Abstract
Purpose of Review
Point-of-care ultrasound (POCUS) has been widely adopted in the management of trauma patients by emergency and surgical specialists. Advances in technology, portability, and affordability have contributed to its exponential growth, particularly in the field of trauma anesthesia where ultrasound usage has steadfastly blossomed in recent years.
Recent Findings
Studies and protocols have expanded beyond the oft-used focused assessment with sonography for trauma examination to include focused cardiac and lung examinations. POCUS may also be useful as an adjunct for airway management, vascular access, and intracranial pressure assessment. There has been a push to incorporate ultrasound use by paramedics and physicians in the pre-hospital trauma setting as well.
Summary
In this review, we discuss POCUS applications in the early stages of trauma care while emphasizing more recently published literature. This review is targeted toward anesthesia providers who wish to familiarize themselves with evidence-based applications of POCUS in various trauma settings.




Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Gleeson T, Blehar D. Point-of-care ultrasound in trauma. Semin Ultrasound, CT MRI. 2018. https://doi.org/10.1053/j.sult.2018.03.007. 2018 review article on point-of-care ultrasound in trauma.
Bakhru RN, Schweickert WD. Intensive care ultrasound: I. physics, equipment, and image quality. Ann Am Thorac Soc. 2014;10:540–8.
Phillips L, Hiew M. Point of care ultrasound: breaking the sound barrier in the emergency department. Australas J Ultrasound Med. 2019;22:3–5.
Ramsingh D, Singh S, Ross M, Williams W, Cannesson M. Review of point-of-care (POC) ultrasound for the 21st century perioperative physician. Curr Anesthesiol Rep. 2015;5:452–64.
Pace J, Arntfield R. Focused assessment with sonography in trauma: a review of concepts and considerations for anesthesiology. Can J Anesth. 2018;65:360–70.
Surgeons AC of (2012) Advanced trauma life support for doctors 10th Ed.
Bahner D, Blaivas M, Cohen HL, Fox JC, Hoffenberg S, Kendall J, et al. AIUM practice guideline for the performance of the focused assessment with sonography for trauma (FAST) examination. J Ultrasound Med. 2008;27:313–8.
Stengel D, Leisterer J, Ferrada P, Ekkernkamp A, Mutze S, Hoenning A. Point-of-care ultrasonography for diagnosing thoracoabdominal injuries in patients with blunt trauma. Cochrane Database Syst Rev. 2018. https://doi.org/10.1002/14651858.CD012669.pub2.
Quinn AC, Sinert R. What is the utility of the focused assessment with sonography in trauma (FAST) exam in penetrating torso trauma? Injury. 2011;42:482–7.
Rowell SE, Barbosa RR, Holcomb JB, et al. The focused assessment with sonography in trauma (FAST) in hypotensive injured patients frequently fails to identify the need for laparotomy: a multiinstitutional pragmatic study. Trauma Surg Acute Care Open. 2019. https://doi.org/10.1136/tsaco-2018-000207.
Liang T, Roseman E, Gao M, Sinert R. The utility of the focused assessment with sonography in trauma examination in pediatric blunt abdominal trauma. Pediatr Emerg Care. 2019:1.
Richards JR, Mcgahan JP. State of the art: focused assessment with sonography in trauma Richards and McGahan. Radiology. 2017. https://doi.org/10.1148/radiol.2017160107.
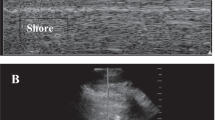
Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Acad Emerg Med. 2010;17:11–7.
Ianniello S, Di Giacomo V, Sessa B, Miele V. First-line sonographic diagnosis of pneumothorax in major trauma: accuracy of e-FAST and comparison with multidetector computed tomography. Radiol Med. 2014;119:674–80.
Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ. Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2013;26:567–81.
