Abstract
Purpose of Review
This review aims to introduce vestibular implants as investigational devices with the potential to provide a novel rehabilitative treatment for patients with vestibular dysfunction.
Recent Findings
Vestibular implants are being investigated in clinical trials in the USA and Europe as a treatment option for patients with bilateral vestibular hypofunction (also called bilateral vestibulopathy). Analogous to cochlear implants, vestibular implants aim to encode head motion information and provide electric stimulation targeting the vestibular nerve of the inner ear. Published clinical trial results suggest vestibular implants can electrically drive vestibular mediated reflexes, including the vestibulo-ocular reflex and vestibulo-cervical reflex, as well as decreasing dizziness-specific symptoms and improving measures of quality of life.
Summary
Vestibular implants are an investigational technology with the potential to provide treatment options for patients with chronic bilateral vestibulopathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The vestibular system senses head motion and tilt and plays a major role in maintaining stable vision and balance. Patients with vestibular hypofunction typically experience difficulty with chronic imbalance, inadequate gaze stabilization with head motion, and are at an increased risk of falling. To date, treatment options for vestibular hypofunction are primarily limited to vestibular rehabilitation exercises intended to encourage central adaptation and compensation, avoiding medications that interfere with central compensation (vestibular suppressants), and safety measures to help prevent falls. Vestibular implants (VI) present a potentially restorative treatment option analogous to the use of cochlear implants for treating severe hearing loss. By modifying existing cochlear implant technology, VIs aim to convert head motion information into an electric signal presented to branches of the implanted ear’s vestibular nerve. Published results from clinical trials describe several promising observations and outcomes.
Vestibular Anatomy
Able to encode head movement and tilt relative to gravity, the vestibular labyrinth provides crucial information for our sensation of balance and equilibrium. Composed of bilateral pairs of five end organs, the vestibular labyrinths sense both angular (rotational) acceleration via the semicircular canals and linear acceleration via the otolith organs. Combined, the three orthogonally oriented semicircular canal pairs (horizontal canals, right anterior and left posterior canals [RALP], and left anterior and right posterior canals [LARP]) sense head rotation in any direction. The otolith organs (saccule and utricle) sense translational head movements and tilt relative to the constant downward acceleration due to gravity.
Normally, vestibular hair cells encode head motion information as a change in a balanced tonic neuronal firing rate (non-zero baseline) such that head movements aligned with each end organ’s hair cells increase the firing rate, encoding an excitatory signal. In contrast, head movements in the opposite direction drive an inhibitory signal of decreased firing rates. The neuronal signal is conveyed along vestibular afferent neurons to the vestibular nuclei in the pons and medulla before being sent forward to vestibular reflex paths mediating the vestibulo-ocular, vestibulo-spinal, and vestibulo-cervical reflexes. In parallel, the signal is also sent to the cerebellum via the inferior olivary nucleus and cerebellar peduncles and to the cerebral cortex via thalamic pathways [1]. Additionally, vestibular signaling to the hippocampus plays a key role in spatial orientation and navigation [2,3,4].
Patient Population
Dizziness and imbalance are complex symptoms and can occur for several reasons, including dysfunction of the peripheral vestibular system. Patients with unilateral vestibular hypofunction often experience imbalance and impaired gaze stabilization with head movement directed towards the affected ear. When vestibular sensation is decreased in both ears (i.e., bilateral vestibular hypofunction [BVH]), patients experience a particularly debilitating disorder, often causing chronic imbalance, postural instability, and oscillopsia [5]. It is estimated that 1.8 million adults worldwide have chronic symptoms of severe BVH [6]. Affected individuals often experience extra economic burdens and suffer reduced quality of life compared to their peers [7]. The current standard-of-care treatment for individuals with BVH includes avoiding vestibular suppressant medication, participating in vestibular rehabilitation, and taking safety precautions to minimize the risk of falling [8]. While some patients successfully manage their symptoms with this treatment approach, there are no restorative treatment options currently widely available for patients with chronic, poorly compensated BVH.
Following the success of cochlear implants in treating patients with severe to profound hearing loss, several groups have explored restoring vestibular function with electrical stimulation. These efforts have led to the development of four investigational VI devices currently being studied in human clinical trials. While patients with unilateral or moderate BVH may eventually have the potential to benefit from VI technology, only patients with more severe BVH are currently considered candidates for inclusion in VI clinical trials [9, 10].
Existing Devices
Four groups have published on VIs in humans: Geneva and Maastricht Universities (Geneva-Maastricht), University of Washington, Johns Hopkins University, and more recently at the University of Las Palmas in the Canary Islands (Table 1). VIs in use by the first three groups typically feature three stimulating electrode arrays, each designed to be inserted into one of the three semicircular canals near the neurosensory epithelium of the ampulla. This intralabyrinthine positioning places the stimulating electrodes near each canal’s ampullary nerve. One or more return electrodes are placed either in the inner ear or far from the stimulating electrodes.
