Abstract
Purpose of Review
The purpose of this review is to assess how residual neuromuscular block impacts postoperative pulmonary complications and whether we can modify the risk by improving certain aspects in daily clinical care.
Recent findings
Postoperative respiratory impairment may be due to various causes, such as age, surgery type, comorbidity, smoking, preoperative anemia, and general anesthesia. However, increasing evidence suggests that residual neuromuscular block is an important risk factor for postoperative pulmonary complications and may affect the outcome. Conflicting data from some recent reports show that the use of quantitative neuromuscular monitoring alone does not preclude residual neuromuscular block and that improvements in the interpretation of neuromuscular monitoring may be required. Pulmonary complications seem to be reduced for train-of-four ratios > 0.95 before tracheal extubation compared with > 0.9.
Summary
This review stresses the need for appropriate management of neuromuscular block in the prevention of postoperative pulmonary complications but acknowledges that the causes are multifactorial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Beecher et al. first reported in 1954 that the use of neuromuscular blocking agents (NMBAs) is associated with anesthesia-related mortality [1]. Cooper and colleagues investigated anesthesia-related complications leading to admission to an intensive care unit. Nearly half of the cases were associated with incomplete neuromuscular recovery [2]. In 1997, Berg et al. demonstrated that if the train-of-four ratio (TOFR) was < 0.7 in the recovery room in patients who had received pancuronium, there was a higher incidence of postoperative pulmonary complications (PPCs) than when TOFRs had recovered to > 0.7 (at the time the study was performed, a TOFR ratio of 0.7 was the accepted threshold for acceptable recovery; that threshold is now recognized as a TOFR ratio of 0.9) [3]. Multiple factors, including surgical, anesthetic, and patient variables, contribute to the etiology of PPCs. Surgical risk factors include emergency surgery, long duration of surgery, and type of surgery. Anesthetic causes include the use of opioids, NMBAs, and general anesthesia. Patient risk factors include chronic obstructive pulmonary disease, diabetes, obesity, and unmodifiable risk factors, such as advanced age and male sex [4, 5]. For instance, PPCs are more common in elderly patients, and hypoxemia and length of hospital stay were significantly increased in the elderly [6].
Residual Neuromuscular Blockade and PPCs: The Evidence From the Past
Mechanisms of PPCs
The partial impairment of muscular activity in the postoperative period through residual effects of intraoperatively administered NMBAs can contribute to the development of PPCs through different mechanisms: impaired contraction of ventilatory muscles with atelectasis formation, inability to cough, and impaired swallowing, with accumulation of airway secretions and aspiration of gastric contents [7••, 8]. The effects of NMBAs, reversal agents, and neuromuscular transmission (NMT) monitoring on the development of PPCs have often been described only by registry-based retrospective studies [9]. However, these studies, together with investigations in volunteers and patients, provide enough evidence about the causes of PPCs, e.g., Sundman et al. found that partial neuromuscular paralysis is associated with a 4-fold increase in the incidence of misdirected swallowing [10]. Furthermore, Asai and Isono concluded that residual neuromuscular block (NMB) after anesthesia is a cause of postoperative aspiration pneumonia [11], while other authors concluded that postoperative residual NMB increased the incidence of oxygen desaturation, postoperative pneumonia, airway obstruction, and reintubation [6, 12,13,14]. Even mild residual NMB can impair hypoxic respiratory drive and thus is a risk factor for increased early postoperative mortality [15, 16]. Postoperative hypoxemia through residual NMB may be produced by several mechanisms: these include the deleterious effects on both chemoreception and upper airway patency in addition to effects on the phrenic nerve-diaphragm neuromuscular junction [17]. Indeed, several researchers have shown that partial NMB disturbs upper airway patency [18]. As in the intensive care unit where silent pulmonary aspiration is the main cause of ventilator-associated pneumonia [19], postoperative pneumonia may also be caused by silent aspiration. In addition, pulmonary function is impaired with residual NMB, e.g., residual NMB after the use of vecuronium, atracurium, or rocuronium results in reductions in forced vital capacity and peak expiratory flow in the immediate postoperative period [20,21,22].
