Abstract
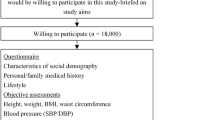
A low level of physical activity has a potential association with high levels of homocysteine, which implies an increased chance of older adults with type 2 diabetes mellitus developing cardiovascular disease (CVD). However, the effects of physical activity on homocysteine levels have been poorly explored in the literature. Therefore, this study compared homocysteine levels and cardiovascular risk among physically active and inactive older women with type 2 diabetes mellitus. Fifty-nine women with type 2 diabetes mellitus, between 60 and 91 years old, were evaluated. The level of physical activity was assessed using the International Physical Activity Questionnaire (IPAQ) long version to identify active and inactive older women. Blood samples were collected and anthropometric, body composition, and blood pressure measurements were performed to determine homocysteine levels and cardiovascular risk. The results demonstrated that active older women with type 2 diabetes mellitus have lower homocysteine values (F = 17.79, p < 0.001, ηp2 = 0.238), cardiovascular risk scores (F = 15.84, p = p < 0.001, ηp2 = 0.217), and waist circumferences (F = 2.95, p = 0.013, ηp2 = 0.049) when compared with inactive older women. It was concluded that there was a difference in the levels of homocysteine, cardiovascular risk, and waist circumference between active and inactive older women with type 2 diabetes. Active older women are less likely to have cardiovascular risk than inactive older women.


Similar content being viewed by others
Abbreviations
- CVD:
-
Cardiovascular disease
- NCDs:
-
Non-communicable diseases
- IPAQ:
-
International physical activity questionnaire
- ICF:
-
Informed consent form
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- VLDL:
-
Very-low-density lipoprotein
- EDTA:
-
Ethylenediaminetetraacetic acid
- HbA1c:
-
Glycated hemoglobin
- HPLC:
-
High-performance liquid chromatography
- SPSS:
-
Statistical Package for the Social Sciences
- BMI:
-
Body mass index
- MVPA:
-
Physical activity of moderate to vigorous intensity
References
Chadt A, Al-Hasani H. Glucose transporters in adipose tissue, liver, and skeletal muscle in metabolic health and disease. Pflugers Arch. 2020;472(9):1273–98. https://doi.org/10.1007/s00424-020-02417-x.
Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol. 2018;17(1):83. https://doi.org/10.1186/s12933-018-0728-6.
Collaborators GBDCoD. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1151–210. https://doi.org/10.1016/S0140-6736(17)32152-9.
Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2(2):1143–211. https://doi.org/10.1002/cphy.c110025.
Booth FW, Roberts CK, Thyfault JP, Ruegsegger GN, Toedebusch RG. Role of inactivity in chronic diseases: evolutionary insight and pathophysiological mechanisms. Physiol Rev. 2017;97(4):1351–402. https://doi.org/10.1152/physrev.00019.2016.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62. https://doi.org/10.1136/bjsports-2020-102955.
Jefferis BJ, Sartini C, Lee IM, Choi M, Amuzu A, Gutierrez C, et al. Adherence to physical activity guidelines in older adults, using objectively measured physical activity in a population-based study. BMC Public Health. 2014;14:382. https://doi.org/10.1186/1471-2458-14-382.
Ortlieb S, Gorzelniak L, Nowak D, Strobl R, Grill E, Thorand B, et al. Associations between multiple accelerometry-assessed physical activity parameters and selected health outcomes in elderly people--results from the KORA-age study. PLoS One. 2014;9(11):e111206. https://doi.org/10.1371/journal.pone.0111206.
Dos Santos CES, Manta SW, Maximiano GP, Confortin SC, Benedetti TRB, d'Orsi E, et al. Accelerometer-measured physical activity and sedentary behavior: a cross-sectional study of Brazilian older adults. J Phys Act Health. 2018;15(11):811–8. https://doi.org/10.1123/jpah.2017-0456.
Ribeiro A, Verlengia R, de Oliveira MRM, Oliveira MVA, Pellegrinotti IL, Crisp AH. Compliance of the physical activity guidelines accumulated in bouts >/=10 min and Nonbouts and its association with body composition and physical function: a cross-sectional study in Brazilian older adults. J Aging Phys Act. 2020; 22:1-8. https://doi.org/10.1123/japa.2020-0181.
Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–29. https://doi.org/10.1016/S0140-6736(12)61031-9.
United Nations. Department of Economic and Social Affairs, population division. World population prospects: the 2015 revision. New York: United Nations; 2015.
de Rezende LF, Rabacow FM, Viscondi JY, Luiz Odo C, Matsudo VK, Lee IM. Effect of physical inactivity on major noncommunicable diseases and life expectancy in Brazil. J Phys Act Health. 2015;12(3):299–306. https://doi.org/10.1123/jpah.2013-0241.
