Abstract
Antithrombotic therapy is the cornerstone of pharmacological treatment in patients undergoing primary percutaneous coronary intervention (PCI). However, the acute management of ST elevation myocardial infarction (STEMI) patients includes therapy for pain relief and potential additional strategies for cardioprotection. The safety and efficacy of some commonly used treatments have been questioned by recent evidence. Indeed a concern about morphine use is the interaction between opioids and oral P2Y12 inhibitors; early beta-blocker treatment has shown conflicting results for the improvement of clinical outcomes; and supplemental oxygen therapy lacks benefit in patients without hypoxia and may be of potential harm. Other additional strategies remain disappointing; however, some treatments may be selectively used. Therefore, we intend to present a critical updated review of complementary pharmacotherapy for a modern treatment approach for STEMI patients undergoing primary PCI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The management of myocardial infarction includes complementary pharmacotherapy for pain relief and cardioprotection. |
The safety and efficacy of some commonly used treatments have been questioned by recent evidences. |
Considering the interaction between opioids and oral P2Y12 inhibitors, morphine administration should be reserved for those patients having persistent severe chest pain despite alternative analgesics which avoid opioids. |
Considering the results of therapies for cardioprotection, many drugs should not be part of routine standard care, but they should be wisely and selectively administered. |
Future research efforts need to focus on novel therapeutic approaches for improving clinical outcomes. |
In the current era of ST elevation myocardial infarction (STEMI) treatment, the “as soon as possible” therapies (“ASAP”) remain Aspirin, Second antiplatelet agent, Anticoagulant and of course Primary percutaneous coronary intervention. |
1 Introduction
Antithrombotic therapy, including antiplatelet and anticoagulant agents, is the cornerstone of pharmacological treatment in patients with ST elevation myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention (PCI) [1, 2]. However, the optimal treatment for pain relief and additional strategies for cardioprotection during the acute phase are debatable. Indeed, the safety and efficacy of some commonly used treatments have been questioned by recent evidence.
We intend to present a critical updated review of complementary pharmacotherapy for a modern treatment approach for STEMI patients undergoing primary PCI.
2 Early Pharmacological Treatment
2.1 Relief of Pain: Opioids
In STEMI patients, intravenous (IV) opioids such as morphine are largely used to relieve pain and anxiety. Opioids are also often used in patients with pulmonary congestion, as it is believed that they can also ameliorate dyspnea and favorably affect ventricular loading conditions through vasodilation. However, the evidence for these mechanisms is relatively poorly demonstrated [3]. The main concerns about morphine use is the interaction between opioids and oral P2Y12 inhibitors; indeed, opioids may delay the absorption of oral P2Y12 inhibitors by delaying gastric emptying, and therefore decreasing P2Y12 inhibitor plasma levels [4].
2.1.1 Interaction Between Opioids and P2Y12 Inhibitors
The pharmacokinetic and pharmacodynamic interaction between opioids and P2Y12 inhibitors has been shown for all the P2Y12 inhibitors in randomized settings (Table 1) [5,6,7,8,9] and in a cross-over study [10]; moreover, morphine use has been associated with delayed onset of action of both prasugrel and ticagrelor, without a difference between the two drugs [11].
The PERSEUS trial evaluated a head-to-head randomized comparison between fentanyl and morphine in STEMI patients requiring analgesia. The trial showed that patients who received fentanyl did not have higher platelet inhibition at 2 h after the ticagrelor loading dose [8]. However, fentanyl might have the potential to reduce the delay of absorption of ticagrelor, resulting in a higher platelet inhibition at 4 h, in comparison to morphine. Nevertheless, the results of this trial are hypothesis generating, considering the loss of statistical power attributable to premature study termination [8].
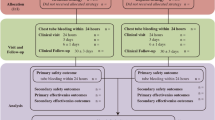
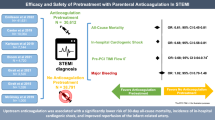
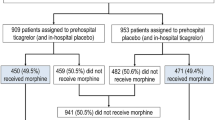
Further studies evaluated whether the effects of morphine on P2Y12 inhibitors may lead to a significant clinical effect. In the ATLANTIC trial, STEMI patients received a ticagrelor loading dose and in half of the cases (49.5%, n = 921) opioids (morphine in 97.6%). Morphine-treated patients had more frequently an absence of pre-PCI thrombolysis in myocardial infarction (TIMI) flow 3 compared to patients with no morphine administration (85.8% vs 79.7%; p = 0.001). In addition, morphine treatment was associated with increased glycoprotein IIb/IIIa inhibitor (GPI) use [12]. On the other hand, the French FAST-MI Registry showed that pre-hospital administration of morphine (n = 453, 19%) was not associated with a higher rate of in-hospital adverse complications or worse long-term survival. However, the rate of non-fatal recurrent myocardial infarction (MI) was higher in patients pretreated with morphine (1.8 vs 0.7%, p = 0.03) [13]. Similarly, in the CIRCUS trial, administration of IV morphine before angiography in half of STEMI patients (57.1%, n = 554) was not associated with a significant increase of major adverse cardiovascular events (MACE) at 1 year, but a non-significant trend towards an increase in the incidence of recurrent MI in the morphine group (3.8% vs 1.7%, p = 0.08) was demonstrated [14]. Interestingly, the use of morphine has been associated with the occurrence of ventricular tachycardia (VT) and ventricular fibrillation (VF) in anterior STEMI [15].