Effect of the Reversal of Residual Block on PPCs
In a large retrospective study of the effect of anesthetic management on perioperative morbidity and mortality in the Netherlands in 2005, Arbous et al. demonstrated that the lack of intraoperative reversal of residual NMB was an independent risk factor for 24 h anesthesia-related postoperative morbidity and mortality [23]. These findings were recently substantiated by a single-center study that also found that PPCs were less frequent if neostigmine had been used [12]. Patients who received an NMBA but not a reversal agent were 2.3 times more likely to develop PPCs than those who received neostigmine. In 2017, a multicenter retrospective study of 11,355 adults in the USA also suggested that the use of neostigmine reduces the risk of PPCs. Not administering neostigmine was associated with a 70% increase in the odds of respiratory complications [24].
Residual NMB and PPCs: The Conflicting Evidence
In 2012, a large observational cohort study by Grosse-Sundrup et al. found that postoperative hypoxia (< 90% saturation) and reintubation requiring unplanned admission to the intensive care unit within 7 days of surgery were significantly increased in the group receiving an NMBA; respective odds ratios were 1.36 and 1.40 [13]. Qualitative monitoring of NMT (use of a peripheral nerve stimulator) did not decrease this risk, and neostigmine reversal increased the risk of postoperative desaturation to less than 90% (odds ratio 1.32) and reintubation (odds ratio 1.76). The use of intermediate-acting NMBAs during anesthesia seemed thus associated with an increased risk of clinically meaningful respiratory complications. These authors attributed the increased respiratory problems after reversal of NMBAs with neostigmine to neostigmine-induced NMB. However, neostigmine-induced “paradoxical weakness” is an uncommon occurrence [25, 26].
A second large cohort study was reported by McLean et al. in 2015 [9]. These authors found a statistically significant association between NMBAs and PPCs and that risk seemed dose-dependent. Another observational cohort study of the effects of NMBAs on postoperative pneumonia in patients was reported by Bulka et al. in 2016 [12]. They found that there was a statistically significant increase in postoperative pneumonia for patients receiving an NMBA compared with patients who did not (odds ratio 1.79) and for patients who received an NMBA but did not receive a reversal agent compared with patients who received an NMBA and a reversal agent.
The most conflicting data came out in 2019 with a publication from the POPULAR study endorsed and funded by the European Society of Anaesthesiology (ESA) [27]. These authors concluded that “the use of neuromuscular blocking drugs is associated with an increased risk of postoperative pulmonary complications, and use of reversal agents or neuromuscular monitoring could not decrease this risk.” However, the POPULAR study reported that 17,150 patients received an NMBA, but in more than 10,000 of these patients, NMT monitoring was not applied, and the extubation of their tracheas was based solely on clinical criteria. Moreover, approximately one-third of the patients who received objective NMT monitoring were extubated with a TOFR< 0.9. It is thus difficult to state that the general conclusion of the POPULAR study is supported by the data. A more relevant conclusion should be to reinforce the fact that when inadequately managed, NMBAs could lead to severe adverse events. Nevertheless, in a subsequent reply to one of the multiple responses that came to the POPULAR study [28], in the Lancet Respir Med, the original authors presented an analysis of bundles of neuromuscular management and reformulated that the patients in their study receiving NMB without quantitative monitoring and without reversal did not have a worse pulmonary outcome than those who did have monitoring and reversal; even more, the use of quantitative NMT monitoring in 4182 patients compared with qualitative NMT monitoring in 2686 patients was seemingly not associated with a reduced risk of PPCs [29].
