Abstract
Background
Diabetes as the leading cause of mortality and morbidity, have been increased by about 35% from 2011 to 2015 worldwide. The objective of this study was to assess the trend and pattern of diabetes and prediabetes prevalence in Iran and also evaluate the diagnosis and status of diabetes management.
Methods
The results of this study are extracted from the National Stepwise approach to non-communicable disease risk factor surveillance (STEPS), conducted in 2007, 2011, 2016, and 2021 in Iran. We evaluated all obtained data by questionnaires (demographic, epidemiologic, risk-related behavioral data), physical measurements, and laboratory measures.
Results
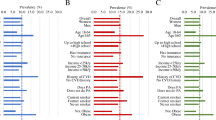
The prevalence of diabetes almost doubled from 2007 to 2021 among adults 25 years old and above. Diabetes prevalence increased from 10.85% (95% CI:10.30–11.40) in 2016 to 14.15% (13.42–14.87) in 2021. Prediabetes prevalence increased from 18.11% (17.46- 18,76) in 2016 to 24.81% (23.88–25.74) in 2021. Diabetes diagnosis stayed constant hence; diabetes coverage improved from 56.87% (54.21–59.52) to 65.04% (62.40- 67.69). Despite an enhancement in diabetes diagnosis and coverage, diabetes effective care did not improve significantly during 2016 and 2021, with a number of 35.98% (32.60- 39.36) in 2016 and 31.35% (28.20- 34.51) in 2021.
Conclusion
The prevalence of diabetes and prediabetes in Iran is almost doubled during the past 14 years. Although, several health policies had been developed to improve the screening and quality of diabetes care; there are still significant gaps in the effective control of diabetes. Accordingly, the current care plan should be reviewed.




Similar content being viewed by others
Abbreviations
- ADA:
-
American Diabetes Association
- COVID-19:
-
Coronavirus disease 2019
- FPG:
-
Fasting blood glucose
- GPAQ 1:
-
Global Physical Activity Questionnaire version 1
- HbA1c:
-
Glycated hemoglobin A1c
- NCD:
-
Non-communicable disease
- NGO:
-
Non-Governmental Organisation
- OHA:
-
Oral Hypoglycemic Agents
- PCA:
-
Principal component analysis
- STEPS:
-
Stepwise approach to non-communicable disease risk factor surveillance
- WHO:
-
World Health Organization
References
Bommer C, Sagalova V, Heesemann E, Manne-Goehler J, Atun R, Bärnighausen T, et al. Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care. 2018;41(5):963–70.
Bommer C, Heesemann E, Sagalova V, Manne-Goehler J, Atun R, Bärnighausen T, et al. The global economic burden of diabetes in adults aged 20–79 years: a cost-of-illness study. The Lancet Diabetes & Endocrinology. 2017;5(6):423–30.
Jafarvand E, Ataey A, Edalati S. Epidemiology and death trends due to diabetes in Iran. Intern Med Today. 2021;27(2):198–213.
Roglic G, Unwin N, Bennett PH, Mathers C, Tuomilehto J, Nag S, et al. The Burden of Mortality Attributable to Diabetes: realistic estimates for the year 2000. Diabetes Care. 2005;28(9):2130–5.
Khodakarami R, Abdi Z, Ahmadnezhad E, Sheidaei A, Asadi-Lari M. Prevalence, awareness, treatment and control of diabetes among iranian population: results of four national cross-sectional STEPwise approach to surveillance surveys. BMC Public Health. 2022;22(1):1216.
Esteghamati A, Larijani B, Aghajani MH, Ghaemi F, Kermanchi J, Shahrami A, et al. Diabetes in Iran: prospective analysis from first nationwide diabetes report of National Program for Prevention and Control of diabetes (NPPCD-2016). Sci Rep. 2017;7(1):13461.
Ogurtsova K, Guariguata L, Barengo NC, Ruiz PL-D, Sacre JW, Karuranga S, et al. IDF diabetes Atlas: global estimates of undiagnosed diabetes in adults for 2021. Diabetes Res Clin Pract. 2022;183:109118.