Ferrada P, Evans D, Wolfe L, et al. Findings of a randomized controlled trial using limited transthoracic echocardiogram (LTTE) as a hemodynamic monitoring tool in the trauma bay. J Trauma Acute Care Surg. 2014;76:31–8.
•• Saranteas T, Mavrogenis AF, Mandila C, Poularas J, Panou F. Ultrasound in cardiac trauma. J Crit Care. 2017;38:144–51. 2017 comprehensive review of cardiac trauma ultrasound.
Rippey JCR, Royse AG. Ultrasound in trauma. Best Pract Res Clin Anaesthesiol. 2009;23:343–62.
•• Pace J, Arntfield R. Focused assessment with sonography in trauma: a review of concepts and considerations for anesthesiology. Can J Anesth. 2018;65:360–70. 2018 review on the considerations for trauma ultrasound for anesthesiologists.
Kelly N, Esteve R, Papadimos TJ, Sharpe RP, Keeney SA, DeQuevedo R, et al. Clinician-performed ultrasound in hemodynamic and cardiac assessment: a synopsis of current indications and limitations. Eur J Trauma Emerg Surg. 2015;41:469–80.
Vegas A, Denault A, Royse C. A bedside clinical and ultrasound-based approach to hemodynamic instability - part II: bedside ultrasound in hemodynamic shock: continuing professional development approaches cliniques et échographiques au chevet du patient pour la gestion de l’instabilité. Can J Anesth Can d’anesthésie. 2014;61:1008–27.
Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, et al. Part 7: adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S444–64.
Gaspari R, Weekes A, Adhikari S, Noble VE, Nomura JT, Theodoro D, et al. Emergency department point-of-care ultrasound in out-of-hospital and in-ED cardiac arrest. Resuscitation. 2016;109:33–9.
Cureton EL, Yeung LY, Kwan RO, Miraflor EJ, Sadjadi J, Price DD, et al. The heart of the matter: utility of ultrasound of cardiac activity during traumatic arrest. J Trauma Acute Care Surg. 2012;73:102–10.
Bolvardi E, Pouryaghobi SM, Farzane R, Chokan NMJ, Ahmadi K, Reihani H. The prognostic value of using ultrasonography in cardiac resuscitation of patients with cardiac arrest. Int J Biomed Sci. 2016;12:110–4.
• Chen R. Synopsis of the point-of-care ultrasound assessment for perioperative emergencies. Can J Anesth. 2019;66:448–60. 2019 narrative review on POCUS applications for perioperative emergencies.
Ferrada P, Vanguri P, Anand RJ, Whelan J, Duane T, Wolfe L, et al. Flat inferior vena cava: indicator of poor prognosis in trauma and acute care surgery patients. Am Surg. 2012;78:1396–8.
• Jaidka A, Hobbs H, Koenig S, Millington SJ, Arntfield RT. Better with ultrasound: transesophageal echocardiography. Chest. 2019;155:194–201. 2019 review on transesophageal echocardiography in critically ill patients.
• Jasudavisius A, Arellano R, Martin J, McConnell B, Bainbridge D. A systematic review of transthoracic and transesophageal echocardiography in non-cardiac surgery: implications for point-of-care ultrasound education in the operating roomRevue méthodique de l’échocardiographie transthoracique et transœsophagienne en chir. Can J Anesth Can d’anesthésie. 2016;63:480–7. 2016 systematic review on the perioperative applications of echocardiography for non-cardiac patients.
• Leichtle SW, Singleton A, Singh M, Griffee MJ, Tobin JM. Transesophageal echocardiography in the evaluation of the trauma patient: a trauma resuscitation transesophageal echocardiography exam. J Crit Care. 2017;40:202–6. Recent review describing the TEE exam for trauma.
• Griffee MJ, Singleton A, Zimmerman JM, Morgan DE, Nirula R. The effect of perioperative rescue transesophageal echocardiography on the management of trauma patients. A A case reports. 2016;6:387–90. Recent case series on the use of TEE for trauma patients.
