Material (OSM) Table A). Fertility treatment attributes used in the DCE were identified through qualitative work [39,40,41,42], including reviewing relevant literature and conducting three focus group discussions (two with members of the general population and one with patients at a large fertility clinic in Sydney, Australia). This qualitative work has been described in more detail previously [28, 43]. Briefly, three broad categories of attributes have been identified from the literature: (1) outcome attributes (e.g., treatment effectiveness), (2) process attributes (e.g., continuity of care), and (3) cost attribute. These findings were supported by information provided in focus group discussions and expert consultations (including two fertility doctors, one fertility nurse and one women’s health academic).
An online pilot study has been conducted with 31 participants to validate the appropriateness of the seven fertility treatment attributes and their levels identified through qualitative work, and these were iteratively revised for clarity until consensus was reached on their framing and wording among the researchers performing the study. Women participating in the pilot study were recruited from a market research company’s (Survey Sampling International) general population panel who had previously undergone or were undergoing fertility treatments to conceive (i.e., ex post perspective). A questionnaire similar to the one used for the main study, including 12 choice tasks, was administered to participants in the pilot study. Results from the pilot study provided prior information on preferences, which informed the fractional experimental design of the final survey for the main study. Furthermore, theoretical validity was explored by confirming that the cost attribute had the expected negative sign, and an additional consistency check was performed confirming that participants did not choose a dominated option (30 participants chose the dominant treatment and one participant chose neither treatment in the choice task used for the consistency check).
2.2 Data
The DCE used a D-efficient Bayesian fractional experimental design and was administered to a sample of 376 women who had previously undergone or were undergoing fertility treatments to conceive (i.e., ex post perspective), recruited from the same market research general population panel as used for the pilot. The questionnaire consisted of a consent form, instructions (including an explanation of the context of the survey, the attributes and their levels, as well as an example choice task), 12 choice tasks, and additional follow-up questions about the difficulty of the choice tasks and respondents’ socio-demographic characteristics. An example choice task is displayed in Fig. 1 and OSM section B includes a sample questionnaire.
The cost attribute had five levels, $40, $600, $4,000, $8,000 or $10,000 in out-of-pocket (OOP) costs (in AU$), respectively, which reflect the range of OOP costs for different types of fertility treatment in Australia (e.g., approximately $40 for a medical prescription for ovulation induction medication to $10,000 for a non-subsidized ART treatment cycle). This cost of treatment variation allowed the calculation of price elasticities of demand for fertility treatment. In addition, information on socio-demographic characteristics was collected, including annual family income before any tax deductions, which was used to control for the impact of income on treatment demand. Ethics approval was obtained from the University of New South Wales, Sydney (HC17255).
2.3 Regression Analysis
According to random utility theory, the utility of an individual i derived from choosing alternative j (Treatment A, B or neither) in choice set t is given by:
where Uijt is the utility, Xijt is a vector of variables representing attributes of alternative j, and \(\beta\) is a vector of coefficients. \({X}_{ijt}\beta\) is the deterministic component, \({\varepsilon }_{ijt}\) the random component, ni the number of respondents, and nt is the number of choice scenarios. We assumed a linear and additive deterministic component as follows:
where \(\beta_{1} \left( {\text{side effects}} \right)\) to \(\beta_{7} \left( {{\text{costs}}} \right)\) are marginal utilities showing individuals’ preferences for fertility treatment attributes and levels. In each of the 12 hypothetical choice scenarios of the DCE participants had to choose their preferred treatment –treatment A, treatment B, or neither. We regressed participants’ choices in each choice task on the levels of each fertility treatment attribute. All attributes were included as categorical variables except for the success rate and treatment costs, which were included as continuous variables. To determine an appropriate regression model, we tested for non-linearity of the cost and success rate attributes (results of these tests are shown in OSM Figs. A1 and A2). Effects coding was used for categorical variables [44]. Given that the DCE was unlabelled, we included alternative-specific constants (ASCs) for choosing treatment A (ASCa) as well as the “Neither” option (ASCn) in our model specifications to capture whether individuals derive (dis)utility from systematically choosing treatment A or neither treatment, respectively.
We first used a main-effects multinomial logit (MNL) model to analyze DCE responses and progressed from there to a main-effects random parameter logit (RPL) model and, finally, to an RPL model also including interaction effects between family income and the treatment cost attribute to control for income effects. Coefficients for attribute levels were assumed to follow a normal distribution except for the cost attribute where we assumed a log-normal distribution. Income was measured as a categorical variable and we assumed a linear shift in the cost coefficient depending on the income category. The models were compared based on goodness-of-fit measures, including log-likelihood, Akaike information criterion (AIC), Bayesian information criterion (BIC), and adjusted Rho-square. The most preferred model was used to derive relative preference weights and the conditional relative importance of each attribute. Preference weights are reflective of respondents’ relative strength of preferences for attribute levels, with higher preference weights associated with more preferred attribute levels. To derive the conditional relative importance of each attribute we first calculated the difference between the preference weights on the most influential attribute level and the least influential attribute level. These differences were then summed across attributes and the sum scaled to 100. Finally, the conditional relative importance of each attribute was calculated as a percentage of this total. Variables were considered to have a significant effect on the preferred treatment choice if the ρ-value was less than 0.05.