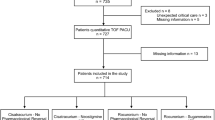
Another study shows that between 2012 and 2018, the management of NMBAs in a single-center operating room had substantially evolved: although NMT monitoring and the reversal of NMB in the operating room had increased over time, residual NMB remained apparent (14%) in the recovery room [30]. Even if monitored, a considerable number of their patients still had a TOFR< 0.9 and even < 0.7 in the recovery room. The authors analyzed six subgroups in their study and provided a complicated overview of the inappropriate practice of NMB management in their institution. For instance, a subgroup of patients was not monitored but received neostigmine probably as routine practice. The limited predictability of neostigmine reversal for moderate NMB has previously been confirmed by Blobner et al. [31]. Even patients who received sugammadex had a TOFR between 0.7 and 0.9 in their study [30]. As these patients’ NMBs were all monitored intraoperatively, the lack of appropriate dosing of sugammadex and the lack of checking the TOFR before the extubation of the patients’ tracheas could be the only explanations for the residual NMBs in the PACU in that particular study. As a consequence, these authors concluded that the failure to recognize residual NMB in their institution could ultimately be attributed to a failure to monitor NMB or a lack of understanding of neuromuscular pharmacology [32]. Their findings suggest that the use of quantitative NMT monitoring alone does not preclude residual NMB and that improvements in the interpretation of NMT monitoring may be required.
Residual NMB and PPCs: The Recent Evidence
The past evidence that PPCs are associated with the use of NMBAs and even more with residual paralysis is clear in the adult surgical population, as described in the first part of this review. Very recently, a study in 6507 non-cardiac surgical procedures was performed in children aged 0 to 10 years, and a high intraoperative NMBA dose seemed to be significantly associated with an increased risk of PPCs within 3 days of surgery [33]. Furthermore, the NMBA dose was significantly associated with an increased risk of intensive care admission, as well as increased costs and prolonged hospital stay. These findings, indeed, align with previous results published in adults [34] but add important considerations unique to infants and children, a population traditionally less investigated in regard to PPCs after NMB.
Even more important is the recent work from Broens et al. [35••]. These authors found that, despite full reversal of partial NMB at the thumb, impairment of the peripheral chemoreflex may persist at a TOFR greater than 0.9 following reversal with neostigmine and sugammadex or spontaneous recovery of the NMB. Eikermann et al. demonstrated that even when the TOFR recovered to 0.95, respiratory function tests may still be depressed in some patients [21]. There is now robust evidence that NMBAs additionally influence ventilatory control by acting within the peripheral chemoreflex loop at the carotid bodies [36, 37]. Indeed, a TOFR of 0.9 is not the equivalent of full recovery, and we now know, from Broens’ work, that the chemoreflex is impaired even at this level of recovery. Remembering that at a TOFR of 0.9, 75–80% of the nicotinic receptors may be blocked, the patient may thus show signs of some neuromuscular (or chemical) imbalance. Perhaps our recommended threshold for neuromuscular recovery needs revision, and particularly in at-risk patients, we should therefore preferably require a TOFR > 0.99 (by electromyography or mechanomyography—likely higher for acceleromyography [38]). A post hoc analysis of the prospective observational European multicenter cohort study (POPULAR) of PPCs now suggests that, in patients receiving quantitative NMT monitoring, PPCs are reduced for TOFR > 0.95 before tracheal extubation compared with TOFR > 0.9 [39]. Second, in Broens’ results, there is also a suggestion that patients receiving sugammadex had less blunting of the hypoxic ventilatory response (45% of patients) than neostigmine (64% of patients) and 83% of patients undergoing spontaneous recovery. This begs the question of whether sugammadex at its recommended or even higher doses assures a better recovery of the chemoreflex.
Are PPCs Reduced with the Use of Sugammadex?