The first device implanted in a human with the intent of prosthetically stimulating the vestibular nerve was performed by Jean-Philippe Guyot, founder of what became the Geneva-Maastricht team, in 2007, in a patient with bilateral deafness and vestibular loss undergoing cochlear implantation. Using a modified MED-EL GmbH cochlear implant, Guyot et al. designed a cochleo-vestibular (CI/VI) implant with a separate vestibular electrode lead positioned near the posterior ampullary nerve outside of the bony labyrinth [11,12,13]. Over time, while maintaining the essential CI/VI design, that research group and the MED-EL engineers working with them have redesigned their electrode arrays for stimulation of all three ampullary nerves and have transitioned to intralabyrinthine implantation rather than trying to place electrodes near nerves without entering the labyrinth. An example CI/VI implant is illustrated in Fig. 1. As of January 2024, published use of their device use was limited to brief episodes of stimulation in a clinical laboratory setting, and recipients only use the device’s CI function in daily life outside the laboratory. Their most recently described device continues to include electrodes for both cochlear and vestibular stimulation while improving the design of the external processor for daily use [14,15,16]. They are currently recruiting patients for a trial investigating the response to 3 weeks of combined CI/VI stimulation (ClinicalTrials.gov: NCT04918745).
Illustration of a cochleo-vestibular implant showing the cochlear electrode lead positioned in the scala tympani and the three vestibular stimulating electrode arrays positioned near the ampulla of each semicircular canal (original figure from [© 45])
The University of Washington (UW) group worked with Cochlear Ltd. Engineering to develop a VI modified from a Cochlear CI24RE (Freedom) cochlear implant [17,18,19]. That device had three electrode arrays with three electrode contacts per array and a separate ball return electrode [18,19,20], and it was initially proposed as a sort of pacemaker intended to mitigate episodes of vertigo due to acute unilateral hypofunction in patients diagnosed with Menière’s disease. Perhaps in part because they had Menière’s disease and preexisting sensorineural hearing loss, all of the first four recipients experienced additional hearing loss after implantation with three of the four developing a profound loss. Their experience with post-implantation hearing loss, in part, led to the development of a second-generation device with a CI/VI design. That device, also modified from the Nucleus Freedom cochlear implant, has three VI arrays with two electrode contacts per array, an intracochlear array with 16 electrodes (16-mm Cochlear Hybrid-L array), and a ball return electrode [21].
The Labyrinth Devices Multichannel Vestibular Implant™ (MVI), the device under investigation by the Johns Hopkins team, is currently the only stand-alone vestibular implant that human recipients use in daily life as a treatment rather than only during experiments (Fig. 2). Although still under study in the first clinical trial of prolonged, continuous VI use, the MVI has already been designated as “investigational, non-experimental” by the United States Food and Drug Administration. The MVI’s design is based on the MED-EL Concerto cochlear implant with three stimulating electrodes positioned at the distal end of each of three electrode arrays, a single return electrode, and a reference electrode for electrophysiologic recording. The MVI early feasibility study (ClinicalTrials.gov: NCT02725463) and associated clinical trials (ClinicalTrials.gov: NCT05676944 and NCT05674786) have characterized safety, tolerability, and efficacy of the MVI for 1–7 years of continuous (24 h/day or during all waking hours) vestibular stimulation [22, 23•].
Overview of the multichannel vestibular implant (MVI) device and motion-modulated stimulation mapping. A MVI receiver/stimulator with a stimulation electrode array and reference electrode. B–D Close-up view of the MVI’s 3 electrode arrays showing the posterior canal array, a forked array designed for interchangeable placement in the horizontal and anterior canal (depending on the side of surgery), and a reference electrode. E Surgical diagram illustrating MVI electrode placement in each of 3 canal ampullae and the optional placement of the reference electrode in the common crus (the Johns Hopkins group has since moved away from positioning the reference electrode in the common crus). F–G The positioning of the external 3D motion sensor in the head-worn unit (HWU) of an MVI recipient. The power and control unit (PCU) hangs on a lanyard and provides power and control signals to the implant. The patient is wearing a 3D video-oculography system used for recording eye movements during MVI testing (electrically evoked vestibulo-ocular reflex [eeVOR]). H–K Example showing how 3D head velocity waveforms are encoded to a pulse rate and amplitude (red, horizontal; blue, LARP; green, RALP) motion-modulated signal. Waveforms can be generated by gyroscopic input or computer-generated for stationary testing (original figure was modified from © Boutros et al. [22])
Most recently, a group at the University of Las Palmas de Gran Canaria has described a CI/VI, the CI24RE(VEST), as a modified version of Cochlear’s CI24RE system, designed with a single vestibular electrode array with three electrode contacts and a 19-contact perimodiolar intracochlear array [24, 25]. Developed by Cochlear Ltd., that device’s VI array is intended to target the otolith organs for implantation near the saccule via an oval window insertion. The team also described placing two separate implants, one targeting the cochlea and the other positioned in the vestibule targeting the otolith organs [26, 27].
