Abstract
Purpose
This prospective study aimed to detect and identify plasma proteins differentially expressed between groups of Brazilian diagnosed with type 1 (T1DM), type 2 (T2DM) diabetes with good and poor glycemic control and the non-diabetic group denominated control group (CG).
Methods
Patients with T1DM and T2DM were subdivided according to their glycated haemoglobin (HbA1c) level: ≥ 53 mmol/mol and < 53 mmol/mol. Each subgroup was composed of ten subjects (n = 10). The plasma from each subgroup was pooled and depleted of albumin and IgG. The reminiscent proteins were quantified and separated by sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS–PAGE). The relative volume of protein bands was determined by densitometry analysis, and those with differential abundance were identified by MALDI-TOF mass spectrometry.
Results
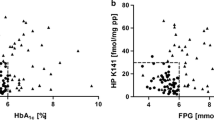
Alpha 2 - Macroglobulin (AMG) was 1.3-fold more abundant in T1DM with HbA1c ≥ 53 mmol/mol and < 53 mmol/mol and 1.4-fold more abundant in T2DM with HbA1c ≥ 53 mmol/mol compared to CG. Ceruloplasmin (Cp) and Haptoglobin (Hp) were overexpressed above 1.5-fold in all DM subgroups. Cp in T1DM and Hp in both types of DM were more expressed in HbA1c ≥ 53 mmol/mol than <53 mmol/mol. Apolipoprotein A-I (Apo A-I) was upregulated only in T2DM subgroups.
Conclusion
In summary, three positive acute-phase proteins, AMG, Cp and Hp were more abundant in diabetic individuals regardless of the diabetes type. The highest Hp abundance in both types of DM with HbA1c ≥ 53 mmol/mol, reinforces Hp as a possible biomarker associated with diabetic complications.




Similar content being viewed by others
References
International Diabetes Federation. IDF Diabetes Atlas, 9th Edn. Brussels, Belgium.; 2019.
Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2020. American Diabetes Association. Diabetes Care. 2020;43 (Supplement 1):S14-S31.
Amin Mohsin Z, Paul A, Devendra S. Pitfalls of using HbA 1c in the diagnosis and monitoring of diabetes. London J Prim Care (Abingdon). 2015;7(4):66–9.
Frantzi M, Bhat A, Latosinska A. Clinical proteomic biomarkers: relevant issues on study design & technical considerations in biomarker development. Clin Transl Med. 2014;3(7):1–22.
Beijer K, Nowak C, Sundström J, Ärnlöv J, Fall T, Lind L. In search of causal pathways in diabetes: a study using proteomics and genotyping data from a cross-sectional study. Diabetologia. 2019;62(11):1998–2006.
Candiano G, Bruschi M, Musante L, Santucci L, Ghiggeri GM, Carnemolla B, et al. Blue silver: a very sensitive colloidal Coomassie G-250 staining for proteome analysis. Electrophoresis. 2004;25(9):1327–33.
Lahiri DK, Nurnberger JI. A rapid non-enzymatic method for the preparation of HMW DNA from blood for RFLP studies. Nucleic Acids Res. 1991;19(19):1.
Koch W, Latz W, Eichinger M, Roguin A, Levy AP, Schömig A, et al. Genotyping of the common haptoglobin Hp 1/2 polymorphism based on PCR. Clin Chem. 2002;48(9):1377–82.
Takada T, Kodera Y, Matsubara M, Kawashima Y, Maeda T, Fujita Y, et al. Serum monomeric α2-macroglobulin as a clinical biomarker in diabetes. Atherosclerosis. 2013;228(1):270–6.
Yoshino S, Fujimoto K, Takada T, et al. Molecular form and concentration of serum α2-macroglobulin in diabetes. Sci Rep. 2019;9(1):1–10.
Lu CH, Lin ST, Chou HC, Lee YR, Chan HL. Proteomic analysis of retinopathy-related plasma biomarkers in diabetic patients. Arch Biochem Biophys. 2013;529(2):146–56.
Annapoorani P, Dhandapany PS, Sadayappan S, Ramasamy S, Rathinavel A, Selvam GS. Cardiac isoform of alpha-2 macroglobulin-a new biomarker for myocardial infarcted diabetic patients. Atherosclerosis. 2006;186(1):173–6.
Aitken JP, Ortiz C, Morales-Bozo I, Rojas-Alcayaga G, Baeza M, Beltran C, et al. Α-2-macroglobulin in saliva is associated with glycemic control in patients with type 2 diabetes mellitus. Dis Markers. 2015;2015:1–5.
Chung TJ, Hsu KY, Chen JH, Liu JS, Chang HW, Li PF, et al. Association of salivary alpha 2-macroglobulin levels and clinical characteristics in type 2 diabetes. J Diabetes Investig. 2016;7(2):190–6.
Rehman AA, Ahsan H, Khan FH. Alpha-2-macroglobulin: a physiological guardian. J Cell Physiol. 2013;228(8):1665–75.
Cunninghamn J, Leffell M, Mearkle P, Harmatz P. Elevated plasma ceruloplasmin in insulin-dependent diabetes mellitus: evidence for increased oxidative stress as a variable complication. Metabolism. 1995;44(8):996–9.
Daimon M, Susa S, Yamatani K, Manaka H, Hama K, Kimura M, et al. Hyperglycemia is a factor for an increase in serum ceruloplasmin in type 2 diabetes. Diabetes Care. 1998;21(9):1525–8.