In recent years, numerous clinical trials analyzed in meta-analyses have shown a decreased incidence of respiratory events and residual curarization in patients treated with sugammadex compared with neostigmine [40,41,42,43]. Since the use of rocuronium-sugammadex significantly reduces the incidence of residual NMB in the recovery room and residual NMB is associated with a greater incidence of major and minor respiratory complications, sugammadex may be beneficial. Fuchs-Buder et al. suggest that sugammadex may improve postoperative pulmonary outcome in a population at risk, most likely by a more efficient reversal of NMB with less residual paralysis [44]. Ledowski et al. found a lower risk for adverse pulmonary outcome in ASA 3 and 4 patients after reversal with sugammadex compared with neostigmine or none. This effect was more pronounced in elderly patients [45]. There is some, albeit very limited, evidence that NMB reversal with sugammadex may be associated with fewer PPCs than neostigmine in patients with obstructive sleep apnea [46]. Finally, Cappellini et al. performed a study in patients who, after rocuronium administration, received neostigmine or sugammadex: the authors found an early (0 min) but not long-lasting (30 min) association between diaphragm failure and recovery drug treatment; a full recovery in baseline diaphragm function was observed only in patients receiving sugammadex [47]. In contrast to these favorable findings for sugammadex and PPCs, another study found no differences in pulmonary function in 130 adult patients reversed with sugammadex or neostigmine after major abdominal surgery [48]. There was no difference in 30-day postoperative outcomes following sugammadex and acetylcholinesterase inhibitor use in colorectal surgery patients [49]. In older adults undergoing prolonged surgery, sugammadex was associated with a 40% reduction in residual neuromuscular block, a 10% reduction in 30-day hospital readmission rate, but no difference in the occurrence of postoperative pulmonary complications [50]. Since the introduction of sugammadex, there has been renewed interest in the application of deep NMB in some types of surgery. To the best of the author’s knowledge, no study has identified that maintaining deep NMB improves surgical outcome or reduces PPCs [51].
Conclusions
The pharmacokinetics of modern NMBAs suggest that they should have little clinical effect a few hours after emergence, yet PPCs occur more frequently for several days in patients receiving them. Multiple factors, including surgical, anesthetic, and patient variables, contribute to the etiology of PPCs. There is, however, enough evidence that residual NMB after anesthesia is a cause of increased oxygen desaturation, postoperative pneumonia, airway obstruction, and reintubation. In recent years, conflicting data have indicated that the use of reversal agents or NMT monitoring could not decrease the risk of PPCs. However, in these studies, guidelines for NMT monitoring were insufficiently implemented, probably because the benefit of the reversal of residual NMB is still poorly understood by clinicians. Sugammadex use might contribute to a greater reduction of residual NMB after surgery compared with neostigmine, and hence, it may possibly reduce postoperative respiratory morbidity. Quantitative NMT monitoring and the correct interpretation of it preclude residual NMB and may, through that mechanism, decrease the incidence of PPCs. Recent data suggest that PPCs are reduced for a TOFR > 0.95 before tracheal extubation compared with > 0.9.
References
Papers of particular interest, published recently, have been highlighted as:•• Of major importance
Beecher HK, Todd DP. A study of the deaths associated with anesthesia and surgery: based on a study of 599, 548 anesthesias in ten institutions 1948-1952, inclusive. Ann Surg. 1954;140:2–35.
Cooper AL, Leigh JM, Tring IC. Admission on the intensive care unit after complications of anaesthetic techniques over 10 years. Anaesthesia. 1989;44:953–8.
Berg J, Viby-Mogensen J, Roed J, et al. Residual neuromuscular block is a risk factor for postoperative pulmonary complications—a prospective, randomised, and blinded study of postoperative pulmonary complications after atracurium, vecuronium and pancuronium. Acta Anaesthesiol Scand. 1997;41:1095–103.
Pedersen T, Viby-Mogensen J, Ringsted C. Anaesthetic practice and postoperative pulmonary complications. Acta Anaesthesiol Scand. 1992;36:812–8.
Karcz M, Papadakos PJ. Respiratory complications in the postanesthesia care unit: a review of pathophysiological mechanisms. Can J Respir Ther. 2013;49:21–9.
Murphy GS, Szokol JW, Avram MJ, Greenberg SB, Shear TD, Vender JS, et al. Residual neuromuscular block in the elderly: incidence and clinical implications. Anesthesiology. 2015;123:1322–36.
