Abstract
Purpose
Non-alcoholic fatty liver disease (NAFLD) is caused by the increase of fat in the liver. The present study aimed to study the association between different dietary patterns and NAFLD in adults.
Methods
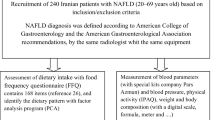
This study included 121 adult patients with NAFLD and 119 non-NAFLD. Dietary intake was calculated by a 168-item food frequency questionnaire. Biochemical markers were measured. Dietary patterns were determined by factor analysis. The association between dietary patterns and NAFLD was evaluated using multiple logistic regression analysis.
Results
Two dietary patterns (healthy, western) were recognized in participants. Western dietary pattern was related with 72 percent increase in the odds of NAFLD (OR: 1.72; 95% CI: 1.32,2.14), after adjustment for covariates. Healthy dietary pattern was associated with 38 percent lower odds of NAFLD (OR: 0.38; 95% CI: 0.11, 0.65). Adherence to the western diet was related to 0.486 greater amounts of ALT, 3.248 mg/dl higher levels of FBS, and 3.989 mg/dl greater amounts of TG and 2.354 mg/dl greater amounts of MDA after adjusting for confounding factors (p > 0.001, p = 0.042, p > 0.001, p = 0.036 respectively). The healthy dietary pattern score was negatively associated with FBS and Cholesterol and TG levels (p = 0.035, p = 0.048, and p = 0.025), respectively. Moreover, it was associated with 3.211 mg/dl higher levels of TAC (p = 0.049).
Conclusions
There is a significant relationship between dietary patterns and non-alcoholic fatty liver disease. Adherence to a western dietary pattern is related to an increase in non-alcoholic fatty liver disease.


Similar content being viewed by others
References
Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA. 2015;313(22):2263–73.
Younossi ZM, Blissett D, Blissett R, Henry L, Stepanova M, Younossi Y, et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology. 2016;64(5):1577–86.
Kumar R, Priyadarshi RN, Anand U. Non-alcoholic fatty liver disease: growing burden, adverse outcomes and associations. J Clin Transl Hepatol. 2020;8(1):76.
Ferramosca A, Di Giacomo M, Zara V. Antioxidant dietary approach in treatment of fatty liver: New insights and updates. World J Gastroenterol. 2017;23(23):4146.
Mokhtari Z, Gibson DL, Hekmatdoost A. Nonalcoholic fatty liver disease, the gut microbiome, and diet. Adv Nutr. 2017;8(2):240–52.
Okanoue T, Umemura A, Yasui K, Itoh Y. Nonalcoholic fatty liver disease and nonalcoholic steatohepatitis in Japan. J Gastroenterol Hepatol. 2011;26:153–62.
Ballestri S, Nascimbeni F, Baldelli E, Marrazzo A, Romagnoli D, Lonardo A. NAFLD as a sexual dimorphic disease: role of gender and reproductive status in the development and progression of nonalcoholic fatty liver disease and inherent cardiovascular risk. Adv Ther. 2017;34(6):1291–326.
Vos MB, Colvin R, Belt P, Molleston JP, Murray KF, Rosenthal P, et al. Correlation of vitamin E, uric acid and diet composition with histologic features of pediatric nonalcoholic fatty liver disease. J Pediatr Gastroenterol Nutr. 2012;54(1):90.
Cheah MC, McCullough AJ, Goh GB. Dietary manipulations for nonalcoholic fatty liver disease (NAFLD). Bioactive food as dietary interventions for diabetes: Elsevier; 2019. p. 69–88.
Mirmiran P, Amirhamidi Z, Ejtahed H-S, Bahadoran Z, Azizi F. Relationship between diet and non-alcoholic fatty liver disease: a review article. Iran J Public Health. 2017;46(8):1007.
Heinonen I, Rinne P, Ruohonen S, Ruohonen S, Ahotupa M, Savontaus E. The effects of equal caloric high fat and western diet on metabolic syndrome, oxidative stress and vascular endothelial function in mice. Acta Physiol. 2014;211(3):515–27.
Lampret BR, Murko S, Tanšek MŽ, Podkrajšek KT, Debeljak M, Šmon A, et al. Selective Screening for Metabolic Disorders in the Slovenian Pediatric Population/Selektivni Skrining Metaboličkih Poremećaja Kod Dečije Populacije U Sloveniji. Journal of medical biochemistry. 2014;34(1):58–63.
Tan BL, Norhaizan ME, Liew W-P-P, Sulaiman Rahman H. Antioxidant and oxidative stress: a mutual interplay in age-related diseases. Frontiers in pharmacology. 2018;9:1162.
