Abstract
Purpose of Review
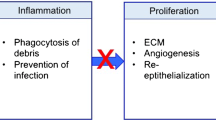
Tissue injury stimulates an inflammatory response that is mediated in part by alarmins. Alarmins are a group of endogenous molecules that trigger inflammation in response to damage. This class of molecules is becoming increasingly recognized for its ability to influence wound healing. This article will provide an overview of alarmins and outline the latest findings on these mediators in cutaneous wound healing.
Recent Findings
In addition to stimulating inflammatory cells, recent evidence suggests that alarmins can act on other cells in the skin to affect wound closure and the extent of scar tissue production. This review will focus on high-mobility group box-1 and IL-33, two alarmins that have received recent attention in the wound healing field.
Summary
Because a properly regulated inflammatory response is critical for optimal healing, further research must be done to fully understand the role of alarmins in the wound repair process.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Wilgus TA. Immune cells in the healing skin wound: influential players at each stage of repair. Pharmacol Res. 2008;58(2):112–6. https://doi.org/10.1016/j.phrs.2008.07.009.
Bianchi ME. DAMPs, PAMPs and alarmins: all we need to know about danger. J Leukoc Biol. 2007;81(1):1–5. https://doi.org/10.1189/jlb.0306164.
Klune JR, Dhupar R, Cardinal J, Billiar TR, Tsung A. HMGB1: endogenous danger signaling. Mol Med. 2008;14(7–8):476–84. https://doi.org/10.2119/2008-00034.Klune.
• Millar NL, O'Donnell C, McInnes IB, Brint E. Wounds that heal and wounds that don’t—the role of the IL-33/ST2 pathway in tissue repair and tumorigenesis. Semin Cell Dev Biol. 2017;61:41–50. This is an informative review article on IL-33 signaling and the role of this pathway in the repair of multiple tissue types. https://doi.org/10.1016/j.semcdb.2016.08.007.
Ranzato E, Patrone M, Pedrazzi M, Burlando B. HMGb1 promotes scratch wound closure of HaCaT keratinocytes via ERK1/2 activation. Mol Cell Biochem. 2009;332(1–2):199–205. https://doi.org/10.1007/s11010-009-0192-4.
Straino S, Di Carlo A, Mangoni A, De Mori R, Guerra L, Maurelli R, et al. High-mobility group box 1 protein in human and murine skin: involvement in wound healing. J Invest Dermatol. 2008;128(6):1545–53. https://doi.org/10.1038/sj.jid.5701212.
Ashcroft GS, Dodsworth J, van Boxtel E, Tarnuzzer RW, Horan MA, Schultz GS, et al. Estrogen accelerates cutaneous wound healing associated with an increase in TGF-beta1 levels. Nat Med. 1997;3(11):1209–15. https://doi.org/10.1038/nm1197-1209.
Ashcroft GS, Greenwell-Wild T, Horan MA, Wahl SM, Ferguson MW. Topical estrogen accelerates cutaneous wound healing in aged humans associated with an altered inflammatory response. Am J Pathol. 1999;155(4):1137–46. https://doi.org/10.1016/S0002-9440(10)65217-0.
Ashcroft GS, Mills SJ, Lei K, Gibbons L, Jeong MJ, Taniguchi M, et al. Estrogen modulates cutaneous wound healing by downregulating macrophage migration inhibitory factor. J Clin Invest. 2003;111(9):1309–18. https://doi.org/10.1172/JCI16288.
Shin JU, Noh JY, Lee JH, Lee WJ, Yoo JS, Kim JY, et al. In vivo relative quantitative proteomics reveals HMGB1 as a downstream mediator of oestrogen-stimulated keratinocyte migration. Exp Dermatol. 2015;24(6):478–80. https://doi.org/10.1111/exd.12713.
Ranzato E, Patrone M, Pedrazzi M, Burlando B. Hmgb1 promotes wound healing of 3T3 mouse fibroblasts via RAGE-dependent ERK1/2 activation. Cell Biochem Biophys. 2010;57(1):9–17. https://doi.org/10.1007/s12013-010-9077-0.
Mitola S, Belleri M, Urbinati C, Coltrini D, Sparatore B, Pedrazzi M, et al. Cutting edge: extracellular high mobility group box-1 protein is a proangiogenic cytokine. J Immunol. 2006;176(1):12–5. https://doi.org/10.4049/jimmunol.176.1.12.
Hirth DA, Singer AJ, Clark RA, McClain SA. Histopathologic staining of low temperature cutaneous burns: comparing biomarkers of epithelial and vascular injury reveals utility of HMGB1 and hematoxylin phloxine saffron. Wound Repair Regen. 2012;20(6):918–27. https://doi.org/10.1111/j.1524-475X.2012.00847.x.