Stimulus Approaches
There have been two prevailing approaches to stimulus patterns in the current literature. The first is to stimulate with pulse trains, which is useful for characterizing the performance of electrodes and measuring physiological responses to stimulation. A VI intended to restore rotational vestibular sensitivity should mimic the natural firing patterns of vestibular afferents in response to head movements. In all cases, cathodic-first biphasic charge-balanced current pulses are delivered to avoid tissue or electrode damage. In general, the excitation of branches of the vestibular nerve can be achieved by modulating three parameters—pulse amplitude, pulse width, and pulse rate/frequency. In the motion-modulated case, stimulation is up- or down-modulated from a baseline stimulus intensity, that the patient has already adapted to, to encode excitatory or inhibitory head movements in the plane of the canal being stimulated.
Initial studies from the Geneva-Maastricht and University of Washington groups used pulse trains with a constant pulse amplitude, width, and rate that were observed to produce eye movement responses, typically at an electrode-specific chosen pulse amplitude and consistent pulse width and pulse frequencies for each experiment [13, 21, 28, 29]. The range of pulse amplitudes used is typically in the range of 100 to 600 µA with the absolute safe maximum current being dependent on electrode design. Pulse trains are also used to characterize electrodes and decide the best motion modulation parameters for each patient [22, 30]. The Las Palmas group, primarily targeting saccular afferents with electrodes placed in the vestibule, report using constant, unmodulated pulse trains intended to replace baseline saccular activity due to the force of gravity [24,25,26,27, 31]. Unlike normal saccular activity, which varies with head tilt relative to gravity and translational motion, the constant-rate, constant-amplitude stimulation they describe conveys no information about head motion or tilt.
Motion-modulated stimulation has been implemented on an experimental basis by the Geneva-Maastricht group [22, 23, 30, 32]. They also performed motion-modulated testing with a sham mode in which they reverse the gyroscopes’ signals, effectively providing antagonistic signaling during head movements [32, 33]. However, the MVI studied at Johns Hopkins is unique in being the only canal-targeting VI thus far to deliver motion-modulated vestibular signaling chronically (currently up to 7 + years), allowing near continuous use by patients at home in daily life [23•]. The MVI modulates pulse amplitude and frequency to each semicircular canal based on the canal-specific gyroscopic inputs corresponding to head rotational velocity and acceleration, as illustrated in Fig. 2H–K. Based on perceived head movement and reflexive eye movements in the direction of the canal, the stimulating electrodes and pulse parameters are chosen to maximize the strength and selectivity of vestibular nerve-branch stimulation. When the head is at rest, each canal is stimulated at a baseline rate to replace the spontaneous firing rate of healthy vestibular afferents. Device testing is performed at both motion-modulated stimulation and with a non-motion-modulated placebo stimulation at the constant baseline pulse rate and amplitude [22, 32, 33]. Placebo or sham modes serve as within-patient controls.
Surgery
Vestibular implantation uses standard neurotologic surgical techniques to place stimulating electrodes near the distal afferent nerve fibers of the targeted vestibular end organ. While extra- and intra-labyrinthine implantation techniques have both been described, the most common technique involves intralabyrinthine positioning via a transmastoid approach [13, 28]. For the three devices under investigation designed for semicircular canal stimulation, the electrodes are placed adjacent to the neurosensory epithelium of the ampullae [18, 34, 35].
Similar to cochlear implant surgery, the initial surgical steps include making a postauricular approach to the mastoid cortex, forming a subperiosteal pocket, creating a bone well for the receiver/stimulator, and completing a cortical mastoidectomy. As the surgery progresses, early aims include identifying the facial nerve and the otic capsule near the ampullae of the three semicircular canals. The location of the horizontal and anterior semicircular canal’s ampullae is often evident early during the surgical approach. However, the posterior canal’s ampulla is not directly visualized during surgery, as it lies medial to the vertical segment of the facial nerve and stapedius muscle. Understanding this anatomic relationship is important while drilling along the posterior canal to prevent facial nerve injury and facilitate proper placement of a canalotomy near but not into the ampulla. After the otic capsule is well defined, bone over the planned insertion site for each electrode is thinned until a “blue line” is visible (i.e., the bone is translucent). The three labyrinthotomies are opened just prior to inserting the stimulating electrode arrays. It is important to minimize the time the bony labyrinth is open, avoid suctioning near the openings, and prevent blood or bone dust from entering the labyrinth by covering the labyrinthotomies with hyaluronic acid gel to create a temporary seal between opening and electrode array insertion. The creation of a fourth labyrinthotomy for placement of a reference electrode has been described for placement of the MVI device; however, the Johns Hopkins team sometimes places the return electrode in a subperiosteal pocket near the receiver/stimulator.
