Abstract
Purpose of Review
Patellofemoral syndrome (PFS) is a common condition seen in people with anterior knee pain. This review explores patient presentations and exam maneuvers used for diagnosis, as well as established/up-and-coming treatment interventions.
Recent Findings
Pain reduction and prevention are the main goals for PFS as they negatively affect quality of life. Combination hip and knee exercises have been found to be most beneficial during therapy due to the multifactorial etiology of PFS. Combining exercise therapy with patellar taping has also shown a reduction in acute pain. Ultrasound may be used to evaluate for associated findings. Blood flow restriction and trigger point injections are options that may be helpful for pain reduction but further research is required.
Summary
PFS is a common clinical diagnosis requiring a robust patient history, supported by various physical exam maneuvers. Treatment involves a patient tailored approach, often with combinations of conservative management and interventional procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patellofemoral syndrome (PFS), commonly known as “runner’s knee,” is a term used to describe pain around or under the patella and is one of the most common conditions causing knee pain [1,2,3]. Common patient presentation includes generalized anterior knee pain caused by activities that stress the patellofemoral joint [1, 2, 4]. Currently, there is no consensus on the etiology of patellofemoral pain syndrome. Multiple factors are thought to be involved, including trauma, overuse, patellar malalignment, and muscular imbalance [1, 3,4,5,6,7]. There have also been a limited number of studies showing that psychological factors such as mental health, fear, anxiety, and depression may contribute to pain in PFS [2, 6, 8, 9]. The condition has been shown to affect young, physically active individuals compared to other groups [5, 9, 10]. There is also a higher prevalence in women compared to men [3, 5, 4,5,6,7,8, 10, 11].
Diagnosis
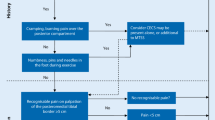
History
Patient history is crucial in the diagnosis of PFS, as it is a clinical one [3]. Patients will generally present reporting anterior knee pain localized around or behind the patella; however, many people will have difficulty in localizing pain [1, 3, 4, 8]. A key point will be worsening pain after running, kneeling, squatting, or prolonged sitting with flexed knees (movie theatre sign) [1, 3, 4, 7•, 8, 9, 12]. Patients may describe the pain as an achy sensation, but characterization of pain can greatly vary and should not be used for diagnosis [4]. Small effusions are possible but uncommon, and any large effusions should elicit investigation into alternative diagnoses [4, 12]. Other diagnoses should be excluded, such as patellofemoral arthritis, prepatellar bursitis, quadriceps tendinopathy, plica syndrome, Osgood Schlatter Disease, and referred pain from the ipsilateral hip [3, 8].
Physical Examination
Inspection of the knee is the first step, as in any musculoskeletal condition. Clinicians should assess for muscular atrophy, effusion, erythema, deformities, foot hyperpronation, pelvic tilt, gait abnormalities, quadriceps/hamstring flexibility, and asymmetry of bilateral lower extremities [7•]. Patellar alignment should be carefully observed and evaluate for any patella alta/baja, trochlear dysplasia, femoral anteversion, genu valgus, and laterally displaced tibial tuberosity as these can predispose to PFS [4, 7•]. Palpation may elicit pain to the retropatellar or peripatellar region. Patient should also be evaluated for crepitus, effusions, or contractures [3, 8, 12]. An ipsilateral hip examination should always be performed to rule out hip pathology with referred pain to the knee [3, 4, 8, 10].
Physical examination maneuvers for PFS are numerous, but a recent meta-analysis of several tests for PFS showed no diagnostic consistency, which further emphasizes significance of obtaining a comprehensive patient history [3, 5, 7•8]. Some exam maneuvers that can be performed include Q angle measurements, J sign, patellar glide, patellar tilt test, patellar grind/Clarke’s test, Ely’s test, and double/single leg squats [8, 12]. Patients should also be asked to perform any activities that reproduce symptoms during the examination.
