Abstract
Purpose of Review
Summarize sex-specific contributors to the genetic architecture of Alzheimer’s disease (AD).
Recent Findings
There are sex differences in the effects of apolipoprotein E (APOE), genes along the APOE pathway, and genes along the neurotrophic signaling pathway in predicting AD. Reported sex differences are largely driven by stronger associations among females. Evidence also suggests that genetic predictors of amyloidosis are largely shared across sexes, while sex-specific genetic effects emerge downstream of amyloidosis and drive the clinical manifestation of AD.
Summary
There is a lack of comprehensive assessments of sex differences in genome-wide analyses of AD and a need for more systematic reporting of sex-stratified genetic effects. The emerging emphasis on sex as a biological variable provides an opportunity for transdisciplinary collaborations aimed at addressing major analytical challenges that have hampered advancements in the field. Ultimately, sex-specific genetic association studies represent a logical first step towards precision medicine.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mazure CM, Swendsen J. Sex differences in Alzheimer’s disease and other dementias. Lancet Neurol. 2016;15(5):451–2.
Nebel RA, Aggarwal NT, Barnes LL, Gallagher A, Goldstein JM, Kantarci K, et al. Understanding the impact of sex and gender in Alzheimer’s disease: a call to action. Alzheimers Dement. 2018;14(9):1171–83.
Barnes LL, Wilson RS, Bienias JL, Schneider JA, Evans DA, Bennett DA. Sex differences in the clinical manifestations of Alzheimer disease pathology. Arch Gen Psychiatry. 2005;62(6):685–91.
Koran MI, Wagener MA, Hohman TJ. Sex differences in the association between AD biomarkers and cognitive decline. Brain Imaging and Behav. 2017;11(1):205–13.
• Oveisgharan S, Arvanitakis Z, Yu L, Farfel J, Schneider JA, Bennett DA. Sex differences in Alzheimer’s disease and common neuropathologies of aging. Acta Neuropathol. 2018;136(6):887–900 Analyzes and reports sex differences in the common neuropathologies of aging, highlighting more AD neuropathology and more servere arteriolosclerosis among females, and a higher likelihood of having gross infarcts among males.
Gamberger D, Lavrač N, Srivatsa S, Tanzi RE, Doraiswamy PMJ Sr. Identification of clusters of rapid and slow decliners among subjects at risk for Alzheimer’s disease. Sci Rep. 2017;7(1):6763.
Tifratene K, Robert P, Metelkina A, Pradier C, Dartigues JF. Progression of mild cognitive impairment to dementia due to AD in clinical settings. Neurology. 2015;85(4):331–8.
Lin KA, Choudhury KR, Rathakrishnan BG, et al. Marked gender differences in progression of mild cognitive impairment over 8 years. Alzheimer’s & Dement: Translational Research & Clinical Interventions. 2015;1(2):103–10.
Alzheimer’s Association. 2018 Alzheimer’s disease facts and figures. Alzheimers Dement. 2018;14(3):367–429.
Mielke MM, Ferretti MT, Iulita MF, Hayden K, Khachaturian AS. Sex and gender in Alzheimer’s disease – does it matter? Alzheimer’s & Dement: The Journal of the Alzheimer's Association. 2018;14(9):1101–3.
Ferretti MT, Iulita MF, Cavedo E, et al. Sex differences in Alzheimer disease—the gateway to precision medicine. Nat Rev Neurol. 2018;14:457–69.
Mielke MM, Vemuri P, Rocca WA. Clinical epidemiology of Alzheimer’s disease: assessing sex and gender differences. Clin Epidemiol. 2014;6:37–48.
Laws KR, Irvine K, Gale TM. Sex differences in Alzheimer’s disease. Curr Opin Psychiatry. 2018;31(2):133–9.
Farrer LA, Cupples LA, Haines JL, et al. Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. A meta-analysis. APOE and Alzheimer Disease Meta Analysis Consortium. JAMA. 1997;278(16):1349–56.