As mentioned previously, the University of Las Palmas team’s CI/VI device is designed to target the saccule. They describe a modified cochlear implantation approach with the extension of the posterior tympanotomy superiorly providing access to the oval and round windows for electrode insertion. After performing a cochlear electrode array insertion via the round window, they insert the VI stimulating electrode array into the vestibule through the oval window via a stapedotomy. This approach was used while placing two cochlear implants concurrently and since transitioning to a combined CI/VI device [25, 27].
Physiologic Outcomes
Vestibular-mediated reflexes provide researchers and clinicians with a way to characterize and measure vestibular function. Video-oculography is a commonly used technique to characterize semicircular canal function through the vestibulo-ocular reflex (VOR) [22]. Other detectable vestibular reflexes include the vestibulo-colic reflex which can be subjectively observed as head motion in response to vestibular stimulation or objectively measured through the cervical vestibular evoked myogenic potentials, which are thought to be mediated by the saccule [36]. Depending on the targeted end organ, researchers can use these vestibular reflexes as an objective measure of a patient’s response to electric vestibular stimulation (Table 2).
Vestibular implants have been shown to drive canal-specific electrically evoked vestibulo-ocular reflex (eeVOR). Data from the first four participants implanted with the MVI at Johns Hopkins were reported to have 3-dimensional (3D) eeVOR approximately aligned with the targeted canal’s anatomic axis. Responses grew with the current amplitude and pulse rate. They observed similar results during whole body sinusoidal rotations on a rotary chair at 0.1–2 Hz. In addition to improvements in VOR gain, they also reported decreased (more normal) phase lead compared to preop in the 3 participants with preoperative data. The eeVOR and responses to whole-body rotations were also found to remain stable after 8 weeks of continuous device use. The University of Washington group published results from four implant recipients in 2015. They observed eeVOR response that scaled with stimulation current in magnitude, albeit with large misalignment between elicited VOR direction and target canal [19]. Geneva-Maastricht has also probed eeVOR responses and their suitability for replacing natural VOR, finding that sinusoidally-modulated stimulation produces eeVOR responses with similar frequency-dependent gain trends as VOR in response to whole-body rotations in healthy participants [37]. However, the magnitude of eye velocities elicited by electrical stimulation was lower than for normal VOR. They have also reported that residual natural and electrical vestibular contributions to the VOR are combined nonlinearly in VI recipients, indicating that more complex mapping strategies may be needed when some residual function is present in patients [38].
The Geneva-Maastricht group has conducted multiple clinical studies to test the performance of their CI/VI in a short-term experimental setting. Using the video head impulse test (vHIT) to test the VI’s ability to drive high-frequency angular vestibulo-ocular reflex in the plan of a canal receiving VI stimulation, they reported VOR that increased with increasing stimulation strength in most cases. They also reported a decrease in the corrective saccades suggesting the VOR was adequate to maintain gaze stabilization during a head impulse [32]. In a separate study, they reported on the VI’s ability to drive eeVOR-mediated gaze stabilization during walking by measuring dynamic visual acuity while walking on a treadmill [33]. The Las Palmas group also reported improvement in DVA scores and an increased organization of corrective saccades during head impulse tests under constant rate stimulation of the otolith organs. They speculated that otolith stimulation can also drive improvements in gaze stabilization, but the mechanism by which a stimulus that provides no motion or tilt information would do that is unclear [25].
Researchers from Las Palmas performed cervical and ocular vestibular evoked myogenic potential (cVEMP and oVEMP) testing for an evaluation of their devices. They report that cVEMP and oVEMP responses were obtained from both participants [27]. The Geneva-Maastricht group reported electromyographic signals they interpreted as electrically-evoked cVEMP responses in 5 of 8 tested patients in response to ampullary nerve stimulation [39].
Taken together, these results show the possibility for VIs to restore functional VOR in a broad frequency range and possible ability to drive otolith-mediated reflexes. Additionally, the responsiveness of the vestibular nerves to electric stimulation appears present even after longstanding (> 20 years) BVH [15, 40].
Clinical Outcomes
In addition to the promising results observed while measuring the physiologic vestibular reflexes during electrical stimulation, clinical trial participants have also demonstrated improvements in clinical assessments of gait and posture and patient-reported improvements in measures of dizziness-specific symptoms and quality of life.