Okura T, Rankinen T, Gagnon J, Lussier-Cacan S, Davignon J, Leon AS, et al. Effect of regular exercise on homocysteine concentrations: the HERITAGE family study. Eur J Appl Physiol. 2006;98(4):394–401. https://doi.org/10.1007/s00421-006-0294-6.
Silva ASMM. Effects of physical activity and training programs on plasma homocysteine levels: a systematic review. Amino Acids. 2014;46(8):1795–804. https://doi.org/10.1007/s00726-014-1741-z.
Han L, Liu Y, Wang C, Tang L, Feng X, Astell-Burt T, et al. Determinants of hyperhomocysteinemia in healthy and hypertensive subjects: a population-based study and systematic review. Clin Nutr. 2017;36(5):1215–30. https://doi.org/10.1016/j.clnu.2016.11.011.
Neves LBMD, Lopes AC. Homocisteína. J Bras Patol Med Lab. 2004;40:311–20.
Rehman T, Shabbir MA, Inam-Ur-Raheem M, Manzoor MF, Ahmad N, Liu ZW, et al. Cysteine and homocysteine as biomarker of various diseases. Food Sci Nutr. 2020;8(9):4696–707. https://doi.org/10.1002/fsn3.1818.
Muniz MT, Siqueira ER, Fonseca RA, D'Almeida V, Hotta JK, dos Santos JE, et al. Evaluation of MTHFR C677T gene polymorphism and homocysteine level in coronary atherosclerotic disease. Arq Bras Endocrinol Metabol. 2006;50(6):1059–65. https://doi.org/10.1590/s0004-27302006000600012.
Wolfgang HOR, Jouma M. Hyperhomocysteinemia and vitamin B-12 deficiency are more striking in Syrians than in Germans - causes and implications. Atherosclerosis. 2003;166(1):143–50. https://doi.org/10.1016/s0021-9150(02)00320-9.
Anderson JL, Muhlestein JB, Horne BD, Carlquist JF, Bair TL, Madsen TE, et al. Plasma homocysteine predicts mortality independently of traditional risk factors and C-reactive protein in patients with angiographically defined coronary artery disease. Circulation. 2000;102(11):1227–32. https://doi.org/10.1161/01.cir.102.11.1227.
Fan R, Zhang A, Zhong F. Association between Homocysteine levels and all-cause mortality: a dose-response meta-analysis of prospective studies. Sci Rep. 2017;7(1):4769. https://doi.org/10.1038/s41598-017-05205-3.
Alomari MA, Khabour OF, Gharaibeh MY, Qhatan RA. Effect of physical activity on levels of homocysteine, folate, and vitamin B12 in the elderly. Phys Sportsmed. 2016;44(1):68–73. https://doi.org/10.1080/00913847.2016.1135037.
Benedetti TM, GZ, de Barros MVG. Aplicação do questionário internacional de atividades físicas para avaliação do nível de atividades física de mulheres idosas: Validade concorrente e reprodutibilidade teste-reteste. Rev Bras Ciênc Mov. 2008;12(1):25–34.
Ichinose S, Nakamura M, Maeda M, Ikeda R, Wada M, Nakazato M, et al. A validated HPLC-fluorescence method with a semi-micro column for routine determination of homocysteine, cysteine and cysteamine, and the relation between the thiol derivatives in normal human plasma. Biomed Chromatogr. 2009;23(9):935–9. https://doi.org/10.1002/bmc.1205.
Ferin R, Pavao ML, Baptista J. Methodology for a rapid and simultaneous determination of total cysteine, homocysteine, cysteinylglycine and glutathione in plasma by isocratic RP-HPLC. J Chromatogr B Analyt Technol Biomed Life Sci. 2012;911:15–20. https://doi.org/10.1016/j.jchromb.2012.10.022.
Sawula W, Banecka-Majkutewicz Z, Kadzinski L, Jakobkiewicz-Banecka J, Wegrzyn G, Nyka W, et al. Improved HPLC method for total plasma homocysteine detection and quantification. Acta Biochim Pol. 2008;55(1):119–25.
Vincent KR, Braith RW, Bottiglieri T, Vincent HK, Lowenthal DT. Homocysteine and lipoprotein levels following resistance training in older adults. Prev Cardiol. 2003;6(4):197–203. https://doi.org/10.1111/j.1520-037x.2003.01723.x.
Chen SM, Shen FC, Chen JF, Chang WD, Chang NJ. Effects of Resistance Exercise on Glycated Hemoglobin and Functional Performance in Older Patients with Comorbid Diabetes Mellitus and Knee Osteoarthritis: A Randomized Trial. Int J Environ Res Public Health. 2019;17(1):224. https://doi.org/10.3390/ijerph17010224.
