Abstract
Objectives
This comprehensive review aims to examine the reciprocal interplay between Type 2 diabetes mellitus (T2DM) and sarcopenia, identify prevailing research gaps, and discuss therapeutic approaches and measures to enhance healthcare practices within hospital settings.
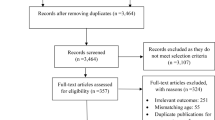
Methods
A thorough literature review was conducted to gather relevant studies and articles on the relationship between T2DM and sarcopenia. Various databases were searched, including Google Scholar, PubMed, Scopus, and Science Direct databases. The search terms included T2DM, sarcopenia, inflammation, insulin resistance, advanced glycation end products, oxidative stress, muscle dimensions, muscle strength, muscle performance, aging, nutrition, hormone levels, and physical activity. The collected articles were critically analysed to extract key findings and identify gaps in current research.
Results
The prevalence and incidence of metabolic and musculoskeletal disorders, notably T2DM and sarcopenia, have surged in recent years. T2DM is marked by inflammation, insulin resistance, accumulation of advanced glycation end products, and oxidative stress, while sarcopenia involves a progressive decline in skeletal muscle mass and function. The review underscores the age-related correlation between sarcopenia and adverse outcomes like fractures, falls, and mortality. Research gaps regarding optimal nutritional interventions for individuals with T2DM and sarcopenia are identified, emphasizing the necessity for further investigation in this area.
Conclusions
The reciprocal interplay between T2DM and sarcopenia holds significant importance. Further research is warranted to address knowledge gaps, particularly in utilizing precise measurement tools during clinical trials. Lifestyle modifications appear beneficial for individuals with T2DM and sarcopenia. Additionally, practical nutritional interventions require investigation to optimize healthcare practices in hospital settings.




Similar content being viewed by others
References
Musumeci G. Sarcopenia and Exercise “The state of the art. J Funct Morphology Kinesiol. 2017;2(4):40.
Greco EA, Pietschmann P, Migliaccio S. Osteoporosis and Sarcopenia increase Frailty Syndrome in the Elderly. Front Endocrinol. 2019;10.
UN. United Nations. Department of Economic and Social Affairs Population Division: World Population Prospects: The 2017 Revision, Key Findings and Advance Table 2017; (accessed on 25 September 2019).
Pal R, Aggarwal A, Singh T, Sharma S, Khandelwal N, Garg A, Bhansali A, Kumar A, Yadav U, Singh P, Dhiman V, Dutta P, Bhadada SK. Diagnostic cut-offs, prevalence, and biochemical predictors of sarcopenia in healthy indian adults: the Sarcopenia-Chandigarh Urban Bone Epidemiological Study (Sarco-CUBES). Eur Geriatr Med. 2020 Oct;11(5):725–36.
Kapoor D, Piplani T, Singh A, Perwaiz A, Chaudhary A. Defining Sarcopenia in the indian Population—a step Forward. Indian J Surg. 2021;83(2):476–82.
Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised european consensus on definition and diagnosis [published correction appears in Age Ageing. 2019 Jul 1;48(4):601]. Age Ageing. 2019;48(1):16–31.
Larsson L, Degens H, Li M, Salviati L, Lee Y il, Thompson W et al. Sarcopenia: Aging-Related Loss of Muscle Mass and Function. Physiol Rev [Internet]. 2018 Nov 14;99(1):427–511.
Samoilova YG, Matveeva MV, Khoroshunova EA, Kudlay DA, Oleynik OA, Spirina LV. Markers for the prediction of probably Sarcopenia in Middle-Aged individuals. J Personalized Med. 2022;12(11):1830.
Chung SM, Moon JS, Chang MC. Prevalence of Sarcopenia and its Association with diabetes: a Meta-analysis of Community-Dwelling Asian Population. Front Med. 2021;8.
de Rekeneire N, Peila R, Ding J, et al. Diabetes, hyperglycemia, and inflammation in older individuals. Diabetes Care. 2006;29(8):1902.