Alavian SM, Esmaillzadeh A, Adibi P, Azadbakht L. Dietary quality indices and biochemical parameters among patients with non alcoholic fatty liver disease (NAFLD). Hepatitis monthly. 2013;13(7).
Di Minno MND, Russolillo A, Lupoli R, Ambrosino P, Di Minno A, Tarantino G. Omega-3 fatty acids for the treatment of non-alcoholic fatty liver disease. World J Gastroenterol: WJG. 2012;18(41):5839.
Yang X, Deng F. Iron overload is associated with non-alcoholic fatty liver disease (NAFLD): results from The NHANES III survey. European Journal of BioMedical Research. 2017;3(1):10–5.
Jia Q, Xia Y, Zhang Q, Wu H, Du H, Liu L, et al. Dietary patterns are associated with prevalence of fatty liver disease in adults. Eur J Clin Nutr. 2015;69(8):914–21.
Zelber-Sagi S, Nitzan-Kaluski D, Goldsmith R, Webb M, Blendis L, Halpern Z, et al. Long term nutritional intake and the risk for non-alcoholic fatty liver disease (NAFLD): a population based study. J Hepatol. 2007;47(5):711–7.
Kim H-Y, Lee J, Kim J. Association between dietary inflammatory index and metabolic syndrome in the general Korean population. Nutrients. 2018;10(5):648.
Mirmiran P, Esfahani FH, Mehrabi Y, Hedayati M, Azizi F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr. 2010;13(5):654–62.
Azar M, Sarkisian E. Food composition table of Iran: National Nutrition and food research institute. Tehran: Shaheed Beheshti University; 1980.
US Department of Agriculture ARS. USDA national nutrient database for standard reference, release 28. Nutrient data laboratory home page. 2011.
Ghafarpour M, Houshiar-Rad A, Kianfar H, Ghaffarpour M. The manual for household measures, cooking yields factors and edible portion of food. Tehran: Keshavarzi Press; 1999.
Aadahl M, Jørgensen T. Validation of a new self-report instrument for measuring physical activity. Med Sci Sports Exerc. 2003;35(7):1196–202.
Ohkawa H, Ohishi N, Yagi K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem. 1979;95(2):351–8.
Benzie IF, Strain JJ. The ferric reducing ability of plasma (FRAP) as a measure of “antioxidant power”: the FRAP assay. Anal Biochem. 1996;239(1):70–6.
Samuels P. Advice on exploratory factor analysis. 2017.
Sherzai A, Heim LT, Boothby C, Sherzai AD. Stroke, food groups, and dietary patterns: a systematic review. Nutr Rev. 2012;70(8):423–35.
Oddy WH, Herbison CE, Jacoby P, Ambrosini GL, O’sullivan TA, Ayonrinde OT, et al. The Western dietary pattern is prospectively associated with nonalcoholic fatty liver disease in adolescence. Am J Gastroenterol. 2013;108(5):778–85.
Shim P, Choi D, Park Y. Association of blood fatty acid composition and dietary pattern with the risk of non-alcoholic fatty liver disease in patients who underwent cholecystectomy. Ann Nutr Metab. 2017;70(4):303–11.
Chung GE, Youn J, Kim YS, Lee JE, Yang SY, Lim JH, et al. Dietary patterns are associated with the prevalence of nonalcoholic fatty liver disease in Korean adults. Nutrition. 2019;62:32–8.
Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation. 2016;133(2):187–225.
Zelber-Sagi S, Ivancovsky-Wajcman D, Isakov NF, Webb M, Orenstein D, Shibolet O, et al. High red and processed meat consumption is associated with non-alcoholic fatty liver disease and insulin resistance. J Hepatol. 2018;68(6):1239–46.
Hashemian M, Merat S, Poustchi H, Jafari E, Radmard A-R, Kamangar F, et al. Red meat consumption and risk of nonalcoholic fatty liver disease in a population with low meat consumption: the golestan cohort study. Am J Gastroenterol. 2021;116(8):1667–75.
Peng H, Xie X, Pan X, Zheng J, Zeng Y, Cai X, et al. Association of meat consumption with NAFLD risk and liver-related biochemical indexes in older Chinese: a cross-sectional study. BMC Gastroenterol. 2021;21(1):1–11.
Lee JW, Park SH. Association between depression and nonalcoholic fatty liver disease: Contributions of insulin resistance and inflammation. J Affect Disord. 2021;278:259–63.