2.1.2 Alternative Analgesics that Avoid Opioids
Various studies searched for effective management of pain in STEMI patients with simultaneously fast and optimal platelet inhibition by investigating alternative analgesics that avoid opioids. The ON-TIME 3 trial compared IV acetaminophen with IV fentanyl in STEMI patients with ongoing chest pain, who all received crushed ticagrelor in a pre-hospital setting [9]. IV acetaminophen did not result in significantly lower platelet reactivity, but was associated with higher plasma concentrations of crushed ticagrelor at several time points and resulted in effective pain relief [9].
Opioid use is recommended by both the European and American STEMI guidelines [1, 2]. However, in the current European guideline, the class of the recommendation has been reduced from class I to IIa (level of evidence C), as a result of the increasing knowledge about the potential adverse effects of opioids. Recently, the US Food and Drug Administration (FDA) posted an official warning on the use of opioids in STEMI patients and recommended consideration of the use of a parenteral anti-platelet agent in acute coronary syndrome (ACS) patients requiring co-administration of morphine or other opioid agonists.
Pain relief remains a priority of any medical care; however, considering current data, morphine administration should be restricted as much as possible in the setting of acute MI. Alternative agents like acetaminophen may be considered, and morphine may be reserved for those having persistent severe chest pain despite the administration of acetaminophen.
2.2 Oxygen
Oxygen (O2) therapy has commonly been used in the initial treatment of patients with STEMI. Indeed, it seems plausible that enhancing O2 supply to an ischemic myocardium would lead to a beneficial effect attenuating ischemic tissue injury. However, evidence questioned the routine administration of supplemental O2 in the absence of hypoxemia. Although the mechanisms of the potential harm of supplemental O2 are not clearly elucidated, hyperoxia may decrease the activity of endothelium-derived vasodilators and may cause a reduction in coronary blood flow due to an increase in coronary vascular resistance [16].
In 2012, a small randomized trial found no difference in MI size in STEMI patients (n = 136) treated with high-concentration (6 L/min) or titrated O2 for 6 h after presentation [17]. The AVOID trial [18] demonstrated in 441 STEMI patients without hypoxia that the use of supplemental O2 (8 L/min) increased early myocardial injury (assessed with cardiac enzymes sampling), which led to a greater infarct size (assessed with cardiac magnetic resonance [CMR] at 6 months) and in more frequent recurrent MI and cardiac arrhythmia, compared to patients without supplemental O2. The subsequent SOCCER trial evaluated 95 STEMI patients and found no effect of high-flow O2 (10 L/min) on myocardial salvage index, myocardium at risk or infarct size at CMR performed 2–6 days after the inclusion, in comparison to patients with only room air [19]. The large DETO2X–AMI trial and its pre-specified subanalysis of STEMI patients (n = 2807) provided solid evidence for a lack of benefit of routine supplemental O2 therapy in normoxemic patients. In these patients, the administration of O2 (6 L/min for 6–12 h) resulted in no significant difference in 1-year clinical outcomes [20]. Moreover, in a subanalysis of DETO2X–AMI trial, O2 therapy compared with ambient air was not associated with improved outcomes regardless of baseline oxygen saturation [21].
In a meta-analysis including eight randomized controlled trials, supplemental O2 therapy was not associated with important clinical benefit in normoxemic patients with suspected or confirmed acute MI [22].
Finally, a recent pragmatic, cluster-randomized, crossover trial neither confirmed nor excluded difference in 30-day mortality from supplementary O2 in a subgroup of patients presenting with STEMI (odds ratio 0.81, 95% confidence interval 0.66–1.00) [23].
Based on the current evidence, supplemental O2 provides no clear benefit and there is no need to administer supplemental O2 in non-hypoxic (O2 saturation of ≥ 90% on pulse oximetry) STEMI patients undergoing primary PCI.
2.3 Nitrates
Most of the data available in literature about the use of nitrates in the setting of acute MI derive from the era before primary PCI had become the standard revascularization strategy.
In 1995, the large ISIS-4 trial demonstrated no significant benefit of nitrates on mortality [24]. The GISSI-3 trial confirmed the lack of beneficial effects of glyceryl trinitrate in acute MI patients, most of whom were treated with fibrinolysis [25].
In everyday clinical practice, nitrates can be useful in hypertensive and/or decompensated STEMI patients. During primary PCI, intracoronary (IC) administration of nitrates can be useful to counteract the component of vasoconstriction which is often present in STEMI patients. However, IV nitrates should be avoided in right ventricular (RV) infarction, in which nitrates may negatively impact the preload in patients who are particularly dependent upon preload for RV filling and for maintaining cardiac output. Furthermore, nitrates should be avoided in patients who have used phosphodiesterase type 5 (PDE5) inhibitors in the previous 48 h, as both drugs share a common mechanism of action in facilitating the release of nitric oxide (NO) and the synergistic lowering of blood pressure may put the patients at a high risk of developing severe hypotension.
Therefore, nitrates should be selectively administered and should not be part of a routine standard therapy in STEMI patients undergoing primary PCI.
3 Cardioprotective Pharmacotherapy
3.1 Beta-Blockers
Acute MI represents a state of reduced O2 supply to the affected portion of the myocardium. Early administration of IV beta-blocker, slowing the heart rate, reducing myocardial contractility, and lowering systemic blood pressure by the blockade of β1 receptors may be beneficial during MI as it results in reduced myocardial workload and O2 demand [26]. The cardioprotective effect associated with beta blockade seems to occur especially when the drug is given before coronary reperfusion [27], suggesting that beta-blockers might also have a role in reducing reperfusion injury, by targeting neutrophils and inhibiting neutrophil–platelet interactions in MI patients [28].