Sartori R, Romanello V, Sandri M. Mechanisms of muscle atrophy and hypertrophy: implications in health and disease. Nat Commun [Internet]. 2021;12(1):330.
Mesinovic J, Zengin A, De Courten B, Ebeling PR, Scott D. Sarcopenia and type 2 diabetes mellitus: a bidirectional relationship. Diabetes Metab Syndr Obes 2019 Jul 8;12:1057–72.
Wang M, Tan Y, Shi Y, Wang X, Liao Z, Wei P. Diabetes and sarcopenic obesity: pathogenesis, diagnosis, and treatments. Front Endocrinol (Lausanne). 2020 Aug;25:11:568.
Singhal S, Dewangan GC, Bansal R, et al. Sarcopenia and its Association with geriatric Syndromes and Quality of Life in older indian outpatients - a cross-sectional pilot observational study. J Indian Acad Geriatr. 2019;15(2):66.
Pacifico J, Geerlings MAJ, Reijnierse EM, Phassouliotis C, Lim WK, Maier AB. Prevalence of sarcopenia as a comorbid disease: a systematic review and meta-analysis. Exp Gerontol. 2020;131:110801.
Therakomen V, Petchlorlian A, Lakananurak N. Prevalence and risk factors of primary sarcopenia in community-dwelling outpatient elderly: a cross-sectional study. Sci Rep. 2020;10(1):19551.
Pang BWJ, Wee S-L, Lau LK, et al. Prevalence and Associated factors of Sarcopenia in singaporean adults—the Yishun Study. J Am Med Dir Assoc. 2021;22(4):885e1–885.
Tey SL, Chew STH, How CH, et al. Factors associated with muscle mass in community-dwelling older people in Singapore: findings from the SHIELD study. PLoS ONE. 2019;14(10):e0223222.
Chung SM, Moon JS, Chang MC. Prevalence of Sarcopenia and its Association with diabetes: a Meta-analysis of Community-Dwelling Asian Population. Front Med (Lausanne). 2021;8:681232.
Minocha S, Thomas T, Kurpad AV. Dietary protein and the healthnutrition-agriculture connection in India. J Nutr. 2017;147(7):1243–50. https://doi.org/10.3945/jn.116.243980.
Nguyen TN, Nguyen TN, Nguyen AT, Nguyen TX, Nguyen HTT, Nguyen TTH et al. Prevalence of sarcopenia and its associated factors in patients attending geriatric clinics in Vietnam: a cross-sectional study. BMJ Open [Internet]. 2020 Sep 1;10(9):e037630.
de Rekeneire N, Peila R, Ding J, et al. Diabetes, hyperglycemia, and inflammation in older individuals. Diabetes Care. 2006;29(8):1902.
Vozarova B, Weyer C, Lindsay RS, Pratley RE, Bogardus C, Tataranni PA. High white blood cell count is associated with a worsening of insulin sensitivity and predicts the development of type 2 diabetes. Diabetes. 2002;51(2):455.
Haddad F, Zaldivar F, Cooper DM, Adams GR. IL-6-induced skeletal muscle atrophy. J Appl Physiol. 2005;98(3):911–7.
Goyal R, Faizy AF, Siddiqui SS, Singhai M. Evaluation of TNF-α and IL-6 levels in obese and non-obese diabetics: pre- and postinsulin effects. N Am J Med Sci. 2012;4(4):180–4.
King DE, Mainous AG, Buchanan TA, Pearson WS. C-reactive protein and glycemic control in adults with diabetes. Diabetes Care. 2003;26(5):1535.
Makki K, Froguel P, Wolowczuk I. Adipose tissue in obesity-related inflammation and insulin resistance: cells, cytokines, and chemokines. ISRN Inflamm. 2013;2013:139239.
Mesinovic J, McMillan BL, Shore-Lorenti C, De Courten B, Ebeling RP, Scott D. Metabolic syndrome and its associations with components of sarcopenia in overweight and obese older adults. J Clin Med. 2019;8:2.