Fukumoto N, Fujii T, Combarros O, et al. Sexually dimorphic effect of the Val66Met polymorphism of BDNF on susceptibility to Alzheimer’s disease: new data and meta-analysis. Am J Med Genet B Neuropsychiatr Genet. 2010;153b(1):235–42.
• Hohman TJ, Dumitrescu L, Barnes LL, et al. Sex-specific effects of apolipoprotein E with cerebrospinal fluid levels of tau. JAMA Neurol. 2018;75(8):989–98 Large meta-anlaysis demonstrating a stronger association between APOE and CSF tau levels among females compared to males.
•• Neu SC, Pa J, Kukull W, et al. Apolipoprotein E genotype and sex risk factors for Alzheimer disease: a meta-analysis. JAMA Neurol. 2017;74(10):1178–89 Large meta-analysis demonstrating a stronger association between APOE (both ε2 and ε4) and clinical AD among females compared to males, particularly between the ages of 55–70.
Riedel BC, Thompson PM, Brinton RD. Age, APOE and sex: triad of risk of Alzheimer’s disease. J Steroid Biochem Mol Biol. 2016;160:134–47.
Gottesman RF, Schneider AL, Zhou Y, et al. The ARIC-PET amyloid imaging study: brain amyloid differences by age, race, sex, and APOE. Neurology. 2016;87(5):473–80.
Reiman EM, Chen K, Liu X, Bandy D, Yu M, Lee W, et al. Fibrillar amyloid-beta burden in cognitively normal people at 3 levels of genetic risk for Alzheimer’s disease. Proc Natl Acad Sci U S A. 2009;106(16):6820–5.
Farfel JM, Yu L, De Jager PL, Schneider JA, Bennett DA. Association of APOE with tau-tangle pathology with and without β-amyloid. Neurobiol Aging. 2016;37:19–25.
Jagust WJ, Landau SM. Apolipoprotein E, not fibrillar beta-amyloid, reduces cerebral glucose metabolism in normal aging. J Neurosci. 2012;32(50):18227–33.
Ossenkoppele R, van der Flier WM, Zwan MD, Adriaanse SF, Boellaard R, Windhorst AD, et al. Differential effect of APOE genotype on amyloid load and glucose metabolism in AD dementia. Neurology. 2013;80(4):359–65.
• Shi Y, Yamada K, Liddelow SA, et al. ApoE4 markedly exacerbates tau-mediated neurodegeneration in a mouse model of tauopathy. Nature. 2017;549(7673):523–7 Demonstrates role of APOE in driving tau-related neurodegeneration downstream of amyloidosis.
Osenkowski P, Ye W, Wang R, Wolfe MS, Selkoe DJ. Direct and potent regulation of γ-secretase by its lipid microenvironment. J Biol Chem. 2008;283(33):22529–40.
Castellano JM, Kim J, Stewart FR, et al. Human apoE isoforms differentially regulate brain amyloid-beta peptide clearance. Sci Transl Med. 2011;3(89):89ra57.
Damoiseaux JS, Seeley WW, Zhou J, Shirer WR, Coppola G, Karydas A, et al. Gender modulates the APOE ε4 effect in healthy older adults: convergent evidence from functional brain connectivity and spinal fluid tau levels. J Neurosci. 2012;32(24):8254–62.
Jack CR, Wiste HJ, Weigand SD, et al. Age, sex, and APOE ε4 effects on memory, brain structure, and β-amyloid across the adult life span. JAMA Neurol. 2015;72(5):511–9.
• Jack CR, Wiste HJ, Weigand SD, et al. Age-specific and sex-specific prevalence of cerebral β-amyloidosis, tauopathy, and neurodegeneration in cognitively unimpaired individuals aged 50–95 years: a cross-sectional study. Lancet Neurol. 2017;16(6):435–44 Provides data on the prevalence of AD related brain changes in the absence of clinical disease.
Altmann A, Tian L, Henderson VW, Greicius MD. Sex modifies the APOE-related risk of developing Alzheimer disease. Ann Neurol. 2014;75(4):563–73.