The effect of beta-blockers in STEMI patients undergoing primary PCI has been investigated in four randomized trials [29,30,31,32] (Table 2), which included patients in Killip class I or II and excluded patients with a low systolic blood pressure, a heart rate < 60 beats/min, or atrioventricular (AV) block type II or III. In the METOCARD-CNIC trial, 15 mg of IV metoprolol administered during transfer to PCI or at the emergency department in patients with anterior STEMI and Killip class I or II was associated with a reduced infarct size when compared to placebo [31]. Interestingly, a subanalysis [33] showed that beta-blockers have a greater cardioprotective effect (smaller infarct size) the sooner they are injected in the course of STEMI. Because myocardial necrosis is a time‐dependent ischemic process, the cardioprotective agent can be effective if administered when cellular ischemic death is not already complete. The time of administration of beta-blockers seems, therefore, fundamental; indeed, beta-blockers, when administered early, may slow the rate of myocardial death during ischemia by reducing myocardial O2 consumption.
However, the results of the METOCARD-CNIC trial were not confirmed by the EARLY-BAMI trial, in which STEMI patients were pre-treated twice with 5 mg of IV metoprolol (first bolus in ambulance and second bolus immediately before PCI) and showed no differences in terms of infarct size at CMR compared to placebo [32]. However, patients who received metoprolol had a lower incidence of malignant arrhythmias (3.6% in the metoprolol group vs 6.9% in the placebo group, p = 0.050) [32].
A patient-pooled meta-analysis of these trials showed that early administration of IV beta-blocker is safe, but no difference in the main outcome of 1-year death or MI was shown [34].
Considering the existing evidence, it seems reasonable and safe to administer beta-blockers early to hemodynamically stable and not bradycardic STEMI patients undergoing primary PCI. Whether higher doses of beta-blocker administered early may be beneficial should be explored in a further large trial.
3.2 Adenosine and Other Coronary Vasodilators
Adenosine is a potent direct vasodilator of coronary microcirculation. Data from animal models with MI suggested that adenosine and adenosine agonists could be myocardial protectants, although the molecular basis for acute adenosinergic cardioprotection remains incompletely understood [35]. The effect of periprocedural adenosine administration on myocardial perfusion and ventricular function in STEMI patients remains in controversy [36,37,38,39,40,41,42,43] (Table 3).
In the large AMISTAD-2 trial, adenosine showed a positive signal for reduction of infarct size [44], but improvement in clinical outcomes was confined to patients with early onset of MI [45]. Similarly, infarct size was significantly reduced by adenosine in those receiving early PCI (ischemia duration < 200 min) [46]. In the REOPEN-AMI trial [47], STEMI patients with TIMI flow grade 0–1 were randomly allocated 1:1:1 to receive adenosine, nitroprusside, or saline, and IC adenosine was shown to improve ST resolution (STR). The improvement in clinical outcomes did not reach statistical significance at 1 month, but adenosine reduced MACE rate at 1 year and was associated with less left ventricular (LV) negative remodeling [48]. Conversely, in the most recent REFLO-STEMI trial [49], IC adenosine (2–3 mg total) immediately following thrombectomy and stenting showed no significant difference in infarct size compared to nitroprusside or control. Moreover, a per-protocol analysis, suggested a potential harm of IC adenosine in terms of mid-term clinical outcomes.
In summary, adenosine has shown the potential to improve no-reflow in STEMI patients [50]; however, whether it can also limit infarct size and improve clinical outcomes is still not clearly proven. Interestingly, a recent meta-analysis of clinical studies undertaken in the primary PCI era suggests a beneficial effect of IC adenosine in terms of less heart failure (HF) following STEMI [51].
Importantly, while early reperfusion of the infarct-related artery may salvage a substantial amount of jeopardized myocardium, flow restoration also results in “reperfusion damage” due to production of oxygen free radicals, neutrophil activation, and endothelial damage. Therefore, ischemia and reperfusion both contribute to myocardial damage. Marzilli et al. [36] used a strategy for selective treatment of the ischemic territory right before the onset of reperfusion, injecting adenosine through the central lumen of an over-the-wire balloon catheter downstream of the obstruction. Adenosine, given distally to the coronary obstruction and before the onset of reperfusion, was associated with beneficial effects on coronary flow and ventricular function, potentially counteracting some of the mechanisms of reperfusion damage [36]. This may suggest that a protective agent should be administered downstream of the occlusion and prior to vessel reopening to be effective. It is also to be noted that the full therapeutic potential of adenosine may be limited by its ultra-short half-life and by possible dilution of the administered dose when delivered via a guiding or balloon catheter. Distal coronary administration of adenosine using a microinfusion catheter may be preferred, and a drug-releasing guidewire platform has been recently developed to allow continuous release of adenosine directly into the microvasculature during a PCI procedure [52].
Other vasodilators such as calcium channel blockers (verapamil, diltiazem, or nicardipine) during primary PCI have been evaluated in a limited number of studies. However, diltiazem or verapamil reverses no-reflow more effectively than nitroglycerin [53, 54]. Also, IC nitroprusside seems to reduce the incidence of angiographic no-reflow during primary PCI [55].
Nowadays, adenosine and other coronary vasodilators are not used routinely during primary PCI; however, they may be used in the attempt to reverse the no-reflow phenomenon on the basis of the potential benefit of the vasodilatation of microcirculation.
3.3 Agents Targeting Mitochondrial Permeability
Mitochondrial permeability transition is a key event in cell death and one of the mechanisms leading to reperfusion injury [56]; various adjunctive agents targeting mitochondria have been administered during the acute phase of MI as a potential cardioprotective strategy. In preclinical studies, many of these therapies were promising; however, most did not show clinical benefit in the clinical trials.