Q angle measurement is obtained by measuring the angle between a line connecting the anterosuperior iliac spine to center of patella as it intersects with a line from the center of patella to the middle of the anterior tibial tuberosity. Some literature noted that > 16 degrees is a risk factor for PFS; however, it is not a consistent finding [4, 6, 13].
J sign is used to evaluate for dynamic patellar tracking. Patients are seated with knees flexed to 90 degrees and then asked to extend the knee into full extension. A normal examination will have the patellar path tracking straight anteriorly, and may have slight lateral deviation. Patellar mal-tracking will show sudden lateral deviation of the patella with terminal extension due to the patellar subluxation out of the trochlear groove in an inverted J sign pattern [4].
Patellar glide test is an assessment of medial/lateral mobility of the patella. With the knee flexed to 30 degrees, the patella is divided into 4 quadrants and displaced either medially or laterally. Displacement of 3 or more quadrants in either direction is indicative of a hypermobile patella which has a correlation with the incidence of patellofemoral pain [4, 6, 8].
The patellar tilt test compares the tilt in the anterior aspects of the medial/lateral patella and is used to assess for tightness in lateral knee structures. The patella is passively displaced laterally and then observed. If the lateral patella edge tilts inferiorly, this is indicative of a tight lateral retinaculum [4, 6, 7•, 8].
The patellar grind and Clarke’s test are used to mechanically evaluate anterior knee pain. In the patellar grind test, the patient’s knee is extended and posteriorly directed pressure is applied to the patella. For Clarke’s test, a posterior and inferior force is applied to the superior aspect of the patella, while the patient actively contracts the quadriceps. Reproduction of pain with these maneuvers is considered positive and indicative of patellofemoral pain [14].
Ely’s test is done to evaluate for rectus femoris tightness, which can contribute to patellofemoral pain. The patient is placed prone, and the examiner stands to the side. The patient’s ankle is held, and the knee is passively flexed, while the other hand stabilizes the pelvis. The test is positive if the ipsilateral hip has compensatory flexion, elevating the anterior hip off the surface [15].
Pain while performing double leg squats has been shown to be the most sensitive physical exam finding for PFS and should always be used as functional diagnostic test during evaluation [5, 7, 8, 12]. Single leg squats can also be performed to evaluate for weak hip abductors and external rotator muscles observed by any pelvic drop, trunk rotation, or loss of hip control. Weakness in these muscles is thought to contribute to PFS due to excessive leg adduction and femoral internal rotation with functional tasks [4].
Imaging
Musculoskeletal ultrasound may be useful to evaluate for associated findings in PFS. These include the following: intraarticular effusion, quadriceps tendon thickness ≥ 0.54 cm, patellar tendon thickness ≥ 0.35 cm, gluteus medius thickness asymmetry during contraction, and a smaller vastus medialis volume, insertion level, and fiber angle [16•]. Radiographic imaging is not usually performed for initial diagnosis of PFS unless there is a history of trauma or dislocation [4]. Radiographic findings do not correlate well to patient symptoms and there are no specific findings associated with PFS. Plain film X-rays may be performed after several weeks of conservative treatment with no improvement to look for other causes of pain such as osteoarthritis, fracture, osteochondritis, or bipartite patella [3, 4, 7•]. CT and MRI are not used for diagnosing PFS, but may evaluate for other causes of pain [3, 7•, 13].
Treatment
As PFS is the most common cause of anterior knee pain in adults, treating patients effectively is of utmost importance. There has been abundant research showing that PFS significantly affects one’s quality of life, as patients often forego recreational activities so as not to experience pain. A recent systematic review showed that the negative effect on quality of life on people with PFS is nearly that of osteoarthritis [17•]. Additionally, the findings indicate that in comparison to athletes without PFS, those athletes with PFS experience a negative effect on quality of life [17•]. The mainstay of treatment for PFS is conservative management. In the acute setting, which may last several weeks, pain management is best achieved with relative rest, ice, and NSAIDs [7•]. Once pain is controlled adequately, the focus of treatment is on preventing further exacerbations by targeting strengthening of the hip and knee muscles and improving patellar tracking. There are a variety of treatment options for those suffering from PFS. The goals of treatment are to reduce pain and inflammation, aid in improved patellar tracking, strengthen the muscles of the hip and knee, and educate the patient on activity modification.
