Abstract
Purpose of Review
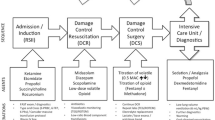
This review highlights the roles and responsibilities of anesthesiologists in the management of critically ill trauma patients in different countries around the world. It provides a summary of the scope of practice of different branches of anesthesiology that are involved in the resuscitation of trauma patients.
Recent Findings
The reduced indication for operative intervention in trauma along with the increasing role for anesthesia in managing trauma patients outside the operating room has created a demand for trauma acute care anesthesiologists. The leading obstacle to more prevalent offsite trauma anesthesia personnel is the lack of formal subspecialty training programs and credentialing requirements of different medical societies.
Summary
Trauma anesthesiologists act as a resource for anesthesiologists in the operating room and trauma patients during the trauma care pathway including prehospital transport, extracorporeal membrane oxygenation or ECMO service, trauma team both civilian and military, and complicated pain management.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
ASA House of Delegates/Executive Committee. Statement of principles of trauma anesthesia. American Society of Anesthesiologists 2013.
Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27:759–69.
Tobin J, et al. A checklist for trauma and emergency anesthesia. Anesth Analg. 2013;117(5):1178–84.
Albrecht E, Taffe P, Yersin B, et al. Undertreatment of acute pain (oligoanesthesia) and medical practice variation in prehospital analgesia of adult trauma patients: a 10-year retrospective study. British J of Anaesthesiol. 2013;11(1):96–106.
Choi JJ, Lin E, Gadsden J. Regional anesthesia for trauma outside the operating theatre. Curr Opin Anaesthesiol. 2013;26(4):495–500.
Lee BH, Kumar KK, Wu EC, et al. Role of regional anesthesia and analgesia in the opioid epidemic. Reg Anesth Pain Med. 2019;44:492–3.
Clay FJ, Watson WL, Newstead SV, et al. A systematic review of early prognostic factors for persisting pain following acute orthopedic trauma. Pain Res Manag. 2012;17(1):35–44.
Wu JJ, Lollo L, Grabinsky A. Regional anesthesia in trauma medicine. Anesth Research and Prac. 2011;2011:1–7.
Malchow RJ, Black IH. The evolution of pain management in the critically ill trauma patient: emerging concepts from the global war on terrorism. Crit Care Med. 2008;36(7):346–57.
Gadsden J, Warlick A. Regional anesthesia for the trauma patient: improving patient outcomes. Local Reg Anesth. 2015;8:45–55.
Helander EM, Eskander JP, Juneau CL. Preemptive analgesia, regional anesthesia, and prevention of chronic postoperative pain. Essentials of Reg Anesth. 2018;9(3):445–62.
Hards M, Brewer A, Bessant G, et al. Efficacy of prehospital analgesia with fascia iliaca compartment block for femoral bone fractures: a systematic review. Prehosp Disaster Med. 2018;33(3):299–307.
Simon BJ, Cushman J, Barraco R, et al. Pain management guidelines for blunt thoracic trauma. J Trauma Acute Care Surg. 2005;59(5):1256–67.
Candido KD, Kusper TM. Regional anesthesia and the patient with preexisting neuropathy. Anesth News 2018:53–61.
Horlocker TT, Wedel DJ, Rowlingson JC, et al. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine evidence-based guidelines. Reg Anesth Pain Med. 2010;35(1):64–101.
Tran AA, Lee D, Fassihi SC, et al. A systematic review of the effect of regional anesthesia on diagnosis and management of acute compartment syndrome in long bone fractures. Eur J Trauma Emerg Surg. 2020;46:1281–90.
Dohlman LE, Kwikiriza A, Ehie O. Benefits and barrier to increasing regional anesthesia in resource-limited settings. Local Reg Anesth. 2020;13:147–58.
Sollid S, et al. The role of the anaesthesiologist in air ambulance medicine. Curr Opin Anaesthesiol. 2017;30(4):513–7.
Marinangeli F, et al. Helicopter emergency medical service in Italy: reality and perspectives. 2007;26(6):292–8.
Lossius HM, et al. Prehospital advanced life support provided by specially trained physicians: is there a benefit in terms of life-years gained? Acta Anaesthesiol Scandc. 2002;46:771–8.
Ruskin et al. Helicopter air ambulance services. Curr Opin Anaesthesiol 2019:32(2):252-256.
Breckwoldt J, et al. Expertise in prehospital endotracheal intubation by emergency medicine physicians-comparing ‘proficient performers’ and ‘experts.’ Resuscitationc. 2012;83:434–9.
Egberink RE, Otten H-J, Ijzerman MJ, et al. Trauma team activation varies across Dutch emergency departments: a national survey. Scand J Trauma Resuscit Emerg Med. 2015;23:100–5.
American College of Surgeons Committee on Trauma. Advanced Trauma Life Support (ATLS) student course manual, 10th. Chicago: American College of Surgeons; 2018.
Cummings GE, Mayes DC. A comparative study of designated Trauma Team Leaders on trauma patient survival and emergency department length-of-stay. CJEM. 2007;9(2):105–10.