Cyclosporin-A, a mitochondrial permeability transition pore (mPTP) inhibitor, failed to protect the myocardium against reperfusion injury in STEMI patients and failed to improve hard clinical outcomes [57,58,59]. Also, the administration of TRO40303, another small-molecule mitochondria pore modulator that inhibits mPTP opening, did not show a reduction of the infarct size compared to placebo [59]. Moreover, elamipretide (MTP-131 or Bendavia), a cell-permeable peptide that preserves the integrity of cardiolipin, a phospholipid on the inner mitochondrial membrane, did not decrease myocardial infarct size in a sizable multicenter trial including STEMI due to a proximal or mid left anterior descending (LAD) lesion [60].
In conclusion, all the presented data show that complementary pharmacotherapies targeting mitochondria in STEMI patients treated with early primary PCI do not provide cardioprotection during the acute phase and are not able to improve clinical outcomes.
4 Ischemic Conditioning
Deep review of reperfusion injury is beyond the scope of this review; however, reperfusion injury could be mitigated through a process known as “conditioning,” which increases the tolerance of the myocardium to sustained ischemia by interrupting reperfusion with short inflation and deflation of the angioplasty balloon immediately after establishing perfusion, i.e., “ischemic post-conditioning.” Early studies suggested that post-conditioning may protect the human heart during acute MI [61], and subsequent small studies of STEMI patients have reported mixed results [62,63,64,65,66]. The largest study powered to detect a reduction in clinical endpoints, the DANAMI-3–iPOST trial [67], showed that ischemic post-conditioning was not superior to conventional primary PCI in terms of all-cause death and hospitalization for HF, in STEMI patients. “Remote ischemic conditioning,” which may also be established with cycles of reversible ischemia and reperfusion applied to a tissue far from the heart, had been a promising potential cardioprotective strategy [68,69,70,71]. Unfortunately, the recent and large CONDI-2/ERIC-PPCI trial [72], including 5401 STEMI patients, provided definitive evidence that remote ischemic conditioning offers no benefits regarding either myocardial infarct size or clinical outcomes.
5 Other Complementary Therapies at the Time of Reperfusion
N-acetylcysteine (NAC) is an antioxidant with reactive O2 species scavenging properties. In the LIPSIA-N-ACC trial [70], IV NAC did not reduce myocardial salvage index assessed with CMR. Conversely, the NACIAM trial [73] showed that NAC given at the moment of primary PCI with a background low dose of nitroglycerin reduced myocardial infarct size and increased myocardial salvage compared to placebo [73]. In another small randomized trial, NAC improved myocardial reperfusion markers (peak high sensitivity troponin T [hs-TnT]) and coronary blood flow (TIMI flow 3) [74]. However, these positive results need to be confirmed in larger studies with relevant clinical endpoints.
Exenatide, a glucagon-like-peptide-1 analog, administered at the time of reperfusion has been shown to increase myocardial salvage, but without improvement in clinical events at 30 days [75]. However, in the recent COMBAT-MI trial [76], exenatide alone or the combination of exenatide and remote ischemic conditioning were not able to reduce the infarct size.
6 Conclusions
Timely and complete reperfusion is the most effective way to improve cardiovascular outcomes in STEMI patients. Primary PCI together with early antithrombotic/antiplatelet therapy remains the cornerstone for achieving this goal. The implementation of additional strategies during the acute phase of STEMI for the improvement of clinical outcomes remains disappointing; however, some treatments may be used in selected patients (Figure 1). Beta-blockers may be administered in non-bradycardic and hemodynamically stable patients. Therapy with nitrates should be selectively administered in hypertensive or decompensated patients with LV MI and avoided in RV infarction. For pain relief, acetaminophen may be considered and morphine reserved for those patients having persistent severe chest pain despite acetaminophen. O2 should be given only in hypoxic patients, and adenosine (or other vasodilators such as calcium channel blockers or nitroprusside) should be given in an attempt to reverse the no-reflow phenomenon. Unfortunately, to date, other pharmacological approaches are not recommended because of a lack of efficacy. Future research efforts need to focus on novel therapeutic approaches to provide cardioprotection during the acute phase of STEMI.
References
Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77. https://doi.org/10.1093/eurheartj/ehx393.
Levine GN, Bates ER, Blankenship JC, et al. 2015 ACC/AHA/SCAI Focused Update on Primary Percutaneous Coronary Intervention for Patients With ST-Elevation Myocardial Infarction: an Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for t. Circulation. 2016;133(11):1135–47. https://doi.org/10.1161/CIR.0000000000000336.
Ellingsrud C, Agewall S. Morphine in the treatment of acute pulmonary oedema—Why? Int J Cardiol. 2016;202:870–3. https://doi.org/10.1016/j.ijcard.2015.10.014.
Silvain J, Storey RF, Cayla G, et al. P2Y12 receptor inhibition and effect of morphine in patients undergoing primary PCI for ST-segment elevation myocardial infarction The PRIVATE-ATLANTIC study. Thromb Haemost. 2016;116(2):369–78. https://doi.org/10.1160/TH15-12-0944.
Hobl E-L, Stimpfl T, Ebner J, et al. Morphine decreases clopidogrel concentrations and effects: a randomized, double-blind, placebo-controlled trial. J Am Coll Cardiol. 2014;63(7):630–5. https://doi.org/10.1016/j.jacc.2013.10.068.
Kubica J, Adamski P, Ostrowska M, et al. Morphine delays and attenuates ticagrelor exposure and actioninpatients with myocardial infarction: the randomized, double-blind, placebo-controlled IMPRESSION trial. Eur Heart J. 2016;37(3):245–52. https://doi.org/10.1093/eurheartj/ehv547.
McEvoy JW, Ibrahim K, Kickler TS, et al. Effect of Intravenous Fentanyl on Ticagrelor Absorption and Platelet Inhibition Among Patients Undergoing Percutaneous Coronary Intervention: the PACIFY Randomized Clinical Trial (Platelet Aggregation With Ticagrelor Inhibition and Fentanyl). Circulation. 2018;137(3):307–9. https://doi.org/10.1161/CIRCULATIONAHA.117.031678.