Bach E, Nielsen RR, Vendelbo MH, et al. Direct effects of TNF-α on local fuel metabolism and cytokine levels in the placebocontrolled, bilaterally infused human leg. Diabetes. 2013;62(12):4023. https://doi.org/10.2337/db12-0863.
Carey AL, Steinberg GR, Macaulay SL, et al. Interleukin-6 increases insulin-stimulated glucose disposal in humans and glucose uptake and fatty acid oxidation in vitro via AMP-activated protein kinase. Diabetes. 2006;55(10):2688–97.
Serrano AL, Baeza-Raja B, Perdiguero E, Jardi M, MunozCanoves P. Interleukin-6 is an essential regulator of satellite cell-mediated skeletal muscle hypertrophy. Cell Metab. 2008;7(1):33–44.
Payette H, Roubenoff R, Jacques PF, et al. Insulin-like growth factor-1 and interleukin 6 predict sarcopenia in very old community-living men and women: the Framingham Heart Study. J Am Geriatr Soc. 2003;51(9):1237–43.
Zinman B, Hoogwerf BJ, Duran Garcia S, et al. The effect of adding exenatide to a thiazolidinedione in suboptimally controlled type 2 diabetes: a randomized trial. Ann Intern Med. 2007;146(7):477–85.
Alemán H, Esparza J, Ramirez FA, Astiazaran H, Payette H. Longitudinal evidence on the association between interleukin-6 and C-reactive protein with the loss of total appendicular skeletal muscle in free-living older men and women. Age Ageing. 2011;40(4):469–75.
Park SW, Goodpaster BH, Strotmeyer ES, et al. Accelerated loss of skeletal muscle strength in older adults with type 2 diabetes: the health, aging, and body composition study. Diabetes Care. 2007;30(6):1507–12.
Visser M, Pahor M, Taaffe DR, et al. Relationship of interleukin-6 and tumor necrosis factor-alpha with muscle mass and muscle strength in elderly men and women: the Health ABC Study. J Gerontol A Biol Sci Med Sci. 2002;57(5):M326–32.
Hamer M, Molloy GJ. Association of C-reactive protein and muscle strength in the English Longitudinal Study of Ageing. Age (Dordr). 2009;31(3):171–7.
Gomes MJ, Martinez PF, Pagan LU, et al. Skeletal muscle aging: influence of oxidative stress and physical exercise. Oncotarget. 2017;8(12):20428–40.
Asmat U, Abad K, Ismail K. Diabetes mellitus and oxidative stress —A concise review. Saudi Pharm J. 2016;24(5):547–53.
Aragno M, Mastrocola R, Catalano MG, Brignardello E, Danni O, Boccuzzi G. Oxidative stress impairs skeletal muscle repair in diabetic rats. Diabetes. 2004;53(4):1082.
Cetrone M, Mele A, Tricarico D. Effects of the antidiabetic drugs on the age-related atrophy and sarcopenia associated with diabetes type II. Curr Diabetes Rev. 2014;10(4):231–7.
Zacarias-Flores M, Sanchez-Rodriguez MA, Garcia-Anaya OD, Correa-Munoz E, Mendoza-Nunez VM. Relationship between oxidative stress and muscle mass loss in early postmenopause: an exploratory study. Endocrinol Diabetes Nutr. 2018;65(6):328–34.
Scicchitano BM, Pelosi L, Sica G, Musarò A. The physiopathologic role of oxidative stress in skeletal muscle. Mech Ageing Dev. 2018;170:37–44.
Short KR, Bigelow ML, Kahl J, et al. Decline in skeletal muscle mitochondrial function with aging in humans. Proc Natl Acad Sci U S A. 2005;102(15):5618–23.
Abbatecola AM, Paolisso G, Fattoretti P, et al. Discovering pathways of sarcopenia in older adults: a role for insulin resistance on mitochondria dysfunction. J Nutr Health Aging. 2011;15(10):890–5.
Morino K, Petersen KF, Dufour S, et al. Reduced mitochondrial density and increased IRS-1 serine phosphorylation in muscle of insulin-resistant offspring of type 2 diabetic parents. J Clin Invest. 2005;115(12):3587–93.