Assmann G, Jabs HU, Kohnert U, Nolte W, Schriewer H. LDL-cholesterol determination in blood serum following precipitation of LDL with polyvinylsulfate. Clin Chim Acta. 1984;140(1):77–83. https://doi.org/10.1016/0009-8981(84)90153-0.
Martins RA, Verissimo MT, Coelho e Silva MJ, Cumming SP, Teixeira AM. Effects of aerobic and strength-based training on metabolic health indicators in older adults. Lipids Health Dis. 2010;9:76. https://doi.org/10.1186/1476-511X-9-76.
Gabriel R, Saiz C, Susi R, Alonso M, Vega S, Lopez I, et al. Epidemiology of lipid profile of the Spanish elderly population: the EPICARDIAN study. Med Clin (Barc). 2004;122(16):605–9. https://doi.org/10.1016/s0025-7753(04)74326-2.
D'Agostino RB Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: the Framingham heart study. Circulation. 2008;117(6):743–53. https://doi.org/10.1161/CIRCULATIONAHA.107.699579.
Stewart A, Marfell-Jones M, Olds T, Ridder H. International standards for anthropometric assessment. International Society for the Advancement of Kinanthropometry: Lower Hutt; 2011.
Orsatti FL, Nahas EA, Nahas-Neto J, Maesta N, Orsatti CL, Fernandes CE. Effects of resistance training and soy isoflavone on body composition in postmenopausal women. Obstet Gynecol Int. 2010;2010:156037. https://doi.org/10.1155/2010/156037.
Christos Z, Tokmakidis SP, Volaklis KA, Kotsa K, Touvra AM, et al. Lipoprotein proWle, glycemic control and physical Wtness after strength and aerobic training in post-menopausal women with type 2 diabetes. Eur J Appl Physiol. 2009;106:901–7. https://doi.org/10.1007/s00421-009-1104-8.
Durnin JV, Womersley J. Body fat assessed from total body density and its estimation from skinfold thickness: measurements on 481 men and women aged from 16 to 72 years. Br J Nutr. 1974;32(1):77–97. https://doi.org/10.1079/bjn19740060.
Rech C, Lima LRA, Cordeiro BA, Petroski EL, Vasconcelos FAG. Validity of anthropometric equations for estimating body fat in the elderly in southern Brazil. Braz J Cineanthropometry Hum Perform. 2010;12(1):1–7. https://doi.org/10.5007/1980-0037.2010v12n1p1.
Sink C, Mvududu NH. Statistical power, sampling, and effect sizes. Couns Outcome Res Eval. 2010;1(2):1–18. https://doi.org/10.1177/2150137810373613.
Buckner SL, Loenneke JP, Loprinzi PD. Single and combined associations of accelerometer-assessed physical activity and muscle-strengthening activities on plasma homocysteine in a national sample. Clin Physiol Funct Imaging. 2017;37(6):669–74. https://doi.org/10.1111/cpf.12356.
Hellgren M, Melander A, Ostgren CJ, Rastam L, Lindblad U. Inverse association between plasma homocysteine, sulphonylurea exposure and physical activity: a community-based sample of type 2 diabetes patients in the Skaraborg hypertension and diabetes project. Diabetes Obes Metab. 2005;7(4):421–9. https://doi.org/10.1111/j.1463-1326.2004.00431.x.
Unt E, Zilmer K, Magi A, Kullisaar T, Kairane C, Zilmer M. Homocysteine status in former top-level male athletes: possible effect of physical activity and physical fitness. Scand J Med Sci Sports. 2008;18(3):360–6. https://doi.org/10.1111/j.1600-0838.2007.00674.x.
Loprinzi PD, Cardinal BJ. Interrelationships among physical activity, depression, homocysteine, and metabolic syndrome with special considerations by sex. Prev Med. 2012;54(6):388–92. https://doi.org/10.1016/j.ypmed.2012.03.016.
Venâncio L, Burini RC, Yoshida WB. Dietary treatment of hyperhomocysteinemia in peripheral arterial disease. J Vasc Bras. 2010;9(1):28–41. https://doi.org/10.1590/S1677-54492010000100006.
Norlund L, Grubb A, Fex G, Leksell H, Nilsson JE, Schenck H, et al. The increase of plasma homocysteine concentrations with age is partly due to the deterioration of renal function as determined by plasma cystatin C. Clin Chem Lab Med. 1998;36(3):175–8. https://doi.org/10.1515/CCLM.1998.032.
Brosnan JT, Jacobs RL, Stead LM, Brosnan ME. Methylation demand: a key determinant of homocysteine metabolism. Acta Biochim Pol. 2004;51(2):405–13.