Exercise Therapy
It is known that a physical therapy program is one of the best treatment approaches to PFS. Most of the evidence points to the importance of strengthening the muscles of the hip and knee. A recent international consensus statement from experts in the field of patellofemoral pain emphasizes the recommendation of an exercise program targeting strength of the hip and knee muscles [18••]. The proposed mechanism is that strengthening these muscles improves patellar tracking [19]. Strengthening the hip abductors and external rotators has also been a cornerstone of treatment in PFS, since weakness of these muscles has been found in patients with PFS [19]. Examples of exercises that are often recommended include one- and two-legged squats, single-leg lunges [20], wall sits or wall slides, straight-leg raises while supine, and side-lying hip abduction [21]. Stretching and soft tissue mobilization of the iliotibial band are also used as an adjunctive approach to treatment, as patients with PFS are reported to have tight and thicker iliotibial bands than the general population [19].
Taping and Bracing
Other modalities used to treat PFS include taping and bracing. There are multiple reported purposes of taping: to medially direct the patella to prevent lateral patellar tracking, to aid in proprioception, to improve blood flow, and to provide stretching to the muscles involved. The purpose of bracing is to help improve the biomechanics of the knee that may be altered in patients with PFS, namely, patellar tilt and lateral tracking. Though there have been some conflicting reports in the literature, it is widely accepted that the adjunct of taping in the acute setting may be of some benefit in treating PFS. The review by Barton et al. found evidence that medially-directed patellar taping reduced pain in the acute setting, as did bracing to prevent lateral tracking of the patella [22]. Additionally, a recent review by Sisk et al. concluded that the use of taping especially when combined with an exercise program improved pain in the acute setting [23]. This review also found that bracing, and specifically the patellar-stabilizing brace over the patellar sleeve, improved pain, and function in the short term (< 52 weeks) in patients with PFS [23].
Foot Orthoses
The purpose of using foot orthoses in patients with PFS is to correct over-pronating of the foot and aiding in improving excessive internal rotation of the affected lower extremity [24]. The literature supports that providers may use foot orthoses as an adjunct to an exercise program in the treatment of PFS especially for improving pain in the short term (less than 6 weeks) [25]. Additionally, at this time, there is not a recommendation to provide custom foot orthoses over prefabricated foot orthoses [25].
Injections
Evidence pointing to the improvement in pain and function in patients with PFS who undergo injections is lacking in the literature, despite injections being a cornerstone of treatment for many musculoskeletal conditions. While plausible that steroid injections may promote homeostasis of the knee joint after trauma, it is unclear to be of any benefit in PFS based on the literature [23]. Botulinum toxin injection to the vastus lateralis has also been studied for the treatment of PFS, though large studies still need to be done. The proposed mechanism behind targeting the vastus lateralis is to improve patellar tracking by balancing the medial and lateral forces on the patella [23]. A recent retrospective review analyzed improvement in pain and function to patients with PFS who underwent a single session of Botox injection to the vastus lateralis followed by physical therapy and found that there was improvement in both pain and function at follow-up and many of these patients did not require planned surgical intervention for PFS at the time of the last follow-up [26].
