Abstract
Background
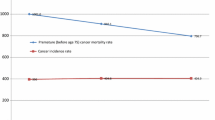
In Slovenia during the period 2000–2010, the number of years of potential life lost before the age of 70 years per 100,000 population under 70 years of age declined 25 %.
Objective
The aim of this study was to test the hypothesis that pharmaceutical innovation played a key role in reducing premature mortality from all diseases in Slovenia, and to examine the effects of pharmaceutical innovation on the age-standardized number of cancer deaths and on hospitalization from all diseases. Estimates and other data were used to calculate the incremental cost effectiveness of pharmaceutical innovation in Slovenia.
Method
Longitudinal disease-level data was analyzed to determine whether diseases for which there was greater pharmaceutical innovation—a larger increase in the number of new chemical entities (NCEs) previously launched—had larger declines in premature mortality, the age-standardized number of cancer deaths, and the number of hospital discharges. My methodology controls for the effects of macroeconomic trends and overall changes in the healthcare system.
Results
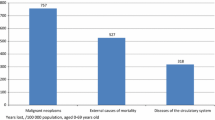
Premature mortality from a disease is inversely related to the number of NCEs launched more than 5 years earlier. On average, the introduction of an additional NCE for a disease reduced premature mortality from the disease by 2.4 % 7 years later. The age-standardized number of cancer deaths is inversely related to the number of NCEs launched 1–6 years earlier, conditional on the age-standardized number of new cancer cases diagnosed 0–2 years earlier. On average, the launch of an NCE reduced the number of hospital discharges 1 year later by approximately 1.5 %.
Conclusions
The estimates imply that approximately two-thirds of the 2000–2010 decline in premature mortality was due to pharmaceutical innovation. If no NCEs had been launched in Slovenia during 1992–2003, the age-standardized number of cancer deaths in 2008 would have been 12.2 % higher. The NCEs launched in Slovenia during 2003–2009 are estimated to have reduced the number of hospital discharges in 2010 by 7 %. If we assume that pharmaceutical expenditure was the only type of expenditure affected by pharmaceutical innovation, the cost per life-year saved was €3,953, which is well below even the lowest estimates of the value of a life-year saved. Moreover, 85 % of the increase in drug expenditure may have been offset by a reduction in hospital expenditure; therefore. the cost per life-year saved may have been only €611.










Similar content being viewed by others
Notes
See Gardner and Sanborn [1] for a discussion of the measurement and significance of YPLL.
A separate model is estimated for each value of k, rather than including multiple values (CUM_NCE i,t-1, CUM_NCE i,t-2, CUM_NCE i,t-3, …) in a single model because CUM_NCE is highly serially correlated (by construction), which would result in extremely high multicollinearity if multiple values were included).
The age-standardized number of cancer deaths is the age-standardized mortality rate × the population. Similarly, the age-adjusted number of new cancer cases diagnosed is the age-standardized incidence rate × the population. An age-standardized rate (ASR) is a summary measure of the rate that a population would have if it had a standard age structure. As indicated by the International Agency for Research on Cancer [15], standardization is necessary when comparing several populations that differ with respect to age because age has a powerful influence on the risk of cancer. The ASR is a weighted mean of the age-specific rates; the weights are taken from population distribution of the standard population. The most frequently used standard population is the World Standard Population.
Mortality data are reported in 5-year age groups in the WHO Mortality Database. The author has assumed that deaths in a 5-year age group occur at the midpoint of the age group. For example, the author has assumed that deaths at age 35–39 years occurred at age 37.5 years.
All of the models described in this article were estimated using the SAS GENMOD procedure [18]. Responses from different subjects were assumed to be statistically independent, and responses within subjects were assumed to be correlated. In the models whose estimates are reported in Table 1, the response variable was ln(YPLL70 it ), the link function was the identity function, and the correlation structure was independent. Estimates of models in which the response variable was ln(YPLL70 it ), the link function was the identity function, and the correlation structure was either exchangeable or first-order autoregressive were virtually identical to the estimates reported in Table 1.