Gerardo CJ, et al. The rapid impact on mortality rates of a dedicated care team including trauma and emergency physicians at an academic medical center. J Emerg Med. 2011;40(5):586–91.
Wong K, Petchell J. Trauma teams in Australia: a national survey. ANZ J Surg. 2003;73:819–25.
Bach JA, Leskovan JJ, Scharschmidt T, Boulger C, Papadimos TJ, Russell S, Bahner DP, Stawicki SPA. Multidisciplinary approach to multi-trauma patient with orthopedic injuries: the right team at the right time. Int J Crit Illn Inj Sci. 2017;7(1):32–7.
Lavigeur 0, et al. The effect of a multidisciplinary trauma team leader paradigm at a tertiary trauma center: 10-year experience. Emerg Med Int 2020:2020:1–7. This article demonstrates the impact of a multidisciplinary TTL program in 2005 on the mortality of trauma patients in at the Montreal General Hospital. There was a significant reduction in mortality of 1.25% or a relative reduction of 16% (p value = 0.0058; rate ratio 0.844 (95% CI 0.747–0.952)).
Groenestege-Kreb D, et al. Trauma team. Br J Anaesth. 2014;113:258–65.
Moore L, et al. Mortality in Canadian trauma systems: a multicenter cohort study. Ann Surg. 2017;265(1):212–7.
Mccunn M, Dutton RP, Heim H, Gilmore CE wet al. Trauma anesthesia contributions to the acute care anesthesiology model and the perioperative surgical home. Curr Anesthesiol Rep 2016:6:22–29. The authors are the first to describe a perioperative surgical home (PSH) model where anesthesiologist subspecialized in trauma and acute care can help improve long-term outcomes that parallels the American College of Surgeons acute care surgery (ACS) model.
Gutsche JT. Cardiac and critical care anesthesiologists may be ideal members of the mobile ECMO team. Journal of cardiothoracic and vascular anesthesia 2016:30(6):1439-1440. Patients cared for with a formal ECMO team had a significant improved survival compared to patients prior to the creation of the team.
Nwozuzu, M.L et al. Mobile extracorporeal membrane oxygenation teams: the North American versus the European experience. J Cardiothorac Vasc Anes 2016:30:1441–48
Firstenberg MS, et al. ECMO and echo: the evolving role of quantitative echo in the management of patients requiring extracorporeal membrane oxygenation. J Am Soc Echocardiogr. 2012;25:641–3.
Platts G, et al. The role of echocardiography in the management of patients supported by extracorporeal membrane oxygenation. J Am Soc Echocardiogr. 2012;25(2):131–41.
Tien et al. Advances in damage control resuscitation and surgery: implications on the organization of future military field forces. Can J Surg 2015:58(3):91–97. Review of NATO policies for medical missions, use of damage control resuscitation, and damage control surgery including organization of field forces.
Beckett A, Tien H. What’s new in operative trauma surgery in the last 10 years. Curr Opin Crit Care. 2013;19:599–604.
Kuckelman J et al. MASCAL management from Baghdad to Boston: top ten lessons learned from modern military and civilian MASCAL events. Current Trauma Reports 2018:4:138-48. This review summarizes lessons learned during mass casualty events that are essential to effectively manage military and civilian MASCAL events.
Torres A C, Bebarta V S, April MD, et al. Ketamine administration in prehospital combat injured patients with traumatic brain injury: a 10-year report of survival. Cureus 2020:12(7):e9248.
Mathais Q, Montcriol A, Cotte J, Gil C, Contargyris C, et al. Anesthesia during deployment of a military forward surgical unit in low-income countries: a register study of 1547 anesthesia cases. PLoS ONE. 2019;14(10):e0223497.
Tobin J et al. Anesthesia for trauma patients. Military Medicine 2018:(183)10:32–35. This paper offers a clinical practice guideline that attempts to provide an outline for the care of traumatic injured patients in the battlefield. Refer to the full JTS CPG at https://jts.amedd.army.mil/index.
Maddry JK, et al. Critical care air transport team evacuation of medical patients without traumatic injury. Mil Med. 2017;182(11):1874–80.
Ingraham AM, Cohen ME, Raval MV, Ko CY, Nathens AB. Effect of trauma center status on 30-day outcomes after emergency general surgery. J Am Coll Surg. 2011;212:277–86.
Liau A, Havidich JE, Dutton RP. An overview of adverse events in the National Anesthesia Clinical Outcomes Registry (NACOR). New Orleans: LA American Society of Anesthesiologists Annual Meeting; 2014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ryan Perlman, Jessie Lo, Vida Zhang, Gabriele Baldini, Alexander Amir, and Joseph Po declare they have no conflict of interest. The authors do not have any potential conflicts of interest to disclose.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Anesthesia for Trauma
Rights and permissions
About this article
Cite this article
Perlman, R., Lo, J., Po, J. et al. Trauma and the Anesthesiologist: an International Perspective. Curr Anesthesiol Rep 12, 258–265 (2022). https://doi.org/10.1007/s40140-021-00507-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-021-00507-9