Other Treatments
There is limited data regarding the use of acupuncture in treatment of PFS [22]. More studies are needed to evaluate the benefit of using acupuncture, although some studies suggest there can be some mitigation of pain [23]. Manual soft tissue techniques (specifically myofascial techniques and ischemic release at the peripatellar or hip regions) are uncertain to be of any benefit in improving pain or function in patients with PFS [18••]. Another area of research that has been of growing interest lately is blood flow restriction training. This technique utilizes a pneumatic cuff placed proximal to the intended target of strength training to restrict blood flow, thereby creating muscle hypertrophy at lower loads of strengthening exercises [27]. One randomized control trial done in 2017 analyzed reduction in pain in those with PFS undergoing blood flow restriction to the quadriceps muscle (performing leg press and leg extension exercises at 30% of their one-repetition maximum) to a control group performing the same exercises but at 70% of their one-repetition maximum found that there was improvement in pain at 8 weeks [27]. Unfortunately, the data is lacking regarding this form of treatment for patients with PFS, and more studies are needed. Trigger point dry needling has also been studied for its effectiveness in treating PFS. A recent randomized, single-blind, parallel-group trial randomized participants to receive dry needling to the vastus medialis, vastus lateralis, and rectus femoris muscles or to receive placebo needling once a week for 6 weeks. Thereafter, they were instructed to stretch the quadriceps muscle. The authors found that the group treated with trigger point dry needling had improved pain compared to the placebo group [28]. Another recent systematic review and meta-analysis analyzed six studies regarding the effect of trigger point dry needling on PFS and found low to moderate evidence of improvement in pain for patients with PFS who were treated with trigger point dry needling [29]. The uses of electrophysical agents such as ultrasound, cryotherapy, and electrical stimulation are currently not recommended in the treatment of PFS [25].
Surgery
A referral to an Orthopedic Surgeon should be a last resort for a patient suffering from PFS. Surgery may be a last resort if the patient fails conservative treatment, which many experts would advise trying for at least 24 months. Surgery, if needed to be performed, may involve removing damaged articular cartilage of the patella and performing a lateral retinacular release so as to allow optimized tracking of the patella in the trochlear groove. A randomized control trial in 2012 compared one group undergoing knee arthroscopy and home exercise program with a group undergoing a home exercise program alone and found that those who were treated with knee arthroscopy and home exercise program did not have superior improvement in pain and function compared to the group treated with home exercise program alone [30].
Conclusion
Treatment for PFS should be individualized to the needs of the patient, based on the history and physical exam. The causes of PFS are thought to be multifactorial, and thus a tailored approach to treatment is warranted, often combining treatment modalities. The literature supports an exercise program specifically focusing on the hip and knee as the mainstay of treatment for PFS. Combining exercise with other treatment modalities including taping and bracing and use of foot orthoses has also been shown to be of benefit in improving pain especially in the short term. Other treatment modalities such as acupuncture, steroid injections, manual soft tissue techniques, and blood flow restriction training require more high-quality research studies before a clear recommendation can be made in regard to using them as adjuncts to treatment.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fredericson M, Powers CM. Practical management of patellofemoral pain. Clin J Sport Med. 2002;12(1):36–8. https://doi.org/10.1097/00042752-200201000-00010.
Maclachlan LR, Collins NJ, Matthews ML, Hodges PW, Vicenzino B. The psychological features of patellofemoral pain: a systematic review. Br. J. Sports Med. 2017;51(9):732–42. https://doi.org/10.1136/bjsports-2016-096705.
Bump JM, Lewis L. Patellofemoral syndrome [Updated 2022 Feb 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557657/
Collado H, Fredericson M. Patellofemoral pain syndrome. Clin Sports Med. 2010;29(3):379–98. https://doi.org/10.1016/j.csm.2010.03.012.
Nunes GS, Stapait EL, Kirsten MH, de Noronha M, Santos GM. Clinical test for diagnosis of patellofemoral pain syndrome: systematic review with meta-analysis. Phys. Ther. Sport. 2012;14(1):54–9. https://doi.org/10.1016/j.ptsp.2012.11.003.
Petersen W, Ellermann A, Gösele-Koppenburg A, et al. Patellofemoral pain syndrome. Knee Surg Sports Traumatol Arthrosc. 2013;22(10):2264–74. https://doi.org/10.1007/s00167-013-2759-6.