Buckley RF, Mormino EC, Amariglio RE, Properzi MJ, Rabin JS, Lim YY, et al. Sex, amyloid, and APOE ε4 and risk of cognitive decline in preclinical Alzheimer’s disease: findings from three well-characterized cohorts. Alzheimers Dement. 2018;14:1193–203.
Sampedro F, Vilaplana E, de Leon MJ, Alcolea D, Pegueroles J, Montal V, et al. APOE-by-sex interactions on brain structure and metabolism in healthy elderly controls. Oncotarget. 2015;6(29):26663–74.
Cavedo E, Chiesa PA, Houot M, Ferretti MT, Grothe MJ, Teipel SJ, et al. Sex differences in functional and molecular neuroimaging biomarkers of Alzheimer’s disease in cognitively normal older adults with subjective memory complaints. Alzheimers Dement. 2018;14(9):1204–15.
Sundermann EE, Tran M, Maki PM, et al. Sex differences in the association between apolipoprotein E ε4 allele and Alzheimer’s disease markers. Alzheimers Dement (Amst). 2018;10:438–47.
Kim J, Fischer CE, Schweizer TA, Munoz DG. Gender and pathology-specific effect of apolipoprotein E genotype on psychosis in Alzheimer’s disease. Curr Alzheimer Res. 2017;14(8):834–40.
Xing Y, Qin W, Li F, Jia X-F, Jia JJD. disorders gcApolipoprotein E ε4 status modifies the effects of sex hormones on neuropsychiatric symptoms of Alzheimer’s disease. Dement Geriatr Cogn Disord. 2012;33(1):35–42.
Cacciottolo M, Christensen A, Moser A, et al. The APOE4 allele shows opposite sex bias in microbleeds and Alzheimer’s disease of humans and mice. Neurobiol Aging. 2016;37(Supplement C):47–57.
Shinohara M, Murray ME, Frank RD, et al. Impact of sex and APOE4 on cerebral amyloid angiopathy in Alzheimer’s disease. Acta Neuropathol. 2016;132(2):225–34.
Liang Y, Li H, Lv C, Shu N, Chen K, Li X, et al. Sex moderates the effects of the Sorl1 gene rs2070045 polymorphism on cognitive impairment and disruption of the cingulum integrity in healthy elderly. Neuropsychopharmacology. 2015;40(6):1519–27.
Wahrle SE, Jiang H, Parsadanian M, Legleiter J, Han X, Fryer JD, et al. ABCA1 is required for normal central nervous system ApoE levels and for lipidation of astrocyte-secreted apoE. J Biol Chem. 2004;279(39):40987–93.
Davies G, Harris SE, Reynolds CA, Payton A, Knight HM, Liewald DC, et al. A genome-wide association study implicates the APOE locus in nonpathological cognitive ageing. Mol Psychiatry. 2014;19(1):76–87.
Smillie KJ, Pawson J, Perkins EM, Jackson M, Cousin MA. Control of synaptic vesicle endocytosis by an extracellular signalling molecule. Nat Commun. 2013;4:2394.
Lucas JJ, Hernandez F, Gomez-Ramos P, Moran MA, Hen R, Avila J. Decreased nuclear beta-catenin, tau hyperphosphorylation and neurodegeneration in GSK-3beta conditional transgenic mice. EMBO J. 2001;20(1–2):27–39.
Sen A, Nelson TJ, Alkon DL. ApoE isoforms differentially regulates cleavage and secretion of BDNF. Mol Brain. 2017;10(1):19–9.
Baker M, Mackenzie IR, Pickering-Brown SM, Gass J, Rademakers R, Lindholm C, et al. Mutations in progranulin cause tau-negative frontotemporal dementia linked to chromosome 17. Nature. 2006;442(7105):916–9.
• Curtis AF, Masellis M, Hsiung GR, et al. Sex differences in the prevalence of genetic mutations in FTD and ALS: a meta-analysis. Neurology. 2017;89(15):1633–42 Reports a higher prevalence of C9orf72 and GRN disease causing mutations among females compared to males.