The RPL regression model results were also used to determine marginal WTP for the fertility treatment attributes and levels explored within the DCE (reported in AU$). Based on the RPL model, price elasticities of demand were derived to predict the change in demand after an increase in treatment costs. More specifically, price elasticities of demand were derived based on predictions for our data before and after increasing the price (i.e., cost attribute) for treatment A or treatment B by 1% in all choice sets (e.g., if the cost attribute was equal to $600 in OOP costs, it was increased to $606) where the alternatives in each choice set were treatment A, treatment B or neither. The predictions indicate the probability that an alternative is chosen in each choice scenario (i.e., observation) at the model estimates, and these can be summed across observations to derive the aggregated predicted demand [45]. By comparing the aggregated predicted demand before and after increasing the price, we were able to compute price elasticity estimates according to the following equation:
Equation 1 Price elasticity of demand formula
Marginal WTP values to accept an attribute level were derived based on the marginal rate of substitution with the payment vehicle (cost) attribute according to Equation 2 [46]. Due to the use of effects coding, we were able to derive marginal WTP values for all levels of each attribute included in the model as categorical variable. Therefore, the values reflect the marginal WTP to accept an attribute level. The marginal WTP for a change in attribute levels can be derived by determining the difference in marginal WTP values of the attribute levels to be compared.
Equation 2 Marginal rate of substitution with the payment vehicle (cost) attribute to derive marginal WTP values
In addition to the RPL regression model, we explored latent class (LC) analysis to identify whether treatment preferences vary across classes where class membership was based on family income and respondent age. The ideal number of classes is theoretically unknown [47], therefore, we explored models with up to six classes and an iterative procedure was used to retain four classes based on comparisons of the log-likelihood, AIC and BIC, after which an additional class did not significantly improve the model fit [48]. All analyses were conducted with the statistical software R, version 4.0.3 [49], and the Apollo package for choice model estimation [45, 50].
3 Results
3.1 Survey Respondents
A total of 376 female participants who underwent fertility treatment completed the DCE survey in September 2018, resulting in 4512 observations (376 participants × 12 hypothetical choice scenarios). On average, participants took 9 min to complete the survey. In 15.14% of choice scenarios the “Neither” option was chosen, 2.39% (n = 9) of participants chose the “Neither” option across all choice scenarios, and 56.12% of participants chose one of the two treatments across all choice scenarios. Most participants (80.85%) indicated that it was very easy, easy or OK to complete the DCE survey. OSM Table A2 presents the socio-demographic characteristics of participants.
Internal validity tests showed that respondents did not have a dominant preference, meaning that no respondent consistently chose the alternative that maximized or minimized the level of a particular attribute without considering the level of other attributes. Furthermore, 40 respondents were presented with a choice scenario where one treatment was dominant (i.e., given the objective ordering of attribute levels, the treatment was superior to the dominated treatment) and 37 (92.50%) respondents chose the dominant treatment, consistent with the theory of rational decision-making, while one respondent chose neither treatment and two respondents chose the dominated treatment.
3.2 Random Parameter Logit Model
Three models were compared: Main-effects MNL and RPL models (models 1 and 2), and RPL model with interaction effects between family income and the cost attribute (model 3). Model 3 was preferred based on goodness-of-fit measures.
The RPL regression results (Table 1) indicate that individuals derived utility from choosing a fertility treatment compared to not choosing a treatment (i.e., choosing the “Neither” option).
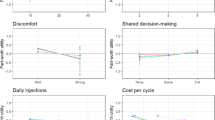
Figure 2 shows respondents’ relative strength of preferences for attributes and levels, and Fig. 3 shows the conditional relative importance of attributes used in the study. Respondents had strong preferences for a high treatment success rate and low OOP costs, with the success rate and cost attributes being the most preferred. These were followed by counselling/peer support, side effects, treatment journey, continuity of care, and availability of experimental treatment, in that order. Patients were willing to pay $383–$524 (range of point estimates across income categories) for one percentage point increase in the treatment success rate. Assuming OOP costs of approximately $7,000 for one IVF cycle in Australia, this means that women were prepared to pay 5–7% more in OOP costs for a one percentage point increase in the success rate. The utility derived from a change in the success rate from 10% to 40% was over three times the utility derived from a change from significant to negligible side effects. Patients were willing to pay $2,155–$2,952 and $3,526–$4,831 in order to avoid moderate and significant side effects from treatment, respectively.