Chao H-W, Chao S-W, Lin H, Ku H-C, Cheng C-F. Homeostasis of glucose and lipid in non-alcoholic fatty liver disease. Int J Mol Sci. 2019;20(2):298.
Dhibi M, Brahmi F, Mnari A, Houas Z, Chargui I, Bchir L, et al. The intake of high fat diet with different trans fatty acid levels differentially induces oxidative stress and non alcoholic fatty liver disease (NAFLD) in rats. Nutr Metab. 2011;8(1):65.
Luo Y, Burrington CM, Graff EC, Zhang J, Judd RL, Suksaranjit P, et al. Metabolic phenotype and adipose and liver features in a high-fat Western diet-induced mouse model of obesity-linked NAFLD. American Journal of Physiology-Endocrinology and Metabolism. 2016;310(6):E418–39.
Tetri LH, Basaranoglu M, Brunt EM, Yerian LM, Neuschwander-Tetri BA. Severe NAFLD with hepatic necroinflammatory changes in mice fed trans fats and a high-fructose corn syrup equivalent. American Journal of Physiology-Gastrointestinal and Liver Physiology. 2008;295(5):G987-G95.
Doost Mohammadi F, Vazirinejad R, Rezaeian M, Vazirinejad E, Bastam D, Ahmadinia H, et al. Fast food consumption and the risk of non-alcoholic fatty liver in adults: A community-based case-control study. Journal of Occupational Health and Epidemiology. 2019;8(4):176–84.
Scapaticci S, D’Adamo E, Mohn A, Chiarelli F, Giannini C. Non-alcoholic fatty liver disease in obese youth with insulin resistance and type 2 diabetes. Frontiers in Endocrinology. 2021;12.
Khatatbeh M, Momani W, Altaani Z, Al Saad R, Al Bourah AR. Fast food consumption, liver functions, and change in body weight among university students: A cross-sectional study. International Journal of Preventive Medicine. 2021;12.
Pistollato F, Iglesias RC, Ruiz R, Aparicio S, Crespo J, Lopez LD, et al. Nutritional patterns associated with the maintenance of neurocognitive functions and the risk of dementia and Alzheimer’s disease: A focus on human studies. Pharmacol Res. 2018;131:32–43.
Fakhoury-Sayegh N, Younes H, Heraoui GN, Sayegh R. Nutritional profile and dietary patterns of lebanese non-alcoholic fatty liver disease patients: a case-control study. Nutrients. 2017;9(11):1245.
Adriano LS, de Carvalho Sampaio HA, Arruda SPM, de Melo Portela CL, de Melo MLP, Carioca AAF, et al. Healthy dietary pattern is inversely associated with non-alcoholic fatty liver disease in elderly. Br J Nutr. 2016;115(12):2189–95.
Yang C-Q, Shu L, Wang S, Wang J-J, Zhou Y, Xuan Y-J, et al. Dietary patterns modulate the risk of non-alcoholic fatty liver disease in Chinese adults. Nutrients. 2015;7(6):4778–91.
Arendt BM, Allard JP. Effect of atorvastatin, vitamin E and C on nonalcoholic fatty liver disease: is the combination required? Am J Gastroenterol. 2011;106(1):78–80.
Musso G, Gambino R, De Michieli F, Cassader M, Rizzetto M, Durazzo M, et al. Dietary habits and their relations to insulin resistance and postprandial lipemia in nonalcoholic steatohepatitis. Hepatology. 2003;37(4):909–16.
Geetha K, Yankanchi GM, Hulamani S, Hiremath N. Glycemic index of millet based food mix and its effect on pre diabetic subjects. Journal of Food Science and Technology. 2020:1–7.
Xia Y, Lu Z, Lu M, Liu M, Liu L, Meng G, et al. Raw orange intake is associated with higher prevalence of non-alcoholic fatty liver disease in an adult population. Nutrition. 2019;60:252–60.
Tajima R, Kimura T, Enomoto A, Saito A, Kobayashi S, Masuda K, et al. No association between fruits or vegetables and non-alcoholic fatty liver disease in middle-aged men and women. Nutrition. 2019;61:119–24.
Venkatachalam M, Sathe SK. Chemical composition of selected edible nut seeds. J Agric Food Chem. 2006;54(13):4705–14.
bing Chen B, Han Y, Pan X, Yan J, Liu W, Li Y, et al. Association between nut intake and non-alcoholic fatty liver disease risk: a retrospective case-control study in a sample of Chinese Han adults. BMJ open. 2019;9(9):e028961.