Posture and Gait
Reporting on static posture tasks in their first 8 participants, the Johns Hopkins team found chronic VI stimulation improved their study participants’ ability to maintain static posture during the modified Romberg test (standing on compliant foam with feet together and eyes closed), and the Bruininks–Oseretsky test (BOT) balance subtest scores. BOT scores, which assess postural stability, were markedly improved compared to the participants’ pre-implantation baseline and placebo mode (non-motion-modulated constant baseline firing rate and pulse amplitude). These improvements were present 6 months after implantation and further improved 1 year after implantation. Regarding gait-related measurements, the reported improvements above the minimally important difference for the Timed Up & Go (TUG) test and the Dynamic Gait Index (DGI), while gait speed appeared unchanged. Similar to posture test outcomes, TUG and DGI scores were improved compared to the participant’s baseline and placebo mode testing, and improvements were reported for 6 months and 1 year after implantation [23•].
Participant-Reported Symptom Scores and Quality of Life
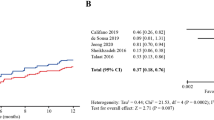
The Johns Hopkins team also analyzed patient-reported outcomes associated with their dizziness symptoms, perceived associated disability, and overall quality of life. The 36-Item Short-Form Health Survey (SF-36) and the Health Utilities Index Mark 3 (HUI-3) were used to assess their reported quality of life. Their first 8 participants mostly reported improvement in their quality of life. They also characterized changes in dizziness symptom scores with the Dizziness Handicap Inventory (DHI) and dizziness-associated disability using the Vestibular Disorders Activities of Daily Living (VADL) questionnaire. They reported improvement in symptom severity and associated disability scores compared to their preoperative baseline [23•]. Additionally, the Johns Hopkins team recently reported early improvements in dizziness symptoms, perceived associated disability, and overall quality of life in their first ten participants after six months of devise use. Except for the HUI-3, the implant participants' improvemnts were greater than the minimally important differences for each tool and, importantly, greater than a control group who did not udergo implantation [41••] .The Las Palmas group reported improvement in 6 of 9 Oscillopsia severity questionnaire questions for their 5 study participants, suggesting improved gaze stability [25].
Hearing Preservation
Although three of the four groups actively investigating VI devices include dedicated cochlear implant electrodes intended to implantation in ears with preexisting severe/profound sensorineural hearing loss, many patients with BVH do not require concurrent cochlear implant stimulation. It is estimated that 50% of patients with BVH have a moderate hearing loss or better, suggesting half the patients with BVH have aidable hearing [42]. Considering the need to include patients with normal or aidable hearing and BVH in the implementation of VI technology, hearing preservation after vestibular implantation is an important clinical safety outcome. Early outcomes from the University of Washington group found, not unexpectedly, that profound hearing loss is a potential risk of vestibular implantation [19]. They later found that combined interleaved stimulation of the cochlear and vestibular arrays produces changes in eeVOR and perceived pitch and loudness when compared to only VI or only CI stimulation. These interactions present additional challenges in restoring hearing with a combined CI/VI [43]. The Geneva-Maastricht team further investigated this risk by monitoring auditory brainstem responses (ABR) in a patient during the placement of a mock vestibular implantation array in a patient undergoing a planned translabyrinthine approach for a vestibular schwannoma. They reported that ABRs could be detected during the surgical approach, labyrinthotomies, and device insertion, before hearing was completely and permanently destroyed by the rest of the translabyrinthine tumor resection [44].
Whereas all other VI studies have focused on participants with hearing poor enough to need a CI, the study performed at Johns Hopkins is the first VI clinical trial to implant participants with normal or nearly normal preoperative hearing in the candidate ear. Including participants with unaided hearing requires careful counseling to adequately inform participants of the risk of hearing loss in the implanted ear. In addition to the other clinical outcomes, they have published audiometric results from their first 8 participants, who all had unaided hearing at the time of implantation. Reporting hearing outcomes for 6 months and 1 year after implantation, they found that most participants lost some hearing, and three participants experienced a severe-to-profound hearing loss. However, hearing sufficient for unaided communication was preserved in 5 of the 8 study participants. When hearing was preserved, the auditory outcomes were stable during the reported period of up to 1 year after implantation. Importantly, in reference to the improvements in their BVH symptoms, all participants, including those with significant hearing loss, reported net benefit and contentment with their decision to undergo vestibular implantation [23•]. A similar sentiment was reported for the early University of Washington participants regarding control of their Meniere’s disease symptoms [19].
Future Directions
Moving forward, several challenges in the field will need to be addressed. As described by a group of leading researchers in this field, these challenges include optimizing electrical stimulation, gaining regulatory approval, and the clinical implementation of this technology as a treatment pathway [45].