Singh R, Barden A, Mori T, Beilin L. Advanced glycation end-products: a review. Diabetologia. 2001;44(2):129–46.
Haus JM, Carrithers JA, Trappe SW, Trappe TA. Collagen, cross-linking, and advanced glycation end products in aging human skeletal muscle. J Appl Physiol. 2007;103(6):2068–76.
Forbes JM, Sourris KC, de Courten MPJ, et al. Advanced glycation end products (AGEs) are cross-sectionally associated with insulin secretion in healthy subjects. Amino Acids. 2014;46(2):321–6.
Mulder DJ, Water TV, Lutgers HL, et al. Skin autofluorescence, a novel marker for glycemic and oxidative stress-derived advanced glycation endproducts: an overview of current clinical studies, evidence, and limitations. Diabetes Technol Ther. 2006;8(5):523–35.
Mori H, Kuroda A, Ishizu M, et al. Association of accumulated advanced glycation end products with a high prevalence of sarcopenia and dynapenia in patients with type 2 diabetes. J Diabetes Investig. 2019;35:731–7.
Momma H, Niu K, Kobayashi Y, et al. Skin advanced glycation endproduct accumulation and muscle strength among adult men. Eur J Appl Physiol. 2011;111(7):1545–52.
Tabara Y, Ikezoe T, Yamanaka M et al. Advanced Glycation End Product Accumulation is Associated with low skeletal muscle Mass, weak muscle strength, and reduced bone density: the Nagahama Study. J Gerontol A Biol Sci Med Sci. 2018.
Chaudhri S, Fan S, Davenport A. Pitfalls in the measurement of skin autofluorescence to determine tissue advanced glycosylation content in haemodialysis patients. Nephrology. 2013;18(10):671–5.
Noordzij MJ, Lefrandt JD, Graaff R, Smit AJ. Dermal factors influencing measurement of skin autofluorescence. Diabetes Technol Ther. 2011;13(2):165–70.
Fowler MJ. Microvascular and macrovascular complications of diabetes. Clin Diabetes. 2008;26(2):77.
McDermott MM, Criqui MH, Greenland P, et al. Leg strength in peripheral arterial disease: associations with disease severity and lower-extremity performance. J Vasc Surg. 2004;39(3):523–30.
Nomura T, Ishiguro T, Ohira M, Ikeda Y. Diabetic polyneuropathy is a risk factor for decline of lower extremity strength in patients with type 2 diabetes. J Diabetes Investig. 2018;9(1):186–92.
Andersen H, Gjerstad MD, Jakobsen J. Atrophy of foot muscles. Diabetes Care. 2004;27(10):2382.
Strotmeyer ES, de Rekeneire N, Schwartz AV, et al. The relationship of reduced peripheral nerve function and diabetes with physical performance in older white and black adults. Diabetes Care. 2008;31(9):1767.
Gupta P, Aravindhan A, Gand ATL, et al. Association between the severity of diabetic retinopathy and falls in an asian population with diabetes: the Singapore Epidemiology of Eye Diseases Study. JAMA Ophthalmol. 2017;135(12):1410–6.
Haddad YK, Bergen G, Florence CS. Estimating the economic burden related to older adult falls by state. J Public Health Manag Pract. 2019;25(2):E17–E24.
Haagsma JA, Graetz N, Bolliger I, et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev. 2016;22(1):3.
Wang XH, Mitch WE. Mechanisms of muscle wasting in chronic kidney disease. Nat Rev Nephrol. 2014;10(9):504–16.
Fung FY, Koh YLE, Malhotra R, et al. Prevalence of and factors associated with sarcopenia among multi-ethnic ambulatory older Asians with type 2 diabetes mellitus in a primary care setting. BMC Geriatr. 2019;19(1):122.
VAd S, Oliveira D, Barbosa SR, et al. Sarcopenia in patients with chronic kidney disease not yet on dialysis: analysis of the prevalence and associated factors. PLoS ONE. 2017;12(4):e0176230–0.