Preference weights of fertility treatment attributes based on random parameter logit (RPL) model with interaction effects between treatment costs and patient family income (vertical bars indicate the 95% confidence interval (CI)). For categorical variables, the parameter estimates are the preference weights corresponding to the effects-coded attribute levels ranging from − 1 to 1. For continuous variables (success rate and out-of-pocket costs), the preference weights are the parameter estimates centered around the mean of parameter estimates for the attribute levels. The preference weights are log odds, which are distributed symmetrically around zero. The vertical bars surrounding each mean preference weight denote the 95% CI about the point estimate.
Conditional relative importance of fertility treatment attributes based on random parameter logit (RPL) model with interaction effects between treatment costs and patient family income. The conditional relative importance is the difference between the preference weights on the most influential attribute level and the least influential attribute level. These differences are summed across attributes and the sum is scaled to 100. The conditional importance of each attribute is a percentage of this total. The vertical bars surrounding each relative importance weight estimate denote the 95% confidence interval around the point estimate.
OSM Table A3 provides comparisons of preference weights for all levels of each attribute to provide more insights about changes in attribute levels. Individuals significantly preferred a treatment with counselling options on-site or without information on counselling options at all over a treatment providing information via brochures as well as a treatment with some level of personalization over a highly personalized treatment. In contrast, there was no significant difference between a treatment with continuity of care of doctors only compared with one without continuity of care of doctors and nurses. Patients either strongly preferred experimental treatments being offered or not being offered compared with them being considered if requested.
Price elasticities Our results suggest a price elasticity of – 0.0040 (95% confidence interval (CI): − 0.0039, − 0.0042), which is a point estimate across the whole range of prices explored within the DCE ($40–$10,000 in OOP costs). Similar price elasticity estimates were found when prices where increased for treatment B by 1%, indicating no choice bias in the DCE between treatments A and B (Table 2). These results suggest that fertility treatment demand was found to be highly inelastic to changes in cost of treatment.
Impact of income The coefficients for interactions between income and the cost attribute were not significant, indicating that income did not have a significant impact on fertility treatment demand.
3.3 Latent Class Model
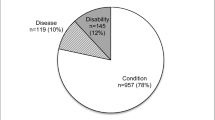
Table 3 and Figs. 4 and 5 present the results of a LC model with four classes. Class membership was not evenly distributed, with 6.56%, 51.32%, 26.34% and 15.79% of individuals belonging to classes 1–4, respectively.
Preference weights of fertility treatment attributes based on latent class (LC) model with 4 classes (vertical bars indicate the 95% confidence interval (CI)). For categorical variables, the parameter estimates are the preference weights corresponding to the effects-coded attribute levels ranging from − 1 to 1. For continuous variables (success rate and out-of-pocket costs), the preference weights are the parameter estimates centered around the mean of parameter estimates for the attribute levels. The preference weights are log odds, which are distributed symmetrically around zero. The vertical bars surrounding each mean preference weight denote the 95% CI about the point estimate.
Class distribution (left) and conditional relative importance of fertility treatment attributes (right) based on latent class model with four classes. The conditional relative importance is the difference between the preference weights on the most influential attribute level and the least influential attribute level. These differences are summed across attributes and the sum is scaled to 100. The conditional importance of each attribute is a percentage of this total. The vertical bars surrounding each relative importance weight estimate denote the 95% confidence interval around the point estimate.
None of the regression coefficients, except for significant side effects, were significant for individuals in class 1 (6.56%), and the level of side effects had a high conditional relative importance of 28.98% (95% CI 0.74, 57.22). Individuals in this class had a strong aversion for a treatment with significant side effects compared with moderate side effects, with a marginal WTP of $9,876 (95% CI $250.96, $19,501.61) to avoid significant side effects, and they did not differentiate between moderate and negligible side effects.
Class 2 individuals (51.32%) were risk-averse success-rate seekers. This class was characterized as having a strong preference for treatment with a high success rate and individuals were willing to pay $1,019.49 (95% CI $674.82, $1,364.16) per one percentage point increase in the success rate. The counselling and peer support attribute were less than half as important as the success rate attribute conditional on the attributes explored in the study. Class 2 individuals were indifferent to changes in the attributes for treatment journey, continuity of care, and the availability of alternative experimental treatments. Individuals in this class also derived utility from a treatment with lower costs. Compared with other classes, the price elasticity was low, indicating almost no decrease in the treatment demand if treatment costs increased by 1%.