One area of active animal research is the targeted stimulation of the otolith end organs. As mentioned previously, three of the four current VI devices target the semicircular canals. This focus has been in part due to the canals’ dominant role in gaze stabilization, their anatomic relationship, and the relative ease in mimicking their neuronal signaling. However, the otolith organs also play an important role in vestibular sensation, especially in sensing head translations and tilt with respect to gravity. They contribute to otolith-ocular reflexes (OORs) and vestibulo-spinal reflexes that relate to posture and gait. The ability to selectively stimulate the otolith end organs, allowing for a more comprehensive restoration of vestibular function, will be an important focus during the continued development of VIs. While the Las Palmas group has targeted the saccule with a constant baseline input [24, 25], a motion-modulated stimulus based on tilt with respect to gravity and translational motion may offer better functional benefit. Considering the complexity of otolith hair cell orientation and signaling, directed otolith stimulation remains challenging without an electrode array with a high spatial resolution. Research in chinchillas with BVH shows prosthetic stimulation targeting the utricle and/or saccule of one implanted ear can partially restore OORs. Additionally, simultaneous prosthetic and natural tilt stimuli can result in better eye movements compared with prosthetic stimulation by itself [46].
Conclusion
Vestibular implants have the potential to fill the treatment gap experienced by patients with persistently debilitating symptoms of poorly compensated BVH. Although VI technology is currently limited to use in clinical trials, available published data highlight the promise this technology has for patients with BVH and other vestibular disorders. Results from the clinical trials described above suggest that VIs can drive semicircular canal-specific eeVOR, rehabilitate deficiencies in clinical measures of gait and posture, decrease BVH-associated symptoms and disability, and improve degradation in quality of life experienced by patients with BVH. Additionally, interim results from the MVI clinical trial suggest it is possible to preserve hearing sufficient for unaided communication, which will increase the reach of this technology to patients with vestibular hypofunction without severe-to-profound hearing loss. While clinical trial results so far have been promising, continued research is needed to better characterize the effect of VI stimulation in patients with BVH.
Data Availability
No datasets were generated or analysed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lysakowski A, et al. Anatomy of the Vestibular System. In: Flint PW, Francis HW, Haughey BH, Lesperance MM, Lund VJ, Robbins KT, et al., editors. Cummings otolaryngology. 7th ed. Philadelphia: Elsevier Inc.; 2021. pp. 1958–1976.e2.
Bigelow RT, Agrawal Y. Vestibular involvement in cognition: visuospatial ability, attention, executive function, and memory. J Vestib Res. 2015;25:73–89.
Bigelow RT, Semenov YR, Trevino C, Ferrucci L, Resnick SM, Simonsick EM, et al. Association between visuospatial ability and vestibular function in the Baltimore Longitudinal Study of Aging. J Am Geriatr Soc. 2015;63:1837–44.
Kamil RJ, Jacob A, Ratnanather JT, Resnick SM, Agrawal Y. Vestibular function and hippocampal volume in the Baltimore Longitudinal Study of Aging (BLSA). Otol Neurotol. 2018;39:765–71.
Strupp M, Kim JS, Murofushi T, Straumann D, Jen JC, Rosengren SM, et al. Bilateral vestibulopathy: diagnostic criteria consensus document of the classification committee of the Barany Society. J Vestib Res. 2017;27:177–89.
Ward BK, Agrawal Y, Hoffman HJ, Carey JP, Santina CC Della. Prevalence and impact of bilateral vestibular hypofunction results from the 2008 US National Health Interview Survey. 2017;139.
Sun DQ, Ward BK, Semenov YR, Carey JP. Santina CC Della. Bilateral vestibular deficiency quality of life and economic implications. 2014;21287:527–34.
Hall CD, Herdman SJ, Whitney SL, Anson ER, Carender WJ, Hoppes CW, et al. Vestibular rehabilitation for peripheral vestibular hypofunction: an updated clinical practice guideline from the Academy of Neurologic Physical Therapy of the American Physical Therapy Association. J Neurol Phys Ther. 2022;46:118–77.
•• van de Berg R, Ramos A, van Rompaey V, Bisdorff A, Perez-Fornos A, Rubinstein JT, et al. The vestibular implant: opinion statement on implantation criteria for research1. J Vestib Res. 2020;30:213–23. Opinion statement from the research groups currently investigating vestibular implant technology in clinical trials aimed at establishing candidacy criteria for vestibular implantation of adult patients with bilateral vestibulopathy (BVH) in a research setting.
van de Berg R, Ramos A, van Rompaey V, Bisdorff A, Perez-Fornos A, Rubinstein JT, et al. Erratum to: the vestibular implant: opinion statement on implantation criteria for research. J Vestib Res. 2023;33:85–85.
Guinand N, Guyot JP, Kingma H, Kos I, Pelizzone M. Vestibular implants: the first steps in humans. Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS. 2011;2262–4.
Guyot JP, Sigrist A, Pelizzone M, Kos MI. Adaptation to steady-state electrical stimulation of the vestibular system in humans. Ann Otol Rhinol Laryngol. 2011;120:143–9.
Wall C, Kos MI, Guyot J-P. Eye Movements in response to electric stimulation of the human posterior ampullary nerve. Ann Otol Rhinol Laryngol. 2007;116:369–74.