Zhang S, Fu J, Zhang Q, Liu L, Meng G, Yao Z, et al. Association between nut consumption and non-alcoholic fatty liver disease in adults. Liver Int. 2019;39(9):1732–41.
Plaz Torres MC, Bodini G, Furnari M, Marabotto E, Zentilin P, Giannini EG. Nuts and Non-Alcoholic Fatty Liver Disease: Are Nuts Safe for Patients with Fatty Liver Disease? Nutrients. 2020;12(11):3363.
Bowen J, Luscombe-Marsh ND, Stonehouse W, Tran C, Rogers GB, Johnson N, et al. Effects of almond consumption on metabolic function and liver fat in overweight and obese adults with elevated fasting blood glucose: A randomised controlled trial. Clinical nutrition ESPEN. 2019;30:10–8.
Agebratt C, Ström E, Romu T, Dahlqvist-Leinhard O, Borga M, Leandersson P, et al. A randomized study of the effects of additional fruit and nuts consumption on hepatic fat content, cardiovascular risk factors and basal metabolic rate. PloS one. 2016;11(1):e0147149.
Sirota R, Gorelik S, Harris R, Kohen R, Kanner J. Coffee polyphenols protect human plasma from postprandial carbonyl modifications. Mol Nutr Food Res. 2013;57(5):916–9.
D Archivio M, Filesi C, Di Benedetto R, Gargiulo R, Giovannini C, Masella R. Polyphenols, dietary sources and bioavailability. Annali-Istituto Superiore di Sanita. 2007;43(4):348.
Bonita JS, Mandarano M, Shuta D, Vinson J. Coffee and cardiovascular disease: in vitro, cellular, animal, and human studies. Pharmacol Res. 2007;55(3):187–98.
Shen H, Rodriguez AC, Shiani A, Lipka S, Shahzad G, Kumar A, et al. Association between caffeine consumption and nonalcoholic fatty liver disease: a systemic review and meta-analysis. Ther Adv Gastroenterol. 2016;9(1):113–20.
Hayat U, Siddiqui AA, Okut H, Afroz S, Tasleem S, Haris A. The effect of coffee consumption on the non-alcoholic fatty liver disease and liver fibrosis: A meta-analysis of 11 epidemiological studies. Annals of Hepatology. 2021;20:100254.
Panchal SK, Poudyal H, Waanders J, Brown L. Coffee extract attenuates changes in cardiovascular and hepatic structure and function without decreasing obesity in high-carbohydrate, high-fat diet-fed male rats. J Nutr. 2012;142(4):690–7.
Bambha K, Wilson LA, Unalp A, Loomba R, Neuschwander-Tetri BA, Brunt EM, et al. Coffee consumption in NAFLD patients with lower insulin resistance is associated with lower risk of severe fibrosis. Liver Int. 2014;34(8):1250–8.
Alferink LJ, Fittipaldi J, Kiefte-de Jong JC, Taimr P, Hansen BE, Metselaar HJ, et al. Coffee and herbal tea consumption is associated with lower liver stiffness in the general population: The Rotterdam study. J Hepatol. 2017;67(2):339–48.
Zou Y, Zhong L, Hu C, Sheng G. Association between the alanine aminotransferase/aspartate aminotransferase ratio and new-onset non-alcoholic fatty liver disease in a nonobese Chinese population: a population-based longitudinal study. Lipids Health Dis. 2020;19(1):1–10.
Buzzetti E, Pinzani M, Tsochatzis EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism. 2016;65(8):1038–48.
Romero-Polvo A, Denova-Gutiérrez E, Rivera-Paredez B, Castañón S, Gallegos-Carrillo K, Halley-Castillo E, et al. Association between dietary patterns and insulin resistance in Mexican children and adolescents. Ann Nutr Metab. 2012;61(2):142–50.
De Biase SG, Fernandes SFC, Gianini RJ, Duarte JLG. Vegetarian diet and cholesterol and triglycerides levels. Arq Bras Cardiol. 2007;88(1):35.
Acknowledgements
This study was extracted from MSc dissertation, which was approved by School of Nutrition & Food Science, Isfahan University of Medical Sciences. We would like to express our appreciation for all those participating in this study for their sincere cooperation.
Funding
This work was supported by the Isfahan University of Medical Sciences [grant numbers IR.MUI.REC. 1398.279].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moradi, F., Moosavian, S.P., Djafari, F. et al. The association between major dietary patterns with the risk of non-alcoholic fatty liver disease, oxidative stress and metabolic parameters: A case–control study. J Diabetes Metab Disord 21, 657–667 (2022). https://doi.org/10.1007/s40200-022-01028-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-022-01028-w