Lee MJ, Jung CH, Kang YM, Jang JE, Leem J, Park JY, et al. Serum Ceruloplasmin level as a predictor for the progression of diabetic nephropathy in Korean men with type 2 diabetes mellitus. Diabetes Metab J. 2015;39(3):230–9.
Nowak M, Wielkoszyński T, Marek B, Kos-Kudła B, Świętochowska E, Siemińska L, et al. Antioxidant potential, paraoxonase 1, ceruloplasmin activity and C-reactive protein concentration in diabetic retinopathy. Clin Exp Med. 2010;10(3):185–92.
Linder MC. Ceruloplasmin and other copper binding components of blood plasma and their functions: an update. Metallomics. 2016;8(9):887–905.
Leoni V, Albertini R, Passi A, Abuja PM, Borroni P, d'Eril GM, et al. Glucose accelerates copper- and Ceruloplasmin-induced oxidation of low-density lipoprotein and whole serum. Free Radic Res. 2002;36(5):521–9.
Liu Z, Feng D, Gu D, Zheng R, Esperat C, Gao W. Differentially expressed haptoglobin as a potential biomarker for type 2 diabetic mellitus in Hispanic population. BioFactors. 2017;43(3):424–33.
Rodrigues KF, Pietrani NT, Carvalho LML, Bosco AA, Sandrim VC, Ferreira CN, et al. Haptoglobin levels are influenced by Hp1–Hp2 polymorphism, obesity, inflammation, and hypertension in type 2 diabetes mellitus. Endocrinol Diabetes y Nutr. 2019;66(2):99–107.
MacKellar M, Vigerust DJ. Role of haptoglobin in health and disease: a focus on diabetes. Clin Diabetes. 2016;34(3):148–57.
Langlois MR, Delanghe JR. Biological and Clinical Significance of Haptoglobin Polymorphism in Humans. 1996;42(10):1589–600.
Sadrzadeh SMH, Bozorgmehr J. Haptoglobin phenotypes in health and disorders. Am J Clin Pathol. 2004;121(Suppl 1):97–104.
Asleh R, Marsh S, Shilkrut M, Binah O, Guetta J, Lejbkowicz F, et al. Genetically determined heterogeneity in hemoglobin scavenging and susceptibility to diabetic cardiovascular disease. Circ Res. 2003;92(11):1193–200.
Levy AP, Hochberg I, Jablonski K, Resnick HE, Lee ET, Best L, et al. Haptoglobin phenotype is an independent risk factor for cardiovascular disease in individuals with diabetes: the strong heart study. J Am Coll Cardiol. 2002;40(11):1984–90.
Asleh R, Guetta J, Kalet-Litman S, Miller-Lotan R, Levy AP. Haptoglobin genotype- and diabetes-dependent differences in iron-mediated oxidative stress in vitro and in vivo. Circ Res. 2005;96(4):435–41.
Cahill LE, Jensen MK, Chiuve SE, Shalom H, Pai JK, Flint AJ, et al. The risk of coronary heart disease associated with glycosylated hemoglobin of 6.5% or greater is pronounced in the haptoglobin 2-2 genotype. J Am Coll Cardiol. 2015;66(16):1791–9.
Mangaraj M, Nanda R, Panda S. Apolipoprotein A-I: a molecule of diverse function. Indian J Clin Biochem. 2016;31(3):253–9.
Heier M, Borja MS, Brunborg C, et al. Reduced HDL function in children and young adults with type 1 diabetes. Cardiovasc Diabetol. 2017;16(1):1–8.
Hashemi M, Saadat M, Behjati M, Kelishadi R. Comparison of serum Apolipoprotein levels of diabetic children and healthy children with or without diabetic parents. Cholesterol. 2012;2012:1–4.
Riaz S, Alam SS, Akhtar MW. Proteomic identification of human serum biomarkers in diabetes mellitus type 2. J Pharm Biomed Anal. 2010;51(5):1103–7.
Wu X, Yu Z, Su W, Isquith DA, Neradilek MB, Lu N, et al. Low levels of ApoA1 improve risk prediction of type 2 diabetes mellitus. J Clin Lipidol. 2017;11(2):362–8.
Jaleel A, Henderson GC, Madden BJ, Klaus KA, Morse DM, Gopala S, et al. Identification of de novo synthesized and relatively older proteins. Accelerated oxidative damage to de novo synthesized Apolipoprotein A-1 in type 1 diabetes. Diabetes. 2010;59(10):2366–74.
Ory DS, Schaffer JE. ApoA-1 in diabetes: damaged goods. Diabetes. 2010;59(10):2358–9.
Goldenstein H, Levy NS, Ward J, Costacou T, Levy AP. Haptoglobin genotype is a determinant of hemoglobin adducts and vitamin E content in HDL. J Diabetes Res. 2018;2018:1–6.
Acknowledgements
This study was supported by the National Council for Scientific and Technological Development (CNPq, grant number: 456684/2014-0).
Availability of data and material
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Funding
This study was supported by National Council for Scientific and Technological Development [CNPq, grant number: 456684/2014–0].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved under the number CAAE n° 01038112.0.0000.0102 by the Ethical Committee of the Federal University of Paraná .
Consent of participate
All participants voluntarily agreed to participate in the research.
Consent for publication
All authors consent to the publication of the manuscript.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Paula Silva, L., de Moraes Rego, F.G., Picheth, G. et al. Prospection of plasma proteins as biomarkers for diabetes mellitus monitoring. J Diabetes Metab Disord 20, 611–620 (2021). https://doi.org/10.1007/s40200-021-00788-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-021-00788-1