Olgiati P, Politis A, Albani D, Rodilossi S, Polito L, Zisaki A, et al. Effects of SORL1 gene on Alzheimer’s disease. Focus on gender, neuropsychiatric symptoms and pro-inflammatory cytokines. Curr Alzheimer Res. 2013;10(2):154–64.
Sundar PD, Feingold E, Minster RL, DeKosky ST, Kamboh MI. Gender-specific association of ATP-binding cassette transporter 1 (ABCA1) polymorphisms with the risk of late-onset Alzheimer’s disease. Neurobiol Aging. 2007;28(6):856–62.
Gallart-Palau X, Lee BS, Adav SS, et al. Gender differences in white matter pathology and mitochondrial dysfunction in Alzheimer’s disease with cerebrovascular disease. Mol Brain. 2016;9:27.
Grimm A, Mensah-Nyagan AG, Eckert A. Alzheimer, mitochondria and gender. Neurosci Biobehav Rev. 2016;67:89–101.
Chen J, Liang X, Li B, Jiang X, Xu Z. Gender-related association of brain-derived neurotrophic factor gene 196A/G polymorphism with Alzheimer’s disease--a meta-analysis including 6854 cases and 6868 controls. Int J Neurosc. 2014;124(10):724–33.
Li GD, Bi R, Zhang DF, et al. Female-specific effect of the BDNF gene on Alzheimer’s disease. Neurobiol Aging. 2017;53:192.e111–9.
Laing KR, Mitchell D, Wersching H, Czira ME, Berger K, Baune BT. Brain-derived neurotrophic factor (BDNF) gene: a gender-specific role in cognitive function during normal cognitive aging of the MEMO-Study? Age (Dordr). 2012;34(4):1011–22.
Seripa D, Matera MG, Franceschi M, Daniele A, Bizzarro A, Rinaldi M, et al. The RELN locus in Alzheimer’s disease. Journal of Alzheimer’s disease : JAD. 2008;14(3):335–44.
Ringstedt T, Linnarsson S, Wagner J, et al. BDNF regulates reelin expression and Cajal-Retzius cell development in the cerebral cortex. Neuron. 1998;21(2):305–15.
Counts SE, Che S, Ginsberg SD, Mufson EJ. Gender differences in neurotrophin and glutamate receptor expression in cholinergic nucleus basalis neurons during the progression of Alzheimer’s disease. J Chem Neuroanat. 2011;42(2):111–7.
Lane RM, He Y. Butyrylcholinesterase genotype and gender influence Alzheimer’s disease phenotype. Alzheimers Dement. 2013;9(2):e1–73.
Green PS, Gridley KE, de Fiebre NC. Role of estrogen replacement therapy in memory enhancement and the prevention of neuronal loss associated with Alzheimer’s disease. Am J Med. 1997;103(3):19S–25S.
Aguirre CC, Baudry M. Progesterone reverses 17β-estradiol-mediated neuroprotection and BDNF induction in cultured hippocampal slices. Eur J Neurosci. 2009;29(3):447–54.
Zhao L, Woody SK, Chhibber AJ. Estrogen receptor β in Alzheimer’s disease: from mechanisms to therapeutics. Ageing Res Rev. 2015;24:178–90.
Engel T, Goni-Oliver P, Lucas JJ, Avila J, Hernandez F. Chronic lithium administration to FTDP-17 tau and GSK-3beta overexpressing mice prevents tau hyperphosphorylation and neurofibrillary tangle formation, but pre-formed neurofibrillary tangles do not revert. J Neurochem. 2006;99(6):1445–55.
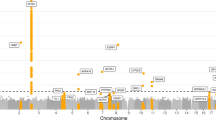
•• Deming Y, Dumitrescu L, Barnes LL, et al. Sex-specific genetic predictors of Alzheimer’s disease biomarkers. Acta Neuropathol. 2018;136:1–16 Performs sex-interaction and sex-stratified genome-wide analyses and demonstrates female-specific genetic associations with CSF Aβ-42 and CSF total tau.
Deming Y, Li Z, Kapoor M, et al. Genome-wide association study identifies four novel loci associated with Alzheimer’s endophenotypes and disease modifiers. Acta Neuropathol. 2017;133(5):839–56.