Dall TM, Yang W, Halder P, Pang B, Massoudi M, Wintfeld N, et al. The economic burden of elevated blood glucose levels in 2012: diagnosed and undiagnosed diabetes, gestational diabetes mellitus, and prediabetes. Diabetes Care. 2014;37(12):3172–9.
Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. 2020;10(1):14790.
Djalalinia S, Modirian M, Sheidaei A, Yoosefi M, Zokaiee H, Damirchilu B et al. Protocol design for large–scale cross–sectional studies of surveillance of risk factors of non–communicable diseases in Iran: STEPs 2016. Arch Iran Med. 2017;20(9).
Djalalinia SAS, Ghasemi E, Yoosefi M, Rezaei N, Farzi Y et al. Protocol design for surveillance of risk factors of non–communicable diseases during the COVID-19 pandemic: an experience from Iran STEPS Survey 2021. Arch Iran Med. 2022.
(ADA) ADA. American Diabetes Association diabetes mellitus Diagnosis [Available from: https://diabetes.org/diabetes/a1c/diagnosis.
WHO. Global physical activity questionnaire (GPAQ) 2021 [Available from: https://www.who.int/publications/m/item/global-physical-activity-questionnaire.
Mirzaei M, Rahmaninan M, Mirzaei M, Nadjarzadeh A, Dehghani Tafti AA. Epidemiology of diabetes mellitus, pre-diabetes, undiagnosed and uncontrolled diabetes in Central Iran: results from Yazd health study. BMC Public Health. 2020;20:1–9.
WHO. NCD global monitoring framework [Available from: https://www.who.int/teams/ncds/surveillance/monitoring-capacity/gmf.
Damm P, Houshmand-Oeregaard A, Kelstrup L, Lauenborg J, Mathiesen ER, Clausen TD. Gestational diabetes mellitus and long-term consequences for mother and offspring: a view from Denmark. Diabetologia. 2016;59:1396–9.
Au CPY, Raynes-Greenow CH, Turner RM, Carberry AE, Jeffery HE. Antenatal management of gestational diabetes mellitus can improve neonatal outcomes. Midwifery. 2016;34:66–71.
Tabatabaei-Malazy O, Saeedi Moghaddam S, Rezaei N, Sheidaei A, Hajipour MJ, Mahmoudi N, et al. A nationwide study of metabolic syndrome prevalence in Iran; a comparative analysis of six definitions. PLoS ONE. 2021;16(3):e0241926.
Djalalinia S, Yoosefi M, Shahin S, Ghasemi E, Rezaei N, Ahmadi N, et al. The levels of BMI and patterns of obesity and overweight during the COVID-19 pandemic: experience from the Iran STEPs 2021 survey. Front Endocrinol. 2022;13:1043894.
Khorrami Z, Yarahmadi S, Etemad K, Khodakarim S, Kameli ME, Hazaveh ARM. Urban-rural differences in the prevalence of self-reported diabetes and its risk factors: the WHO STEPS iranian noncommunicable disease risk factor surveillance in 2011. Iran J Med Sci. 2017;42(5):481.
Nejadghaderi SA, Ahmadi N, Rashidi M-M, Ghanbari A, Noori M, Abbasi-Kangevari M, et al. Physical activity pattern in Iran: findings from STEPS 2021. Front Public Health. 2023;10:1036219.
Aung WP, Htet AS, Bjertness E, Stigum H, Chongsuvivatwong V, Kjøllesdal MKR. Urban–rural differences in the prevalence of diabetes mellitus among 25–74 year-old adults of the Yangon Region, Myanmar: two cross-sectional studies. BMJ open. 2018;8(3):e020406.
Chentli F, Azzoug S, Mahgoun S. Diabetes mellitus in elderly. Indian J Endocrinol Metab. 2015;19(6):744–52.
Esteghamati A, Etemad K, Koohpayehzadeh J, Abbasi M, Meysamie A, Noshad S, et al. Trends in the prevalence of diabetes and impaired fasting glucose in association with obesity in Iran: 2005–2011. Diabetes Res Clin Pract. 2014;103(2):319–27.