Burns JM, Sing RF, Mostafa G, et al. The role of transesophageal echocardiography in optimizing resuscitation in acutely injured patients. J Trauma - Inj Infect Crit Care. 2005;59:36–42.
Watts S, Smith JE, Gwyther R, Kirkman E. Closed chest compressions reduce survival in an animal model of haemorrhage-induced traumatic cardiac arrest. Resuscitation. 2019;140:37–42.
Teran F, Dean AJ, Centeno C, Panebianco NL, Zeidan AJ, Chan W, et al. Evaluation of out-of-hospital cardiac arrest using transesophageal echocardiography in the emergency department. Resuscitation. 2019;137:140–7.
Michels G, Breitkreutz R, Pfister R. Value of lung ultrasound in emergency and intensive care medicine. Dtsch Med Wochenschr. 2014. https://doi.org/10.1055/s-0034-1387309.
Bouhemad B, Mongodi S, Via G, Rouquette I. Ultrasound for “lung monitoring” of ventilated patients. Anesthesiology. 2015. https://doi.org/10.1097/ALN.0000000000000558.
Kendall JL, Hoffenberg SR, Smith RS. History of emergency and critical care ultrasound: the evolution of a new imaging paradigm. Crit Care Med. 2007. https://doi.org/10.1097/01.CCM.0000260623.38982.83.
Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure the BLUE protocol. Chest. 2008. https://doi.org/10.1378/chest.07-2800.
•• Kruisselbrink R, Chan V, Cibinel GA, Abrahamson S, Goffi A. I-AIM (Indication, acquisition, interpretation, medical decision-making) framework for point of care lung ultrasound. Anesthesiology. 2017. https://doi.org/10.1097/aln.0000000000001779. 2017 paper describing focused lung ultrasound protocol designed for anesthesiologists.
Saraogi A. Lung ultrasound: present and future. Lung India. 2015. https://doi.org/10.4103/0970-2113.156245.
Ding W, Shen Y, Yang J, He X, Zhang M. Diagnosis of pneumothorax by radiography and ultrasonography: a meta-analysis. Chest. 2011;140:859–66.
Stone M. Ultrasound diagnosis of traumatic pneumothorax. J Emergencies, Trauma Shock. 2009. https://doi.org/10.4103/0974-2700.41788.
Lichtenstein DA, Mezière G, Lascols N, Biderman P, Courret JP, Gepner A, et al. Ultrasound diagnosis of occult pneumothorax. Crit Care Med. 2005. https://doi.org/10.1097/01.CCM.0000164542.86954.B4.
Lichtenstein DA, Menu Y. A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding Chest. 1995;108:1345–8.
Retief J, Chopra M. Pitfalls in the ultrasonographic diagnosis of pneumothorax. J Intensive Care Soc. 2017. https://doi.org/10.1177/1751143716681034.
Ball CG, Wyrzykowski AD, Kirkpatrick AW, Dente CJ, Nicholas JM, Salomone JP, et al. Thoracic needle decompression for tension pneumothorax: clinical correlation with catheter length. Can J Surg. 2010;53:184–8.
Karkhanis VS, Joshi JM. Pleural effusion: diagnosis, treatment, and management. Open Access Emerg Med. 2012;4:31.
Pumarejo Gomez L, Tran VH (2019) Hemothorax.
Grimberg A, Shigueoka DC, Atallah ÁN, Ajzen S, Iared W. Diagnostic accuracy of sonography for pleural effusion: systematic review. Sao Paulo Med J. 2010;128:90–5.
Abusedera M, Alkady O. Ultrasound-guided pleural effusion drainage with a small catheter using the single-step trocar or modified seldinger technique. J Bronchol Interv Pulmonol. 2016. https://doi.org/10.1097/LBR.0000000000000276.
Meyer KC. Diagnosis and management of interstitial lung disease. Transl Respir Med. 2014;2:4.