In the models estimated, the response variable was N_DEATHS_STD st , the link function was the identity function, and the correlation structure was independent.
In the models estimated, the response variable was ln(DISCHARGES it ), the link function was the identity function, and the correlation structure was independent.
When we estimated a model in which the response variable was DISCHARGES it , the link function was the log function, and the correlation structure was independent; the magnitude of the point estimate of the coefficient on CUM_NCE i,t−1 was about twice as large: −0.0281 (Z = 2.07, p = 0.039). However, the convergence of this model was questionable.
According to the Merriam Webster dictionary, one definition of vintage is “a period of origin or manufacture (e.g. a piano of 1845 vintage)” [http://www.merriam-webster.com/dictionary/vintage]. Robert Solow [22] introduced the concept of vintage into economic analysis. Solow’s basic idea was that technical progress is ‘built into’ machines and other goods and that this must be taken into account when making empirical measurements of their roles in production. This was one of the contributions to the theory of economic growth that the Royal Swedish Academy of Sciences cited when it awarded Solow the 1987 Alfred Nobel Memorial Prize in Economic Sciences.
Outpatient prescription drug claims usually do not show the indication of the drug prescribed. Claims for drugs administered by doctors and nurses (e.g. chemotherapy) often show the indication of the drug. For the US, data from MEDSTAT MarketScan and IMS Health’s National Sales Perspectives indicate that approximately 70 % of cancer drug expenditure is on drugs administered by providers [23]. (Only 10 % of expenditure on other (non-cancer) drugs is on drugs administered by providers.) These data are not available for Slovenia.
Source: US Medical Expenditure Panel Survey, 2007 Full-Year Consolidated Data File. Lichtenberg [26] found that therapeutic procedure innovation increased the life expectancy of Western Australia hospital patients (whose mean life expectancy was approximately 10 years) by 2–3 months between 2000 and 2007. Since the fraction of the population that is hospitalized is fairly low, the implied contribution of hospital procedure innovation to aggregate longevity growth is fairly modest—much smaller than estimates of the contribution of pharmaceutical innovation to aggregate longevity growth.
The OECD also publishes estimates of YPLL before the age of 70 years per 100,000 population under 70 years of age. For unknown reasons, the OECD figures for Slovenia are quite a bit lower, but declined more rapidly, than the estimates based on WHO data. (The OECD figures for the US are also lower than estimates provided by the CDC [14] but the differences are not as great.) According to the OECD, YPLL before the age of 70 years per 100,000 population under 70 years of age declined by 1,684 (or 33 %), from 5,091 in 2000 to 3,407 in 2010. The OECD estimate of the absolute decline is only 11 % lower than the WHO-based estimate.
Aldy and Viscusi [34] estimated that, in the US, the average value of (willingness to pay for) a life-year is $300,000. Per capita gross domestic product (GDP) in Slovenia is just over half (53 %) of US per capita GDP; if the value of a statistical life-year (VSLY) was proportional to per capita GDP, the value of a statistical life-year in Slovenia might be $159,000 (=53 % × $300,000). However, Viscusi [35] argues that “estimates of the income elasticity of the value of a statistical life range from 0.5 to 0.6”: when income falls by 10 %, the value of a statistical life declines by only 5–6 %. This implies that the value of a statistical life-year in Slovenia might be $212,125 (=0.530.55 × $300,000).
References
Gardner JW, Sanborn JS. Years of potential life lost (YPLL): what does it measure? Epidemiology. 1990;1(4):322–9.
Rehm J, et al. Alcohol accounts for a high proportion of premature mortality in central and eastern Europe. Int J Epidemiol. 2007;36(2):458–467. http://ije.oxfordjournals.org/content/36/2/458.full. Accessed 9 Dec 2014.