Individuals in class 3 (26.34%) cared about all attributes explored in this study, with the cost and success rate attributes having the highest conditional relative importance. Attribute levels for the treatment journey and availability of experimental treatments were disordered, with some level of personalization and experimental treatments not being available significantly preferred over a high level of personalization and experimental treatments being considered on request, respectively (OSM Table A4). Individuals significantly preferred a treatment with lower costs.
Class 4 respondents (15.79%) seemed to be willing to sacrifice some treatment quality in exchange for lower costs. The continuity of care and cost attributes had the highest conditional relative importance. Respondents in this class significantly preferred a treatment with some level of personalization over a highly personalized treatment and were willing to pay an additional $6,724.12 (95% CI $1,812.44, $11,635.82) for some personalization. Patients in this class derived utility if the continuity of care attribute changed from patients being seen by the same doctor but different nurses to being seen by different doctors and nurses or same team of doctors and nurses at each visit. Patients either strongly preferred experimental treatments being offered or not being offered compared with them being considered if requested. The side effects, counselling and success rate attributes had the lowest conditional relative importance.
Table 3 presents the WTP results from the LC analysis in more detail. Furthermore, OSM Figs. A3 and A4 present class membership by family income category and respondent age. These figures indicate that 40% of class 2 individuals (risk-averse success-rate seekers) had an income ≥$100,000 and 55% of respondents were ≤ 40 years old. Interestingly, 35% of individuals in class 4, who seemed to be willing to sacrifice some treatment quality for lower costs, had an annual family income of at least $100,000 and respondents in this class tended to be younger, with 44% being aged 18–34 years and a further 20% being aged 35–40 years.
Price elasticities Elasticity estimates based on the LC model results ranged from − 0.00153 in class 2 to − 0.02321 in class 4 (Table 2). This indicates highly inelastic demand for fertility treatment with almost no impact on treatment demand when treatment costs increase by 1%.
4 Discussion
Based on the RPL and LC models, we derived price elasticity estimates for fertility treatment ranging from − 0.00153 to − 0.02461, which suggests highly inelastic demand. This suggests that changes in cost of fertility treatment had almost no impact on the demand for fertility treatment. This suggests that women value fertility treatment and having a baby highly. Compared with published estimates, the elasticity estimates from this study are mostly lower in magnitude, suggesting less elastic demand than most other studies, possibly due to different settings (countries) or using different methodologies and perspectives (ex ante or ex post) among other things. Among the publications reporting price elasticity estimates for fertility treatment summarized in OSM Table A5, only one study is based on stated-preference methods using contingent valuation. Unlike our results, elasticity estimates of the contingent valuation study suggest elastic demand for IVF and intrauterine insemination with the quantity demanded decreasing by 1.32–1.48% for every 1% increase in treatment costs [33]. Studies based on market data report more varied estimates: While some suggest elastic demand [34, 37], others report inelastic demand [35, 36] with positive price elasticities for some countries including Australia [36]. Similar to published price elasticity estimates for an Australian context, we also found inelastic demand for fertility treatment. However, in contrast to the positive estimates reported in the literature for Australia, our estimates seem to be more in line with economic theory assuming fertility treatments are ordinary goods (i.e., goods for which the quantity demanded decreases when price increases). We were not able to derive income elasticities for fertility treatment because income was not explicitly explored within the DCE and because it was measured on a categorical, instead of continuous, scale. However, our RPL regression model suggests no significant impact of income on treatment demand. In contrast, published literature reports a positive relationship between income or socio-economic status and treatment demand [37, 51,52,53], which is in line with economic theory that for most goods the quantity demanded increases with income.
In summary, our results suggest women are willing to pay high amounts for fertility treatment in the hope of having children regardless of their income level or ability to pay. This finding demonstrates the high value women place on their fertility and desire for a child. It also has implications for equity of access to fertility care with financial barriers likely to be a significant reason for women not being able to access much desired treatment if they cannot afford it.
Our study only included women who have undergone or were going through fertility treatment (ex post perspective), meaning they have been able to afford to undertake at least one treatment cycle, thus the initial financial barrier to commencing treatment was not experienced or was overcome. Furthermore, it is well recognized that many patients find it difficult to discontinue ART treatment because it signals they are giving up on their goal or dream of having a child [54, 55]. While further research should investigate how price-sensitive women are to entering the fertility market, these results might explain why women continue fertility treatment once they have commenced regardless of their financial capacity to pay.
