Abstract
Background
The role of aspirin in cardiovascular primary prevention remains controversial. Moreover, evidence for the potential benefits of aspirin in patients with high cardiovascular risk remains limited.
Objective
The aim of this study was to explore the role of low-dose aspirin in primary prevention.
Methods
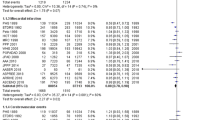
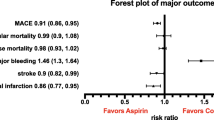
The PubMed, EMBASE, Cochrane Library, and ClinicalTrials.gov databases were searched for randomized clinical trials (RCTs) from the date of inception to August 2021. The efficacy outcomes were major adverse cardiovascular events (MACE), myocardial infarction (MI), ischemic stroke (IS), all-cause mortality, and cardiovascular mortality, whereas safety outcomes were major bleeding, intracranial hemorrhage, and gastrointestinal (GI) bleeding. Subgroup analyses were based on different cardiovascular risks and diabetes statuses. Pooled risk ratios (RRs) with 95% confidence intervals (CIs) were calculated using the fixed- and random-effects models, and trial sequential analysis (TSA) was conducted to determine the robustness of the results.
Results
A total of 10 RCTs fulfilled the inclusion criteria. The use of aspirin was associated with a significant reduction in the risk of MACE (RR 0.89, 95% CI 0.84–0.93), MI (RR 0.86, 95% CI 0.78–0.95), and IS (RR 0.84, 95% CI 0.76–0.93); however, aspirin also increased the risk of safety outcomes, i.e. major bleeding (RR 1.42, 95% CI 1.26–1.60), intracranial hemorrhage (RR 1.33, 95% CI 1.11–1.59), and GI bleeding (RR 1.91, 95% CI 1.44–2.54). Subgroup analyses revealed that in the absence of a statistically significant interaction, a trend toward a net benefit of lower incidence of cardiovascular events (number needed to treat of MACE: high risk: 682 vs. low risk: 2191) and lesser risk of bleeding events (number needed to harm of major bleeding: high risk: 983 vs. low risk: 819) was seen in the subgroup of high cardiovascular risk. Meanwhile, the greater MACE reduction was also detected in the high-risk group of diabetes or nondiabetes patients. Furthermore, a post hoc subgroup analysis indicated a significant rate reduction in patients aged ≤ 70 years but not in patients aged > 70 years. TSA confirmed the benefit of aspirin for MACE up to a relative risk reduction of 10%.
Conclusion
The current study demonstrated that the cardiovascular benefits of low-dose aspirin were equally balanced by major bleeding events. In addition, the potential beneficial effects might be seen in the population ≤ 70 years of age with high cardiovascular risk and no increased risk of bleeding.






Similar content being viewed by others
References
Dagenais GR, Leong DP, Rangarajan S, et al. Variations in common diseases, hospital admissions, and deaths in middle-aged adults in 21 countries from five continents (PURE): a prospective cohort study. Lancet. 2020;395:785–94.
Zhao D, Liu J, Wang M, et al. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16:203–12.
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2019;140:e596–646.
Jones WS, Mulder H, Wruck LM, et al. Comparative effectiveness of aspirin dosing in cardiovascular disease. N Engl J Med. 2021;384:1981–90.
Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324:71–86.
Gaziano JM, Brotons C, Coppolecchia R, et al. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. Lancet. 2018;392:1036–46.
Bowman L, Mafham M, Wallendszus K, et al. Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med. 2018;379:1529–39.
Mcneil JJ, Nelson MR, Woods RL, et al. Effect of Aspirin on All-Cause Mortality in the Healthy Elderly. N Engl J Med. 2018;379:1519–28.
Mcneil JJ, Wolfe R, Woods RL, et al. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med. 2018;379:1509–18.
Zheng SL, Roddick AJ. Association of aspirin use for primary prevention with cardiovascular events and bleeding events a systematic review and meta-analysis. JAMA. 2019;321:277–87.
Xie W, Luo Y, Liang X, et al. The efficacy and safety of aspirin as the primary prevention of cardiovascular disease: an updated meta-analysis. Ther Clin Risk Manag. 2019;15:1129–40.
Shah R, Khan B, Latham SB, et al. A meta-analysis of aspirin for the primary prevention of cardiovascular diseases in the context of contemporary preventive strategies. Am J Med. 2019;132:1295-1304.e3.
Lin M-H, Lee C-H, Lin C, et al. Low-dose aspirin for the primary prevention of cardiovascular disease in diabetic individuals: a meta-analysis of randomized control trials and trial sequential analysis. J Clin Med. 2019;8:609.
Gelbenegger G, Postula M, Pecen L, et al. Aspirin for primary prevention of cardiovascular disease: a meta-analysis with a particular focus on subgroups. BMC Med. 2019;17:198.
Nudy M, Cooper J, Ghahramani M, et al. Aspirin for primary atherosclerotic cardiovascular disease prevention as baseline risk increases a meta-regression analysis. Am J Med. 2020;133:1056–64.