Pereira RA, Cordeiro AC, Avesani CM, et al. Sarcopenia in chronic kidney disease on conservative therapy: prevalence and association with mortality. Nephrol Dial Transplant. 2015;30(10):1718–25.
Zhou Y, Hellberg M, Svensson P, Hoglund P, Clyne N. Sarcopenia and relationships between muscle mass, measured glomerular filtration rate and physical function in patients with chronic kidney disease stages 3–5. Nephrol Dial Transplant. 2018;33(2):342–8.
Gamboa JL, Billings F, Bojanowski MT, et al. Mitochondrial dysfunction and oxidative stress in patients with chronic kidney disease. Physiol Rep. 2016;4(9):e12780.
Doğan MH, Karadag B, Ozyigit T, Kayaoglu S, Ozturk AO, Altuntas Y. Correlations between sarcopenia and hypertensive target organ damage in a turkish cohort. Acta Clin Belg. 2012;67(5):328–32.
Dziubek W, Bulińska K, Stefańska M, et al. Peripheral arterial disease decreases muscle torque and functional walking capacity in elderly. Maturitas. 2015;81(4):480–6.
McDermott Mary M. Lower extremity manifestations of peripheral artery disease. Circ Res. 2015;116(9):1540–50.
Fehér A, Gazdecki M, Véha M, Szakály M, Szakály Z. A Comprehensive Review of the benefits of and the barriers to the switch to a plant-based Diet. Sustainability. 2020;12(10):4136.
Boettcher M, Machann J, Stefan N, et al. Intermuscular adipose tissue (IMAT): association with other adipose tissue compartments and insulin sensitivity. J Magn Reson Imaging. 2009;29(6):1340–5.
Scott D, Shore-Lorenti C, McMillan LB, et al. Calf muscle density is independently associated with physical function in overweight and obese older adults. J Musculoskelet Neuronal Interact. 2018;18(1):9–17.
Marcus RL, Addison O, Dibble LE, Foreman KB, Morrell G, LaStayo P. Intramuscular adipose tissue, sarcopenia, and mobility function in older individuals. J Aging Res. 2012.
Goodpaster BH, Thaete FL, Kelley DE. Thigh adipose tissue distribution is associated with insulin resistance in obesity and in type 2 diabetes mellitus. Am J Clin Nutr. 2000;71(4):885–92.
Scott D, Johansson J, McMillan LB, Ebeling PR, Nordstrom A, Nordstrom P. Mid-calf skeletal muscle density and its associations with physical activity, bone health and incident 12-month falls in older adults: the healthy Ageing Initiative. Bone. 2018;120:446–51.
Frank-Wilson AW, Farthing JP, Chilibeck PD, et al. Lower leg muscle density is independently associated with fall status in community-dwelling older adults. Osteoporos Int. 2016;27(7):2231–40.
Skundric DS, Lisak RP. Role of neuropoietic cytokines in development and progression of diabetic polyneuropathy: from glucose metabolism to neurodegeneration. Exp Diabesity Res. 2003;4(4):303–12.
Csapo R, Malis V, Sinha U, Du J, Sinha S. Age-associated differences in triceps surae muscle composition and strength – an MRIbased cross-sectional comparison of contractile, adipose and connective tissue. BMC Musculoskelet Disord. 2014;15(1):209.
Musi N, Hirshman MF, Nygren J, et al. Metformin increases AMP-activated protein kinase activity in skeletal muscle of subjects with type 2 diabetes. Diabetes. 2002;51(7):2074–81.
Lee CG, Boyko EJ, Barrett-Connor E, et al. Insulin sensitizers may attenuate lean mass loss in older men with diabetes. Diabetes Care. 2011;34(11):2381.
Mele A, Calzolaro S, Cannone G, Cetrone M, Conte D, Tricarico D. Database search of spontaneous reports and pharmacological investigations on the sulfonylureas and glinides-induced atrophy in skeletal muscle. Pharmacol Res Perspect. 2014;2(1):e00028–8.