Martinez-Mir A, Gonzalez-Perez A, Gayan J, et al. Genetic study of neurexin and neuroligin genes in Alzheimer’s disease. J Alzheimer's Dis : JAD. 2013;35(2):403–12.
Viswanathan J, Makinen P, Helisalmi S, Haapasalo A, Soininen H, Hiltunen M. An association study between granulin gene polymorphisms and Alzheimer's disease in Finnish population. Am J Med Gen Part B Neuropsychiatric Gen : the official publication of the International Society of Psychiatric Genetics. 2009;150b(5):747–50.
Suzuki M, Lee H-C, Kayasuga Y, et al. Roles of progranulin in sexual differentiation of the developing brain and adult neurogenesis. J Reprod Dev. 2009;55(4):351–5.
Suzuki M, Nishiahara M. Granulin precursor gene: a sex steroid-inducible gene involved in sexual differentiation of the rat brain. Mol Genet Metab. 2002;75(1):31–7.
Piccio L, Deming Y, Del-Aguila JL, et al. Cerebrospinal fluid soluble TREM2 is higher in Alzheimer disease and associated with mutation status. Acta Neuropathol. 2016;131(6):925–33.
Aberg D, Johansson P, Isgaard J, et al. Increased cerebrospinal fluid level of insulin-like growth factor-II in male patients with Alzheimer’s disease. J Alzheimer’s Dis : JAD. 2015;48(3):637–46.
Puertas Mdel C, Martinez-Martos JM, Cobo M, et al. Plasma renin-angiotensin system-regulating aminopeptidase activities are modified in early stage Alzheimer’s disease and show gender differences but are not related to apolipoprotein E genotype. Exp Gerontol. 2013;48(6):557–64.
Arias E, Heron M, Xu J. United States life tables, 2013. National Vital Statistics Reports. 2017;66(3):1–64.
Mayeda ER, Tchetgen EJT, Power MC, et al. A simulation platform for quantifying survival bias: an application to research on determinants of cognitive decline. Am J Epidemiol. 2016;184(5):378–87.
Hernan MA, Hernandez-Diaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15(5):615–25.
Rosvall L, Rizzuto D, Wang H-X, Winblad B, Graff C, Fratiglioni L. APOE-related mortality: effect of dementia, cardiovascular disease and gender. Neurobiol Aging. 2009;30(10):1545–51.
Hayden KM, Zandi PP, Lyketsos CG, Tschanz JAT, Norton MC, Khachaturian AS, et al. Apolipoprotein E genotype and mortality: findings from the Cache County Study. J Am Geriatr Soc. 2005;53(6):935–42.
Ewbank DC. Mortality differences by APOE genotype estimated from demographic synthesis. Genet Epidemiol. 2002;22(2):146–55.
Lahoz C, Schaefer EJ, Cupples LA, Wilson PWF, Levy D, Osgood D, et al. Apolipoprotein E genotype and cardiovascular disease in the Framingham Heart Study. Atherosclerosis. 2001;154(3):529–37.
Foverskov E, Glymour MM, Mortensen EL, Holm A, Lange T, Lund R. Education and cognitive aging: accounting for selection and confounding in linkage of data from the Danish registry and survey of health, ageing and retirement in Europe. Am J Epidemiol. 2018;187(11):2423–30.
Yang P, Sun Y-M, Liu Z-J, et al. Association study of ABCA7 and NPC1 polymorphisms with Alzheimer’s disease in Chinese Han ethnic population. Psychiatr Genet. 2013;23(6):268.
Reitz C, Mayeux R. Genetics of Alzheimer’s disease in Caribbean Hispanic and African American populations. Biol Psychiatry. 2014;75(7):534–41.
Reitz C, Jun G, Naj A. Variants in the atp-binding cassette transporter (abca7), apolipoprotein e-4, and the risk of late-onset alzheimer disease in african americans. JAMA. 2013;309(14):1483–92.