Belch J, Maccuish A, Campbell I, et al. The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. BMJ. 2008;337: a1840.
Fowkes FG, Price JF, Stewart MC, et al. Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index: a randomized controlled trial. JAMA. 2010;303:841–8.
Masson W, Barbagelata L, Lavalle-Cobo A, et al. Low-doses aspirin in the primary prevention of cardiovascular disease in patients with diabetes: meta-analysis stratified by baseline cardiovascular risk. Diabetes Metab Syndr. 2022;16: 102391.
Masson G, Lobo M, Masson W, et al. Aspirin in primary prevention. Meta-analysis stratified by baseline cardiovascular risk. Arch Cardiol Mex. 2020;90:293–9.
Zhao B, Wu Q, Wang L, et al. Pros and cons of aspirin for the primary prevention of cardiovascular events: a secondary study of trial sequential analysis. Front Pharmacol. 2020;11: 592116.
Yusuf S, Joseph P, Dans A, et al. Polypill with or without aspirin in persons without cardiovascular disease. N Engl J Med. 2021;384:216–28.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339: b2700.
Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Guirguis-Blake JM, Evans CV, Senger CA, et al. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the us preventive services task force. Ann Intern Med. 2016;164:804–13.
Mahmoud AN, Gad MM, Elgendy AY, et al. Efficacy and safety of aspirin for primary prevention of cardiovascular events: a meta-analysis and trial sequential analysis of randomized controlled trials. Eur Heart J. 2019;40:607–17.
Piepoli MF, Hoes AW, Agewall S, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts): developed with the special contribution of the European Association for Cardiovascular Prevention and Rehabilitation (EACPR). Eur Heart J. 2016;37:2315–81.
Visseren FLJ, Mach F, Smulders YM, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42:3227–337.
Kulinskaya E, Wood J. Trial sequential methods for meta-analysis. Res Synth Methods. 2014;5:212–20.
Brok J, Thorlund K, Gluud C, et al. Trial sequential analysis reveals insufficient information size and potentially false positive results in many meta-analyses. J Clin Epidemiol. 2008;61:763–9.
Wetterslev J, Jakobsen JC, Gluud C. Trial sequential analysis in systematic reviews with meta-analysis. BMC Med Res Methodol. 2017;17:39.
Wetterslev J, Thorlund K, Brok J, et al. Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J Clin Epidemiol. 2008;61:64–75.
Kang H. Trial sequential analysis: novel approach for meta-analysis. Anesth Pain Med. 2021;16:138–50.
Saito Y, Okada S, Ogawa H, et al. Low-dose aspirin for primary prevention of cardiovascular events in patients with type 2 diabetes mellitus: 10-year follow-up of a randomized controlled trial. Circulation. 2017;135:659–70.
Ikeda Y, Shimada K, Teramoto T, et al. Low-dose aspirin for primary prevention of cardiovascular events in Japanese patients 60 years or older with atherosclerotic risk factors: a randomized clinical trial. JAMA. 2014;312:2510–20.
Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352:1293–304.
Roncaglioni MC. Low-dose aspirin and vitamin E in people at cardiovascular risk: a randomised trial in general practice. Lancet. 2001;357:89–95.
Meade TW, Wilkes HC, Kelleher CC, et al. Thrombosis prevention trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. Lancet. 1998;351:233–41.
Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351:1755–62.
Chinese Society of Cardiology of Chinese Medical Association, et al. Chinese guideline on the primary prevention of cardiovascular diseases [in Chinese]. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48:1000–38.
Anonymous. Aspirin use to prevent cardiovascular disease: preventive medication. Available at: www.uspreventiveservicestaskforce.org/uspstf/draft-recommendation/aspirin-use-to-prevent-cardiovascular-disease-preventive-medication#fullrecommendationstart.;375
Mahase E. US taskforce advises against low dose aspirin for primary prevention of cardiovascular disease. BMJ. 2021;375: n2521.
Draznin B, Aroda VR, Bakris G, et al. 10. Cardiovascular disease and risk management: standards of medical care in diabetes—2022. Diabetes Care. 2022;45:S144-s174.
Chen Y, Yin C, Li Q, et al. Misuse of aspirin and associated factors for the primary prevention of cardiovascular disease. Front Cardiovasc Med. 2021;8: 720113.
Christensen MB, Jimenez-Solem E, Ernst MT, et al. Low-dose aspirin for primary and secondary prevention of cardiovascular events in Denmark 1998–2018. Sci Rep. 2021;11:13603.
Hira RS, Gosch KL. Potential impact of the 2019 ACC/AHA guidelines on the primary prevention of cardiovascular disease recommendations on the inappropriate routine use of aspirin and aspirin use without a recommended indication for primary prevention of cardiovascular disease in cardiology practices: insights from the NCDR PINNACLE Registry. Circ Cardiovasc Qual Outcomes. 2022;15(3): e007979.