Although participants were asked to make their choices as they would in real life, they were not asked to consider undergoing multiple cycles, which are often required to achieve a live birth (if at all). In reality, patients also make a decision about the number of treatment cycles to undergo, particularly if previous treatment attempts have been unsuccessful. It is likely that treatment costs and patient income are restrictive factors in this decision: An analysis of changes in public funding for IVF treatment in Australia suggested that a substantial proportion of patients were not able to afford the number of cycles they desire after a reduction in funding [56]. Therefore, future research should explore price elasticities for a likely treatment program of multiple cycles. Another limitation of our study is that the results might be affected by hypothetical bias, thereby limiting our ability to draw conclusions. Hypothetical bias could also be a reason why we were unable to find a significant effect of income on preferences if respondents under-stated the importance of the cost attribute. In this context, a recent systematic literature review and meta-analysis of DCEs in the healthcare sector found only moderate accuracy of DCEs for predicting health-related choices [57].
Perhaps unsurprisingly, our results show that infertile women who accessed or were going through fertility treatment generally derived utility from a treatment with high success rates, low costs, on-site counselling, negligible side effects, some personalization of the treatment journey, continuity of care of fertility doctors and nurses, and availability of experimental treatments, in that order conditional on the attributes and levels included in the study. This is mostly in line with the results of a recently published analysis of a similar DCE exploring preferences and marginal WTP for fertility treatment attributes from a societal/taxpayer perspective in Australia [28]. While taxpayers were willing to pay more for a treatment that considers or offers experimental add-on treatments compared with one where experimental treatments are not available, the patient perspective presented in this study indicates an aversion for a treatment considering experimental treatments if requested compared with a treatment where experimental treatments are either offered or not available. Furthermore, patients cared about the treatment journey and being offered some level of treatment personalization, whereas this attribute was not important for taxpayers. Latent class model results further suggest that approximately one-sixth of patients prefer not having continuity of care of doctors and nurses over continuity of care of doctors only. Given that price elasticity estimates for patients in this class were highest in magnitude, it might indicate a preference for low-cost fertility treatment. Patients would be willing to compromise on the treatment process in exchange for lower costs. Comparing our results to the broader literature suggests that marginal WTP values for some attributes of fertility treatment are similar across countries. For instance, our study indicated a marginal WTP value of $383–$524 across income categories for a one percentage point increase in the treatment success rate, which is comparable to values reported for European countries [23, 29, 58]. Given that other studies used different fertility treatment attributes, a direct comparison of the marginal WTP values is often not possible. However, the literature generally suggests a high marginal WTP for reducing the level of side effects or complications [21, 23], which is in line with our findings.
Interestingly, the preference weights for some attributes are often v-shaped, indicating disordering of attribute levels, which means that an objectively worse attribute was preferred. This suggests that patients had a strong preference for certain characteristics of treatment. For instance, patients either strongly preferred experimental treatments being offered or not being offered compared with them being considered if requested. This disordering might reflect that some patients actively seek experimental treatments hoping to increase their chances of having a baby even though their benefits are not supported by scientific evidence [59], whereas others prefer purely evidence-based treatment [60].
Similarly, disordering in the counselling attribute might have been due to a general disinterest in brochures, which is in line with evidence showing that patients rarely browse through or take home brochures [61]. Finally, some level of personalization was preferred over no or highly personalized treatment in our analysis, which could have been due to patients wanting to benefit from treatment personalization [62] without being overwhelmed by too many options [60, 63].
Knowing the responsiveness of demand for fertility treatments to changes in treatment cost is valuable information for policymakers, insurers and providers who regularly make decisions about treatment funding and pricing. Price increases deter women or couples from undergoing effective fertility treatment and price elasticity estimates can provide an indication of the quantity of treatments displaced due to policy interventions affecting funding.
5 Conclusion
Our study shows that infertile women who had previously undergone or were undergoing fertility treatment valued fertility treatment highly as reflected by highly price-inelastic demand. Success rate of treatment and out-of-pocket costs were the most important attributes, and largely determined patients’ WTP for fertility treatment relative to the attributes and levels used in the study. Income level had no significant effect on WTP for fertility treatment. While further research should investigate how price-sensitive women are to entering the fertility market, these results might explain why women continue fertility treatment once they have commenced despite their financial capacity to pay. Future research should also determine price elasticities for those who have not experienced fertility treatment for a fertility treatment program with multiple treatment cycles.
References
Zegers-Hochschild F, Adamson GD, De Mouzon J, Ishihara O, Mansour R, Nygren K, et al. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92(5):1520–4.
Inhorn MC, Patrizio P. Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update. 2015;21(4):411–26.
Cui W. Mother or nothing: the agony of infertility. Bull World Health Organ. 2010;88(12):881–2.
Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9(12): e1001356.
Cohen MA, Sauer MV. Fertility in Perimenopausal Women. Clin Obstet Gynecol. 1998;41(4):958–65.
Petraglia F, Serour GI, Chapron C. The changing prevalence of infertility. Int J Gynecol Obstet. 2013;123(S2):S4–8.
