Abstract
The perioperative period represents a challenging situation for antithrombotic management. There is a lack of data on the perioperative use of direct oral anticoagulants (DOACs). We sought to describe the initial perioperative experience with these agents at our institution. Patients who were taking dabigatran, rivaroxaban, or apixaban prior to cardiac valve or coronary artery bypass surgery were included if they were at least 18 years old and had a platelet count >100,000 and hemoglobin >8 g/dl. We evaluated bleeding and thromboembolic events. Dabigatran, rivaroxaban, and apixaban were stopped a median (IQR) of 5 (4–6), 4 (3–7), and 9 (5–14) days prior to surgery (p = 0.35). Bridge therapy was used in 17 (30.9 %) patients. There were 10 (18.2 %) bleeding events and 1 (1.8 %) thromboembolism. In this single-center report, oral anticoagulation with DOACs was suspended earlier than recommended in patients undergoing major cardiac surgery. Bridge therapy was used frequently and associated with a non-statistically significant increase in bleeding. These findings highlight the need for larger studies.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Siegal D, Yudin J, Kaatz S, Douketis JD, Lim W, Spyropoulos AC. Periprocedural heparin bridging in patients receiving vitamin K antagonists: systematic review and meta-analysis of bleeding and thromboembolic rates. Circulation. 2012;126(13):1630–9.
Steinberg BA, Peterson ED, Kim S, et al. Use and outcomes associated with bridging during anticoagulation interruptions in patients with atrial fibrillation: findings from the outcomes registry for better informed treatment of atrial fibrillation (ORBIT-AF). Circulation. 2015;131(5):488–94.
Clark NP, Witt DM, Davies LE, et al. Bleeding, recurrent venous thromboembolism, and mortality risks during warfarin interruption for invasive procedures. JAMA Intern Med. 2015;175(7):1163–8.
Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114(2):119–25.
Gallego P, Apostolakis S, Lip GYH. Bridging evidence-based practice and practice-based evidence in periprocedural anticoagulation. Circulation. 2012;126(13):1573–6.
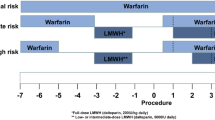
•• Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis. American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S–50S. These guidelines provide clinicians with valuable insight into the periprocedural management of many antithrombotic drugs.
Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955–62.
• van der Hulle T, Kooiman J, den Exter PL, Dekkers OM, Klok FA, Huisman MV. Effectiveness and safety of novel oral anticoagulants as compared with vitamin K antagonists in the treatment of acute symptomatic venous thromboembolism: a systematic review and meta-analysis. J Thromb Haemost. 2014;12(3):320–8. This meta-analysis nicely summarizes the effects of direct oral anticoagulants for the treatment of venous thromboembolism.
• Dyke C, Aronson S, Dietrich W, et al. Universal definition of perioperative bleeding in adult cardiac surgery. J Thorac Cardiovasc Surg. 2014;147:1458.e1–63.e1. This meta-analysis nicely summarizes the effects of direct oral anticoagulants for the treatment of venous thromboembolism.
Heidbuchel H, Verhamme P, Alings M, et al. European Heart Rhythm Association Practical Guide on the use of new oral anticoagulants in patients with non-valvular atrial fibrillation. Europace. 2013;15(5):625–51.
Boehringer Ingelheim Inc. Dabigatran (Pradaxa). Ridgefield: Boehringer Ingelheim Inc.; 2015.
Janssen Ortho LLC. Rivaroxaban (Xarelto). Gurabo: Janssen Ortho LLC; 2015.
Bristol-Myers Squibb Co. Apixaban (Eliquis). Gurabo: Bristol-Myers Squibb Co.; 2015.
Sherwood MW, Douketis JD, Patel MR, et al. Outcomes of temporary interruption of rivaroxaban compared with warfarin in patients with nonvalvular atrial fibrillation: results from the rivaroxaban once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke. Circulation. 2014;129(18):1850–9.
Healey JS, Eikelboom J, Douketis J, et al. Periprocedural bleeding and thromboembolic events with dabigatran compared with warfarin: results from the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) randomized trial. Circulation. 2012;126(3):343–8.
Garcia D, Alexander JH, Wallentin L, et al. Management and clinical outcomes in patients treated with apixaban vs warfarin undergoing procedures. Blood. 2014;124(25):3692–8.
Schulman S, Carrier M, Lee AYY, et al. Perioperative management of dabigatran: a prospective Cohort study. Circulation. 2015;132(3):167–73.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
Drs Buckley, Stevens, Deicicchi, Barra, Aldemerdash, and Fanikos all declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pharmacology of Acute Care.
Rights and permissions
About this article
Cite this article
Buckley, L.F., Stevens, C.A., Deicicchi, D.J. et al. Invited Commentary: Initial Experience with Direct Oral Anticoagulants in the Perioperative Setting. Curr Emerg Hosp Med Rep 4, 88–92 (2016). https://doi.org/10.1007/s40138-016-0096-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-016-0096-z