Iglesias JF, Valgimigli M, Carbone F, Lauriers N, Giorgio Masci P, Degrauwe S. Effects of fentanyl versus morphine on ticagrelor-induced platelet inhibition in patients with ST-segment elevation myocardial infarction. Circulation. 2020;142(25):2479–81. https://doi.org/10.1161/CIRCULATIONAHA.120.049287.
Tavenier AH, Hermanides RS, Ottervanger JP, et al. Impact of opioids on P2Y12 receptor inhibition in patients with ST-elevation myocardial infarction who are pre-treated with crushed ticagrelor: Opioids aNd crushed Ticagrelor In Myocardial infarction Evaluation (ON-TIME 3) trial. Eur Hear J Cardiovasc Pharmacother. 2020. https://doi.org/10.1093/ehjcvp/pvaa095.
Thomas MR, Morton AC, Hossain R, et al. Morphine delays the onset of action of prasugrel in patients with prior history of ST-elevation myocardial infarction. Thromb Haemost. 2016;116(1):96–102. https://doi.org/10.1160/TH16-02-0102.
Parodi G, Bellandi B, Xanthopoulou I, et al. morphine is associated with a delayed activity of oral antiplatelet agents in patients with ST-elevation acute myocardial infarction undergoing primary percutaneous coronary intervention. Circ Cardiovasc Interv. 2015. https://doi.org/10.1161/CIRCINTERVENTIONS.114.001593.
Lapostolle F, Van’t Hof AW, Hamm CW, et al. Morphine and Ticagrelor Interaction in Primary Percutaneous Coronary Intervention in ST-Segment Elevation Myocardial Infarction: ATLANTIC-Morphine. Am J Cardiovasc Drugs. 2019;19(2):173–183. https://doi.org/10.1007/s40256-018-0305-0
Puymirat E, Lamhaut L, Bonnet N, et al. Correlates of pre-hospital morphine use in ST-elevation myocardial infarction patients and its association with in-hospital outcomes and long-term mortality: the FAST-MI (French Registry of Acute ST-elevation and non-ST-elevation Myocardial Infarction) pr. Eur Heart J. 2016;37(13):1063–71. https://doi.org/10.1093/eurheartj/ehv567.
Bonin M, Mewton N, Roubille F, et al. Effect and safety of morphine use in acute anterior ST-segment elevation myocardial infarction. J Am Heart Assoc. 2018. https://doi.org/10.1161/JAHA.117.006833.
Sauer F, Jesel L, Marchandot B, et al. Life-threatening arrhythmias in anterior ST-segment elevation myocardial infarction patients treated by percutaneous coronary intervention: adverse impact of morphine. Eur Hear journal Acute Cardiovasc care. 2021;10(4):427–36. https://doi.org/10.1093/ehjacc/zuaa005.
Farquhar H, Weatherall M, Wijesinghe M, et al. Systematic review of studies of the effect of hyperoxia on coronary blood flow. Am Heart J. 2009;158(3):371–7. https://doi.org/10.1016/j.ahj.2009.05.037.
Ranchord AM, Argyle R, Beynon R, et al. High-concentration versus titrated oxygen therapy in ST-elevation myocardial infarction: a pilot randomized controlled trial. Am Heart J. 2012;163(2):168–75. https://doi.org/10.1016/j.ahj.2011.10.013.
Stub D, Smith K, Bernard S, et al. Air versus oxygen in ST-segment–elevation myocardial infarction. Circulation. 2015;131(24):2143–50. https://doi.org/10.1161/CIRCULATIONAHA.114.014494.
Khoshnood A, Carlsson M, Akbarzadeh M, et al. Effect of oxygen therapy on myocardial salvage in ST elevation myocardial infarction: the randomized SOCCER trial. Eur J Emerg Med. 2018;25(2):78–84. https://doi.org/10.1097/MEJ.0000000000000431.
Hofmann R, Witt N, Lagerqvist B, et al. Oxygen therapy in ST-elevation myocardial infarction. Eur Heart J. 2018;39(29):2730–9. https://doi.org/10.1093/eurheartj/ehy326.
James SK, Erlinge D, Herlitz J, et al. Effect of oxygen therapy on cardiovascular outcomes in relation to baseline oxygen saturation. JACC Cardiovasc Interv. 2020;13(4):502–13. https://doi.org/10.1016/j.jcin.2019.09.016.
Sepehrvand N, James SK, Stub D, Khoshnood A, Ezekowitz JA, Hofmann R. Effects of supplemental oxygen therapy in patients with suspected acute myocardial infarction: a meta-analysis of randomised clinical trials. Heart. 2018;104(20):1691–8. https://doi.org/10.1136/heartjnl-2018-313089.
Stewart RAH, Jones P, Dicker B, et al. High flow oxygen and risk of mortality in patients with a suspected acute coronary syndrome: pragmatic, cluster randomised, crossover trial. BMJ. 2021. https://doi.org/10.1136/bmj.n355.
ISIS-4: a randomised factorial trial assessing early oral captopril, oral mononitrate, and intravenous magnesium sulphate in 58,050 patients with suspected acute myocardial infarction. ISIS-4 (Fourth International Study of Infarct Survival) Collaborative. Lancet (London, England). 1995;345(8951):669–685. https://doi.org/10.1016/S0140-6736(95)90865-X
GRUPPOITALIANOPERLOSTUDIODELL. GISSI-3: effects of lisinopril and transdermal glyceryl trinitrate singly and together on 6-week mortality and ventricular function after acute myocardial infarction. Gruppo Italiano per lo Studio della Sopravvivenza nell’infarto Miocardico. Lancet (London, England). 1994;343(8906):1115–1122. https://doi.org/10.1016/S0140-6736(94)90232-1
López-Sendón J, Swedberg K, McMurray J, et al. Expert consensus document on beta-adrenergic receptor blockers. Eur Heart J. 2004;25(15):1341–62. https://doi.org/10.1016/j.ehj.2004.06.002.