•• Ramsingh D, Mangunta VR. The use of point-of-care ultrasonography in trauma anesthesia. Anesthesiol Clin. 2019;37:93–106. 2019 review article on point-of-care ultrasound in trauma anesthesia.
• Skaarup SH, Løkke A, Laursen CB. The area method: a new method for ultrasound assessment of diaphragmatic movement. Crit Ultrasound J. 2018. https://doi.org/10.1186/s13089-018-0092-5. New method for more reliable quantification of diaphragm movement.
• Gottlieb M, Holladay D, Peksa GD. Ultrasonography for the confirmation of endotracheal tube intubation: a systematic review and meta-analysis. Ann Emerg Med. 2018;72:627–36. 2018 meta-analysis showing the additional value of ultrasound in determing tube position after intubation.
Osman A, Sum KM. Role of upper airway ultrasound in airway management. J Intensive Care. 2016;5:10.
•• Kristensen MS, Teoh WH, Graumann O, Laursen CB. Ultrasonography for clinical decision-making and intervention in airway management: from the mouth to the lungs and pleurae. Insights Imaging. 2014;5:253–79. Concise review of clinical applications of airway ultrasound.
Sitzwohl C, Langheinrich A, Schober A, Krafft P, Sessler DI, Herkner H, et al. Endobronchial intubation detected by insertion depth of endotracheal tube, bilateral auscultation, or observation of chest movements: randomised trial. BMJ. 2010;341:1143.
Ramsingh D, Frank E, Haughton R, Schilling J, Gimenez KM, Banh E, et al. Auscultation versus point-of-care ultrasound to determine endotracheal versus bronchial intubation. Anesthesiology. 2016;124:1012–20.
Chou HC, Tseng WP, Wang CH, Ma MH, Wang HP, Huang PC, et al. Tracheal rapid ultrasound exam (T.R.U.E.) for confirming endotracheal tube placement during emergency intubation. Resuscitation. 2011;82:1279–84.
Adi O, Chuan TW, Rishya M. A feasibility study on bedside upper airway ultrasonography compared to waveform capnography for verifying endotracheal tube location after intubation. Crit Ultrasound J. 2013;5:1–11.
Kristensen MS, Teoh WH, Rudolph SS. Ultrasonographic identification of the cricothyroid membrane: best evidence, techniques, and clinical impact. Br J Anaesth. 2016;117:i39–48.
Mallin M, Curtis K, Dawson M, Ockerse P, Ahern M. Accuracy of ultrasound-guided marking of the cricothyroid membrane before simulated failed intubation. Am J Emerg Med. 2014. https://doi.org/10.1016/j.ajem.2013.07.004.
Kristensen MS, Teoh WH, Rudolph SS, Tvede MF, Hesselfeldt R, Børglum J, et al. Structured approach to ultrasound-guided identification of the cricothyroid membrane: a randomized comparison with the palpation method in the morbidly obese. Br J Anaesth. 2015;114:1003–4.
Kristensen MS, Teoh WH, Rudolph SS, Hesselfeldt R, Børglum J, Tvede MF. A randomised cross-over comparison of the transverse and longitudinal techniques for ultrasound-guided identification of the cricothyroid membrane in morbidly obese subjects. Anaesthesia. 2016;71:675–83.
Airway management for anaesthesiologists. Pearls. http://airwaymanagement.dk/pearls. Accessed 17 Jun 2019.
Airway management for anaesthesiologists. TACA. http://airwaymanagement.dk/taca.
•• Perlas A, Arzola C, Van de Putte P. Point-of-care gastric ultrasound and aspiration risk assessment: a narrative review Échographie gastrique au chevet et évaluation du risque d’aspiration : un compte rendu narratif. Can J Anesth Can d’anesthésie. 2018;65:437–48. 2018 narrative review summarizes the knowledge on gastric ultrasound.