• Fornos AP, Cavuscens S, Ranieri M, Van De Berg R, Stokroos R, Kingma H, et al. The vestibular implant: a probe in orbit around the human balance system. J Vestib Res. 2017;27:51–61. Review of clinical trial results from The Geneva-Maastricht team, describing their experience with a combined cochleo-vestibular implant over ten years and including their first 13 participants.
Guinand N, van de Berg R, Cavuscens S, Stokroos RJ, Ranieri M, Pelizzone M, et al. Vestibular implants: 8 years of experience with electrical stimulation of the vestibular nerve in 11 patients with bilateral vestibular loss. ORL. 2015;77:227–40.
Guyot JP, Perez FA. Milestones in the development of a vestibular implant. Curr Opin Neurol. 2019;32:145–53.
Phillips C, DeFrancisci C, Ling L, Nie K, Nowack A, Phillips JO, et al. Postural responses to electrical stimulation of the vestibular end organs in human subjects. Exp Brain Res. 2013;229:181–95.
Golub JS, Ling L, Nie K, Nowack A, Shepherd SJ, Bierer SM, et al. Prosthetic implantation of the human vestibular system. Otol Neurotol. 2014;35:136–47.
Phillips JO, Ling L, Nie K, Jameyson E, Phillips CM, Nowack AL, et al. Vestibular implantation and longitudinal electrical stimulation of the semicircular canal afferents in human subjects. J Neurophysiol. 2015;113:3866–92.
Phillips C, Ling L, Oxford T, Nowack A, Nie K, Rubinstein JT, et al. Longitudinal performance of an implantable vestibular prosthesis. Hear Res. 2015;322:200–11.
Rubinstein JT, Ling L, Nowack A, Nie K, Phillips JO. Results from a second-generation vestibular implant in human subjects: diagnosis may impact electrical sensitivity of vestibular afferents. Otol Neurotol. 2020;41:68–77.
Boutros PJ, Schoo DP, Rahman M, Valentin NS, Chow MR, Ayiotis AI, et al. Continuous vestibular implant stimulation partially restores eye-stabilizing reflexes. JCI Insight. 2019;4.
• Chow MR, Ayiotis AI, Schoo DP, Gimmon Y, Lane KE, Morris BJ, et al. Posture, gait, quality of life, and hearing with a vestibular implant. N Engl J Med. 2021;384:521–32. Describes the early clinical outcomes from the first eight participants implanted in the Multichannel Vestibular Implant Early Feasibility Study being performed at Johns Hopkins, the first clinical trial looking at long-term chronic vestibular implant stimulation.
Rodriguez Montesdeoca I, Ramos de Miguel A, González JCF, Barreiro SB, Pérez Fernández N, Vanspauwen R, et al. Differences in vestibular-evoked myogenic potential responses by using cochlear implant and otolith organ direct stimulation. Front Neurol. 2021;12.
Rodríguez-Montesdeoca I, de Miguel ÁR, Falcón-González JC, Borkoski-Barreiro S, Benítez-Robaina S, Guerra-Jimenez G, et al. Dynamic visual acuity results in otolith electrical stimulation in bilateral vestibular dysfunction. J Clin Med. 2022;11:5706.
Miguel A, Falcon Gonzalez JC, Ramos de Miguel Macias A. Vestibular response to electrical stimulation of the otolith organs. Implications in the development of a vestibular implant for the improvement of the sensation of gravitoinertial accelerations. J Int Adv Otol. 2017;13:154–61.
Macias AR, De Miguel AR, Montesdeoca IR, Barreiro SB, González JCF. Chronic electrical stimulation of the otolith organ: preliminary results in humans with bilateral vestibulopathy and sensorineural hearing loss. Audiol Neurotol. 2020;25:79–90.
Guyot JP, Sigrist A, Pelizzone M, Feigl GC, Kos MI. Eye movements in response to electrical stimulation of the lateral and superior ampullary nerves. Ann Otol Rhinol Laryngol. 2011;120:81–7.
Boutabla A, Cavuscens S, Ranieri M, Crétallaz C, Kingma H, van de Berg R, et al. Simultaneous activation of multiple vestibular pathways upon electrical stimulation of semicircular canal afferents. J Neurol. 2020;267:273–84.
Fornos AP, Guinand N, Van De Berg R, Stokroos R, Micera S, Kingma H, et al. Artificial balance: restoration of the vestibulo-ocular reflex in humans with a prototype vestibular neuroprosthesis. Front Neurol. 2014;5 APR:1–11.
Curthoys IS, Smith PF, de Miguel AR. Why should constant stimulation of saccular afferents modify the posture and gait of patients with bilateral vestibular dysfunction? The saccular substitution hypothesis. J Clin Med. 2022;11:1132.