Ibanez B, Cimmino G, Prat-González S, et al. The cardioprotection granted by metoprolol is restricted to its administration prior to coronary reperfusion. Int J Cardiol. 2011;147(3):428–32. https://doi.org/10.1016/j.ijcard.2009.09.551.
García-Prieto J, Villena-Gutiérrez R, Gómez M, et al. Neutrophil stunning by metoprolol reduces infarct size. Nat Commun. 2017;8(1):14780. https://doi.org/10.1038/ncomms14780.
Hanada K, Higuma T, Nishizaki F, et al. Randomized study on the efficacy and safety of landiolol, an ultra-short-acting β1-adrenergic blocker, in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention. Circ J. 2012;76(2):439–45. https://doi.org/10.1253/circj.cj-11-0947.
Er F, Dahlem KM, Nia AM, et al. Randomized Control of Sympathetic Drive With Continuous Intravenous Esmolol in Patients With Acute ST-Segment Elevation Myocardial Infarction: The BEtA-Blocker Therapy in Acute Myocardial Infarction (BEAT-AMI) Trial. JACC Cardiovasc Interv. 2016;9(3):231–40. https://doi.org/10.1016/j.jcin.2015.10.035.
Ibanez B, Macaya C, Sánchez-Brunete V, et al. Effect of early metoprolol on infarct size in ST-segment-elevation myocardial infarction patients undergoing primary percutaneous coronary intervention: the Effect of Metoprolol in Cardioprotection During an Acute Myocardial Infarction (METOCARD-CNIC) trial. Circulation. 2013;128(14):1495–503. https://doi.org/10.1161/CIRCULATIONAHA.113.003653.
Roolvink V, Ibáñez B, Ottervanger JP, et al. Early intravenous beta-blockers in patients with ST-segment elevation myocardial infarction before primary percutaneous coronary intervention. J Am Coll Cardiol. 2016;67(23):2705–15. https://doi.org/10.1016/j.jacc.2016.03.522.
García-Ruiz JM, Fernández-Jiménez R, García-Alvarez A, et al. Impact of the timing of metoprolol administration during STEMI on infarct size and ventricular function. J Am Coll Cardiol. 2016;67(18):2093–104. https://doi.org/10.1016/j.jacc.2016.02.050.
Hoedemaker NP, Roolvink V, de Winter RJ, et al. Early intravenous beta-blockers in patients undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a patient-pooled meta-analysis of randomized clinical trials. Eur Hear J Acute Cardiovasc Care. 2020;9(5):469–77. https://doi.org/10.1177/2048872619830609.
Headrick JP, Hack B, Ashton KJ. Acute adenosinergic cardioprotection in ischemic-reperfused hearts. Am J Physiol Circ Physiol. 2003;285(5):H1797–818. https://doi.org/10.1152/ajpheart.00407.2003.
Marzilli M, Orsini E, Marraccini P, Testa R. Beneficial effects of intracoronary adenosine as an adjunct to primary angioplasty in acute myocardial infarction. Circulation. 2000;101(18):2154–9. https://doi.org/10.1161/01.CIR.101.18.2154.
Petronio AS, De Carlo M, Ciabatti N, et al. Left ventricular remodeling after primary coronary angioplasty in patients treated with abciximab or intracoronary adenosine. Am Heart J. 2005;150(5):1015.1–1015.e9. https://doi.org/10.1016/j.ahj.2005.07.012
Stoel MG, Marques KMJ, de Cock CC, Bronzwaer JGF, von Birgelen C, Zijlstra F. High dose adenosine for suboptimal myocardial reperfusion after primary PCI: a randomized placebo-controlled pilot study. Catheter Cardiovasc Interv. 2007;71(3):283–9. https://doi.org/10.1002/ccd.21334.
Grygier M, Araszkiewicz A, Lesiak M, et al. New method of intracoronary adenosine injection to prevent microvascular reperfusion injury in patients with acute myocardial infarction undergoing percutaneous coronary intervention. Am J Cardiol. 2011;107(8):1131–5. https://doi.org/10.1016/j.amjcard.2010.12.010.
Desmet W, Bogaert J, Dubois C, et al. High-dose intracoronary adenosine for myocardial salvage in patients with acute ST-segment elevation myocardial infarction. Eur Heart J. 2011;32(7):867–77. https://doi.org/10.1093/eurheartj/ehq492.
Wang J, Chen Y-D, Zhi G, et al. Beneficial effect of adenosine on myocardial perfusion in patients treated with primary percutaneous coronary intervention for acute myocardial infarction. Clin Exp Pharmacol Physiol. 2012;39(3):247–52. https://doi.org/10.1111/j.1440-1681.2012.05668.x.
Zhang H, Tian N-L, Hu Z-Y, et al. Three hours continuous injection of adenosine improved left ventricular function and infarct size in patients with ST-segment elevation myocardial infarction. Chin Med J (Engl). 2012;125(10):1713–1719. http://www.ncbi.nlm.nih.gov/pubmed/22800889.
Fokkema ML, Vlaar PJ, Vogelzang M, et al. Effect of high-dose intracoronary adenosine administration during primary percutaneous coronary intervention in acute myocardial infarction. Circ Cardiovasc Interv. 2009;2(4):323–9. https://doi.org/10.1161/CIRCINTERVENTIONS.109.858977.109.858977.