Kotseva K, De Backer G, De Bacquer D, et al. Primary prevention efforts are poorly developed in people at high cardiovascular risk: a report from the European Society of Cardiology EURObservational Research Programme EUROASPIRE V survey in 16 European countries. Eur J Prev Cardiol. 2021;28(4):370–9.
Maiello M, Cecere A, Zito A, et al. Low-dose aspirin for primary prevention of cardiovascular events in postmenopausal women with type-2 diabetes: the prescriptive approach in the real world. Int J Prev Med. 2021;12:140.
Bugiardini R, Pavasović S, Yoon J, et al. Aspirin for primary prevention of ST segment elevation myocardial infarction in persons with diabetes and multiple risk factors. EClinicalMedicine. 2020;27: 100548.
Joseph P, Roshandel G, Gao P, et al. Fixed-dose combination therapies with and without aspirin for primary prevention of cardiovascular disease: an individual participant data meta-analysis. Lancet. 2021;398:1133–46.
Baigent C, Blackwell L, Collins R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009;373:1849–60.
Burns RB, Pignone M, Michos ED. Would you recommend aspirin to this patient for primary prevention of atherosclerotic cardiovascular disease? Grand rounds discussion from Beth Israel Deaconess Medical Center. Ann Intern Med. 2021;174:1439–46.
Chou R, Dana T, Blazina I, et al. Statins for prevention of cardiovascular disease in adults: evidence report and systematic review for the US Preventive Services task force. JAMA. 2016;316:2008–24.
Oh YJ, Kim AJ, Ro H, et al. Low-dose aspirin was associated with an increased risk of cardiovascular events in patients with chronic kidney disease patients and low bodyweight: results from KNOW-CKD study. Sci Rep. 2021;11:6691.
Derry S, Loke YK. Risk of gastrointestinal haemorrhage with long term use of aspirin: meta-analysis. BMJ. 2000;321:1183–7.
Palmer RH. Risk of upper and lower gastrointestinal bleeding in patients taking nonsteroidal anti-inflammatory drugs, antiplatelet agents, or anticoagulants. Clin Gastroenterol Hepatol. 2015;13:2023–4.
Siller-Matula JM, Delle-Karth G. Addition of omeprazole to dual antiplatelet therapy with clopidogrel plus aspirin lowers the risk of upper gastrointestinal bleeding. Evid Based Med. 2011;16:144–5.
Ingram CA, Giang G, Mccrory K, et al. Yosprala: coordinated delivery of a proton pump inhibitor and aspirin. J Pharm Technol. 2020;36:78–83.
Khodayar S, Bardania H, Shojaosadati SA, et al. Optimization and characterization of aspirin encapsulated nano-liposomes. Iran J Pharm Res. 2018;17:11–22.
Mollace R, Gliozzi M, Macrì R. Efficacy and safety of novel aspirin formulations: a randomized, double-blind, placebo-controlled study. Pharmaceutics. 2022;14:187.
Rothwell PM, Cook NR, Gaziano JM, et al. Effects of aspirin on risks of vascular events and cancer according to bodyweight and dose: analysis of individual patient data from randomised trials. Lancet. 2018;392:387–99.
Christiansen M, Grove EL, Hvas A-M. Primary prevention of cardiovascular events with aspirin: toward more harm than benefit—a systematic review and meta-analysis. Semin Thromb Hemost. 2019;45:478–89.
Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003;326:219.
Harrington D, D’agostino RB Sr, Gatsonis C, et al. New guidelines for statistical reporting in the journal. N Engl J Med. 2019;381:285–6.
Bangalore S, Kumar S, Wetterslev J, et al. Angiotensin receptor blockers and risk of myocardial infarction: meta-analyses and trial sequential analyses of 147 020 patients from randomised trials. BMJ. 2011;342: d2234.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
As this was a systematic review of meta-analyses, no ethical approval was required.
Funding
The authors received no support from any organizations for the submitted work.
Conflict of interest
Mingming Wang, Haijie Yu, Zuojing Li, Daxin Gong, and Xiaoxi Liu have no financial or proprietary interests in any material discussed in this article.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors
Consent to participate
Not applicable (meta-analysis).
Consent for publication
Not applicable.
Code availability
Not applicable.
Data availability
The authors confirm that the data supporting the findings of this study are available in the article and its online supplementary material.
Author contributions
MW and HY were engaged in the design of the study, interpretation of the data, statistical analyses, and drafting of the manuscript. ZL and DG were responsible for data extraction, statistical analyses, interpretation of the data, and administrative and technical support. MW and XL were responsible for the conception and critical revision of the manuscript. All authors read and approved the final version of manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, M., Yu, H., Li, Z. et al. Benefits and Risks Associated with Low-Dose Aspirin Use for the Primary Prevention of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Randomized Control Trials and Trial Sequential Analysis. Am J Cardiovasc Drugs 22, 657–675 (2022). https://doi.org/10.1007/s40256-022-00537-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-022-00537-6