Guinand N, Van de Berg R, Cavuscens S, Ranieri M, Schneider E, Lucieer F, et al. The video head impulse test to assess the efficacy of vestibular implants in humans. Front Neurol. 2017;8.
Guinand N, Van de Berg R, Cavuscens S, Stokroos R, Ranieri M, Pelizzone M, et al. Restoring visual acuity in dynamic conditions with a vestibular implant. Front Neurosci. 2016;10:1–6.
van de Berg R, Guinand N, Guyot JP, Kingma H, Stokroos RJ. The modified ampullar approach for vestibular implant surgery: feasibility and its first application in a human with a long-term vestibular loss. Front Neurol. 2012;FEB:1–7.
Schoo DP, Ward BK, Chow MR, Ayiotis AI, Fernández Brillet C, Boutros PJ, et al. Vestibular implant surgery. Laryngoscope. 2024;134:1842–6.
Fife TD, Colebatch JG, Kerber KA, Brantberg K, Strupp M, Lee H, et al. Practice guideline: cervical and ocular vestibular evoked myogenic potential testing. Neurology. 2017;89:2288–96.
van de Berg R, Guinand N, Khoa Nguyen TA, Ranieri M, Cavuscens S, Guyot JP, et al. The vestibular implant: frequency-dependency of the electrically evoked vestibulo-ocular reflex in humans. Front Syst Neurosci. 2015;8:1–12.
van de Berg R, Guinand N, Ranieri M, Cavuscens S, Nguyen TAK, Guyot JP, et al. The vestibular implant input interacts with residual natural function. Front Neurol. 2017;8.
Fornos AP, van de Berg R, Armand S, Cavuscens S, Ranieri M, Crétallaz C, et al. Cervical myogenic potentials and controlled postural responses elicited by a prototype vestibular implant. J Neurol. 2019;266:33–41.
Schoo DP, Ayiotis AI, Fernandez Brillet C, Chow MR, Lane KE, Ward BK, et al. Vestibular implantation can work even after more than 20 years of bilateral vestibular hypofunction. Otol Neurotol. 2023;44:168–71.
•• Ayiotis Al, Schoo DP, Fernandez Brillet C, Lane KE, Carey JP, Della Santina CC. Patient-reported outcomes after vestibular implantation for bilateral vestibular hypofunction. JAMA Otorlaryngology-Head & Neck Surgery. 2024;150:240. Describes improvements in dizziness symptoms, perceived associated vestibular disability, and health-related quality of ife in the first etn participants implanted with the MVI after six months of device use.
Lucieer F, Vonk P, Guinand N, Stokroos R, Kingma H, van de Berg R. Bilateral vestibular hypofunction: insights in etiologies, clinical subtypes, and diagnostics. Front Neurol. 2016;7:1–11.
Phillips JO, Ling L, Nowack A, Rebollar B, Rubinstein JT. Interactions between auditory and vestibular modalities during stimulation with a combined vestibular and cochlear prosthesis. Audiol Neurotol. 2020;25:96–108.
van de Berg R, Lucieer F, Guinand N, van Tongeren J, George E, Guyot JP, et al. The vestibular implant: hearing preservation during intralabyrinthine electrode insertion-A case report. Front Neurol. 2017;8:1–7.
Stultiens JJA, Lewis RF, Phillips JO, Boutabla A, Della Santina CC, Glueckert R, et al. The next challenges of vestibular implantation in humans. J Assoc Res Otolaryngol. 2023;24:401–12.
Chow MR, Fernandez Brillet C, Hageman KN, Roberts DC, Ayiotis AI, Haque RM, et al. Binocular 3-D otolith-ocular reflexes: responses of chinchillas to natural and prosthetic stimulation after ototoxic injury and vestibular implantation. J Neurophysiol. 2023;129:1157–76.
Funding
This work was supported in part by funding from the National Institute on Deafness and Other Communications Disorders (U01DC019364, and R01DC18300); the National Institute on Aging (R01AG076701); and the National Institute of Biomedical Imaging and Bioengineering (T32EB003383).
Author information
Authors and Affiliations
Contributions
All authors contributed significantly to the preparation of the manuscript. EOV and RS contributed equally as the first authors.
Corresponding author
Ethics declarations
Conflict of Interest
CCDS is the founder and chief executive officer/chief scientific officer of, and holds an equity interest in Labyrinth Devices, LLC which has a partnership with Med-El GmbH. These conflicts of interest are managed according to the Johns Hopkins School of Medicine’s policies. DPS, EOV, and RS do not have any conflicts of interests associated with this work to disclose.
Ethics Approval
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki Declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vesper, E.O., Sun, R., Della Santina, C.C. et al. Vestibular Implantation. Curr Otorhinolaryngol Rep (2024). https://doi.org/10.1007/s40136-024-00502-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s40136-024-00502-8