Ross AM, Gibbons RJ, Stone GW, Kloner RA, Alexander RW. A Randomized, double-blinded, placebo-controlled multicenter trial of adenosine as an adjunct to reperfusion in the treatment of acute myocardial infarction (AMISTAD-II). J Am Coll Cardiol. 2005;45(11):1775–80. https://doi.org/10.1016/j.jacc.2005.02.061.
Kloner RA, Forman MB, Gibbons RJ, Ross AM, Alexander RW, Stone GW. Impact of time to therapy and reperfusion modality on the efficacy of adenosine in acute myocardial infarction: the AMISTAD-2 trial. Eur Heart J. 2006;27(20):2400–5. https://doi.org/10.1093/eurheartj/ehl094.
Garcia-Dorado D, García-del-Blanco B, Otaegui I, et al. Intracoronary injection of adenosine before reperfusion in patients with ST-segment elevation myocardial infarction: a randomized controlled clinical trial. Int J Cardiol. 2014;177(3):935–41. https://doi.org/10.1016/j.ijcard.2014.09.203.
Niccoli G, Rigattieri S, De Vita MR, et al. Open-Label, randomized, placebo-controlled evaluation of intracoronary adenosine or nitroprusside after thrombus aspiration during primary percutaneous coronary intervention for the prevention of microvascular obstruction in acute myocardial infarction. JACC Cardiovasc Interv. 2013;6(6):580–9. https://doi.org/10.1016/j.jcin.2013.02.009.
Niccoli G, Spaziani C, Crea F. Left ventricular remodeling and 1-year clinical follow-up of the REOPEN-AMI trial. J Am Coll Cardiol. 2014;63(14):1454–5. https://doi.org/10.1016/j.jacc.2013.10.042.
Nazir SA, McCann GP, Greenwood JP, et al. Strategies to attenuate micro-vascular obstruction during P-PCI: the randomized reperfusion facilitated by local adjunctive therapy in ST-elevation myocardial infarction trial. Eur Heart J. 2016;37(24):1910–9. https://doi.org/10.1093/eurheartj/ehw136.
Su Q, Nyi TS, Li L. Adenosine and verapamil for no-reflow during primary percutaneous coronary intervention in people with acute myocardial infarction. Cochrane database Syst Rev. 2015;5:CD009503. https://doi.org/10.1002/14651858.CD009503.pub3.
Bulluck H, Sirker A, Loke YK, Garcia-Dorado D, Hausenloy DJ. Clinical benefit of adenosine as an adjunct to reperfusion in ST-elevation myocardial infarction patients: an updated meta-analysis of randomized controlled trials. Int J Cardiol. 2016;202:228–37. https://doi.org/10.1016/j.ijcard.2015.09.005.
Forman MB, Brewer EC, Brown ZR, Menshikova EV, Lowman AM, Jackson EK. Novel guidewire design and coating for continuous delivery of adenosine during interventional procedures. J Am Heart Assoc. 2021. https://doi.org/10.1161/JAHA.120.019275.
Huang D, Qian J, Ge L, et al. REstoration of COronary flow in patients with no-reflow after primary coronary interVEntion of acute myocaRdial infarction (RECOVER). Am Heart J. 2012;164(3):394–401. https://doi.org/10.1016/j.ahj.2012.06.015.
Werner GS, Lang K, Kuehnert H, Figulla HR. Intracoronary verapamil for reversal of no-reflow during coronary angioplasty for acute myocardial infarction. Catheter Cardiovasc Interv. 2002;57(4):444–51. https://doi.org/10.1002/ccd.10375.
Zhao S, Qi G, Tian W, Chen L, Sun Y. Effect of intracoronary nitroprusside in preventing no reflow phenomenon during primary percutaneous coronary intervention: a meta-analysis. J Interv Cardiol. 2014;27(4):356–64. https://doi.org/10.1111/joic.12133.
Ong S-B, Samangouei P, Kalkhoran SB, Hausenloy DJ. The mitochondrial permeability transition pore and its role in myocardial ischemia reperfusion injury. J Mol Cell Cardiol. 2015;78:23–34. https://doi.org/10.1016/j.yjmcc.2014.11.005.
Cung T-T, Morel O, Cayla G, et al. Cyclosporine before PCI in patients with acute myocardial infarction. N Engl J Med. 2015;373(11):1021–31. https://doi.org/10.1056/NEJMoa1505489.
Ottani F, Latini R, Staszewsky L, et al. Cyclosporine A in Reperfused Myocardial Infarction: The Multicenter, Controlled, Open-Label CYCLE Trial. J Am Coll Cardiol. 2016;67(4):365–74. https://doi.org/10.1016/j.jacc.2015.10.081.
Upadhaya S, Madala S, Baniya R, Subedi SK, Saginala K, Bachuwa G. Impact of cyclosporine A use in the prevention of reperfusion injury in acute myocardial infarction: a meta-analysis. Cardiol J. 2017;24(1):43–50. https://doi.org/10.5603/CJ.a2016.0091.
Gibson CM, Giugliano RP, Kloner RA, et al. EMBRACE STEMI study: a Phase 2a trial to evaluate the safety, tolerability, and efficacy of intravenous MTP-131 on reperfusion injury in patients undergoing primary percutaneous coronary intervention. Eur Heart J. 2016;37(16):1296–303. https://doi.org/10.1093/eurheartj/ehv597.
Staat P, Rioufol G, Piot C, et al. Postconditioning the human heart. Circulation. 2005;112(14):2143–8. https://doi.org/10.1161/CIRCULATIONAHA.105.558122.