Becker C, Lord SR, Studenski SA, et al. Myostatin antibody (LY2495655) in older weak fallers: a proof-of-concept, randomised, phase 2 trial. Lancet Diabetes Endocrinol. 2015;3(12):948–57.
Dalton JT, Barnette KG, Bohl CE, et al. The selective androgen receptor modulator GTx-024 (enobosarm) improves lean body mass and physical function in healthy elderly men and postmenopausal women: results of a double-blind, placebo-controlled phase II trial. J Cachexia Sarcopenia Muscle. 2011;2(3):153–61.
Papanicolaou DA, Ather SN, Zhu H, et al. A phase IIA randomized, placebo-controlled clinical trial to study the efficacy and safety of the selective androgen receptor modulator (SARM), MK-0773 in female participants with sarcopenia. J Nutr Health Aging. 2013;17(6):533–43.
Butcher Joshua T, Mintz James D, Larion S, et al. Increased muscle mass protects against hypertension and renal injury in obesity. J Am Heart Assoc. 2018;7(16):e009358.
Lv Q, Yuan L, Deng J, et al. Efficient generation of myostatin gene mutated rabbit by CRISPR/Cas9. Sci Rep. 2016;6:25029.
Mitranun W, Deerochanawong C, Tanaka H, Suksom D. Continuous vs interval training on glycemic control and macro- and microvascular reactivity in type 2 diabetic patients. Scand J Med Sci Sports. 2014;24:e69–e76.
Tan S, Li W, Wang J. Effects of six months of combined aerobic and resistance training for elderly patients with a long history of type 2 diabetes. J Sports Sci Med. 2012;11:495–501.
Egger A, Niederseer D, Diem G, Finkenzeller T, Ledl-Kurkowski E, Forstner R, Pirich C, Patsch W, Weitgasser R, Niebauer J. Different types of resistance training in type 2 diabetes mellitus: Effects on glycaemic control, muscle mass and strength. Eur J Prev Cardiol. 2012;20:1051–60.
Chen H-T, Chung Y-C, Chen Y-J, Ho S-Y, Wu H-J. Effects of different types of Exercise on body composition, muscle strength, and IGF-1 in the Elderly with sarcopenic obesity. J Am Geriatr Soc. 2017;65:827–32.
Lustosa LP, Silva JP, Coelho FM, Pereira DS, Parentoni AN, Pereira LS. Impact of resistance exercise program on functional capacity and muscular strength of knee extensor in pre-frail community-dwelling older women: a randomized crossover trial. Rev Bras Fisioter. 2011;15:318–24.
Latham NK, Anderson CS, Lee A, Bennett DA, Moseley A, Cameron ID. Fitness Collaborative Group. A randomized, controlled trial of quadriceps resistance exercise and vitamin D in frail older people: the Frailty Interventions Trial in Elderly subjects (FITNESS). J Am Geriatr Soc. 2003;51:291–9.
Terada T, Friesen A, Chahal BS, Bell GJ, McCargar LJ, Boulé NG. Feasibility and preliminary efficacy of high intensity interval training in type 2 diabetes. Diabetes Res Clin Pract. 2013;99:120–9.
Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403.
Gregg EW, Chen H, Wagenknecht LE, et al. Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA. 2012;308(23):2489–96.
Steffl M, Bohannon RW, Sontakova L, Tufano JJ, Shiells K, Holmerova I. Relationship between sarcopenia and physical activity in older people: a systematic review and meta-analysis. Clin Interv Aging. 2017;12:835–45.
Villareal DT, Aguirre L, Gurney AB, et al. Aerobic or resistance exercise, or both, in dieting obese older adults. N Engl J Med. 2017;376(20):1943–55.
Greco M, Chiefari E, Montalcini T, et al. Early effects of a hypocaloric, mediterranean diet on laboratory parameters in obese individuals. Mediators Inflamm. 2014;2014:750860.
Phillips S, Chevalier S, Leidy H. Protein “Requirements” beyond the RDA: implications for Optimizing Health. Appl Physiol Nutr Metab. 2016;41(5):565–72.