Gaitonde DY, Ericksen A, Robbins RC. Patellofemoral pain syndrome. Am Fam Physician. 2019;99(2):88–94. This article describes the epidemiology, clinical presentation, diagnosis and treatment of PFS. It provides evidence ratings for different clinical recommendations in the treatment of PFS.
Willy RW, Hoglund LT, Barton CJ, et al. Patellofemoral pain. J Orthop Sports Phys Ther. 2019;49(9):CPG1–CPG95. https://doi.org/10.2519/jospt.2019.0302 This is a clinical practice guideline reviewing up to date knowledge regarding the diagnosis, classification, examinations, and treatments regarding PFS.
Jensen R. Knee function and pain related to psychological variables in patients with long-term patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2005;35(9):594–600. https://doi.org/10.2519/jospt.2005.2119.
Powers CM, Bolgla LA, Callaghan MJ, Collins N, Sheehan FT. Patellofemoral pain; proximal, distal, and local factors. 2nd International Research Retreat. J Orthop Sports Phys Ther. 2012;42(6):A1–54. https://doi.org/10.2519/jospt.2012.0301.
Rathleff MS, Roos EM, Olesen JL, Rasmussen S, Arendt-Nielsen L. Lower mechanical pressure pain thresholds in female adolescents with patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2013;43(6):414–21. https://doi.org/10.2519/jospt.2013.4383.
Crossley KM, Stefanik JJ, Selfe J, et al. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 1: Terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measures. Br. J. Sports Med. 2016;50(14):839–43. https://doi.org/10.1136/bjsports-2016-096384.
Gulati A, McElrath C, Wadhwa V, Shah JP, Chhabra A. Current clinical, radiological and treatment perspectives of patellofemoral pain syndrome. Brit. J. Radiol. 2018;91(1086):20170456-20170456. https://doi.org/10.1259/bjr.20170456.
Fredericson M, Yoon K. Physical examination and patellofemoral pain syndrome. Am J Phys Med Rehabil. 2006;85(3):234–43. https://doi.org/10.1097/01.phm.0000200390.67408.f0.
Peeler J, Anderson JE. Reliability of the Ely’s test for assessing rectus femoris muscle flexibility and joint range of motion. J. Orthop. 2008;26(6):793–9. https://doi.org/10.1002/jor.20556.
Kasitinon D, Li WX, Wang EX, Fredericson M (2021). Physical examination and patellofemoral pain syndrome: an updated review. Curr. Rev. Musculoskelet. Med, 14(6), 406–412. https://doi.org/10.1007/s12178-021-09730-7. This is a review article describing how musculoskeletal ultrasound continues to gain importance as a diagnostic tool for patellofemoral syndrome.
Coburn SL, Barton CJ, Filbay SR, Hart HF, Rathleff MS, Crossley KM. Quality of life in individuals with patellofemoral pain: a systematic review including meta-analysis. Phys. Ther. Sport.. 2018;33:96-108. https://doi.org/10.1016/j.ptsp.2018.06.006. This is a systematic review looking at five databases describing quality of life in patients with PFS. The authors found that patients under the age of 50 years with PFS had worse quality of life scores compared with pain-free controls.
Collins NJ, Barton CJ, van Middelkoop M, et al. 2018 Consensus statement on exercise therapy and physical interventions (orthoses, taping and manual therapy) to treat patellofemoral pain: recommendations from the 5th International Patellofemoral Pain Research Retreat, Gold Coast, Australia, 2017. Br. J. Sports Med. 2018;52(18):1170-1178. https://doi.org/10.1136/bjsports-2018-099397. This is a consensus statement written by an international group of experts on PFS in 2018 and gives key recommendations based on expert panel voting after they undertook an extensive literature review. They note that exercise is recommended for pain reduction, specifically hip and knee exercises, and foot orthoses are recommended for pain reduction.