•• Miskovic A, Lumb AB. Postoperative pulmonary complications. Br J Anaesth. 2017;118:317–34 “State of the art” review of the mechanisms of postoperative pulmonary complications and approaches on how to minimize them.
Farhan H, Moreno-Duarte I, McLean D, Eikermann M. Residual paralysis: does it influence outcome after ambulatory surgery? Curr Anesthesiol Rep. 2014;4:290–302.
McLean DJ, Diaz-Gil D, Farhan HN, Ladha KS, Kurth T, Eikermann M. Dose-dependent association between intermediate-acting neuromuscular-blocking agents and postoperative respiratory complications. Anesthesiology. 2015;122:1201–13.
Sundman E, Witt H, Olsson R, Ekberg O, Kuylenstierna R, Eriksson LI. The incidence and mechanisms of pharyngeal and upper esophageal dysfunction in partially paralyzed humans: pharyngeal videoradiography and simultaneous manometry after atracurium. Anesthesiology. 2000;92:977–84.
Asai T, Isono S. Residual neuromuscular blockade after anesthesia: a possible cause of postoperative aspiration-induced pneumonia. Anesthesiology. 2014;120:260–2.
Bulka CM, Terekhov MA, Martin BJ, Dmochowski RR, Hayes RM, Ehrenfeld JM. Nondepolarizing neuromuscular blocking agents, reversal, and risk of postoperative pneumonia. Anesthesiology. 2016;125:647–55.
Grosse-Sundrup M, Henneman JP, Sandberg WS, et al. Intermediate acting non-depolarizing neuromuscular blocking agents and risk of postoperative respiratory complications: prospective propensity score matched cohort study. BMJ. 2012;345:e6329.
Murphy GS, Szokol JW, Marymont JH, et al. Intraoperative acceleromyographic monitoring reduces the risk of residual neuromuscular blockade and adverse respiratory events in the postanesthesia care unit. Anesthesiology. 2008;109:389–98.
Murphy GS, Brull SJ. Residual neuromuscular block: lessons unlearned. Part I: definitions, incidence, and adverse physiologic effects of residual neuromuscular block. Anesth Analg. 2010;111:120–8.
Fernandez-Bustamante A, Frendl G, Sprung J, Kor DJ, Subramaniam B, Martinez Ruiz R, et al. Postoperative pulmonary complications, early mortality, and hospital stay following noncardiothoracic surgery: a multicenter study by the perioperative research network investigators. JAMA Surg. 2017;152:157–66.
Eriksson LI, Sundman E, Olsson R, Nilsson L, Witt H, Ekberg O, et al. Functional assessment of the pharynx at rest and during swallowing in partially paralyzed humans: simultaneous videomanometry and mechanomyography of awake human volunteers. Anesthesiology. 1997;87:1035–43.
Cedborg AI, Sundman E, Bodén K, Hedström HW, Kuylenstierna R, Ekberg O, et al. Pharyngeal function and breathing pattern during partial neuromuscular block in the elderly: effects on airway protection. Anesthesiology. 2014;120:312–25.
Pneumatikos IA, Dragoumanis CK, Bouros DE. Ventilator-associated pneumonia or endotracheal tube-associated pneumonia? An approach to the pathogenesis and preventive strategies emphasizing the importance of endotracheal tube. Anesthesiology. 2009;110:673–80.
Kumar GV, Nair AP, Murthy HS, Jalaja KR, Ramachandra K, Parameshwara G. Residual neuromuscular blockade affects postoperative pulmonary function. Anesthesiology. 2012;117:1234–44.
Eikermann M, Groeben H, Hüsing J, Peters J. Accelerometry of adductor pollicis muscle predicts recovery of respiratory function from neuromuscular blockade. Anesthesiology. 2003;98:1333–7.
Eikermann M, Groeben H, Bünten B, Peters J. Fade of pulmonary function during residual neuromuscular blockade. Chest. 2005;127:1703–9.