Trumbo P, Schlicker S, Yates AA, Poos M. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J Am Diet Assoc. 2002;102(11):1621–30.
Nowson C, O’Connell S. Protein requirements and recommendations for older people: a review. Nutrients. 2015;7(8):6874–99.
Health ABCS, Newman AB, Nicklas BJ, et al. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the Health, Aging, and body composition (Health ABC) Study. Am J Clin Nutr. 2008;87(1):150–5.
Shang X, Scott D, Sanders KM, et al. Dietary protein intake and risk of type 2 diabetes: results from the Melbourne Collaborative Cohort Study and a meta-analysis of prospective studies. Am J Clin Nutr. 2016;104(5):1352–65.
van Vliet S, Burd NA, van Loon LJC. The skeletal muscle anabolic response to plant- versus animal-based protein consumption. J Nutr. 2015;145(9):1981–91.
Morton RW, Murphy KT, McKellar SR, et al. A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults. Br J Sports Med. 2018;52(6):376.
Beaudart C, Dawson A, Shaw SC, et al. Nutrition and physical activity in the prevention and treatment of sarcopenia: systematic review. Osteoporos Int. 2017;28(6):1817–33.
Dang M, Shore-Lorenti C, McMillan BL et al. Associations of serum 25-hydroxyvitamin D with physical performance and bone health in overweight and obese older adults. Int J Environ Res Public Health. 2019;16(3).
Mirhosseini N, Vatanparast H, Mazidi M, Kimball SM, Vitamin D. Supplementation, glycemic control, and insulin resistance in prediabetics: a meta-analysis. J Endocr Soc. 2018;2(7):687–709.
Shea MK, Fielding RA, Dawson-Hughes B. The effect of vitamin D supplementation on lower-extremity power and function in older adults: a randomized controlled trial. Am J Clin Nutr. 2019;109(2):369–79.
Antoniak AE, Greig CA. The effect of combined resistance exercise training and vitamin D(3) supplementation on musculoskeletal health and function in older adults: a systematic review and meta-analysis. BMJ Open. 2017;7(7):e014619–9.
Gulseth HL, Wium C, Angel K, Eriksen EF, Birkeland KI. Effects of vitamin D supplementation on insulin sensitivity and insulin secretion in subjects with type 2 diabetes and vitamin D deficiency: a randomized controlled trial. Diabetes Care. 2017;40(7):872–8.
Lee CJ, Iyer G, Liu Y, et al. The effect of vitamin D supplementation on glucose metabolism in type 2 diabetes mellitus: a systematic review and meta-analysis of intervention studies. J Diabetes Complications. 2017;31(7):1115–26.
Wu C, Qiu S, Zhu X, Li L. Vitamin D supplementation and glycemic control in type 2 diabetes patients: a systematic review and meta-analysis. Metabolism. 2017;73:67–76.
Hu Z, Chen J, Sun X, Wang L, Wang A. Efficacy of vitamin D supplementation on glycemic control in type 2 diabetes patients: a meta-analysis of interventional studies. Med (Baltim). 2019;98(14):e14970.
Jamka M, Woźniewicz M, Jeszka J, Mardas M, Bogdański P, Stelmach-Mardas M. The effect of vitamin D supplementation on insulin and glucose metabolism in overweight and obese individuals: systematic review with meta-analysis. Sci Rep. 2015;5:16142.
Hutchins-Wiese HL, Kleppinger A, Annis K, et al. The impact of supplemental n-3 long chain polyunsaturated fatty acids and dietary antioxidants on physical performance in postmenopausal women. J Nutr Health Aging. 2013;17(1):76–80.
Smith GI, Julliand S, Reeds DN, Sinacore DR, Klein S, Mittendorfer B. Fish oil-derived n-3 PUFA therapy increases muscle mass and function in healthy older adults. Am J Clin Nutr. 2015;102(1):115–22.
Sneddon AA, Tsofliou F, Fyfe CL, et al. Effect of a conjugated linoleic acid and omega-3 fatty acid mixture on body composition and adiponectin. Obes (Silver Spring). 2008;16(5):1019–24.