Malinow MR, Duell PB, Williams MA, Kruger WD, Evans AA, Anderson PH, et al. Short-term folic acid supplementation induces variable and paradoxical changes in plasma homocyst(e)ine concentrations. Lipids. 2001;36 Suppl:S27–32. https://doi.org/10.1007/s11745-001-0678-8.
Chen KJ, Pan WH, Yang FL, Wei IL, Shaw NS, Lin BF. Association of B vitamins status and homocysteine levels in elderly Taiwanese. Asia Pac J Clin Nutr. 2005;14(3):250–5.
Dankner RGG, Farber N, Novikov I, Segev S, Sela BA. Cardiorespiratory fitness and plasma homocysteine levels in adult males and females. Isr Med Assoc J. 2009;11(2):78–82.
Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123–32. https://doi.org/10.7326/M14-1651.
Baker PR, Costello JT, Dobbins M, Waters EB. The benefits and challenges of conducting an overview of systematic reviews in public health: a focus on physical activity. J Public Health (Oxf). 2014;36(3):517–21. https://doi.org/10.1093/pubmed/fdu050.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke Statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–360. https://doi.org/10.1161/CIR.0000000000000350.
Sattelmair J, Pertman J, Ding EL, Kohl HW 3rd, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation. 2011;124(7):789–95. https://doi.org/10.1161/CIRCULATIONAHA.110.010710.
Woodcock J, Franco OH, Orsini N, Roberts I. Non-vigorous physical activity and all-cause mortality: systematic review and meta-analysis of cohort studies. Int J Epidemiol. 2011;40(1):121–38. https://doi.org/10.1093/ije/dyq104.
Koning L, Merchant AT, Pogue J, Anand SS. Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: meta-regression analysis of prospective studies. Eur Heart J. 2007;28(7):850–6. https://doi.org/10.1093/eurheartj/ehm026.
Han TS, Tajar A, Lean ME. Obesity and weight management in the elderly. Br Med Bull. 2011;97:169–96. https://doi.org/10.1093/bmb/ldr002.
Figueiro TH, Arins GCB, Santos C, Cembranel F, Medeiros PA, d'Orsi E, et al. Association of objectively measured sedentary behavior and physical activity with cardiometabolic risk markers in older adults. PLoS One. 2019;14(1):e0210861. https://doi.org/10.1371/journal.pone.0210861.
Loureiro NSL, Amaral TLM, Amaral CA, Monteiro GTR, Vasconcellos MTL, Bortolini MJS. Relationship between anthropometric indicators and risk factors for cardiovascular disease in adults and older adults of Rio Branco, Acre. Rev Saude Publica. 2020;54:24. https://doi.org/10.11606/s1518-8787.2020054001088.
Del Pozo-Cruz J, Garcia-Hermoso A, Alfonso-Rosa RM, Alvarez-Barbosa F, Owen N, Chastin S, et al. Replacing sedentary time: meta-analysis of objective-assessment studies. Am J Prev Med. 2018;55(3):395–402. https://doi.org/10.1016/j.amepre.2018.04.042.
Carbone S, Del Buono MG, Ozemek C, Lavie CJ. Obesity, risk of diabetes and role of physical activity, exercise training and cardiorespiratory fitness. Prog Cardiovasc Dis. 2019;62(4):327–33. https://doi.org/10.1016/j.pcad.2019.08.004.
Silva ASE, Lacerda FV, da Mota MPG. Effect of strength training on plasma levels of Homocysteine in patients with type 2 diabetes. Int J Prev Med. 2019;10:80. https://doi.org/10.4103/ijpvm.IJPVM_313_17.
Silva ASLF, Mota MPG. Effect of aerobic training on homocysteine levels in type 2 diabetic individuals. Rev Bras Med Esporte. 2015;21(4):275–8. https://doi.org/10.1590/1517-869220152104140828.
Silva A, Lacerda FV, da Mota MPG. The effect of aerobic vs. resistance training on plasma homocysteine in individuals with type 2 diabetes. J Diabetes Metab Disord. 2020;19(2):1003–9. https://doi.org/10.1007/s40200-020-00596-z.
Acknowledgments
The authors would like to thank the volunteers, collaborators of the research, and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES) for the financial support through scholarships—Finance Code 001.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest associated with this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Oliveira, J.J., e Silva, A.d.S., Ribeiro, A.G.S.V. et al. The effect of physical activity on total homocysteine concentrations and cardiovascular risk in older Brazilian adults with type 2 diabetes. J Diabetes Metab Disord 20, 407–416 (2021). https://doi.org/10.1007/s40200-021-00759-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-021-00759-6