Lanier ST, McClain SA, Lin F, Singer AJ, Clark RA. Spatiotemporal progression of cell death in the zone of ischemia surrounding burns. Wound Repair Regen. 2011;19(5):622–32. https://doi.org/10.1111/j.1524-475X.2011.00725.x.
McNamara AR, Zamba KD, Sokolich JC, Jaskille AD, Light TD, Griffin MA, et al. Apoptosis is differentially regulated by burn severity and dermal location. J Surg Res. 2010;162(2):258–63. https://doi.org/10.1016/j.jss.2009.01.038.
Singer AJ, McClain SA, Taira BR, Guerriero JL, Zong W. Apoptosis and necrosis in the ischemic zone adjacent to third degree burns. Acad Emerg Med. 2008;15(6):549–54. https://doi.org/10.1111/j.1553-2712.2008.00115.x.
Holmes CJ, Plichta JK, Gamelli RL, Radek KA. Burn injury alters epidermal cholinergic mediators and increases HMGB1 and caspase 3 in autologous donor skin and burn margin. Shock. 2017;47(2):175–83. https://doi.org/10.1097/SHK.0000000000000752.
Marchetti C, Di Carlo A, Facchiano F, Senatore C, De Cristofaro R, Luzi A, et al. High mobility group box 1 is a novel substrate of dipeptidyl peptidase-IV. Diabetologia. 2012;55(1):236–44. https://doi.org/10.1007/s00125-011-2213-6.
Tepper OM, Galiano RD, Capla JM, Kalka C, Gagne PJ, Jacobowitz GR, et al. Human endothelial progenitor cells from type II diabetics exhibit impaired proliferation, adhesion, and incorporation into vascular structures. Circulation. 2002;106(22):2781–6. https://doi.org/10.1161/01.CIR.0000039526.42991.93.
Sinagra T, Merlo S, Spampinato SF, Pasquale RD, Sortino MA. High mobility group box 1 contributes to wound healing induced by inhibition of dipeptidylpeptidase 4 in cultured keratinocytes. Front Pharmacol. 2015;6:126.
Marfella R, Sasso FC, Rizzo MR, Paolisso P, Barbieri M, Padovano V, et al. Dipeptidyl peptidase 4 inhibition may facilitate healing of chronic foot ulcers in patients with type 2 diabetes. Exp Diabetes Res. 2012;2012:892706.
Schurmann C, Linke A, Engelmann-Pilger K, Steinmetz C, Mark M, Pfeilschifter J, et al. The dipeptidyl peptidase-4 inhibitor linagliptin attenuates inflammation and accelerates epithelialization in wounds of diabetic ob/ob mice. J Pharmacol Exp Ther. 2012;342(1):71–80. https://doi.org/10.1124/jpet.111.191098.
Wilgus TA. Regenerative healing in fetal skin: a review of the literature. Ostomy Wound Manage. 2007;53(6):16–31.
Walmsley GG, Maan ZN, Wong VW, Duscher D, Hu MS, Zielins ER, et al. Scarless wound healing: chasing the holy grail. Plast Reconstr Surg. 2015;135(3):907–17. https://doi.org/10.1097/PRS.0000000000000972.
Dardenne AD, Wulff BC, Wilgus TA. The alarmin HMGB-1 influences healing outcomes in fetal skin wounds. Wound Repair Regen. 2013;21(2):282–91. https://doi.org/10.1111/wrr.12028.
Zhang Q, O'Hearn S, Kavalukas SL, Barbul A. Role of high mobility group box 1 (HMGB1) in wound healing. J Surg Res. 2011.
Ali S, Mohs A, Thomas M, Klare J, Ross R, Schmitz ML, et al. The dual function cytokine IL-33 interacts with the transcription factor NF-kappaB to dampen NF-kappaB-stimulated gene transcription. J Immunol. 2011;187(4):1609–16. https://doi.org/10.4049/jimmunol.1003080.
Carriere V, Roussel L, Ortega N, Lacorre DA, Americh L, Aguilar L, et al. IL-33, the IL-1-like cytokine ligand for ST2 receptor, is a chromatin-associated nuclear factor in vivo. Proc Natl Acad Sci U S A. 2007;104(1):282–7. https://doi.org/10.1073/pnas.0606854104.
Chackerian AA, Oldham ER, Murphy EE, Schmitz J, Pflanz S, Kastelein RA. IL-1 receptor accessory protein and ST2 comprise the IL-33 receptor complex. J Immunol. 2007;179(4):2551–5. https://doi.org/10.4049/jimmunol.179.4.2551.
