Abstract
Background
The newer P2Y12 inhibitors have better efficacy than clopidogrel. However, whether ticagrelor or prasugrel have a better comparative safety and efficacy profile, especially in the long-term, remains inconclusive.
Objective
We compared prasugrel and ticagrelor in patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI).
Methods
MEDLINE and the Cochrane library were queried for randomized controlled trials (RCTs) or observational studies comparing prasugrel with ticagrelor in patients with ACS undergoing PCI. Random-effects pooling was used to calculate odds ratios (ORs) with 95% confidence intervals (CI). Analyses were stratified by duration of follow-up (short term [≤ 3 months] and long term [≥ 1 year]) and study design.
Results
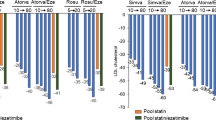
In total, 14 studies (six RCTs, eight observational studies), including 40,188 patients, met eligibility criteria. Pooled analysis did not indicate that prasugrel significantly decreased all-cause mortality compared with ticagrelor in the short term (OR 0.49; 95% CI 0.20–1.20; p = 0.11) or long term (OR 0.74; 95% CI 0.48–1.15; p = 0.38). Pooled observational studies showed significantly lower long-term all-cause mortality (OR 0.63; 95% CI 0.43–0.92; p = 0.02) and short-term stent thrombosis (OR 0.46; 95% CI 0.28–0.75; p = 0.002) with prasugrel. No significant difference was observed in the risk of nonfatal myocardial infarction, ischemic stroke, bleeding, or repeat revascularization between the two groups. Results remained similar after stratification according to follow-up and study design.
Conclusions
The present analysis suggests that prasugrel might have a better efficacy profile than ticagrelor in patients with ACS undergoing PCI. However, this advantage was only seen in pooled observational studies and is likely to be affected by selection bias.


Similar content being viewed by others
References
Mauri L, Kereiakes DJ, Yeh RW, Driscoll-Shempp P, Cutlip DE, Steg PG, et al. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med. 2014;371(23):2155–66. https://doi.org/10.1056/NEJMoa1409312.
Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045–57. https://doi.org/10.1056/NEJMoa0904327.
Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357(20):2001–15. https://doi.org/10.1056/NEJMoa0706482.
Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease. J Am Coll Cardiol. 2016;68(10):1082.
Valgimigli M, Bueno H, Byrne RA, Collet J-P, Costa F, Jeppsson A, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTSThe Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2018;39(3):213–60. https://doi.org/10.1093/eurheartj/ehx419.
Watti H, Dahal K, Zabher HG, Katikaneni P, Modi K, Abdulbaki A. Comparison of prasugrel and ticagrelor in patients with acute coronary syndrome undergoing percutaneous coronary intervention: a meta-analysis of randomized and non-randomized studies. Int J Cardiol. 2017;249:66–72. https://doi.org/10.1016/j.ijcard.2017.07.103.
Motovska Z, Hlinomaz O, Kala P, Hromadka M, Knot J, Varvarovsky I, et al. 1-Year outcomes of patients undergoing primary angioplasty for myocardial infarction treated with prasugrel versus ticagrelor. J Am Coll Cardiol. 2018;71(4):371–81. https://doi.org/10.1016/j.jacc.2017.11.008.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Higgins JPT, Green S (editors). Cochrane handbook for systematic reviews of interventions version 5.1.0 The Cochrane Collaboration; 2011. http://www.handbook.cochrane.org. Accessed 4 Oct 2018.
Rao G, Lopez-Jimenez F, Boyd J, D’Amico F, Durant NH, Hlatky MA, et al. methodological standards for meta-analyses and qualitative systematic reviews of cardiac prevention and treatment studies: a scientific statement from the American Heart Association. Circulation. 2017;136(10):e172.
Stang A. Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. https://doi.org/10.1007/s10654-010-9491-z.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:D5928.
DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28(2):105–14. https://doi.org/10.1016/j.cct.2006.04.004.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557.
Alexopoulos D, Xanthopoulou I, Gkizas V, Kassimis G, Theodoropoulos KC, Makris G, et al. Randomized assessment of ticagrelor versus prasugrel antiplatelet effects in patients with ST-segment-elevation myocardial infarction. Circ Cardiovasc Interv. 2012;5(6):797–804. https://doi.org/10.1161/circinterventions.112.972323.
De Backer O, Ratcovich H, Biasco L, Pedersen F, Helqvist S, Saunamaki K, et al. Prehospital administration of P2Y12 inhibitors and early coronary reperfusion in primary PCI: an observational comparative study. Thromb Haemost. 2015;114(3):623–31. https://doi.org/10.1160/th15-01-0026.
Parodi G, Bellandi B, Valenti R, Migliorini A, Marcucci R, Carrabba N, et al. Comparison of double (360 mg) ticagrelor loading dose with standard (60 mg) prasugrel loading dose in ST-elevation myocardial infarction patients: the Rapid Activity of Platelet Inhibitor Drugs (RAPID) primary PCI 2 study. Am Heart J. 2014;167(6):909–14. https://doi.org/10.1016/j.ahj.2014.03.011.
Parodi G, Valenti R, Bellandi B, Migliorini A, Marcucci R, Comito V, et al. Comparison of prasugrel and ticagrelor loading doses in ST-segment elevation myocardial infarction patients: RAPID (Rapid Activity of Platelet Inhibitor Drugs) primary PCI study. J Am Coll Cardiol. 2013;61(15):1601–6. https://doi.org/10.1016/j.jacc.2013.01.024.