Levine H, Jørgensen N, Martino-Andrade A, Mendiola J, Weksler-Derri D, Mindlis I, et al. Temporal trends in sperm count: a systematic review and meta-regression analysis. Hum Reprod Update. 2017;23(6):646–59.
Newman JE, Paul RC, Chambers GM. Assisted reproductive technology in Australia and New Zealand 2019. Sydney; 2021.
Gameiro S, Boivin J, Peronace L, Verhaak CM. Why do patients discontinue fertility treatment? A systematic review of reasons and predictors of discontinuation in fertility treatment. Hum Reprod Update. 2012;18(6):652–69.
Adamson GD, de Mouzon J, Chambers GM, Zegers-Hochschild F, Mansour R, Ishihara O, et al. International Committee for Monitoring Assisted Reproductive Technology: world report on assisted reproductive technology, 2016 (preliminary) 2020 [updated 7 July 2020. https://secureservercdn.net/198.71.233.47/3nz.654.myftpupload.com/wp-content/uploads/ICMART-ESHRE-WR2016-FINAL-20200901.pdf. 15 April 2022.
Newman JE, Paul RC, Chambers GM. Assisted reproductive technology in Australia and New Zealand 2018. Sydney: National Perinatal Epidemiology and Statistics Unit, Unit NPEaS; 2020.
Chambers GM, Keller E, Choi S, Khalaf Y, Crawford S, Botha W, et al. Funding and public reporting strategies for reducing multiple pregnancy from fertility treatments. Fertil Steril. 2020;114(4):715–21.
Berg Brigham K, Cadier B, Chevreul K. The diversity of regulation and public financing of IVF in Europe and its impact on utilization. Hum Reprod. 2013;28(3):666–75.
Fertility Europe, European Society of Human Reproduction and Embryology. A Policy Audit on Fertility: Analysis of 9 EU Countries: March 2017. Brussels; 2017.
International Federation of Fertility Societies. IFFS Surveillance 2016. Glob Reprod Health. 2016;1: e1.
Australian Government Department of Health. Medicare benefits schedule book: operating from 1 august 2019. Canberra: Commonwealth of Australia; 2019.
Brown RCH. Irresponsibly infertile? Obesity, efficiency, and exclusion from treatment. Health Care Anal. 2019;27(2):61–76.
Devlin N, Parkin D. Funding fertility: Issues in the allocation and distribution of resources to assisted reproduction technologies. Hum Fertil. 2003;6:S2–6.
van Empel IWH, Dancet EAF, Koolman XHE, Nelen WLDM, Stolk EA, Sermeus W, et al. Physicians underestimate the importance of patient-centredness to patients: a discrete choice experiment in fertility care. Hum Reprod. 2011;26(3):584–93.
Goh ES-Y, Miller FA, Marshall DA, Ungar WJ. Genetic counselors’ preferences for coverage of preimplantation genetic diagnosis: a discrete choice experiment. Clin Genet. 2019;95(6):684–92.
Braam SC, de Bruin JP, Mol BWJ, van Wely M. The perspective of women with an increased risk of OHSS regarding the safety and burden of IVF: a discrete choice experiment. Human Reprod Open. 2020;2. 1-8
van den Wijngaard L, Rodijk ICM, van der Veen F, Gooskens-van Erven MHW, Koks CAM, Verhoeve HR, et al. Patient preference for a long-acting recombinant FSH product in ovarian hyperstimulation in IVF: a discrete choice experiment. Hum Reprod. 2015;30(2):331–7.
Abdulrahim B, Scotland G, Bhattacharya S, Maheshwari A. Assessing couples’ preferences for fresh or frozen embryo transfer: a discrete choice experiment. Hum Reprod. 2021;36(11):2891–903.
Weiss NS, Schreurs AMF, van der Veen F, Hompes PGA, Lambalk CB, Mol BW, et al. Women’s perspectives on ovulation induction with or without IUI as treatment for normogonadotrophic anovulation: a discrete choice experiment. Human Reprod Open. 2017;3. 1-7
van den Wijngaard L, van Wely M, Dancet EAF, van Mello NM, Koks CAM, van der Veen F, et al. Patients’ preferences for gonadotrophin-releasing hormone analogs in in vitro fertilization. Gynecol Obstet Invest. 2014;78(1):16–21.
Musters AM, de Bekker-Grob EW, Mochtar MH, van der Veen F, van Mello NM. Women’s perspectives regarding subcutaneous injections, costs and live birth rates in IVF. Hum Reprod. 2011;26(9):2425–31.
Huppelschoten AG, Verkerk EW, Appleby J, Groenewoud H, Adang EMM, Nelen WLDM, et al. The monetary value of patient-centred care: results from a discrete choice experiment in Dutch fertility care. Hum Reprod. 2014;29(8):1712–20.