Perlas A, Van De Putte P, Van Houwe P, Chan VWS. I-AIM framework for point-of-care gastric ultrasound. Br J Anaesth. 2016;116:7–11.
Bouvet L, Desgranges FP, Aubergy C, Boselli E, Dupont G, Allaouchiche B, et al. Prevalence and factors predictive of full stomach in elective and emergency surgical patients: a prospective cohort study. Br J Anaesth. 2017;118:372–9.
Bainbridge D, McConnell B, Royse C. A review of diagnostic accuracy and clinical impact from the focused use of perioperative ultrasoundRevue de l’exactitude diagnostique et de l’impact clinique de l’utilisation ciblée de l’échographie périopératoire. Can J Anesth Can d’anesthésie. 2018;65:371–80.
• Alakkad H, Kruisselbrink R, Chin KJ, Niazi AU, Abbas S, VWS C, et al. Point-of-care ultrasound defines gastric content and changes the anesthetic management of elective surgical patients who have not followed fasting instructions: a prospective case seriesL’échographie au chevet détermine le contenu gastrique et modifie la. Can J Anesth Can d’anesthésie. 2015;62:1188–95. “Real world” data showing the impact of gastric ultrasound on decision making elective surgical patients.
Costantino TG, Parikh AK, Satz WA, Fojtik JP. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med. 2005;46:456–61.
Saugel B, Scheeren TWL, Teboul JL. Ultrasound-guided central venous catheter placement: a structured review and recommendations for clinical practice. Crit Care. 2017. https://doi.org/10.1186/s13054-017-1814-y.
de Souza TH, Brandão MB, Nadal JAH, Nogueira RJN. Ultrasound guidance for pediatric central venous catheterization: a meta-analysis. Pediatrics. 2018. https://doi.org/10.1542/peds.2018-1719.
Gregg SC, Murthi SB, Sisley AC, Stein DM, Scalea TM. Ultrasound-guided peripheral intravenous access in the intensive care unit. J Crit Care. 2010;25:514–9.
Huang H, Feng BH. Do not fear the difficult IV. Anesth Analg. 2017. https://doi.org/10.1213/ANE.0000000000002270.
•• Ueda K, Hussey P. Dynamic ultrasound-guided short-axis needle tip navigation technique for facilitating cannulation of peripheral veins in obese patients. Anesth Analg. 2017. https://doi.org/10.1213/ANE.0000000000001653. Newly defined method of ultrasound-guided IV access with significant increase in success rate.
• White L, Halpin A, Turner M, Wallace L. Ultrasound-guided radial artery cannulation in adult and paediatric populations: A systematic review and meta-analysis. Br J Anaesth. 2016. https://doi.org/10.1093/bja/aew097. Recent meta-analysis showing improved success rates for arterial line placement in adults using ultrasound vs. palpation.
• Moussa Pacha H, Alahdab F, Al-khadra Y, et al. Ultrasound-guided versus palpation-guided radial artery catheterization in adult population: A systematic review and meta-analysis of randomized controlled trials. Am Heart J. 2018. https://doi.org/10.1016/j.ahj.2018.06.007. Recent meta-analysis showing improved success rates for arterial line placement in children using ultrasound vs. palpation.
Sobolev M, Slovut DP, Lee Chang A, Shiloh AL, Eisen LA. Ultrasound-guided catheterization of the femoral artery: a systematic review and meta-analysis of randomized controlled trials. J Invasive Cardiol. 2015;27:318–23.
Hawthorne C, Piper I. Monitoring of intracranial pressure in patients with traumatic brain injury. Front Neurol. 2014. https://doi.org/10.3389/fneur.2014.00121.
Kinoshita K. Traumatic brain injury: pathophysiology for neurocritical care. J Intensive Care. 2016. https://doi.org/10.1186/s40560-016-0138-3.
Dubourg J, Javouhey E, Geeraerts T, Messerer M, Kassai B. Ultrasonography of optic nerve sheath diameter for detection of raised intracranial pressure: a systematic review and meta-analysis. Intensive Care Med. 2011;37:1059–68.