Arbous MS, Meursing AE, van Kleef JW, et al. Impact of anesthesia management characteristics on severe morbidity and mortality. Anesthesiology. 2005;102:257–68.
Bronsert MR, Henderson WG, Monk TG, Richman JS, Nguyen JD, Sum-Ping JT, et al. Intermediate acting nondepolarizing neuromuscular blocking agents and risk of postoperative 30-day morbidity and mortality, and long-term survival. Anesth Analg. 2017;124:1476–83.
Song IA, Seo KS, Oh AY, No HJ, Hwang JW, Jeon YT, et al. Timing of reversal with respect to three nerve stimulator end-points from cisatracurium-induced neuromuscular block. Anaesthesia. 2015;70:797–802.
Choi ES, Oh AT, Seo KS, et al. Optimum dose of neostigmine to reverse shallow neuromuscular blockade with rocuronium and cisatracurium. Anaesthesia. 2016;71:443–9.
Kirmeier E, Eriksson LI, Lewald H, Jonsson Fagerlund M, Hoeft A, Hollmann M, et al. Post-anesthesia pulmonary complications after use of muscle relaxants (POPULAR): a multicenter prospective observational study. Lancet Respir Med. 2019;7:129–40.
Fuchs-Buder T. Neuromuscular monitoring and reversal: responses to the POPULAR study. Lancet Respir Med. 2019;7:e3.
Blobner M, Hunter JM, Ulm K, Hollmann M. Neuromuscular monitoring and reversal: responses to the POPULAR study – authors’ reply. Lancet Respir Med. 2019;7:e7–8.
Cammu G, Klewais L, Vandeput D, Foubert L. Neuromuscular monitoring, reversal and postoperative residual neuromuscular block: an intradepartmental survey over the years. Anaesth Intensive Care. 2020;48:73–5.
Blobner M, Eriksson LI, Scholz J, Motsch J, Della Rocca G, Prins ME. Reversal of rocuronium-induced neuromuscular blockade with sugammadex compared with neostigmine during sevoflurane anaesthesia: results of a randomised controlled trial. Eur J Anaesthesiol. 2010;27:874–81.
Prielipp RC, Magro M, Morell RC, Brull SJ. The normalization of deviance: do we (un) knowingly accept doing the wrong thing? Anesth Analg. 2010;110:1499–502.
Scheffenbichler FT, Rudolph MI, Friedrich S, Althoff FC, Xu X, Spicer AC, et al. Effects of high neuromuscular blocking agent dose on post-operative respiratory complications in infants and children. Acta Anaesthesiol Scand. 2020;64:156–67.
Thevathasan T, Shih SL, Safavi KC, Berger DL, Burns SM, Grabitz SD, et al. Association between intraoperative non-depolarising neuromuscular blocking agent dose and 30-day readmission after abdominal surgery. Br J Anaesth. 2017;119:595–605.
•• Broens SJL, Boon M, Martini CH, et al. Reversal of partial neuromuscular block and the ventilatory response to hypoxia: a randomized controlled trial in healthy volunteers. Anesthesiology. 2019;131:467–76 At a first view controversial or at least unexpected findings: highly recommended and good for teaching.
Eriksson LI. Reduced hypoxic chemosensitivity in partially paralysed man. A new property of muscle relaxants? Acta Anaesthesiol Scand. 1996;40:520–3.
Jonsson M, Wyon N, Lindahl SG, Fredholm BB, Eriksson LI. Neuromuscular blocking agents block carotid body neuronal nicotinic acetylcholine receptors. Eur J Pharmacol. 2004;497:173–80.
Capron F, Alla F, Hottier C, Meistelman C, Fuchs-Buder T. Can acceleromyography detect low levels of residual paralysis? A probability approach to detect a mechanomyographic train-of-four ratio of 0.9. Anesthesiology. 2004;100:1119–24.