Tarantini G, Favaretto E, Marra MP, et al. Postconditioning during coronary angioplasty in acute myocardial infarction: the POST-AMI trial. Int J Cardiol. 2012;162(1):33–8. https://doi.org/10.1016/j.ijcard.2012.03.136.
Hahn J-Y, Song Y Bin, Kim EK, et al. Ischemic postconditioning during primary percutaneous coronary intervention: the effects of postconditioning on myocardial reperfusion in patients with ST-segment elevation myocardial infarction (POST) randomized trial. Circulation. 2013;128(17):1889-1896. doi:https://doi.org/10.1161/CIRCULATIONAHA.113.001690
Thibault H, Piot C, Staat P, et al. Long-term benefit of postconditioning. Circulation. 2008;117(8):1037–44. https://doi.org/10.1161/CIRCULATIONAHA.107.729780.
Laskey WK. Brief repetitive balloon occlusions enhance reperfusion during percutaneous coronary intervention for acute myocardial infarction: a pilot study. Catheter Cardiovasc Interv. 2005;65(3):361–7. https://doi.org/10.1002/ccd.20397.
Traverse JH, Swingen CM, Henry TD, et al. NHLBI-sponsored randomized trial of postconditioning during primary percutaneous coronary intervention for ST-elevation myocardial infarction. Circ Res. 2019;124(5):769–78. https://doi.org/10.1161/CIRCRESAHA.118.314060.
Engstrøm T, Kelbæk H, Helqvist S, et al. Effect of ischemic postconditioning during primary percutaneous coronary intervention for patients with ST-segment elevation myocardial infarction: a randomized clinical trial. JAMA Cardiol. 2017;2(5):490–7. https://doi.org/10.1001/jamacardio.2017.0022.
Stiermaier T, Jensen J-O, Rommel K-P, et al. Combined intrahospital remote ischemic perconditioning and postconditioning improves clinical outcome in ST-elevation myocardial infarction. Circ Res. 2019;124(10):1482–91. https://doi.org/10.1161/CIRCRESAHA.118.314500.
Gaspar A, Lourenço AP, Pereira MÁ, et al. Randomized controlled trial of remote ischaemic conditioning in ST-elevation myocardial infarction as adjuvant to primary angioplasty (RIC-STEMI). Basic Res Cardiol. 2018;113(3):14. https://doi.org/10.1007/s00395-018-0672-3.
McLeod SL, Iansavichene A, Cheskes S. Remote ischemic perconditioning to reduce reperfusion injury during acute ST-segment-elevation myocardial infarction: a systematic review and meta-analysis. J Am Heart Assoc. 2017. https://doi.org/10.1161/JAHA.117.005522.
Crimi G, Pica S, Raineri C, et al. Remote ischemic post-conditioning of the lower limb during primary percutaneous coronary intervention safely reduces enzymatic infarct size in anterior myocardial infarction: a randomized controlled trial. JACC Cardiovasc Interv. 2013;6(10):1055–63. https://doi.org/10.1016/j.jcin.2013.05.011.
Hausenloy DJ, Kharbanda RK, Møller UK, et al. Effect of remote ischaemic conditioning on clinical outcomes in patients with acute myocardial infarction (CONDI-2/ERIC-PPCI): a single-blind randomised controlled trial. Lancet (London, England). 2019;394(10207):1415–24. https://doi.org/10.1016/S0140-6736(19)32039-2.
Pasupathy S, Tavella R, Grover S, et al. Early use of N-acetylcysteine with nitrate therapy in patients undergoing primary percutaneous coronary intervention for ST-segment-elevation myocardial infarction reduces myocardial infarct size (the NACIAM trial [N-acetylcysteine in acute myocardial inf. Circulation. 2017;136(10):894–903. https://doi.org/10.1161/CIRCULATIONAHA.117.027575.
Nozari Y, Eshraghi A, Talasaz AH, et al. Protection from reperfusion injury with intracoronary N-acetylcysteine in patients with STEMI undergoing primary percutaneous coronary intervention in a cardiac tertiary center. Am J Cardiovasc Drugs. 2018;18(3):213–21. https://doi.org/10.1007/s40256-017-0258-8.
Lønborg J, Vejlstrup N, Kelbæk H, et al. Exenatide reduces reperfusion injury in patients with ST-segment elevation myocardial infarction. Eur Heart J. 2012;33(12):1491–9. https://doi.org/10.1093/eurheartj/ehr309.
García Del Blanco B, Otaegui I, Rodríguez-Palomares JF, et al. Effect of COMBinAtion therapy with remote ischemic conditioning and exenatide on the Myocardial Infarct size: a two-by-two factorial randomized trial (COMBAT-MI). Basic Res Cardiol. 2021;116(1):4. https://doi.org/10.1007/s00395-021-00842-2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this article.
Conflict of interest
Dr. E. Kedhi reports personal fees from Abbott and personal fees from Medtronic, outside this submitted work; Dr. A. van't Hof reports grants from Medtronic, Abbott, Boehringer Ingelheim, and AstraZeneca, all outside this submitted work; Dr. E. Fabris, A. Selvarajah, A. Tavenier, R. Hermanides, and G. Sinagra have declared no potential conflicts of interest that might be relevant to this work.
Author contributions
All authors have contributed significantly to the paper, in particular: EF, AvH: conception and design of paper; EF: drafting of the manuscript; AS, AT, RH, EK, GS, and AvH: revising critically the manuscript for important intellectual content.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Fabris, E., Selvarajah, A., Tavenier, A. et al. Complementary Pharmacotherapy for STEMI Undergoing Primary PCI: An Evidence-Based Clinical Approach. Am J Cardiovasc Drugs 22, 463–474 (2022). https://doi.org/10.1007/s40256-022-00531-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-022-00531-y