Lee JH, Cheng R, Barral S, Reitz C, Medrano M, Lantigua R, et al. Identification of novel loci for Alzheimer disease and replication of CLU, PICALM, and BIN1 in Caribbean Hispanic individuals. Arch Neurol. 2011;68(3):320–8.
Jun GR, Chung J, Mez J, Barber R, Beecham GW, Bennett DA, et al. Transethnic genome-wide scan identifies novel Alzheimer’s disease loci. Alzheimers Dement. 2017;13(7):727–38.
Gotwals P, Cameron S, Cipolletta D, Cremasco V, Crystal A, Hewes B, et al. Prospects for combining targeted and conventional cancer therapy with immunotherapy. Nat Rev Cancer. 2017;17(5):286–301.
Reitz C. Toward precision medicine in Alzheimer’s disease. Ann Transl Med. 2016;4(6):107.
Haywood WM, Mukaetova-Ladinska EB. Sex influences on cholinesterase inhibitor treatment in elderly individuals with Alzheimer’s disease. Am J Geriatr Pharmacother. 2006;4(3):273–86.
Claxton A, Baker LD, Wilkinson CW, Trittschuh EH, Chapman D, Watson GS, et al. Sex and ApoE genotype differences in treatment response to two doses of intranasal insulin in adults with mild cognitive impairment or Alzheimer’s disease. J Alzheimer’s Dis : JAD. 2013;35(4):789–97.
Canevelli M, Quarata F, Remiddi F, Lucchini F, Lacorte E, Vanacore N, et al. Sex and gender differences in the treatment of Alzheimer’s disease: a systematic review of randomized controlled trials. Pharmacol Res. 2017;115:218–23.
Torkamani A, Wineinger NE, Topol EJ. The personal and clinical utility of polygenic risk scores. Nat Rev Genet. 2018;19(9):581–90.
Mormino EC, Sperling RA, Holmes AJ, Buckner RL, de Jager PL, Smoller JW, et al. Polygenic risk of Alzheimer disease is associated with early- and late-life processes. Neurology. 2016;87(5):481–8.
Ge T, Sabuncu MR, Smoller JW, Sperling RA, Mormino EC. Dissociable influences of APOE epsilon4 and polygenic risk of AD dementia on amyloid and cognition. Neurology. 2018;90(18):e1605–12.
Stocker H, Möllers T, Perna L, Brenner H. The genetic risk of Alzheimer’s disease beyond APOE ε4: systematic review of Alzheimer’s genetic risk scores. Transl Psychiatry. 2018;8(1):166.
Tan CH, Fan CC, Mormino EC, et al. Polygenic hazard score: an enrichment marker for Alzheimer’s associated amyloid and tau deposition. Acta Neuropathol. 2018;135(1):85–93.
Tan CH, Hyman BT, Tan JJX, Hess CP, Dillon WP, Schellenberg GD, et al. Polygenic hazard scores in preclinical Alzheimer disease. Ann Neurol. 2017;82(3):484–8.
Desikan RS, Fan CC, Wang Y, Schork AJ, Cabral HJ, Cupples LA, et al. Genetic assessment of age-associated Alzheimer disease risk: development and validation of a polygenic hazard score. PLoS Med. 2017;14(3):e1002258.
Acknowledgements
This research was supported in part by R01 AG059716 (TJH), K01 AG049164 (TJH), R21 AG05994 (TJH), K12 HD043483 (TJH), HHSN311201600276P (TJH), R00 AG053410 (ERM), and the Vanderbilt Memory & Alzheimer’s Center. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Logan Dumitrescu, Kavya Sharman, Annah M. Moore, and Timothy J. Hohman each report an NIH grant. Elizabeth Rose Mayeda reports a grant from the NIA.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurogenetics and Psychiatric Genetics
Rights and permissions
About this article
Cite this article
Dumitrescu, L., Mayeda, E.R., Sharman, K. et al. Sex Differences in the Genetic Architecture of Alzheimer’s Disease. Curr Genet Med Rep 7, 13–21 (2019). https://doi.org/10.1007/s40142-019-0157-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40142-019-0157-1