Botha W, Donnolley N, Shanahan M, Norman RJ, Chambers GM. Societal preferences for fertility treatment in Australia: a stated preference discrete choice experiment. J Med Econ. 2019;22(1):95–107.
Skedgel C, Ralphs E, Finn E, Markert M, Samuelsen C, Whitty JA. How Do people with experience of infertility value different aspects of assistive reproductive therapy? Results from a multi-country discrete choice experiment. The Patient Patient-Centered Outcomes Res. 2022. 15 459-472
Loutfy M, Kennedy VL, Sanandaji M, Barry F, Ongoiba F, Muchenje M, et al. Pregnancy planning preferences among people and couples affected by human immunodeficiency virus: Piloting a discrete choice experiment. Int J STD AIDS. 2018;29(4):382–91.
Facey KM, Hansen HP, Single ANV. Patient involvement in health technology assessment. Singapore: Springer Nature Signapore Pte Ltd.; 2017.
Wiseman V. Demand and supply: measuring demand. In: Guinness L, Wiseman V, editors. Introduction to health economics. 2nd ed. Maidenhead: Open University Press; 2011. p. 55–68.
Darvishi A, Goudarzi R, Zadeh VH, Barouni M. Cost-benefit Analysis of IUI and IVF based on willingness to pay approach; case study: Iran. PLoS ONE. 2020;15(7): e0231584.
Hamilton BH, Jungheim E, McManus B, Pantano J. Health care access, costs, and treatment dynamics: evidence from in vitro fertilization. Am Econ Rev. 2018;108(12):3725–77.
Connolly MP, Griesinger G, Ledger W, Postma MJ. The impact of introducing patient co-payments in Germany on the use of IVF and ICSI: a price-elasticity of demand assessment. Hum Reprod. 2009;24(11):2796–800.
Chambers GM, Sullivan EA, Ishihara O, Chapman MG, Adamson GD. The economic impact of assisted reproductive technology: a review of selected developed countries. Fertil Steril. 2009;91(6):2281–94.
Chambers GM, Hoang VP, Sullivan EA, Chapman MG, Ishihara O, Zegers-Hochschild F, et al. The impact of consumer affordability on access to assisted reproductive technologies and embryo transfer practices: an international analysis. Fertil Steril. 2014;101(1):191–8.
Collins JA. An international survey of the health economics of IVF and ICSI. Hum Reprod Update. 2002;8(3):265–77.
Coast J, Al-Janabi H, Sutton EJ, Horrocks SA, Vosper AJ, Swancutt DR, et al. Using qualitative methods for attribute development for discrete choice experiments: issues and recommendations. Health Econ. 2012;21(6):730–41.
Vass C, Rigby D, Payne K. The role of qualitative research methods in discrete choice experiments: a systematic review and survey of authors. Med Decis Making. 2017;37(3):298–313.
Ikenwilo D, Heidenreich S, Ryan M, Mankowski C, Nazir J, Watson V. The best of both worlds: an example mixed methods approach to understand men’s preferences for the treatment of lower urinary tract symptoms. The Patient Patient-Centered Outcomes Res. 2018;11(1):55–67.
Katz DA, Stewart KR, Paez M, Vander Weg MW, Grant KM, Hamlin C, et al. Development of a discrete choice experiment (DCE) questionnaire to understand veterans’ preferences for tobacco treatment in primary care. The Patient Patient-Centered Outcomes Res. 2018;11(6):649–63.
Botha W, Donnolley N, Shanahan M, Chambers GM. Assessment of the societal and individual preferences for fertility treatment in Australia: study protocol for stated preference discrete choice experiments. BMJ Open. 2018;8: e020509.
Bech M, Gyrd-Hansen D. Effects coding in discrete choice experiments. Health Econ. 2005;14(10):1079–83.
Hess S, Palma D. Apollo version 0.2.6: User manual. 2019.
Mariel P, Hoyos D, Meyerhoff J, Czajkowski M, Dekker T, Glenk K, et al. Econometric modelling: basics. In: Environmental valuation with discrete choice experiments: guidance on design, implementation and data analysis. Lorraine Klimowich (Ed). Cham: Springer International Publishing; 2021, p. 61–81.
Hole AR. Discrete choice methods in health economics. Health econometrics. In: Contributions to economic analysis. Badi H. Baltagi and Francesco Moscone (Ed). 294. Emerald Publishing Limited; 2018, p. 85–99.
Goossens LMA, Utens CMA, Smeenk FWJM, Donkers B, van Schayck OCP, Rutten-van Mölken MPMH. Should i stay or should i go home? A latent class analysis of a discrete choice experiment on hospital-at-home. Value in Health. 2014;17(5):588–96.