Kolšek M. Primary health care European project on alcohol. Country report PHEPA II—Slovenia. 2009. http://www.gencat.cat/salut/phepa/units/phepa/html/en/dir360/doc8883.html. Accessed 9 Dec 2014.
Lichtenberg FR. The quality of medical care, behavioral risk factors, and longevity growth. Int J Health Care Fin Econ. 2011;11(1):1–34.
Lichtenberg FR. Contribution of pharmaceutical innovation to longevity growth in Germany and France, 2001–2007. Pharmacoeconomics. 2012;30(3):197–211.
Lichtenberg FR. Pharmaceutical innovation and longevity growth in 30 developing and high-income countries, 2000–2009. Health Policy Technol. 2014;3(1):36–58.
Semerl JS, Sesok J. Years of potential life lost and valued years of potential life lost in assessing premature mortality in Slovenia. Croat Med J. 2002;43(4):439–45.
Artnik B, Vidmar G, Javornik J, Laaser U. Premature mortality in Slovenia in relation to selected biological, socioeconomic, and geographical determinants. Croat Med J. 2006;47(1):103–13.
OECD. Premature mortality. In: Health at a glance 2011: OECD indicators. OECD Publishing. 2011. doi:10.1787/health_glance-2011-en. http://dx.doi.org/10.1787/health_glance-2011-5-en. Accessed 9 Dec 2014.
Murphy KM, Topel RH. The value of health and longevity. J Polit Econ. 2006;114(5):871–904.
Romer P. Endogenous technological change. J Polit Econ. 1990;98(5 Pt 2):S71–102.
Jones C. Introduction to economic growth. New York: Norton; 1998.
National Science Foundation. U.S. Corporate R&D. Vol. 1: Top 500 firms in R&D by industry category; 2012. http://www.nsf.gov/statistics/nsf00301/expendit.htm. Accessed 9 Dec 2014.
Centers for Disease Control, WISQARS. Years of potential life lost (YPLL) report, 1999 and later—NCIPC; 2013. http://webappa.cdc.gov/sasweb/ncipc/ypll10.html. Accessed 9 Dec 2014.
International Agency for Research on Cancer, EUREG. Glossary of terms. 2014. http://eco.iarc.fr/eureg/Glossary.aspx. Accessed 9 Dec 2014.
Centre National Hospitalier d’Information sur le Médicament. Thériaque database. 2014. http://www.theriaque.org/. Accessed 9 Dec 2014.
Steliarova-Foucher E, O’Callaghan M, Ferlay J, Masuyer E, Forman D, Comber H, et al. European Cancer Observatory: cancer incidence, mortality, prevalence and survival in Europe. Version 1.0 (September 2012). European Network of Cancer Registries, International Agency for Research on Cancer. 2013. http://eco.iarc.fr. Accessed 9 Dec 2014.
SAS Institute. The GENMOD procedure. 2014. http://support.sas.com/documentation/cdl/en/statug/63033/HTML/default/viewer.htm#genmod_toc.htm. Accessed 9 Dec 2014.
Lichtenberg FR, Pettersson B. The impact of pharmaceutical innovation on longevity and medical expenditure in Sweden, 1997–2010: evidence from longitudinal, disease-level data. Econo Innov New Technol. 2013;23(3):239–73.
Lichtenberg FR, Tatar M, Çalışkan Z. The effect of pharmaceutical innovation on longevity, hospitalization and medical expenditure in Turkey, 1999–2010. Health Policy. 2014;117(3):361–73.
Lichtenberg FR. The impact of pharmaceutical innovation on disability days and the use of medical services in the United States, 1997–2010. J Human Capital. 2014;8(4).
Solow RM. Investment and technological progress. In: Arrow K, Karlin S, Suppes P (eds.), Mathematical methods in the social sciences, 1959. Stanford University Press, Stanford; 1960: pp. 89–104.