Sisk D, Fredericson M. Update of risk factors, diagnosis, and management of patellofemoral pain. Curr. Rev. Musculoskelet. Med. 2019;12(4):534–41. https://doi.org/10.1007/s12178-019-09593-z This is a review article looking at recent updates on risk factors, physical examination, and treatment of PFS. The authors note overuse in new runners is a risk factor for PFS, as well as inflexibility of the muscles surrounding the knee. Quadriceps strengthening is recommended for the treatment of PFS, and they discuss blood flow restriction therapy can lead to improved strength with lower-level exercise; however, more studies are needed in this area.
Lun VM, Wiley JP, Meeuwisse WH, Yanagawa TL. Effectiveness of patellar bracing for treatment of patellofemoral pain syndrome. Clin J Sport Med. 2005;15(4):235–40. https://doi.org/10.1097/01.jsm.0000171258.16941.13.
Nakagawa TH, Muniz TB, Baldon RD, Dias Maciel C, de Menezes Reiff RB, Serrão FV. The effect of additional strengthening of hip abductor and lateral rotator muscles in patellofemoral pain syndrome: a randomized controlled pilot study. Clin. Rehabil. 2008;22(12):1051–60. https://doi.org/10.1177/0269215508095357.
Barton CJ, Lack S, Hemmings S, Tufail S, Morrissey D. The “Best Practice Guide to Conservative Management of Patellofemoral Pain”: incorporating level 1 evidence with expert clinical reasoning. Br. J. Sports Med. 2015;49(14):923–34. https://doi.org/10.1136/bjsports-2014-093637.
Sisk D, Fredericson M. Taping, bracing, and injection treatment for patellofemoral pain and patellar tendinopathy. Curr. Rev. Musculoskelet. Med. 2020;13(4):537–44. https://doi.org/10.1007/s12178-020-09646-8.
Gross MT, Foxworth JL. The role of foot orthoses as an intervention for patellofemoral pain. J. Orthop. Sports Phys. Ther. 2003;33(11):661–70. https://doi.org/10.2519/jospt.2003.33.11.661.
Willy RW, Hoglund LT, Barton CJ, et al. Patellofemoral pain. J. Orthop. Sports Phys. Ther. 2019;49(9):CPG1–CPG95. https://doi.org/10.2519/jospt.2019.0302.
Kesary Y, Singh V, Frenkel-Rutenberg T, et al. Botulinum toxin injections as salvage therapy is beneficial for management of patellofemoral pain syndrome. Knee Surg Relat Res. 2021;33(1):39-39. https://doi.org/10.1186/s43019-021-00121-3.
Giles L, Webster K, McClelland J, Cook J. Quadriceps strengthening with and without blood-flow restriction in the treatment of patellofemoral pain – a double blind randomised trial. J Sci Med Sport. 2017;20:e100-e100. https://doi.org/10.1016/j.jsams.2017.01.081.
Ma YT, Li LH, Han Q, et al. Effects of trigger point dry needling on neuromuscular performance and pain of individuals affected by patellofemoral pain: a randomized controlled trial [Corrigendum]. J. Pain Res. 2020;13:2237–8. https://doi.org/10.2147/JPR.S278493.
Rahou-El-Bachiri Y, Navarro-Santana MJ, Gómez-Chiguano GF, et al. Effects of trigger point dry needling for the management of knee pain syndromes: a systematic review and meta-analysis. J. Clin. Med. 2020;9(7):2044. https://doi.org/10.3390/jcm9072044.
Kettunen JA, Harilainen A, Sandelin J, et al. Knee arthroscopy and exercise versus exercise only for chronic patellofemoral pain syndrome: a randomized controlled trial. BMC Med. 2007;5(1):38-38. https://doi.org/10.1186/1741-7015-5-38.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Walli, O., McCay, M. & Tiu, T. Patellofemoral Syndrome: a Review of Diagnosis and Treatment. Curr Phys Med Rehabil Rep 11, 139–143 (2023). https://doi.org/10.1007/s40141-023-00385-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-023-00385-8