Bonello L, Laine M, Cluzel M, Frere C, Mancini J, Hasan A, et al. Comparison of ticagrelor versus prasugrel to prevent periprocedural myonecrosis in acute coronary syndromes. Am J Cardiol. 2015;116(3):339–43. https://doi.org/10.1016/j.amjcard.2015.04.050.
Dery JP, Mehta SR, Fisher HN, Zhang X, Zhu YE, Welsh RC, et al. Baseline characteristics, adenosine diphosphate receptor inhibitor treatment patterns, and in-hospital outcomes of myocardial infarction patients undergoing percutaneous coronary intervention in the prospective Canadian Observational AntiPlatelet sTudy (COAPT). Am Heart J. 2016;181:26–34. https://doi.org/10.1016/j.ahj.2016.07.014.
Kim C, Shin DH, Ahn CM, Kim JS, Kim BK, Ko YG, et al. The use pattern and clinical impact of new antiplatelet agents including prasugrel and ticagrelor on 30-day outcomes after acute myocardial infarction in Korea: korean health insurance review and assessment data. Korean Circ J. 2017;47(6):888–97. https://doi.org/10.4070/kcj.2017.0072.
Laine M, Frere C, Toesca R, Berbis J, Barnay P, Pansieri M, et al. Ticagrelor versus prasugrel in diabetic patients with an acute coronary syndrome. A pharmacodynamic randomised study. Thromb Haemost. 2014;111(2):273–8. https://doi.org/10.1160/th13-05-0384.
Larmore C, Effron MB, Molife C, DeKoven M, Zhu Y, Lu J, et al. “Real-world” comparison of prasugrel with ticagrelor in patients with acute coronary syndrome treated with percutaneous coronary intervention in the united states. Catheter Cardiovasc Interv. 2016;88(4):535–44. https://doi.org/10.1002/ccd.26279.
Yudi MB, Clark DJ, Farouque O, Eccleston D, Andrianopoulos N, Duffy SJ, et al. Clopidogrel, prasugrel or ticagrelor in patients with acute coronary syndromes undergoing percutaneous coronary intervention. Intern Med J. 2016;46(5):559–65. https://doi.org/10.1111/imj.13041.
Alexopoulos D, Xanthopoulou I, Deftereos S, Hamilos M, Sitafidis G, Kanakakis I, et al. Contemporary antiplatelet treatment in acute coronary syndrome patients undergoing percutaneous coronary intervention: 1-year outcomes from the GReek AntiPlatElet (GRAPE) Registry. J Thromb Haemost. 2016;14(6):1146–54. https://doi.org/10.1111/jth.13316.
Rasia M, Solinas E, Marino M, Guastaroba P, Menozzi A, Cattabiani MA, et al. Comparison of 4 different strategies of DAPT after PCI in ACS real world population from a Northern Italy registry. J Thromb Thrombolysis. 2017;44(4):466–74. https://doi.org/10.1007/s11239-017-1567-0.
Song C, Sukul D, Seth M, Dupree JM, Khandelwal A, Dixon SR, et al. Ninety-day readmission and long-term mortality in medicare patients (>/=65 years) treated with ticagrelor versus prasugrel after percutaneous coronary intervention (from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium). Am J Cardiol. 2017;120(11):1926–32. https://doi.org/10.1016/j.amjcard.2017.08.009.
Biondi-Zoccai G, Lotrionte M, Agostoni P, Abbate A, Romagnoli E, Sangiorgi G, et al. Adjusted indirect comparison meta-analysis of prasugrel versus ticagrelor for patients with acute coronary syndromes. Int J Cardiol. 2011;150(3):325–31. https://doi.org/10.1016/j.ijcard.2010.08.035.
Husted S, James S, Becker RC, Horrow J, Katus H, Storey RF, et al. Ticagrelor versus clopidogrel in elderly patients with acute coronary syndromes: a substudy from the prospective randomized PLATelet inhibition and patient outcomes (PLATO) trial. Circ Cardiovasc Qual Outcomes. 2012;5(5):680–8. https://doi.org/10.1161/circoutcomes.111.964395.
Costa F, van Klaveren D, James S, Heg D, Raber L, Feres F, et al. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet. 2017;389(10073):1025–34. https://doi.org/10.1016/s0140-6736(17)30397-5.
Schulz S, Angiolillo DJ, Antoniucci D, Bernlochner I, Hamm C, Jaitner J, et al. Randomized comparison of ticagrelor versus prasugrel in patients with acute coronary syndrome and planned invasive strategy—design and rationale of the iNtracoronary Stenting and Antithrombotic Regimen: rapid early action for coronary treatment (ISAR-REACT) 5 trial. J Cardiovasc Transl Res. 2014;7(1):91–100. https://doi.org/10.1007/s12265-013-9527-3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of external funding were used to conduct this study or prepare this manuscript.
Conflict of interest
MSK, MMM, MSU, SA, SUK, ARK, NY, SF, FM, RAK, and RD have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Ethical approval
Ethical approval was not required as our study does not include confidential participant data and interventions.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Khan, M.S., Memon, M.M., Usman, M.S. et al. Prasugrel vs. Ticagrelor for Acute Coronary Syndrome Patients Undergoing Percutaneous Coronary Intervention: A Systematic Review and Meta-Analysis. Am J Cardiovasc Drugs 19, 465–476 (2019). https://doi.org/10.1007/s40256-019-00337-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-019-00337-5