R Core Team. R: a language and environment for statistical computing. 403rd ed. Vienna: R Foundation for Statistical Computing; 2020.
Hess S, Palma D. Apollo: A flexible, powerful and customisable freeware package for choice model estimation and application. J Choice Modell. 2019;32: 100170.
Bitler MP, Schmidt L. Utilization of infertility treatments: the effects of insurance mandates. Demography. 2011;49(1):125–49.
Chambers GM, Adamson GD, Eijkemans MJC. Acceptable cost for the patient and society. Fertil Steril. 2013;100(2):319–27.
Chambers GM, Hoang VP, Illingworth PJ. Socioeconomic disparities in access to ART treatment and the differential impact of a policy that increased consumer costs. Hum Reprod. 2013;28(11):3111–7.
Peddie VL, Van Teijlingen E, Bhattacharya S. A qualitative study of women’s decision-making at the end of IVF treatment. Hum Reprod. 2005;20(7):1944–51.
Copp T, Kvesic D, Lieberman D, Bateson D, McCaffery KJ. ‘Your hopes can run away with your realistic expectations’: a qualitative study of women and men’s decision-making when undergoing multiple cycles of IVF. Human Reprod Open. 2020;4. 1-8
Chambers GM, Hoang VP, Zhu R, Illingworth PJ. A reduction in public funding for fertility treatment—an econometric analysis of access to treatment and savings to government. BMC Health Serv Res. 2012;12(1):142.
Quaife M, Terris-Prestholt F, Di Tanna GL, Vickerman P. How well do discrete choice experiments predict health choices? A systematic review and meta-analysis of external validity. Eur J Health Econ. 2018;19(8):1053–66.
Palumbo A, De La Fuente P, Rodríguez M, Sánchez F, Martínez-Salazar J, Muñoz M, et al. Willingness to pay and conjoint analysis to determine women’s preferences for ovarian stimulating hormones in the treatment of infertility in Spain. Hum Reprod. 2011;26(7):1790–8.
Wilkinson J, Malpas P, Hammarberg K, Mahoney Tsigdinos P, Lensen S, Jackson E, et al. Do à la carte menus serve infertility patients? The ethics and regulation of in vitro fertility add-ons. Fertil Steril. 2019;112(6):973–7.
Perrotta M, Hamper J. The crafting of hope: contextualising add-ons in the treatment trajectories of IVF patients. Soc Sci Med. 2021;287: 114317.
Jansen CJM, Koops van’t Jagt R, Reijneveld SA, van Leeuwen E, de Winter AF, Hoeks JCJ. Improving health literacy responsiveness: a randomized study on the uptake of brochures on doctor-patient communication in primary health care waiting rooms. Int J Environ Res Public Health. 2021;18(9):5025.
Mol BW, Bossuyt PM, Sunkara SK, Garcia Velasco JA, Venetis C, Sakkas D, et al. Personalized ovarian stimulation for assisted reproductive technology: study design considerations to move from hype to added value for patients. Fertil Steril. 2018;109(6):968–79.
Human Fertilisation and Embryology Authority (HFEA). Pilot national fertility patient survey 2018. London; 2018.
Acknowledgements
The authors thank patients who agreed to participate in the DCE survey.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by an Australian National Health and Medical Research Council project grant (APP1104543) and a scholarship from the University of New South Wales School of Women’s and Children’s Health.
Conflicts of interest
GMC declares that the Fertility Society of Australia and New Zealand provides funding for the University of New South Wales (UNSW), Sydney, to manage the Australia and New Zealand Assisted Reproduction Database (ANZARD). GMC is the Data Custodian of ANZARD and an employee of UNSW. EK and WB report no conflicts of interest.
Ethics approval
Ethics approval was obtained from the University of New South Wales, Sydney (HC17255). The study has been performed in accordance with the ethical standards of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all respondents in the study.
Consent for publication (from patients)
The ethics approval covered consent to publish de-identified results from the data collected in the survey.
Data and/or code availability
The datasets generated during and/or analyzed during the current study are not publicly available due to ethical restrictions. A request for the code can be made directly to the corresponding author.
Authors’ contributions
All authors contributed to the study concept and design. WB and GC were responsible for the acquisition of data; EK undertook the data analyses. The first draft of the manuscript was written by EK and all authors commented on earlier versions of the manuscript. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Keller, E., Botha, W. & Chambers, G.M. What Features of Fertility Treatment do Patients Value? Price Elasticity and Willingness-to-Pay Values from a Discrete Choice Experiment. Appl Health Econ Health Policy 21, 91–107 (2023). https://doi.org/10.1007/s40258-022-00764-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-022-00764-7