Blobner M, Hunter JM, Meistelman C, Hoeft A, Hollmann MW, Kirmeier E, et al. Use of a train-of-four ratio of 0.95 versus 0.9 for tracheal extubation: an exploratory analysis of POPULAR data. Br J Anaesth. 2020;124:63–72.
Brueckmann B, Sasaki N, Grobara P, Li MK, Woo T, de Bie J, et al. Effects of sugammadex on incidence of postoperative residual neuromuscular blockade: a randomized, controlled study. Br J Anaesth. 2015;115:743–51.
Abad-Gurumeta A, Ripollés-Melchor J, Casans-Francés R, Evidence Anaesthesia Review Group, et al. A systematic review of sugammadex vs neostigmine for reversal of neuromuscular blockade. Anaesthesia. 2015;70:1441–52.
Carron M, Zarantonello F, Tellaroli P, Ori C. Efficacy and safety of sugammadex compared to neostigmine for reversal of neuromuscular blockade: a meta-analysis of randomized controlled trials. J Clin Anesth. 2016;35:1–12.
Hristovska AM, Duch P, Allingstrup M, Afshari A. The comparative efficacy and safety of sugammadex and neostigmine in reversing neuromuscular blockade in adults. A Cochrane systematic review with meta-analysis and trial sequential analysis. Anaesthesia. 2018;73:631–41.
Fuchs-Buder T, Nemes R, Schmartz D. Residual neuromuscular blockade: management and impact on postoperative pulmonary outcome. Curr Opin Anaesthesiol. 2016;29:662–7.
Ledowski T, Falke L, Johnston F, et al. Retrospective investigation of postoperative outcome after reversal of residual neuromuscular blockade: sugammadex, neostigmine or no reversal. Eur J Anaesthesiol. 2014;31:423–9.
Hafeez KR, Tuteja A, Singh M, et al. Postoperative complications with neuromuscular blocking drugs and/or reversal agents in obstructive sleep apnea patients: a systematic review. BMC Anesthesiol. 2018;18:91.
Cappellini I, Ostento D, Loriga B, Tofani L, De Gaudio AR, Adembri C. Comparison of neostigmine vs. sugammadex for recovery of muscle function after neuromuscular block by means of diaphragm ultrasonography in microlaryngeal surgery: a randomised controlled trial. Eur J Anaesthesiol. 2020;37:44–51.
Alday E, Muñoz M, Planas A, Mata E, Alvarez C. Effects of neuromuscular block reversal with sugammadex versus neostigmine on postoperative respiratory outcomes after major abdominal surgery: a randomized-controlled trial. Can J Anaesth. 2019;66:1328–37.
Chae YJ, Joe HB, Oh J, Lee E, Yi IK. Thirty-day postoperative outcomes following sugammadex use in colorectal surgery patients. Retrospective Study J Clin Med. 2019;8:E97.
Togioka BM, Yanez D, Aziz MF, Higgins JR, Tekkali P, Treggiari MM. Randomised controlled trial of sugammadex or neostigmine for reversal of neuromuscular block on the incidence of pulmonary complications in older adults undergoing prolonged surgery. Br J Anaesth. 2020.
Bruintjes MH, van Helden EV, Braat AE, Dahan A, Scheffer GJ, van Laarhoven C, et al. Deep neuromuscular block to optimize surgical space conditions during laparoscopic surgery: a systematic review and meta-analysis. Br J Anaesth. 2017;118:834–42.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Guy Cammu is a principal consultant for MSD (Merck Sharp & Dohme). He has received research grants and lecture fees over the years and performed funded research on sugammadex.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
All reported studies/experiments with human or animal subjects performed by the author have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neuromuscular Blockade
Rights and permissions
About this article
Cite this article
Cammu, G. Residual Neuromuscular Blockade and Postoperative Pulmonary Complications: What Does the Recent Evidence Demonstrate?. Curr Anesthesiol Rep 10, 131–136 (2020). https://doi.org/10.1007/s40140-020-00388-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-020-00388-4