Cornish SM, Chilibeck PD. Alpha-linolenic acid supplementation and resistance training in older adults. Appl Physiol Nutr Metab. 2009;34(1):49–59.
Flessa S, Huebner C. Innovations in Health Care-A conceptual Framework. Int J Environ Res Public Health. 2021 Sep;24(19):10026.
Rosen MA, DiazGranados D, Dietz AS, Benishek LE, Thompson D, Pronovost PJ, Weaver SJ. Teamwork in healthcare: key discoveries enabling safer, high-quality care. Am Psychol. 2018 May-Jun;73(4):433–50.
Marty E, Liu Y, Samuel A, Or O, Lane J. A review of sarcopenia: enhancing awareness of an increasingly prevalent disease. Bone. 2017 Dec;105:276–86.
Bokhour BG, Fix GM, Mueller NM, Barker AM, Lavela SL, Hill JN, et al. How can healthcare organizations implement patient-centered care? Examining a large-scale cultural transformation. BMC Health Serv Res [Internet]. 2018;18(1):168.
Fehér A, Gazdecki M, Véha M, Szakály M, Szakály Z. A Comprehensive Review of the benefits of and the barriers to the switch to a plant-based Diet. Sustainability. 2020;12(10):4136.
Tiwary A, Rimal A, Paudyal B, Sigdel KR, Basnyat B. Poor communication by health care professionals may lead to life-threatening complications: examples from two case reports. Wellcome Open Res. 2019;4:7.
Verstraeten LM, van Wijngaarden JP, Tol-Schilder M, Meskers CG, Maier AB. Combating sarcopenia in geriatric rehabilitation patients: study protocol of the EMPOWER-GR observational cohort, sarcopenia awareness survey and randomised controlled feasibility trial. BMJ Open. 2022;12(3):e054950.
Hunter DJ. The slow, lingering death of the English NHS: comment on “Who killed the English National Health Service? Int J Health Policy Manag. 2015;5(1):55–7.
Edwards N, Saltman RB. Re-thinking barriers to organizational change in public hospitals. Isr J Health Policy Res. 2017;6:8.
Giusto M, Lattanzi B, Albanese C, et al. Sarcopenia in liver cirrhosis: the role of computed tomography scan for the assessment of muscle mass compared with dual-energy X‐ray absorptiometry and anthropometry. Eur J Gastroenterol Hepatol. 2015;27:328–34.
Lee DH, Keum N, Hu FB, et al. Development and validation of anthropometric prediction equations for lean body mass, fat mass and percent fat in adults using the National Health and Nutrition Examination Survey (NHANES) 1999-2006. Br J Nutr. 2017;118:858–66.
Landi F, Onder G, Russo A, et al. Calf circumference, frailty and physical performance among older adults living in the community. Clin Nutr. 2014;33:539–44.
Beaudart C, McCloskey E, Bruyere O, et al. Sarcopenia in daily practice: assessment and management. BMC Geriatr. 2016;16:170.
Ni M, Brown LG, Lawler D, et al. Reliability, validity, and minimal detectable change of four-step stair climb power test in community‐dwelling older adults. Phys Ther. 2017;97:767–73.
Ascenzi F, Barberi L, Dobrowolny G, Villa Nova Bacurau A, Nicoletti C, Rizzuto E, Rosenthal N, Scicchitano BM, Musarò A. Effects of IGF-1 isoforms on muscle growth and sarcopenia. Aging Cell. 2019 Jun;18(3):e12954.
Bian A, Ma Y, Zhou X, Guo Y, Wang W, Zhang Y, Wang X. Association between sarcopenia and levels of growth hormone and insulin-like growth factor-1 in the elderly. BMC Musculoskelet Disord. 2020 Apr 7;21(1):214.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This paper is devoid of any conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Johri, N., Vengat, M., Kumar, D. et al. A comprehensive review on the risks assessment and treatment options for Sarcopenia in people with diabetes. J Diabetes Metab Disord 22, 995–1010 (2023). https://doi.org/10.1007/s40200-023-01262-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-023-01262-w