Aswathi V, Chowta MN, Achappa B, Madi D. Correlation of awareness of the disease with glycaemic control and diabetic complications among patients attending a tertiary care hospital. Clin Diabetol. 2019;8(3):143–53.
Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet Global Health. 2018;6(11):e1196–e252.
Akbarialiabad H, Rastegar A, Bastani B. How sanctions have impacted iranian healthcare sector: a brief review. Arch Iran Med. 2021;24(1):58–63.
Fattahi N, Azadnajafabad S, Mohammadi E, Aminorroaya A, Rezaei S, Ghasemi E et al. Geographical, gender and age inequalities in non-communicable diseases both at national and provincial levels in Iran. J Diabetes Metabolic Disorders. 2021:1–7.
Khosravi Shadmani F, Farzadfar F, Larijani B, Mirzaei M, Haghdoost AA. Trend and projection of mortality rate due to non-communicable diseases in Iran: a modeling study. PLoS ONE. 2019;14(2):e0211622.
Mirahmadizadeh A, Sharifi MH, Hassanzadeh J, Heiran A, Ardekani FM, Hadizadeh N, et al. The effect of COVID-19 pandemic on diabetes care indices in Southern Iran: an interrupted time series analysis. BMC Health Serv Res. 2023;23(1):1–9.
Noshad S, Afarideh M, Heidari B, Mechanick JI, Esteghamati A. Diabetes care in Iran: where we stand and where we are headed. Annals of Global Health. 2015;81(6):839–50.
Dehghani Firouzabadi M, Sheikhy A, Poopak A, Esteghamati A, Mechanick JI, Dehghani Firouzabadi F. Challenges to Lifestyle Medicine for type 2 diabetes in Iran: a synoptic review. Am J Lifestyle Med. 2023:15598276231167787.
Moradi G, Shokri A, Mohamadi-Bolbanabad A, Zareie B, Piroozi B. Evaluating the quality of care for patients with type 2 diabetes mellitus based on the HbA1c: a national survey in Iran. Heliyon. 2021;7(3).
Acknowledgements
The authors would like to express their gratitude for their partnership with the Deputy for Research and Technology and the Deputy of Health of the Ministry of Health and Medical Education, the National Institute for Health Research, and the World Health Organization. The authors would also like to thank the Non-Communicable Diseases Research Center’s staff of the Endocrinology and Metabolism Population Sciences Institute of Tehran University of Medical Sciences for their wholehearted cooperation. We are also grateful for the help and guidance of Dr. Mohammad Mehdi Khadembashiri in applying some revisions. This conducted study was an endocrinology and metabolism fellowship thesis project of Dr. Aslan Ameli.
Funding
This study received no grants or funding support.
Author information
Authors and Affiliations
Contributions
Conceptualization: Aslan Ameli, Negar Rezaei, Bagher Larijani, Farshad Farzadfar. Data Curation: Moein Yoosefi, Naser Ahmadi. Formal Analysis: Naser Ahmadi. Investigation: Bagher Larijani and all of the co-authors. Methodology: Aslan Ameli, Ali Sheikhy, Ozra Tabatabaei-Malazy, Naser Ahmadi, Negar Rezaei, Bagher Larijani. Writing—Original Draft Preparation: Aslan Ameli, Ali Sheikhy, Ozra Tabatabaei-Malazy. All of the authors participated in rewriting and finalizing the article and approved it.
Corresponding author
Ethics declarations
Ethical considerations
Every participant received detailed information about the survey’s objectives and procedures. Participation in the survey was entirely voluntary, and both verbal and written consent were obtained from each participant. The study received ethical approval from the ethical committee of the National Institute for Health Research (ID: IR.TUMS.NIHR.REC.1398.006).
Conflict of interest
The authors had no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material {comment: please change “diabetes” in table-4 supplementary to “prediabetes” I uploaded new file as attachment}
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ameli, A., Sheikhy, A., Tabatabaei-Malazy, O. et al. The diabetes cascade of care through the 14 years in Iran: findings of nationwide STEPS surveys 2007–2021. J Diabetes Metab Disord 22, 1731–1743 (2023). https://doi.org/10.1007/s40200-023-01308-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-023-01308-z