Dubourg J, Messerer M, Karakitsos D, Rajajee V, Antonsen E, Javouhey E, et al. Individual patient data systematic review and meta-analysis of optic nerve sheath diameter ultrasonography for detecting raised intracranial pressure: protocol of the ONSD research group. Syst Rev. 2013;2:1–6. https://doi.org/10.1186/2046-4053-2-62.
•• Robba C, Cardim D, Tajsic T, et al. Ultrasound non-invasive measurement of intracranial pressure in neurointensive care: a prospective observational study. PLoS Med. 2017. https://doi.org/10.1371/journal.pmed.1002356. Defining old and new ultrasound parameters to better correlate with increased ICP.
Helmke K, Hansen HC. Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension. I. Experimental study. Pediatr Radiol. 1996;26:701–5.
• Ketelaars R, Reijnders G, van Geffen GJ, Scheffer GJ, Hoogerwerf N. ABCDE of prehospital ultrasonography: a narrative review. Crit Ultrasound J. 2018. https://doi.org/10.1186/s13089-018-0099-y. 2018 narrative review presenting the use of prehospital ultrasound in the well-known ABCD approach.
Meadley B, Olaussen A, Delorenzo A, Roder N, Martin C, Clair TS, et al. Educational standards for training paramedics in ultrasound: a scoping review. BMC Emerg Med. 2017;17:1–14. https://doi.org/10.1186/s12873-017-0131-8.
• Bøtker MT, Jacobsen L, Rudolph SS, Knudsen L. The role of point of care ultrasound in prehospital critical care: a systematic review. Scand J Trauma Resusc Emerg Med. 2018. https://doi.org/10.1186/s13049-018-0518-x. 2018 systematic review showing that prehospital POCUS is feasible and changes management in trauma patients.
Nelson BP, Chason K. Use of ultrasound by emergency medical services: a review. Int J Emerg Med. 2008;1:253–9.
McCallum J, Vu E, Sweet D, Kanji HD. Assessment of paramedic ultrasound curricula: a systematic review. Air Med J. 2015;34:360–8.
Brun PM, Bessereau J, Chenaitia H, Pradel AL, Deniel C, Garbaye G, et al. Stay and play eFAST or scoop and run eFAST? That is the question! Am J Emerg Med. 2014;32:166–70.
Kim CH, Shin SD, Song KJ, Park CB. Diagnostic accuracy of focused assessment with Sonography for trauma (FAST) examinations performed by emergency medical technicians. Prehospital Emerg Care. 2012;16:400–6.
Walcher F, Weinlich M, Conrad G, Schweigkofler U, Breitkreutz R, Kirschning T, et al. Prehospital ultrasound imaging improves management of abdominal trauma. Br J Surg. 2006;93:238–42.
Garrone M. Prehospital ultrasound as the evolution of the Franco-German model of prehospital EMS. Crit Ultrasound J. 2011;3:141–7.
Liao SF, Chen PJ, Chaou CH, Lee CH. Top-cited publications on point-of-care ultrasound: the evolution of research trends. Am J Emerg Med. 2018;36:1429–38.
D’Alessandro PCP, Drennan IR, Newbigging J, Johri AM. Review: paramedic POCUS, turning our heads to the Prehospital side of the fence: a narrative review of education, training and future direction. POCUS J. 2018;3:6–12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Frederick H. Kuo, Holger M. Baumann, Pablo Perez d’Empaire, and Yi Deng declare they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Anesthesia for Trauma
Rights and permissions
About this article
Cite this article
Kuo, F.H., Baumann, H.M., d’Empaire, P.P. et al. Role of Point-of-Care Ultrasound in the Early Stages of Trauma Care. Curr Anesthesiol Rep 10, 69–79 (2020). https://doi.org/10.1007/s40140-020-00369-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-020-00369-7