Lichtenberg FR. Has medical innovation reduced cancer mortality? CESifo Econ Stud. 2014;60(1):135–77.
Lichtenberg FR. The impact of pharmaceutical innovation on longevity and medical expenditure in France, 2000–2009. Econ Hum Biol. 2014;13:107–27.
Food and Drug Administration. Drugs@FDA data files; 2014. http://www.fda.gov/Drugs/InformationOnDrugs/ucm079750.htm. Accessed 9 Dec 2014.
Lichtenberg FR. The impact of therapeutic procedure innovation on hospital patient longevity: evidence from Western Australia, 2000–2007. Social Sci Med. 2013;77:50–9.
Center for Medicare and Medicaid Services. National health expenditure data. 2014. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/tables.pdf. Accessed 9 Dec 2014.
Dorsey ER, et al. Financial anatomy of biomedical research, 2003–2008. JAMA. 2010;303(2):137–43.
Sampat BN, Lichtenberg FR. What are the respective roles of the public and private sectors in pharmaceutical innovation? Health Aff (Millwood). 2011;30(2):332–9.
OECD. OECD.Stat. http://stats.oecd.org. Accessed 9 Dec 2014.
Pennington M, Baker R, Brouwer W, Mason H, Hansen DG, Robinson A, et al.; the Eurovaq Team. Comparing WTP values of different types of QALY gain elicited from the general public. Health Econ. 2013. http://onlinelibrary.wiley.com/doi/10.1002/hec.3018/full. Accessed 9 Dec 2014.
Obradovic M, Mrhar A, Kos M. Cost-effectiveness analysis of HPV vaccination alongside cervical cancer screening programme in Slovenia. Eur J Public Health. 2010;20(4):415–21.
Braithwaite RS, Meltzer DO, King JT Jr, Leslie D, Roberts MS. What does the value of modern medicine say about the $50,000 per quality-adjusted life-year decision rule? Med Care. 2008;46(4):349–56.
Aldy JE, Viscusi WK. Adjusting the value of a statistical life for age and cohort effects. Rev Econ Stat. 2008;90(3):573–81.
Viscusi WK. The value of a statistical life: a critical review of market estimates throughout the world. J Risk Uncertain. 2003;27(1):5–76.
Eurostat. Causes of death—absolute number—annual data (table hlth_cd_anr). http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=hlth_cd_anr&lang=en. Accessed 18 Dec 2014.
Eurostat. Population on 1 January by age and sex (demo_pjan table). http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=demo_pjan&lang=en. Accessed 18 Dec 2014.
Eurostat. Hospital discharges by diagnosis, in-patients, total number (hlth_co_disch1 table). http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=hlth_co_disch1&lang=en. Accessed 18 Dec 2014.
World Health Organization. WHO Mortality Database. http://www.who.int/healthinfo/mortality_data/en/. Accessed 18 Dec 2014.
IMS Life Cycle New Product Focus. http://www.imshealth.com/deployedfiles/imshealth/Global/Content/Technology/Syndicated%20Analytics/Lifecycle%20and%20Portfolio%20Management/IMS_LifeCycle_New_Product_Focus_Global_Brochure%5B1%5D.pdf. Accessed 18 Dec 2014.
Thériaque. http://www.theriaque.org/. Accessed 18 Dec 2014.
Funding and conflict of interest
This research was supported by Mednarodni forum znanstvenoraziskovalnih farmacevtskih družb, GIZ /Forum of International R & D Pharmaceutical Companies, EIG. The sponsor placed no restrictions or limitations on data, methods, or conclusions, and had no right of review or control over the outcome of the research.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lichtenberg, F.R. The Impact of Pharmaceutical Innovation on Premature Mortality, Cancer Mortality, and Hospitalization in Slovenia, 1997–2010. Appl Health Econ Health Policy 13, 207–222 (2015). https://doi.org/10.1007/s40258-014-0144-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-014-0144-3