Palmer G, Lipsky BP, Smithgall MD, Meininger D, Siu S, Talabot-Ayer D, et al. The IL-1 receptor accessory protein (AcP) is required for IL-33 signaling and soluble AcP enhances the ability of soluble ST2 to inhibit IL-33. Cytokine. 2008;42(3):358–64. https://doi.org/10.1016/j.cyto.2008.03.008.
Kakkar R, Lee RT. The IL-33/ST2 pathway: therapeutic target and novel biomarker. Nat Rev Drug Discov. 2008;7(10):827–40. https://doi.org/10.1038/nrd2660.
Moussion C, Ortega N, Girard JP. The IL-1-like cytokine IL-33 is constitutively expressed in the nucleus of endothelial cells and epithelial cells in vivo: a novel ‘alarmin’? PLoS One. 2008;3(10):e3331. https://doi.org/10.1371/journal.pone.0003331.
Pichery M, Mirey E, Mercier P, Lefrancais E, Dujardin A, Ortega N, et al. Endogenous IL-33 is highly expressed in mouse epithelial barrier tissues, lymphoid organs, brain, embryos, and inflamed tissues: in situ analysis using a novel Il-33-LacZ gene trap reporter strain. J Immunol. 2012;188(7):3488–95. https://doi.org/10.4049/jimmunol.1101977.
Kuchler AM, Pollheimer J, Balogh J, Sponheim J, Manley L, Sorensen DR, et al. Nuclear interleukin-33 is generally expressed in resting endothelium but rapidly lost upon angiogenic or proinflammatory activation. Am J Pathol. 2008;173(4):1229–42. https://doi.org/10.2353/ajpath.2008.080014.
Yin H, Li X, Hu S, Liu T, Yuan B, Gu H, et al. IL-33 accelerates cutaneous wound healing involved in upregulation of alternatively activated macrophages. Mol Immunol. 2013;56(4):347–53. https://doi.org/10.1016/j.molimm.2013.05.225.
• Rak GD, Osborne LC, Siracusa MC, Kim BS, Wang K, Bayat A, et al. IL-33-dependent group 2 innate lymphoid cells promote cutaneous wound healing. J Invest Dermatol. 2016;136(2):487–496. This paper demonstrates an important role for IL-33 in the recruitment of ILC2 cells during skin repair. https://doi.org/10.1038/JID.2015.406.
• Oshio T, Komine M, Tsuda H, Tominaga SI, Saito H, Nakae S, et al. Nuclear expression of IL-33 in epidermal keratinocytes promotes wound healing in mice. J Dermatol Sci. 2017;85(2):106–114. This study suggests opposing nuclear and extracellular activities of IL-33 in wound healing. https://doi.org/10.1016/j.jdermsci.2016.10.008.
Khanna S, Biswas S, Shang Y, Collard E, Azad A, Kauh C, et al. Macrophage dysfunction impairs resolution of inflammation in the wounds of diabetic mice. PLoS One. 2010;5(3):e9539. https://doi.org/10.1371/journal.pone.0009539.
Mirza RE, Fang MM, Ennis WJ, Koh TJ. Blocking interleukin-1beta induces a healing-associated wound macrophage phenotype and improves healing in type 2 diabetes. Diabetes. 2013;62(7):2579–87. https://doi.org/10.2337/db12-1450.
Lee JS, Seppanen E, Patel J, Rodero MP, Khosrotehrani K. ST2 receptor invalidation maintains wound inflammation, delays healing and increases fibrosis. Exp Dermatol. 2016;25(1):71–4. https://doi.org/10.1111/exd.12833.
Yin H, Li X, Hu S, Liu T, Yuan B, Ni Q, et al. IL-33 promotes Staphylococcus aureus-infected wound healing in mice. Int Immunopharmacol. 2013;17(2):432–8. https://doi.org/10.1016/j.intimp.2013.07.008.
Li C, Li H, Jiang Z, Zhang T, Wang Y, Li Z, et al. Interleukin-33 increases antibacterial defense by activation of inducible nitric oxide synthase in skin. PLoS Pathog. 2014;10(2):e1003918. https://doi.org/10.1371/journal.ppat.1003918.
Acknowledgements
NIH funding (R21 ES022749 to TAW) is acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Wilgus has nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Wound Healing and Tissue Repair
Rights and permissions
About this article
Cite this article
Wilgus, T.A. Alerting the Body to Tissue Injury: The Role of Alarmins and DAMPs in Cutaneous Wound Healing. Curr Pathobiol Rep 6, 55–60 (2018). https://doi.org/10.1007/s40139-018-0162-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40139-018-0162-1